Abstract
It has long been recognized that intestinal parasite infections and undernutrition are closely linked. However, little is known about the role of intestinal parasite infections (IPIs), or parasite clearance, in these processes. The aim of this scoping review was to summarize published evidence on the association between IPIs and body composition. PRISMA guidelines, PubMed/MEDLINE, EMBASE and Cochrane Library databases were searched up until June 2021. Studies reporting on IPIs in relation to (proxies for) body composition were eligible. Study quality and risk of bias were assessed using Joanna Briggs Institute (JBI) critical appraisal tools. Twenty-four studies were included, two Randomized Control Trials (RCTs) and 22 observational. Most observational studies showed IPIs to be associated with lower Body Mass Index (BMI) or being underweight as proxies for body composition. One RCT showed no effect of antiparasitic treatment on body composition, while the other one showed a significant post-treatment increase in body fat, as measured by BMI z-scores and skinfolds. This review lends support to distinct associations between IPIs and body composition. More longitudinal studies are needed using direct measures of body composition to investigate whether weight gained after antiparasitic treatment concerns an increase in body fat or healthy weight gain.
1. Introduction
Intestinal parasite infections and undernutrition are major health problems in low- and middle-income countries (LMIC). According to World Health Organization (WHO), more than 1.5 billion people, or 24% of the world’s population, are infected with soil-transmitted helminths, the largest group of intestinal parasite infections, contributing 5.2 million disability-adjusted life-years worldwide in 2010 [1,2]. Globally, 47 million children under 5 years of age are wasted, and 144 million are stunted [3]. Around 45% of deaths among children under 5 years of age are linked to undernutrition [3].
Prior research has demonstrated that undernutrition early in life is associated with an increased risk of a number of chronic disease outcomes [4,5,6,7,8,9]. Further studies have shown that the increased risk of chronic disease is specifically related to accelerated weight gain [10] even during recovery from undernutrition [11,12]. Research from Brazil has shown that stunted children deposited more fat and suffered more from overweight and obesity than non-stunted children [13]. Furthermore, undernourished children were likely to experience rapid weight gain during nutritional rehabilitation [14]. Moreover, studies have shown that during a period of rapid weight gain, fat mass is disproportionately accrued over fat-free mass [15]. Hence, undernutrition and nutritional recovery are associated with weight gain and body fat deposits.
It is well-known that intestinal parasite infections and early child undernutrition are closely interrelated [14,16,17]. However, little is known about the relationship between intestinal parasite infections, parasite clearance, and weight gain or (changes in) body fat. Sawaya et al. [8] showed that a combination of dietary and anti-parasitic measures was able to alter metabolic changes in Brazilian children. Moreover, a study in Chile suggested that dietary interventions which only target undernutrition can lead to an increased risk of overweight/obesity [18]. In addition, Mexican children infected with Entamoeba coli were found to have a significantly higher waist circumference, waist to height ratio, and percentage of body and abdominal fat than children not infected or with a light infection [19]. These results suggest that intestinal parasite infection may play a role in the relationship between child undernutrition and overweight/obesity [20].
The importance of clarifying the relationship between intestinal parasite infection, early child undernutrition, weight gain and body fat deposits is underscored by documented global trends of increasing overweight and obesity prevalence [21] in LMIC. Current estimates show that 3.3 billion adults will be overweight or obese by 2030 [20]. This rapid rise in overweight and obesity is of particular concern because it occurs in addition to continuing child undernutrition [22], and in countries where parasitic infections remain endemic. In this context, the aim of this review is to summarize published findings reporting on the association between intestinal parasite infections (IPIs) and body composition.
2. Materials and Methods
2.1. Data Sources and Search Strategy
Searches were conducted on MEDLINE, EMBASE and Cochrane Library. Search terms included several variations on body fat, BMI, body composition, overweight, obesity, parasitic infections, parasites, helminths, intestinal parasites, protozoa, Entamoeba coli, Giardia, Entamoeba histolytica, Cryptosporidium, Ascaris, Trichuris, Ancylostoma, Necator, hookworm, whipworm, roundworm, pinworm, deworm, Strongyloides in the titles and abstracts of studies and where possible as MeSH terms or Emtree terms (Table 1). The references obtained from the three search engines were merged in a single file using Endnote X8-software (Thompson Reuters, San Francisco, CA, USA). After removing duplicates, the titles, abstracts, and keywords were reviewed for inclusion. When the articles met the inclusion criteria, they were entirely scrutinized and the data were extracted.

