Abstract
Cow’s milk allergy (CMA) is one of the most common pediatric food allergies. The prevalence and severity of CMA have increased dramatically in the last decades, under the pressure of environmental factors in genetically predisposed individuals. Among the environmental influences, nutritional factors play a crucial role. Diet is the most modifiable factor, representing a potential target for the prevention and treatment of CMA. In this review, we report the most scientific-based nutritional strategies for preventing and managing pediatric CMA. In addition, we propose the most complete supplement of compounds able to prevent nutrient deficiencies in CMA pediatric patients and to positively influence the disease course.
1. Introduction
Cow’s milk allergy (CMA) is one of the most common pediatric food allergies (FAs), affecting up to 3% of the children population. CMA derives from a breakdown of immune tolerance against cow’s milk proteins (α-lactalbumin, β-lactoglobulin, serum albumin, caseins, bovine serum albumins and others) that generally occurs in the first years of life [1]. Commercial milk is subjected to a heat treatment process to make it sterile, which through the Maillard reaction can induce the formation of deleterious compounds, such as the advanced glycation end products Nε-(carboxyethyl) lysine, Nε-(carboxymethyl) lysine, pentosidine, pyrraline, methylglyoxal-lysine dimer, glyoxal-lysine dimer and argpyrimidine, that may play a role in the pathogenesis of allergies [2]. CMA may present different phenotypes based on the immune mechanisms: IgE mediated, non-IgE mediated or mixed [1]. Infants with IgE-CMA may present from gastrointestinal (i.e., vomiting and diarrhea), cutaneous (i.e., erythema, urticarial and angioedema), respiratory and/or systemic symptoms up to the most severe reaction anaphylaxis, occurring within 2 h after cow’s milk exposure. Non-IgE-CMA is characterized by subacute or chronic gastrointestinal symptoms and affected infants may present bloody stools, delayed vomiting, crying and chronic diarrhea with the risk of malnutrition and failure to thrive [1]. The diagnosis of CMA requires a positive oral food challenge to cow’s milk protein; that is the gold standard test to confirm CMA [3,4]. The type and the severity of CMA symptoms dramatically worsened in the last years, as well the epidemiology picture showed an increase in CMA prevalence and persistence [5,6]. Several hypotheses have been postulated to explain the spread of CMA in the last years and the most likely one seems related to an impaired gene-environment interaction [6,7]. Some dietary habits (i.e., the Western diet), infections, cesarean delivery, formula consumption in the first week of life and the massive use of drugs in the first stage of life have been proposed as the main environmental factors responsible for the occurrence of FAs, including CMA [8,9,10]. Indeed, operating on an unfavorable genetic background, these factors impair the gut microbiome (GM), with consequent alterations of the GM-immune system axis. The perturbation of this axis could lead to a breakdown of immune tolerance and to CMA occurrence [9,10]. On the other hand, the Mediterranean diet, vaginal delivery and breastfeeding could positively modulate the axis and may represent an innovative approach to prevent and treat GM-immune system-derived diseases, such as CMA [9,10,11]. Among the environmental factors, diet represents one of the main modifiable ones. Since dietary habits have a role in eliciting potentially negative or positive effects in CMA occurrence, nutritional modulation could be considered an effective target for the prevention and management of CMA. The potential to influence the immune system functionality of selected dietary habits has been described with the term “immunonutrition” that, in the FA field, is based on a proactive approach focused on the prevention and the acquisition of immune tolerance in allergy treatment [12]. In this review we analyze the nutritional strategies from different points of view, covering different aspects of an effective approach to prevent or manage CMA.
2. Cow’s Milk Allergy Preventive Nutritional Strategies
The alarming increasing rate of CMA prevalence advocates the necessity for effective preventive nutritional strategies against the disease burden.
The CMA’s primary prevention should start from the prenatal period, focusing on a maternal healthy lifestyle and food diversity during pregnancy [13]. Maternal diet during pregnancy has been considered a potential target for allergy prevention. Maternal diet may affect, through direct or indirect mechanisms, infant GM, which is associated with a range of allergy outcomes [13,14,15]. High adherence to the Mediterranean diet has been reported to increase GM diversity [16]. Thus, a maternal diet rich in Mediterranean diet-based foods, including vegetables and yogurt, was associated with protective effects for offspring allergies [17]. On the contrary, dietary intake of Western heat-processed foods high in advanced glycation end products (e.g., fried foods, red and processed meat and fruit juice), has been associated with a reduced diversity of GM and the occurrence of pediatric allergies [2]. In addition, the maternal avoidance of allergenic solids foods during pregnancy and lactation have been considered ineffective for CMA prevention and no recommendation by international guidelines have been provided [8]. Indeed, the maternal intake of allergenic solids foods during pregnancy could ensure the placental transmission of inhibitory IgG- allergen immune complexes, reducing the risk of pediatric allergy occurrence [18,19]. Furthermore, no international recommendations for or against the use of prebiotics, probiotics or synbiotics during breastfeeding and lactation alone or in combination with other approaches to prevent pediatric allergies have been formulated [8].
Through a positive modulation of the GM and the proper development of the immune system during infancy, breastfeeding is the first nutritional postnatal factor able to protect against allergy occurrence [20]. Several protective mechanisms of breastfeeding have been proposed. Breast milk has anti-allergic immune properties and contains a large amount of biologically active compounds, including lysozyme, lactoferrin, immunoglobulins (Ig)A, IgM, cytokines, nucleotides, microRNAs and hormones that provide passive immunity and could induce oral tolerance to food antigens [21,22,23]. Among the most abundant protective component of breast milk, are the human milk oligosaccharides (HMOs) and prebiotics, resulting in the production of sub-products such as lactate and short-chain fatty acids (SCFAs) and metabolites, able to modulate the immune system function [24]. In particular, the SCFA butyrate enhances the suppressive capacity of regulatory T cells (Treg), suppressing the allergic response and sustaining immune tolerance to allergens in the offspring [25,26]. Butyrate in human milk modulates the mechanisms of immune tolerance, including the increase in biomarkers of gut barrier integrity and tolerogenic cytokines in concentrations able to protect against allergy occurrence [27]. Nevertheless, due to the low certainty of evidence, no recommendations for or against using breastfeeding to prevent food allergy or CMA have been provided at the European level [8]. Thus, considering the multiple benefits for infants and mothers, breastfeeding should be encouraged wherever possible, as stated by most scientific society guidelines [28]. Notably, guidelines from the European Academy of Allergy and Clinical Immunology (EAACI) recommend avoiding supplementation with cow’s milk formula in the first week of life. Other possible temporary supplementary options for breastfed infants could include donor breast milk, amino acid or hydrolyzed formula [8]. Regarding the introduction of complementary foods in infants’ diets for allergy prevention, the European guidelines recommend the importance of not avoiding the intake of potentially allergenic foods during weaning, emphasizing that there is no reason for delaying their introduction after 12 months nor for an early introduction <4 months [29]. Evidence supports the role of early exposure to potential allergens in the development of immune tolerance [30,31]; indeed, the regular ingestion of food allergens between 4 and 6 months of life can lead to immune tolerance and alter the immunological responses to food antigens; conversely, the skin passage of food antigens in the condition of inflammation, before the achievement of immune tolerance, can lead to sensitization to food allergens [32]. In addition, the infants’ diet, influencing the GM composition and function, could have a pivotal role in protecting against the occurrence of food allergy. Evidence has shown that a high diet diversity and the introduction in the first year of life of fruits, vegetables, yogurt and fish, through a fecal increase in the tolerogenic metabolite butyrate, is associated with protection against the development of allergies, even in later stages of life [33,34]. Figure 1 shows a summary of the protective and risk nutritional factors in CMA occurrence.
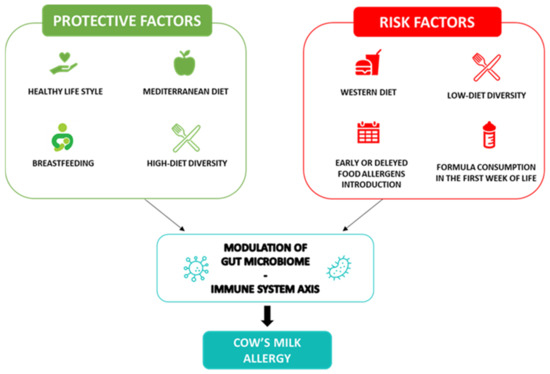
Figure 1.
Cow’s milk allergy protective and risk nutritional factors. Legend: The figure depicts the nutritional protective and risk factors in CMA.
3. Nutritional Strategies for the Management of Cow’s Milk Allergy
In pediatric patients with a confirmed CMA diagnosis, international guidelines recommend a strict cow’s milk protein elimination diet as the only therapeutic strategy to treat CMA. Obviously, the first aim of the elimination diet is to prevent an allergic reaction in CMA patients; but for specialists working in the FA field, avoiding nutritional deficit and ensuring optimal body growth are pivotal aspects that need to be considered [35,36,37,38]. In Table 1 are reported the nutritional intervention cornerstones in CMA pediatric patients. Nutritional counseling for CMA management should be based on the parental/patients’ education about accidental exposure prevention, cow’s milk restrictions, use of an alternative formula in non-breastfed CMA patients, supplementation of avoided nutrients and adequate follow-up.

Table 1.
Nutritional intervention cornerstones in CMA pediatric patients.
3.1. Accidental Exposures Prevention
Another cornerstone of nutritional counseling is educating patients and their parents/tutors to prevent accidental ingestion of the allergen. Since cow’s milk is used in many products such as cakes, pastry cream, chocolate, candies, etc., and it represents the main food of child nutrition, especially in the first years of life, its elimination from the diet could be even more difficult [39]. For this reason, accidental exposures could be common and should be prevented. Parents/patients need to be educated regarding:
- (1)
- Contamination: They should be careful about the contact or contamination of foods with cow’s milk protein, especially in places such as bakeries and restaurants, laying out side-by-side of these foods or using the same knife while cutting or using the same fork while serving increases the risk of contamination;
- (2)
- Food labels: All ingredient labels on food packages should be read carefully. Foods containing casein, whey, lactalbumin, albumin, etc. should be avoided [40]. There is no consensus yet on the restriction of foods containing advisory labeling such as “may contain milk” because the allergic risks of these products are not yet fully known and the amount of cow’s milk protein contamination of them are variable [41];
- (3)
- Cross reactions: Due to the high cross-reactivity with cow’s milk protein of sheep, goats, buffalo, ibex, deer, donkey, camel and horse milk, parents should be aware of cross-reactions that may occur and should strictly avoid the consumption of these alternative milks;
- (4)
- Non-food products: Drugs, cosmetics and supplements may contain cow’s milk. The labels of these products should also be read carefully.
3.2. Cow’s Milk Protein Elimination Diet
The CMA treatment is based on the exclusion from the diet of cow’s milk and milk derivatives (dairy products). In breast-fed CMA patients, lactating mothers should be encouraged to continue breastfeeding following a cow’s milk protein-free diet. Appropriate nutritional counseling to completely exclude milk and hidden sources of cow’s milk protein from lactating women’s diets and to ensure their nutritional needs (including calcium and vitamin D supplementation) should be performed [42]. In cases where breast milk is not possible and till the second year of age, formula based on cow’s milk and milk from other mammals (e.g., goat’s milk, sheep’s milk, etc.) should be strictly avoided and a hypoallergenic formula should be chosen [42]. In non-breastfed infants, an extensively hydrolyzed formula (eHF) of casein or whey proteins should be the first choice [43]. The use of an amino acid-based formula (AAF) is recommended in patients with severe CMA symptoms or in patients that have no improvement within 2 weeks of using eHF [42]. Formula based on soy protein could be chosen after the establishment of tolerance to soy protein for infants >6 months who do not tolerate the eHF taste or for its more affordability; formula based on rice protein that is partially or extensively hydrolyzed may be considered in infants who refuse or do not tolerate eHF or in vegan families [43].
Since cow’s milk and its derivatives are not only a major source of proteins and fats but also of micronutrients, such as calcium, zinc, riboflavin, magnesium, phosphorus, pantothenic acid, vitamin B12 and vitamin D, a cow’s milk elimination diet without proper substitution of its components could represent a risk for nutritional status of CMA patients [44]. These macros/micronutrients are crucial for infant development and an inadequate elimination diet could lead to serious consequences, including poor growth and malnutrition [45]. Thus, to avoid the high risk of nutritional deficits for CMA patients following an elimination diet, any nutrient supplementation should be considered during nutritional counseling. In particular, calcium supplementation should be performed for mothers of breast-fed CMA patients (e.g., 1000 mg/day), and should be evaluated for children after the introduction of solid foods when milk consumption progressively decreases. Calcium supplementation should be considered for the entire duration of the exclusion diet of non-breastfed infants considering the amount and the composition of the hypoallergenic formula consumed [42]. The vitamin D supplementation should be performed in all patients during the first year of life and should be considered if continuing the administration throughout the entire period of the exclusion diet [46]. In addition to calcium and vitamin D, cow’s milk is an ideal vehicle for the introduction of ω-3-polyunsaturated fatty acids (PUFAs), exerting several beneficial immune-modulatory effects [47]. Low ω-3 PUFA levels in plasma have been reported in CMA pediatric patients [48,49,50]. Their supplementation should be evaluated in CMA patients, also considering the ω-3 PUFAs plasma profile.