Table 1.
Search strategies used in the Databases.
A first search was conducted in June 2021 by ICM and replicated by a second researcher in August 2021 by CR. The review was carried out in accordance with the PRISMA reporting checklist [23] for scoping reviews (Table S1).
2.2. Eligibility Criteria
2.2.1. Study Inclusion Criteria
No restrictions by study design were applied. Thus, all published, relevant, peer-reviewed scientific articles including randomized controlled trials (RCTs), other interventions, or observational studies were eligible for inclusion. Studies were included if they reported on intestinal, i.e., protozoan or helminthic, parasitic infections and one or more measures of body composition. Studies that used microscopy, molecular and/or serological tests to detect intestinal parasite infection were selected; other methods of assessment (e.g., questionnaires) were not eligible. Studies were eligible if they reported on body composition using measures that distinguish between fat and fat-free mass, such as skinfolds, Dual-energy X-ray absorptiometry—DEXA/DXA, and bio-electrical impedance analysis (BIA). In addition, studies were selected if they reported proxy measurements of body composition using weight-for-height measures, such as body mass index (BMI), BMI z-scores (BMIZ), and weight-for-height z-scores (WHZ), or overweight/obesity using WHO definitions [24]. Studies with any effect estimates or statistical comparisons indicating associations between intestinal parasite infection and body composition were included, such as mean values/differences (±Standard Deviations, SD’s), Odds Ratios (OR) and Relative Risk (RR) with 95% Confidence Intervals (CI), p-values (p < 0.05 significance) or regression coefficients.
2.2.2. Study Exclusion Criteria
Studies were excluded if they were not in English, were non-human studies and/or were not published in peer review journals. Additionally, all review articles, editorial papers and abstracts from symposia, conferences, or seminars were excluded. Articles reporting on interim results or incomplete findings did not meet the eligibility criteria. All published studies related to parasites other than intestinal parasites were excluded. Similarly, studies reporting only anthropometric measures, such as height or stunting, but not on body composition were excluded. Lastly, studies that reported having measured intestinal parasite infections and body composition but did not specifically analyze or report on the association between the two were also excluded.
2.3. Quality Assessment of Included Studies
The quality of eligible studies and the potential for risk of bias were independently assessed by two reviewers; any discrepancies were resolved by discussion or arbitration by a third reviewer. The risk of bias was assessed by using the Joanna Briggs Institute (JBI) critical appraisal tool [25]. The checklists for cross-sectional and RCTs studies were applied with 8 and 13 questions, respectively. Each study was scored according to the structured questions. The responses were scored 0 for “Not reported”, 1 for “Yes” and NA for “Not Applicable”. Studies with medium (fulfilling 50% of quality assessment parameters) and high quality were included for analysis.
2.4. Data Extraction and Comparison
Extracted data included first author/year, study setting and design, the number of participants, age, intestinal parasites identified, and body composition measures used. Moreover, the time frame of the observational studies was included.
From studies identified as RCTs, additional information pertaining to antiparasitic treatment and follow-up times was also included. Observational studies were described and compared separately from RCTs. For the observational studies, results could only be compared between studies using similar measures of anthropometric outcomes. Where mean differences were not reported, these were calculated using the group means reported by the authors. All other results were reported as presented by the authors.
3. Results
The results of combined searches from MEDLINE, EMBASE and the COCHRANE Library databases are shown in Figure 1. From the three search engines, 1435 references were obtained. Duplicate references were identified and removed, leaving 1358 references. After screening, 124 articles for full-text screening remained. Based on the potentially relevant full-text articles, 25 articles met the initial criteria for inclusion in this review. We further excluded one article only reporting a p-value with no indication of the effect estimate or the direction of the association and another one that did not compare if weight categories (by BMI) were related to helminth/no helminth infection, leaving 24 articles, of which 22 reported on observational studies and two on experimental studies (randomized controlled trials). All the studies were included based on the JBI quality assessment criteria as they all fulfilled 100% of the quality assessment parameters (Table S2).