The monitoring of a CMA patient’s nutrient intake is of pivotal importance during nutritional counseling to prevent or correct nutritional status alterations. Body growth is determined by genetic factors, and everyone generally follows a certain growth curve if conditions are favorable [51]. Among these factors, diet plays a key role: an adequate diet, in terms of quantity and quality, providing the necessary substrates, can exert an appropriate stimulus to growth [52]. Unfortunately, data on CMA patients’ body growth are conflicting [49,53], paving the way for the hypothesis that alterations of weight and/or length indexes may not only depend on an inadequate elimination diet but also from other causes. In several studies, it has been reported that children with CMA are often at risk of metabolic bone disorders, leading to pathologic conditions such as ricket or osteopenia [54], characterized by a reduction in body bone mineral content, bone mineral density for age, delay of bone age and reduced height for age index [55]. Bone is a mineralized connective tissue in which calcium represents the major component [56] and phosphorus (P) is as a percentage the second mineral component of bone tissue [57]. During the growth period, an adequate intake of calcium is required to maintain a positive calcium balance [58], essential for the development of bones [59] and for optimizing bone mass accretion. The appropriate levels of calcium and phosphorus are crucial for the activity of osteoblasts and osteocytes in the process of matrix mineralization [57]. Patients affected by CMA also showed lower vitamin D concentrations [60]. Vitamin D is known for its role in calcium [61] and phosphorus [62] homeostasis and for optimal skeletal health because it acts as a prohormone essential for the normal absorption of calcium and phosphorus from the gut [63]. With an adequate vitamin D state, intestinal calcium absorption increases from 30% to 40% but without it, the body absorbs no more than 10–15% of the dietary calcium [64]. A deficiency of vitamin D and/or calcium has been observed to lead to a defect in the growth plates and osteoid mineralization, resulting in reduced differentiation of chondrocytes and apoptosis in the growth plate and a consequent increase in osteoid tissue, leading to the appearance of clinical and radiological features of rickets [65]. Chondrocytes both contain the vitamin D receptor (at least in hypertrophic but nonproliferating chondrocytes) and can produce 1,25(OH)2D [66]. Vitamin D is directly involved in endochondral ossification [66]. The process of endochondral ossification affects height. Endochondral ossification occurs within the cartilaginous sketch, where chondrocytes multiply and degenerate; these are later replaced by osteoblasts, which produce bone substance, remain enclosed, and turn into osteocytes. The progression of endochondral ossification and linear growth is regulated by the influence of endocrine/paracrine/autocrine signals and zinc, which mediate a cascade of signals through different pathways [67]. Zinc also has a very important role within the growth cartilage since up to 10% of human genes encode proteins with zinc-binding domains [68]. Several randomized studies have examined the effect of zinc supplementation on child growth, and some of these have concluded that zinc supplementation has a positive effect on children’s growth [69,70,71,72,73], while others have not reported effects [74,75]. Differences obtained may concern variability in study settings, period of supplementation (maternal or infancy/childhood), inclusion or exclusion criteria, dose, duration or type of zinc, presence of iron supplementation or types of results evaluated. Furthermore, another issue for nutritional deficiencies in CMA patients may be because the disease is accompanied by an aberrant inflammatory process that can affect serum concentrations of micronutrients [76]. Inflammation inhibits endochondral ossification through the action of mediators, including proinflammatory cytokines [77]. Major proinflammatory cytokines known to inhibit endochondral ossification include TNF-α, IL-1 (particularly IL-1β), and IL-6 [78]. High concentrations of these cytokines suppress growth by decreasing chondrocyte proliferation while increasing apoptosis [79]. TNF-α is produced endogenously throughout the growth cartilage and can inhibit chondrocyte proliferation, especially in combination with IL-1β [80]. IL-1β induces rapid dedifferentiation of cultured chondrocytes [81] and acts synergistically with TNF-α to inhibit longitudinal bone growth of cultured rats [82].
3.3. Proposal of the Most Complete Compounds Supplement for Nutrients Deficiencies Prevention and to Positively Drive the Disease Course in CMA Pediatric Patients
Interventions are required to avoid the harmful consequences of nutritional deficiencies, including nutrition education, fortification and supplementation [83]. An elimination diet does not necessarily affect the growth of children if their diet is adequately supplemented. This underscores the importance of an adequate supplementation of deficient nutrients during the dietary management in CMA children, and in general of FA children [84]. Several nutrient supplements available on the market are selective only for some types of nutrients and are deficient in others. For this reason, based on emerging data in the CMA field, with this review, we would like to propose the most complete nutrient supplements for children affected by CMA for preventing and treating nutritional status alterations and nutritional deficiencies. We propose a complete list of trace elements, vitamins, minerals and essential fatty acids, which are necessary for the well-being of the child, and which are mostly deficient in children affected by CMA. In addition to the nutrients mentioned above, we would like to add to the list specific probiotics, prebiotics and postbiotics which have an important role in children’s health and CMA disease course [85]. Emerging data suggest that GM manipulation with the use of pro-, pre- and postbiotics may have a role in the prevention or treatment of FAs, such as CMA [86,87]. Several studies have examined the effects of probiotic supplementation in CMA treatment. Our group has previously shown that the supplementation with the probiotic Lactobacillus rhamnosus GG (LGG) of an extensively hydrolyzed casein formula (EHCF) induced higher tolerance rates to milk in CMA pediatric patients compared with EHCF alone and other formulas [88]. Indeed, the LGG is a butyrate producer, which might modulate the expression of genes involved in the allergic pathway, improving the tolerance to cow’s milk proteins [89]. An additional approach to positively modulate the GM is based on the use of prebiotics [85], such as HMOs, fructooligosaccharides (FOSs), galactooligosaccharides (GOSs) and inulin. HMOs provide health benefits in terms of microbiota composition, modulation of gut epithelial cell responses, and provide immunomodulatory and anti-inflammatory effects [90]. Moreover, HMOs can indirectly increase the production of SCFAs [91], which may improve the main immune defensive functions of the intestinal epithelium [92]. FOSs, GOSs and inulin, through a positive modulation of the GM composition and activity, could elicit beneficial effects on immune system function [93,94]. Furthermore, for the tolerogenic properties of the SCFA butyrate, this postbiotic could be useful for its beneficial effects on the GM-immune system axis [25,26,27].
Other compounds with potential beneficial effects in CMA patients could be quercetin, a flavonoid with several pharmacological properties, including anti-inflammatory and immunomodulatory properties [95], curcumin, which could alleviate allergic symptoms [96], and finally berberine and limonin, bioactive compounds which may suppress the IgE production by human B cells and peripheral blood mononuclear cells, as shown in allergic patients [97].
Starting from this evidence, in Table 2 are listed the compounds that could be necessary for the prevention of nutritional status alterations/deficiencies in CMA pediatric patients and improve the disease course of milk allergies. Obviously, the compounds’ dosage in the supplement will respect the recommended levels of national guidelines and dietary reference values (DRVs) for age [98]. For the compounds, such as probiotics, prebiotics and others, further evidence is needed to establish the recommended amounts to be included in our supplement.

Table 2.
Proposal of the most complete compounds supplement for nutrients deficiencies prevention and to positively drive the disease course in CMA pediatric patients.
3.4. Follow-Up of CMA Patients
The anthropometric parameters assessment represents the most important step of nutritional follow-up since body growth is a sensitive indicator of an adequate nutritional status and optimal intake of energy and nutrients. Weight, length/height and head circumference should be measured, and the values should be reported on the reference growth curves [99]. The nutritional follow-up through the evaluation of body growth parameters and relative percentiles/z-scores should be performed at 1, 2 and 4 months in the first semester of life and every 3 months in the second semester. After the first year, the anthropometric measurements should be performed every 6–12 months. The nutritional intake assessment should be performed at least once a year in CMA patients with normal growth or two or more times per year when patients present an alteration in the body growth pattern [46]. Nutritional status alterations of infants and children are classified by the World Health Organization (WHO) as shown in Table 3. In these cases, a personalized nutritional intervention properly planned and monitored has proven to be an effective strategy to correct body growth alterations [46].

Table 3.
Classification of nutritional status alterations of infants and children according to WHO.
Regarding CMA recovery, several studies indicate that ~80% of CMA patients achieve oral tolerance to milk within 3 to 4 years but this generally depends on different factors that could predict the CMA duration (e.g., the occurrence of other atopic manifestations, such as asthma, rhinitis and eczema and other skin and/or gastrointestinal symptoms) [43] and the CMA-symptoms severity at the diagnosis is associated with worse prognosis for the duration of allergy [100]. Thus, a periodical re-evaluation of tolerance to cow’s milk through oral food challenges according to the guidelines and based on the immunologic mechanism (IgE/non-IgE) is mandatory to prevent CMA patients from continuing unnecessary elimination diets [43]. Surprisingly, more than half of children with CMA may tolerate processed-extensively heated/baked forms of cow’s milk [101]. An oral food challenge with baked milk is the only way to evaluate this tolerance, and it has been shown that patients who tolerate baked milk have a better prognosis of CMA and are more likely prone to tolerate lightly processed forms of cow’s milk in the future [102]. After introducing food products with well-cooked cow’s milk associated with a matrix (e.g., a muffin), it could be useful to stimulate the immune tolerance to milk through the consumption of less heated cow’s milk food products till the uncooked milk, following the “milk ladder” approach [103]. Another approach to induce oral tolerance to milk could be achievable using oral immunotherapy (OIT). This strategy provides the administration of increasing quantities of milk until achieving tolerance. Unfortunately, the OIT procedures should be better standardized, and its efficacy requires further studies [104].
4. Conclusions
The prevalence and severity of pediatric CMA have increased dramatically in the last decades under the pressure of environmental factors in genetically predisposed individuals. Among environmental factors, nutrition plays a pivotal role. Diet is one of the most relevant modifiable factors, representing a potential target for the prevention and treatment of CMA. Indeed, the immune system development and function could be modulated by immunonutrition strategies. This narrative review provided an overview of the most scientific-based nutritional strategies for the prevention and management of pediatric CMA.
Author Contributions
S.C., L.C., F.O., C.D.S., G.O. and R.B.C. analyzed the literature and wrote and read the manuscript. All authors have substantially contributed to the development, conception, and design of the present review and those listed have made a direct and intellectual contribution to the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
Funder: Project funded under the National Recovery and Resilience Plan (NRRP), Mission 4 Component 2 Investment 1.3—Call for tender No. 341 of 15 March 2022 of Italian Ministry of University and Research funded by the European Union—NextGenerationEU; Award Number: Project code PE00000003, Concession Decree No. 1550 of 11 October 2022 adopted by the Italian Ministry of University and Research, CUP D93C22000890001, Project title “ON Foods—Research and innovation network on food and nutrition Sustainability, Safety and Security—Working ON Foods”.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Jensen, S.A.; Fiocchi, A.; Baars, T.; Jordakieva, G.; Nowak-Wegrzyn, A.; Pali-Schöll, I.; Passanisi, S.; Pranger, C.L.; Roth-Walter, F.; Takkinen, K.; et al. Diagnosis and Rationale for Action against Cow’s Milk Allergy (DRACMA) Guidelines up-date—III—Cow’s milk allergens and mechanisms triggering immune activation. World Allergy Organ. J. 2022, 15, 100668. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.K.; Masilamani, M.; Li, X.M.; Sampson, H.A. The false alarm hypothesis: Food allergy is associated with high dietary advanced glycation end-products and proglycating dietary sugars that mimic alarmins. J. Allergy Clin. Immunol. 2017, 139, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Bird, J.A.; Leonard, S.; Groetch, M.; Assa’ad, A.; Cianferoni, A.; Clark, A.; Crain, M.; Fausnight, T.; Fleischer, D.; Green, T.; et al. Conducting an Oral Food Challenge: An Update to the 2009 Adverse Reactions to Foods Committee Work Group Report. J. Allergy Clin. Immunol. Pract. 2020, 8, 75–90.e17. [Google Scholar] [CrossRef] [PubMed]
- Muraro, A.; Werfel, T.; Hoffmann-Sommergruber, K.; Roberts, G.; Beyer, K.; Bindslev-Jensen, C.; Cardona, V.; Dubois, A.; duToit, G.; Eigenmann, P.; et al. EAACI food allergy and anaphylaxis guidelines: Diagnosis and management of food allergy. Allergy 2014, 69, 1008–1025. [Google Scholar] [CrossRef] [PubMed]
- Nocerino, R.; Leone, L.; Cosenza, L.; Berni Canani, R. Increasing rate of hospitalizations for food-induced anaphylaxis in Italian children: An analysis of the Italian ministry of health database. J. Allergy Clin. Immunol. 2015, 135, 833–835.e3. [Google Scholar] [CrossRef]
- Flom, J.D.; Sicherer, S.H. Epidemiology of cow’s milk. Allergy Nutr. 2019, 11, 1051. [Google Scholar]
- Neeland, M.R.; Martino, D.J.; Allen, K.J. The role of gene-environment interactions in the development of food allergy. Expert Rev. Gastroenterol. Hepatol. 2015, 9, 1371–1378. [Google Scholar] [CrossRef]