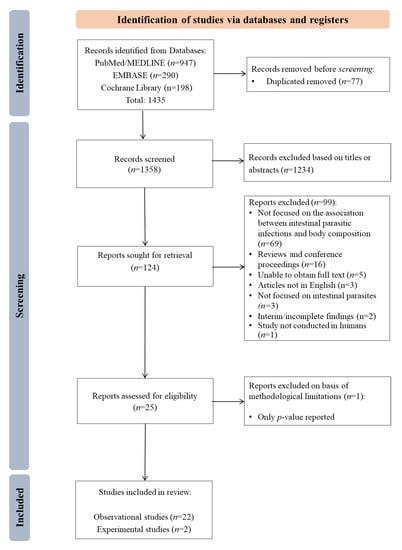
Figure 1.
Flowchart of the search and selection of the studies for review.
The characteristics of all studies included in this review are presented in Table 2. Studies were carried out worldwide, with a majority of studies being from South America and Asia. Most study designs were reported as cross-sectional or retrospective, with only two of the observational studies being reported as longitudinal. The sample size of the studies varied, ranging from smaller studies (n = 150) to larger studies (n = 16,347). Although most studies were conducted on children, the age of study participants varied from infants to the elderly. Most of the intestinal parasite infections measured were soil-transmitted helminths (i.e., Ascaris, Trichuris and hookworm) and BMI was the basis for most of the reported body composition measures.

Table 2.
Characteristics of the studies included.
Table 2.
Characteristics of the studies included.
| Author, Year | Study Setting, Years | Study Design | No. of Participant | Age of the Participants | Intestinal Parasite Infections (IPI’s) Reported | Body Composition Reported | References |
|---|---|---|---|---|---|---|---|
| Amare et al., 2013 | Ethiopia, 2008 | Cross-Sectional | 405 | 12.09 ± 2.54 y | Ascaris, Hookworm, Trichuris, Strongyloides Giardia, Entamoeba spp. | BMI, BMIZ | [26] |
| Campos-Ponce et al., 2012 | Venezuela, 2010 | Cross-Sectional | 225 | 0–19 y, >19 y | Giardia, Geohelminths, IPI | BMI | [18] |
| Casapia et al., 2007 | Peru, 2005–2006 | Cross-Sectional | 252 | <5 y | Ascaris, Hookworm, Trichuris | WHZ | [27] |
| Chu et al., 2013 | Taiwan, 2010 | Cross-Sectional | 11,080 | 7–14 y | Pinworm | BMI | [28] |
| Geltman et al., 2001 | USA, 1995–1998 | Cross-Sectional | 1825 | <18 y | IPI | WHZ, BMI | [29] |
| Gerber et al., 2018 | South Africa, 2015 | Cross-Sectional | 801 | 8–12 y | Ascaris, Trichuris | BMI, Body fat | [30] |
| Jardim-Botelho et al., 2008 | Brazil, 2004 | Cross-Sectional | 1113 | 0–18, >18 y | Ascaris, Hookworm, Trichuris, Strongyloides | Triceps SF, WHZ, BMI, BMI/AGE, MUAC | [31] |
| Kurscheid et al., 2020 | Indonesia, 2015 | Cross-Sectional | 998 | 2–12 y | Ascaris, Hookworm, Trichuris | BMI | [32] |
| Lander et al., 2015 | Brazil, 2010 | Cross-Sectional | 376 | 3–6 y | Helminths | WHZ, BMI, BMIZ | [33] |
| Li et al., 2015 | China, 2012 | Cross-Sectional | 369 | 50–70 y | Hookworm, Ascaris, Protozoa, Helminths | BMI | [34] |
| Orden et al., 2014 | Argentina, 2009–2011 | Cross-Sectional | 708 | 3–11 y | Giardia, Ascaris, Trichuris | BMI, Triceps, Subscapular SF, BMIZ | [35] |
| Patel and Khandekar, 2006 | Oman, 2004–2005 | Cross-Sectional | 436 | 9–10 y | Entamoeba, Giardia, Ascaris, Trichuris, Hookworm, Strongyloides | BMI | [36] |
| Rivero et al., 2018 | Argentina, 2017 | Cross-Sectional | 303 | <15 y | Helminths (Enterobius, Hookworms, Strongyloides, Hymenolepis, Ascaris), Protozoans (Giardia, Entamoeba, Blastocystis, Chilomastix, Endolimax, Cryptosporidium, Iodamoeba) | BMIZ | [37] |
| Quihui-Cota et al., 2015 | Mexico, 2008–2009 | Cross-Sectional | 405 | 6–13 y | Cryptosporidium | BMI/AGE | [38] |
| Sanchez et al., 2013 | Honduras, 2011 | Cross-Sectional | 320 | 7–14 y | Ascaris, Hookworm, Trichuris, STH | BMI/AGE | [39] |