- Halken, S.; Muraro, A.; de Silva, D.; Khaleva, E.; Angier, E.; Arasi, S.; Arshad, H.; Bahnson, H.T.; Beyer, K.; Boyle, R.; et al. EAACI guideline: Preventing the development of food allergy in infants and young children (2020 update). Pediatr. Allergy Immunol. 2021, 32, 843–858. [Google Scholar] [CrossRef]
- Aitoro, R.; Paparo, L.; Amoroso, A.; Di Costanzo, M.; Cosenza, L.; Granata, V.; Di Scala, C.; Nocerino, R.; Trinchese, G.; Montella, M.; et al. Gut Microbiota as a Target for Preventive and Therapeutic Intervention against Food Allergy. Nutrients 2017, 9, 672. [Google Scholar] [CrossRef]
- Devonshire, A.; Gautam, Y.; Johansson, E.; Mersha, T.B. Multi-omics profiling approach in food allergy. World Allergy Organ. J. 2023, 16, 100777. [Google Scholar] [CrossRef]
- Lee, K.H.; Song, Y.; Wu, W.; Yu, K.; Zhang, G. The gut microbiota, environmental factors, and links to the development of food allergy. Clin. Mol. Allergy 2020, 18, 5. [Google Scholar] [CrossRef]
- Carucci, L.; Coppola, S.; Luzzetti, A.; Voto, L.; Giglio, V.; Paparo, L.; Nocerino, R.; Berni Canani, R. Immunonutrition for Pediatric Patients with Cow’s Milk Allergy: How Early Interventions Could Impact Long-Term Outcomes. Front. Allergy 2021, 2, 676200. [Google Scholar] [CrossRef]
- Venter, C.; Agostoni, C.; Arshad, S.H.; Ben-Abdallah, M.; Du Toit, G.; Fleischer, D.M.; Greenhawt, M.; Glueck, D.H.; Groetch, M.; Lunjani, N.; et al. Dietary factors during pregnancy and atopic outcomes in childhood: A systematic review from the European Academy of Allergy and Clinical Immunology. Pediatr. Allergy Immunol. 2020, 31, 889–912. [Google Scholar] [CrossRef]
- Selma-Royo, M.; García-Mantrana, I.; Calatayud, M.; Parra-Llorca, A.; Martínez-Costa, C.; Collado, M.C. Maternal diet during pregnancy and intestinal markers are associated with early gut microbiota. Eur. J. Nutr. 2021, 60, 1429–1442. [Google Scholar] [CrossRef]
- García-Mantrana, I.; Selma-Royo, M.; González, S.; Parra-Llorca, A.; Martínez-Costa, C.; Collado, M.C. Distinct maternal microbiota clusters are associated with diet during pregnancy: Impact on neonatal microbiota and infant growth during the first 18 months of life. Gut Microbes 2020, 11, 962–978. [Google Scholar] [CrossRef]
- De Filippis, F.; Pellegrini, N.; Vannini, L.; Jeffery, I.B.; La Storia, A.; Laghi, L.; Serrazanetti, D.I.; Di Cagno, R.; Ferrocino, I.; Lazzi, C.; et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut 2016, 65, 1812–1821. [Google Scholar] [CrossRef]
- Venter, C.; Palumbo, M.P.; Glueck, D.H.; Sauder, K.A.; O’Mahony, L.; Fleischer, D.M.; Ben-Abdallah, M.; Ringham, B.M.; Dabelea, D. The maternal diet index in pregnancy is associated with offspring allergic diseases: The Healthy Start study. Allergy 2022, 77, 162–172. [Google Scholar] [CrossRef]
- Bunyavanich, S.; Rifas-Shiman, S.L.; Platts-Mills, T.A.; Workman, L.; Sordillo, J.E.; Camargo, C.A., Jr.; Gillman, M.W.; Gold, D.R.; Litonjua, A.A. Peanut, milk, and wheat intake during pregnancy is associated with reduced allergy and asthma in children. J. Allergy Clin. Immunol. 2014, 133, 1373–1382. [Google Scholar] [CrossRef]
- Uthoff, H.; Spenner, A.; Reckelkamm, W.; Ahrens, B.; Wölk, G.; Hackler, R.; Hardung, F.; Schaefer, J.; Scheffold, A.; Renz, H.; et al. Critical role of preconceptional immunization for protective and nonpathological specific immunity in murine neonates. J. Immunol. 2003, 171, 3485–3492. [Google Scholar] [CrossRef]
- Järvinen, K.M.; Martin, H.; Oyoshi, M.K. Immunomodulatory effects of breast milk on food allergy. Ann. Allergy Asthma Immunol. 2019, 123, 133–143. [Google Scholar] [CrossRef]
- Yeruva, L.; Munblit, D.; Collado, M.C. Editorial: Impact of Early Life Nutrition on Immune System Development and Related Health Outcomes in Later Life. Front. Immunol. 2021, 25, 668569. [Google Scholar] [CrossRef] [PubMed]
- Adel-Patient, K.; Bernard, H.; Fenaille, F.; Hazebrouck, S.; Junot, C.; Verhasselt, V. Prevention of Allergy to a Major Cow’s Milk Allergen by Breastfeeding in Mice Depends on Maternal Immune Status and Oral Exposure During Lactation. Front. Immunol. 2020, 21, 1545. [Google Scholar] [CrossRef] [PubMed]
- Ohsaki, A.; Venturelli, N.; Buccigrosso, T.M.; Osganian, S.K.; Lee, J.; Blumberg, R.S.; Oyoshi, M.K. Maternal IgG immune complexes induce food allergen-specific tolerance in offspring. J. Exp. Med. 2018, 215, 91–113. [Google Scholar] [CrossRef] [PubMed]
- Plaza-Díaz, J.; Fontana, L.; Gil, A. Human Milk Oligosaccharides and Immune System Development. Nutrients 2018, 10, 1038. [Google Scholar] [CrossRef] [PubMed]
- Vonk, M.M.; Blokhuis, B.R.J.; Diks, M.A.P.; Wagenaar, L.; Smit, J.J.; Pieters, R.H.H.; Garssen, J.; Knippels, L.M.J.; van Esch, B.C.A.M. Butyrate Enhances Desensitization Induced by Oral Immunotherapy in Cow’s Milk Allergic Mice. Mediat. Inflamm. 2019, 16, 9062537. [Google Scholar] [CrossRef]
- Folkerts, J.; Redegeld, F.; Folkerts, G.; Blokhuis, B.; van den Berg, M.P.M.; de Bruijn, M.J.W.; van IJcken, W.F.J.; Junt, T.; Tam, S.Y.; Galli, S.J.; et al. Butyrate inhibits human mast cell activation via epigenetic regulation of FcεRI-mediated signaling. Allergy 2020, 75, 1966–1978. [Google Scholar] [CrossRef]
- Paparo, L.; Nocerino, R.; Ciaglia, E.; Di Scala, C.; De Caro, C.; Russo, R.; Trinchese, G.; Aitoro, R.; Amoroso, A.; Bruno, C.; et al. Butyrate as a bioactive human milk protective component against food allergy. Allergy 2021, 76, 1398–1415. [Google Scholar] [CrossRef]
- WHO. Maternal, Infant and Young Child Nutrition. Available online: https://apps.who.int/iris/handle/10665/250636 (accessed on 26 June 2023).