| Sayasone et al., 2015 | Lao PDR, 2007 | Cross-Sectional | 1313 | 6 mo–12 y | Ascaris, Hookworm, Trichuris | BMI/AGE, WHZ | [40] |
| Stephenson et al., 1989 | Kenya, 1986 | Randomized controlled trial | 150 | 6–16 y | Ascaris, Hookworm, Trichuris | WH, Triceps, subscapular SF | [41] |
| Verhagen et al., 2013 | Venezuela, 2010–2011 | Cross-Sectional | 390 | 4–6 y | Ascaris, Trichuris, Hookworm, Giardia, Strongyloides, Helminths | BMI/AGE, WHZ | [42] |
| Wiria et al., 2013a | Indonesia, 2008–2010 | Randomized controlled trial | 4004 | >2 y (at semi-urban areas) and 5–15 y (at rural areas) | Helminths, Ascaris, Hookworm, Trichuris, Strongyloides, Ancylostoma | BMI | [43] |
| Wiria et al., 2013b | Indonesia, 2009 | Cross-Sectional | 675 | 18–80 y | Ascaris, Trichuris, Strongyloides, Ancylostoma | BMI | [44] |
| Zavala et al., 2016 | Mexico, 2013 | Cross-Sectional | 296 | 6–10 y | Ascaris, Balantidium coli, Hookworm, Giardia, E. coli, E. histolytica, E. nana, | BMI/AGE, Body Composition (Body Fat) | [19] |
| Zavala et al., 2019 | Mexico, 2000, 2006 and 2012 | Ecological | 1–5 y (8927), 6–10 y (16,347) and 11–19 y (13,992) | 1–19 y | Ascaris, Protozoa | BMI/AGE | [38] |
| Zhou et al., 2007 | China, 2001–2005 | Longitudinal | 274 | 10–12 y | Ascaris, Trichuris | BMI, BMI/AGE | [34] |
BMI: Body mass index; BMI/AGE: BMI-for-age z-score; BMIZ: Body mass index z-score; mo: months; MUAC: Mid-Upper Arm Circumference; NR: Not reported; SF: skinfolds; y: years old; WH: Weight-for-height; WHZ: Weight-for-height z-score.
Table 3 shows the results of the experimental (RCT) studies. Stephenson et al. [17] reported that albendazole treatment was associated with a greater increase in both triceps and subscapular skinfolds and a greater increase in weight-for-height percentage compared to the placebo group at 6 months follow-up. Wiria et al. [43] found no significant change in BMIZ or BMI, in children and adults, respectively, at 9 and 21 months after treatment.

Table 3.
Characteristics of the experimental studies included (RCT’s).
The results of observational studies reporting on the association between intestinal parasite infections and direct measures of body composition are presented in Table 4. Zavala et al. [19] showed that children infected with intestinal parasites tended to have higher body fat (in kg) but less abdominal or body fat (in %) but these results were not statistically significant. In the same article, Zavala et al. [19] described a species-specific effect of the non-pathogenic intestinal parasite Entamoeba coli (results not shown in Table 4). According to them, children with a moderate-heavy infection with E. coli had significantly higher body fat and abdominal fat compared to children that were not infected or had a light intensity infection (p < 0.05). Similar results were observed in moderate-heavy infection with E. nana and in light infection with Ascaris; however, the results were not statistically significant. The results of Jardim-Botelho et al. [31] showed that both children and adults that were infected with either Ascaris or hookworm were more likely to have lower body (fat and fat-free) mass using skinfold measures. Gerber et al. [30] showed that for every unit increase in skinfolds, children were less likely to be infected by Ascaris, Trichuris, or both, although these results were not statistically significant.