- Muraro, A.; Halken, S.; Arshad, S.H.; Beyer, K.; Dubois, A.E.; Du Toit, G.; Eigenmann, P.A.; Grimshaw, K.E.; Hoest, A.; Lack, G.; et al. EAACI food allergy and anaphylaxis guidelines. Primary prevention of food allergy. Allergy 2014, 69, 590–601. [Google Scholar] [CrossRef]
- Du Toit, G.; Roberts, G.; Sayre, P.H.; Bahnson, H.T.; Radulovic, S.; Santos, A.F.; Brough, H.A.; Phippard, D.; Basting, M.; Feeney, M.; et al. LEAP Study Team. Randomized trial of peanut consumption in infants at risk for peanut allergy. N. Engl. J. Med. 2015, 372, 803–813. [Google Scholar] [CrossRef]
- Du Toit, G.; Roberts, G.; Sayre, P.H.; Plaut, M.; Bahnson, H.T.; Mitchell, H.; Radulovic, S.; Chan, S.; Fox, A.; Turcanu, V.; et al. Identifying infants at high risk of peanut allergy: The Learning Early About Peanut Allergy (LEAP) screening study. J. Allergy Clin. Immunol. 2013, 131, 135–143.e12. [Google Scholar] [CrossRef]
- Lack, G. Update on risk factors for food allergy. J. Allergy Clin. Immunol. 2012, 129, 1187–1197. [Google Scholar] [CrossRef]
- Roduit, C.; Frei, R.; Depner, M.; Schaub, B.; Loss, G.; Genuneit, J.; Pfefferle, P.; Hyvärinen, A.; Karvonen, A.M.; Riedler, J.; et al. Increased food diversity in the first year of life is inversely associated with allergic diseases. J. Allergy Clin. Immunol. 2014, 133, 1056–1064. [Google Scholar] [CrossRef]
- Roduit, C.; Frei, R.; Ferstl, R.; Loeliger, S.; Westermann, P.; Rhyner, C.; Schiavi, E.; Barcik, W.; Rodriguez-Perez, N.; Wawrzyniak, M.; et al. High levels of butyrate and propionate in early life are associated with protection against atopy. Allergy 2019, 74, 799–809. [Google Scholar] [CrossRef]
- Muraro, A.; de Silva, D.; Halken, S.; Worm, M.; Khaleva, E.; Arasi, S.; Dunn-Galvin, A.; Nwaru, B.I.; De Jong, N.W.; Rodríguez Del Río, P.; et al. Managing food allergy: GA2LEN guideline 2022. World Allergy Organ. J. 2022, 15, 100687. [Google Scholar] [CrossRef]
- Luyt, D.; Ball, H.; Makwana, N.; Green, M.R.; Bravin, K.; Nasser, S.M.; Clark, A.T.; Standards of Care Committee (SOCC) of the British Society for Allergy and Clinical Immunology (BSACI). BSACI guideline for the diagnosis and management of cow’s milk allergy. Clin. Exp. Allergy 2014, 44, 642–672. [Google Scholar] [CrossRef]
- Wright, K.; Feeney, M.; Yerlett, N.; Meyer, R. Nutritional Management of Children with Food Allergies. Curr. Treat. Options Allergy 2022, 9, 375–393. [Google Scholar] [CrossRef]
- Stróżyk, A.; Ruszczyński, M.; Horvath, A.; Dahdah, L.; Fiocchi, A.; Nowak-Węgrzyn, A.; Shamir, R.; Spergel, J.; Vandenplas, Y.; Venter, C.; et al. World Allergy Organization (WAO) Diagnosis and Rationale for Action against Cow’s Milk Allergy (DRACMA) Guidelines update—IV—A quality appraisal with the AGREE II instrument. World Allergy Organ. J. 2022, 15, 100613. [Google Scholar] [CrossRef]
- Fiocchi, A.; Schünemann, H.J.; Brozek, J.; Restani, P.; Beyer, K.; Troncone, R.; Martelli, A.; Terracciano, L.; Bahna, S.L.; Rancé, F.; et al. Diagnosis and Rationale for Action Against Cow’s Milk Allergy (DRACMA): A summary report. J. Allergy Clin. Immunol. 2010, 126, 1119–1128.e12. [Google Scholar] [CrossRef]
- Dupont, C.; Chouraqui, J.P.; de Boissieu, D.; Bocquet, A.; Bresson, J.L.; Briend, A.; Darmaun, D.; Frelut, M.L.; Ghisolfi, J.; Girardet, J.P.; et al. Dietary treatment of cows’ milk protein allergy in childhood: A commentary by the Committee on Nutrition of the French Society of Paediatrics. Br. J. Nutr. 2012, 107, 325–338. [Google Scholar] [CrossRef]
- Crotty, M.P.; Taylor, S.L. Risks associated with foods having advisory milk labeling. J. Allergy Clin. Immunol. 2010, 125, 935–937. [Google Scholar] [CrossRef]
- Koletzko, S.; Niggemann, B.; Arato, A.; Dias, J.A.; Heuschkel, R.; Husby, S.; Mearin, M.L.; Papadopoulou, A.; Ruemmele, F.M.; Staiano, A.; et al. Diagnostic approach and management of cow’s-milk protein allergy in infants and children: ESPGHAN GI Committee practical guidelines. J. Pediatr. Gastroenterol. Nutr. 2012, 55, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Fiocchi, A.; Brozek, J.; Schünemann, H.; Bahna, S.L.; von Berg, A.; Beyer, K.; Bozzola, M.; Bradsher, J.; Compalati, E.; Ebisawa, M.; et al. World Allergy Organization (WAO) Diagnosis and Rationale for Action against Cow’s Milk Allergy (DRACMA) Guidelines. Pediatr. Allergy Immunol. 2010, 21, 1–125. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kwon, J.; Noh, G.; Lee, S.S. The effects of elimination diet on nutritional status in subjects with atopic dermatitis. Nutr. Res. Pract. 2013, 7, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Mehta, H.; Groetch, M.; Wang, J. Growth and nutritional concerns in children with food allergy. Curr. Opin. Allergy Clin. Immunol. 2013, 13, 275–279. [Google Scholar] [CrossRef]
- Giovannini, M.; D’Auria, E.; Caffarelli, C.; Verduci, E.; Barberi, S.; Indinnimeo, L.; Iacono, I.D.; Martelli, A.; Riva, E.; Bernardini, R. Nutritional management and follow up of infants and children with food allergy: Italian Society of Pediatric Nutrition/Italian Society of Pediatric Allergy and Immunology Task Force Position Statement. Ital. J. Pediatr. 2014, 40, 1. [Google Scholar] [CrossRef]
- Hebeisen, D.F.; Hoeflin, F.; Reusch, H.P.; Junker, E.; Lauterburg, B.H. Increased concentrations of omega-3 fatty acids in milk and platelet rich plasma of grass-fed cows. Int. J. Vitam. Nutr. Res. 1993, 63, 229–233. [Google Scholar]
- Aldámiz-Echevarría, L.; Bilbao, A.; Andrade, F.; Elorz, J.; Prieto, J.A.; Rodríguez-Soriano, J. Fatty acid deficiency profile in children with food allergy managed with elimination diets. Acta Paediatr. 2008, 97, 1572–1576. [Google Scholar] [CrossRef]
- Isolauri, E.; Sutas, Y.; Salo, M.K.; Isosomppi, R.; Kaila, M. Elimination diet in cow’s milk Allergy: Risk of impaired growth in young children. J. Pediatr. 1998, 132, 1004–1009. [Google Scholar] [CrossRef]
- Christie, L.; Hine, R.J.; Parker, J.G.; Burks, W. Food allergies in children affect nutrient intake and growth. J. Am. Diet. Assoc. 2002, 102, 1648–1651. [Google Scholar] [CrossRef]
- Tanner, J.M. A concise history of growth studies from Buffon to Boas. In Human Growth: A Comprehensive Treatise, In Neurobiology and Nutrition; Faulkner, F., Tanner, J.M., Eds.; Plenum: New York, NY, USA, 1979; Volume 3, pp. 515–593. [Google Scholar]
- Millward, D.J.; Rivers, J.P. The need for indispensable amino acids: The concept of the anabolic drive. Diabetes Metab. Rev. 1989, 5, 191–211. [Google Scholar] [CrossRef]
- Vandenplas, Y.; Dupont, C.; Eigenmann, P.; Heine, R.G.; Høst, A.; Järvi, A.; Kuitunen, M.; Mukherjee, R.; Ribes-Koninckx, C.; Szajewska, H.; et al. Growth in Infants with Cow’s Milk Protein Allergy Fed an Amino Acid-Based Formula. Pediatr. Gastroenterol. Hepatol. Nutr. 2021, 24, 392–402. [Google Scholar] [CrossRef]
- Doulgeraki, A.E.; Manousakis, E.M.; Papadopoulos, N.G. Bone health assessment of food allergic children on restrictive diets: A practical guide. J. Pediatr. Endocrinol. Metab. 2017, 30, 133–139. [Google Scholar] [CrossRef]
- Jensen, V.B.; Jorgensen, I.M.; Rasmussen, K.B.; Molgaard, C.; Prahl, P. Bone mineral status in children with cow’s milk allergy. Pediatr. Allergy Immunol. 2004, 15, 562–565. [Google Scholar] [CrossRef]
- Vannucci, L.; Fossi, C.; Quattrini, S.; Guasti, L.; Pampaloni, B.; Gronchi, G.; Giusti, F.; Romagnoli, C.; Cianferotti, L.; Marcucci, G.; et al. Calcium Intake in Bone Health: A Focus on Calcium-Rich Mineral Waters. Nutrients 2018, 10, 1930. [Google Scholar] [CrossRef]
- Ciosek, Ż.; Kot, K.; Kosik-Bogacka, D.; Łanocha-Arendarczyk, N.; Rotter, I. The Effects of Calcium, Magnesium, Phosphorus, Fluoride, and Lead on Bone Tissue. Biomolecules 2021, 11, 506. [Google Scholar] [CrossRef]
- Mailhot, G.; Perrone, V.; Alos, N.; Dubois, J.; Delvin, E.; Paradis, L.; Des Roches, A. Cow’s Milk Allergy and Bone Mineral Density in Prepubertal Children. Pediatrics 2016, 137, e20151742. [Google Scholar] [CrossRef]
- Çelik, M.N.; Köksal, E. Nutritional Targets in Cow’s Milk Protein Allergy: A Comprehensive Review. Curr. Nutr. Rep. 2022, 11, 329–336. [Google Scholar] [CrossRef]
- Pereira, A.P.D.S.; Mendonça, R.B.; Fonseca, F.L.A.; Mallozi, M.C.; Sarni, R.O.S. Vitamin D deficiency in children and adolescents with food allergy: Association with number of allergens, sun exposure and nutritional status. Allergol. Immunopathol. 2022, 50, 10–16. [Google Scholar] [CrossRef]
- Khazai, N.; Judd, S.E.; Tangpricha, V. Calcium and vitamin D: Skeletal and extraskeletal health. Curr. Rheumatol. Rep. 2008, 10, 110–117. [Google Scholar] [CrossRef]
- Bergwitz, C.; Jüppner, H. Regulation of Phosphate Homeostasis by PTH, Vitamin D, and FGF23. Annu. Rev. Med. 2010, 61, 91–104. [Google Scholar] [CrossRef]
- Sahay, M.; Sahay, R. Rickets-vitamin D deficiency and dependency. Indian J. Endocrinol. Metab. 2012, 16, 164–176. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Vitamin D deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef]
- Saggese, G.; Vierucci, F.; Prodam, F.; Cardinale, F.; Cetin, I.; Chiappini, E.; De’ Angelis, G.L.; Massari, M.; Miraglia Del Giudice, E.; Miraglia Del Giudice, M.; et al. Vitamin D in pediatric age: Consensus of the Italian pediatric society and the Italian society of preventive and social pediatrics, jointly with the Italian federation of pediatricians. Ital. J. Pediatr. 2018, 44, 51. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhu, J.; DeLuca, H.F. Identification of the vitamin D receptor in osteoblasts and chondrocytes but not osteoclasts in mouse bone. J. Bone Miner. Res. 2014, 29, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Lui, J.C.; Nilsson, O.; Baron, J. Recent insights into the regulation of the growth plate. J. Mol. Endocrinol. 2014, 53, T1–T9. [Google Scholar] [CrossRef]
- Cousins, R.J.; Liuzzi, J.P.; Lichten, L.A. Mammalian zinc transport, trafficking, and signals. J. Biol. Chem. 2006, 281, 24085–24089. [Google Scholar] [CrossRef]
- Brown, K.H.; Peerson, J.M.; Baker, S.K.; Hess, S.Y. Preventive zinc supplementation among infants, preschoolers, and older prepubertal children. Food Nutr. Bull. 2009, 30, S12–S40. [Google Scholar] [CrossRef]
- Brown, K.H.; Peerson, J.M.; Rivera, J.; Allen, L.H. Effect of supplemental zinc on the growth and serum zinc concentrations of prepubertal children: A meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2002, 75, 1062–1071. [Google Scholar] [CrossRef]
- Imdad, A.; Bhutta, Z.A. Effect of preventive zinc supplementation on linear growth in children under 5 years of age in developing countries: A meta-analysis of studies for input to the lives saved tool. BMC Public Health 2011, 11, S22. [Google Scholar] [CrossRef]
- Mayo-Wilson, E.; Junior, J.A.; Imdad, A.; Dean, S.; Chan, X.H.; Chan, E.S.; Jaswal, A.; Bhutta, Z.A. Zinc supplementation for preventing mortality, morbidity, and growth failure in children aged 6 months to 12 years of age. Cochrane Database Syst. Rev. 2014, 15, CD009384. [Google Scholar] [CrossRef]
- Dean, S.; Bhutta, Z.A. Preventive zinc supplementation for children, and the effect of additional iron: A systematic review and meta-analysis. BMJ Open 2014, 4, e004647. [Google Scholar]
- Ramakrishnan, U.; Nguyen, P.; Martorell, R. Effects of micronutrients on growth of children under 5 y of age: Meta-analyses of single and multiple nutrient interventions. Am. J. Clin. Nutr. 2009, 89, 191–203. [Google Scholar] [CrossRef]
- Stammers, A.L.; Lowe, N.M.; Medina, M.W.; Patel, S.; Dykes, F.; Perez-Rodrigo, C.; Serra-Majam, L.; Nissensohn, M.; Moran, V.H. The relationship between zinc intake and growth in children aged 1–8 years: A systematic review and meta-analysis. Eur. J. Clin. Nutr. 2015, 69, 147–153. [Google Scholar] [CrossRef]
- Flammarion, S.; Santos, C.; Guimber, D.; Jouannic, L.; Thumerelle, C.; Gottrand, F.; Deschildre, A. Diet and nutritional status of children with food allergies. Pediatr. Allergy Immunol. 2011, 22, 161–165. [Google Scholar] [CrossRef]
- Millward, D.J. Nutrition, infection and stunting: The roles of deficiencies of individual nutrients and foods, and of inflammation, as determinants of reduced linear growth of children. Nutr. Res. Rev. 2017, 30, 50–72. [Google Scholar] [CrossRef]
- Nakajima, S.; Naruto, T.; Miyamae, T.; Imagawa, T.; Mori, M.; Nishimaki, S.; Yokota, S. Interleukin-6 inhibits early differentiation of ATDC5 chondrogenic progenitor cells. Cytokine 2009, 47, 91–97. [Google Scholar] [CrossRef]