Table 4.
Association between intestinal parasite infections and direct measures of body composition.
Table 5 shows the results of the observational studies that describe the association between intestinal parasite infection status and indirect measures/proxies of body composition, reported mainly as BMI followed by WHZ and dichotomous evaluations of weight-for-height measures. Both Wiria et al. [44] and Li et al. [34] showed that adults infected with intestinal parasites were more likely to have a lower BMI (p < 0.05). This same pattern was observed in children using various measures of weight-for-height, as reported by Gerber et al. [30], Verhagen et al. [42], Zhou et al. [45], Geltman et al. [29], Chu et al. [28], Sayasone et al. [40], Lander et al. [33] and Zavala et al. for Ascaris infection (p < 0.05) [46]. Several other studies also showed parasitic infections associated with lower weight-for-height indicators, although the outcomes were not statistically significant (Patel and Khandekar [36], Casapia et al. [27], Amare et al. [26], Sanchez et al. [39], Orden et al. [35] and Rivero et al. [37]). Zavala et al. showed an opposite, statistically significant association for intestinal protozoa [46] and for IPI [19]. The same pattern was also found by Quihui-Cota et al. [38] and Campos Ponce et al. [18], although it was not statistically significant. Wasilewska et al. [47] found no association between BMIZ and Ascaris infection in children (OR = 0.98). Likewise, Kurscheid et al. [32] found no association between BMI and Trichuris and/or hookworm and/or Ascaris infection. However, the results of both studies were not statistically significant.

Table 5.
Associations between intestinal parasite infection status and proxy (weight-for-height) measures of body composition.
4. Discussion
We identified 24 studies that reported on the association between intestinal parasite infection and body composition. Of these, most used weight-for-height measures (BMI, BMIZ or WHZ) as proxies for body composition. The observational studies showed a clear and consistent pattern by which intestinal parasite infection was associated with a lower BMI or with being underweight. Likewise, those with intestinal parasites were less likely to be overweight/obese. These findings are consistent with the existing literature showing parasitic infection to be associated with undernutrition, such as stunting or micronutrient deficiency [48,49].
Consistent with the findings of the observational studies, the RCT by Stephenson et al. [17] found albendazole treatment to be associated with a greater increase in weight-for-height percentage than the comparison group, a result that was confirmed using skinfold measures as a more direct measure for body fat. The potential increase in weight is even more important given the findings of a systematic review by Welch et al. [50] showing deworming to have no effect on growth in height. In contrast, the RCT by Wiria et al. [43] showed almost no change in BMI after albendazole treatment. However, this study was carried out in a broader age group, including adults. Children are more vulnerable to adipose weight gain than adults because the relationship between adiposity development and rapid weight gain is thought to be driven by growth hormones [51]. These RCTs used BMI and skinfolds considering that they are simple, inexpensive and easily applicable in fieldwork. Moreover, the tools suggested in each study are ideal considering the age of the participant but less sensitive to directly determining body composition.
It is important to note a number of limitations in this review. Since the studies used different (in)direct measures of body composition (BMI, BMIZ, WHZ, Mid-Upper Arm Circumference—MUAC, skinfolds taken at different time points, and DEXA), results could not be directly compared, and therefore, a meta-analysis could not be done. The limitations of weight-for-height measures (BMI/BMIZ/WHZ) of body composition are well known [52]. Although weight-for-height measures are commonly used as indicators of thinness, wasting, underweight, overweight and obesity, these measures do not distinguish between weight gained as fat versus fat-free mass [50]. Some studies reported skinfold measures, which were taken in different places, such as triceps or subscapular skinfolds. Skinfold measures provide more direct proxies for body fat and fat distribution than weight-for-height measures, but the validity is sensitive to the skills of the anthropometrist [50].