- Sederquist, B.; Fernandez-Vojvodich, P.; Zaman, F.; Sävendahl, L. Recent research on the growth plate: Impact of inflammatory cytokines on longitudinal bone growth. J. Mol. Endocrinol. 2014, 53, T35–T44. [Google Scholar] [CrossRef]
- Liao, C.R.; Wang, S.N.; Zhu, S.Y.; Wang, Y.Q.; Li, Z.Z.; Liu, Z.Y.; Jiang, W.S.; Chen, J.T.; Wu, Q. Advanced oxidation protein products increase TNF-α and IL-1β expression in chondrocytes via NADPH oxidase 4 and accelerate cartilage degeneration in osteoarthritis progression. Redox Biol. 2020, 28, 101306. [Google Scholar] [CrossRef]
- Seifarth, C.; Csaki, C.; Shakibaei, M. Anabolic actions of IGF-I and TGF-beta1 on Interleukin-1beta-treated human articular chondrocytes: Evaluation in two and three dimensional cultures. Histol. Histopathol. 2009, 24, 1245–1262. [Google Scholar]
- Mårtensson, K.; Chrysis, D.; Sävendahl, L. Interleukin-1beta and TNF-alpha act in synergy to inhibit longitudinal growth in fetal rat metatarsal bones. J. Bone Miner. Res. 2004, 19, 1805–1812. [Google Scholar] [CrossRef]
- Cole, C.R. Preventing hidden hunger in children using micronutrient supplementation. J. Pediatr. 2012, 161, 777–778. [Google Scholar] [CrossRef]
- Berry, M.J.; Adams, J.; Voutilainen, H.; Feustel, P.J.; Celestin, J.; Järvinen, K.M. Impact of elimination diets on growth and nutritional status in children with multiple food allergies. Pediatr. Allergy Immunol. 2015, 26, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Parracho, H.; McCartney, A.L.; Gibson, G.R. Probiotics and prebiotics in infant nutrition. Proc. Nutr. Soc. 2007, 66, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Fox, A.; Bird, J.A.; Fiocchi, A.; Knol, J.; Meyer, R.; Salminen, S.; Sitang, G.; Szajewska, H.; Papadopoulos, N. The potential for pre-, pro- and synbiotics in the management of infants at risk of cow’s milk allergy or with cow’s milk allergy: An exploration of the rationale, available evidence and remaining questions. World Allergy Organ. J. 2019, 12, 100034. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Li, X.; Yang, Y.; Shoaie, S.; Zhang, C.; Ji, B.; Wei, Y. Advances in the Relationships Between Cow’s Milk Protein Allergy and Gut Microbiota in Infants. Front. Microbiol. 2021, 16, 716667. [Google Scholar] [CrossRef]
- Berni Canani, R.; Di Costanzo, M.; Bedogni, G.; Amoroso, A.; Cosenza, L.; Di Scala, C.; Granata, V.; Nocerino, R. Extensively hydrolyzed casein formula containing Lactobacillus rhamnosus GG reduces the occurrence of other allergic manifestations in children with cow’s milk allergy: 3-year randomized controlled trial. J. Allergy Clin. Immunol. 2017, 139, 1906–1913.e4. [Google Scholar] [CrossRef]
- Nocerino, R.; Di Costanzo, M.; Bedogni, G.; Cosenza, L.; Maddalena, Y.; Di Scala, C.; Della Gatta, G.; Carucci, L.; Voto, L.; Coppola, S.; et al. Dietary Treatment with Extensively Hydrolyzed Casein Formula Containing the Probiotic Lactobacillus rhamnosus GG Prevents the Occurrence of Functional Gastrointestinal Disorders in Children with Cow’s Milk Allergy. J. Pediatr. 2019, 213, 137–142.e2. [Google Scholar] [CrossRef]
- Bode, L. Recent advances on structure, metabolism, and function of human milk oligosaccharides. J. Nutr. 2006, 136, 2127–2130. [Google Scholar] [CrossRef]
- Kulinich, A.; Liu, L. Human milk oligosaccharides: The role in the fine-tuning of innate immune responses. Carbohydr. Res. 2016, 432, 62–70. [Google Scholar] [CrossRef]
- Correa-Oliveira, R.; Fachi, J.L.; Vieira, A.; Sato, F.T.; Vinolo, M.A. Regulation of immune cell function by short-chain fatty acids. Clin. Transl. Immunol. 2016, 5, e73. [Google Scholar] [CrossRef]
- Carlson, J.L.; Erickson, J.M.; Lloyd, B.B.; Slavin, J.L. Health Effects and Sources of Prebiotic Dietary Fiber. Curr. Dev. Nutr. 2018, 29, nzy005. [Google Scholar] [CrossRef]
- Maryniak, N.Z.; Sancho, A.I.; Hansen, E.B.; Bøgh, K.L. Alternatives to Cow’s Milk-Based Infant Formulas in the Prevention and Management of Cow’s Milk Allergy. Foods 2022, 11, 926. [Google Scholar] [CrossRef]
- Li, Y.; Yao, J.; Han, C.; Yang, J.; Chaudhry, M.T.; Wang, S.; Liu, H.; Yin, Y. Quercetin, Inflammation and Immunity. Nutrients 2016, 8, 167. [Google Scholar] [CrossRef]
- Karaman, M.; Firinci, F.; Cilaker, S.; Uysal, P.; Tugyan, K.; Yilmaz, O.; Uzuner, N.; Karaman, O. Anti-inflammatory effects of curcumin in a murine model of chronic asthma. Allergol. Immunopathol. 2012, 40, 210–214. [Google Scholar] [CrossRef]
- Yang, N.; Wang, J.; Liu, C.; Song, Y.; Zhang, S.; Zi, J.; Zhan, J.; Masilamani, M.; Cox, A.; Nowak-Wegrzyn, A.; et al. Berberine and limonin suppress IgE production by human B cells and peripheral blood mononuclear cells from food-allergic patients. Ann. Allergy Asthma Immunol. 2014, 113, 556–564.e4. [Google Scholar] [CrossRef]
- Integratori Alimentari e Linee Guida Ministeriali (LGM). Available online: https://www.salute.gov.it/portale/temi/p2_6.jsp?area=Alimenti%20particolari%20e%20integratori&id=1267&menu=integratori (accessed on 26 June 2023).
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; WHO Press: Geneva, Switzerland, 2006. [Google Scholar]
- Fiocchi, A.; Terracciano, L.; Bouygue, G.R.; Veglia, F.; Sarratud, T.; Martelli, A.; Restani, P. Incremental prognostic factors associated with cow’s milk allergy outcomes in infant and child referrals: The Milan Cow’s Milk Allergy Cohort study. Ann. Allergy Asthma Immunol. 2008, 101, 166–173. [Google Scholar] [CrossRef]
- Cherkaoui, S.; Bégin, P.; Paradis, L.; Paradis, J.; Des Roches, A. Powder milk: A user-friendly and safe product for heated-milk food challenge? Allergy Asthma Clin. Immunol. 2015, 23, 39. [Google Scholar] [CrossRef]
- Nowak-Węgrzyn, A.; Lawson, K.; Masilamani, M.; Kattan, J.; Bahnson, H.T.; Sampson, H.A. Increased Tolerance to Less Extensively Heat-Denatured (Baked) Milk Products in Milk-Allergic Children. J. Allergy Clin. Immunol. Pract. 2018, 6, 486–495.e5. [Google Scholar] [CrossRef]
- Dunlop, J.H.; Keet, C.A.; Mudd, K.; Wood, R.A. Long-Term Follow-Up After Baked Milk Introduction. J. Allergy Clin. Immunol. Pract. 2018, 6, 1699. [Google Scholar] [CrossRef]
- Tosca, M.A.; Olcese, R.; Marinelli, G.; Schiavetti, I.; Ciprandi, G. Oral Immunotherapy for Children with Cow’s Milk Allergy: A Practical Approach. Children 2022, 30, 1872. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).