In addition to different outcomes related to body composition, the studies used different age groups, with some studies specifically looking at a narrow age range in children, others with more broad age ranges only in adults or only in children, and others combining both adults and children. Moreover, as can be seen from Table 2, nearly every study investigated different (sets of) parasitic infections, and only a few reported findings separately by parasite species. Additionally, the respective studies showed important variations by country and year. These (and other) differences in methodology, design and context hampered direct comparison between studies and may explain some of the inconsistent findings, in particular for the two RCT studies.
Despite the differences, there is consistency across multiple studies lending support to the association between intestinal parasite infections and body composition. As previously stated, we do not know whether the thinness related to parasite infections is due to loss of fat-free mass, loss of fat, or both together. The same holds for weight gain related to parasite clearance and whether this can be attributed to muscle gain, fat gain, or both. However, the findings by Stephenson et al. [17] imply that, under some circumstances, antiparasitic treatment can be related to a relative increase in fat mass.
5. Conclusions
While the treatment of parasitic infections is generally assumed to be essential to recovery from undernutrition, it is important to study changes in body composition to ensure healthy weight gain after recovery from parasitic infection. Longitudinal studies are needed to monitor individual, household and community risk factors that can contribute to changes in body composition after antiparasitic treatment. Such studies are of particular interest in Africa, where intestinal parasite infections are still endemic and where obesity is likely to emerge and/or spread. Additionally, these studies should target body composition using more sensitive tools, such as computed tomography (CT) scanning, or DEXA/DXA and/or BIA scanning.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14112229/s1, Table S1: Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist and Table S2: Study design and quality assessment of the studies included in scoping review.
Author Contributions
Conceptualization, C.D., M.C.-P. and K.P.; methodology, C.D., K.P., C.R. and I.C.-M.; validation, K.P., C.D., M.C.-P. and C.R.; formal analysis, I.C.-M.; investigation, I.C.-M.; resources, I.C.-M., C.R., M.C.-P. and C.D.; data curation, I.C.-M. and C.R.; writing—original draft preparation, I.C.-M. and C.R.; writing—review and editing, I.C.-M., C.R., T.M.Q., M.C.-P., N.d.D., K.P. and C.D.; supervision, C.D., M.C.-P. and K.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the ethical reasons.
Acknowledgments
The authors would like to acknowledge Miglé Abromaviciute (M.A.) for her help in replicating the first search.
Conflicts of Interest
The authors declare no conflict of interest.
References
- WHO|Soil-Transmitted Helminthiases. Available online: http://www.who.int/gho/neglected_diseases/soil_transmitted_helminthiases/en/ (accessed on 16 December 2020).
- World Health Organization (WHO). Preventive Chemotherapy to Control Soil-Transmitted Helminth Infections in at-Risk Population Groups Guideline; World Health Organization: Geneva, Switzerland, 2017; ISBN 978 92 4 155011 6. [Google Scholar]
- Fact Sheets—Malnutrition. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 16 December 2020).
- Barker, D.J.P.; Eriksson, J.G.; Forsén, T.; Osmond, C. Fetal Origins of Adult Disease: Strength of Effects and Biological Basis. Int. J. Epidemiol. 2002, 31, 1235–1239. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, J.G.; Kajantie, E.; Thornburg, K.L.; Osmond, C.; Barker, D.J.P. Mother’s Body Size and Placental Size Predict Coronary Heart Disease in Men. Eur. Heart J. 2011, 32, 2297–2303. [Google Scholar] [CrossRef] [PubMed]
- Forsén, T.; Eriksson, J.; Tuomilehto, J.; Reunanen, A.; Osmond, C.; Barker, D. The Fetal and Childhood Growth of Persons Who Develop Type 2 Diabetes. Ann. Intern. Med. 2000, 133, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Stanner, S.A.; Yudkin, J.S. Fetal Programming and the Leningrad Siege Study. Twin Res. 2001, 4, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Sawaya, A.L.; Sesso, R.; Florêncio, T.M.; Fernandes, M.T.; Martins, P.A. Association between Chronic Undernutrition and Hypertension. Matern. Child. Nutr. 2005, 1, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, D.J.; Martins, P.A.; Roberts, S.B.; Sawaya, A.L. Body Fat Distribution in Stunted Compared with Normal-Height Children from the Shantytowns of São Paulo, Brazil. Nutrition 2007, 23, 640–646. [Google Scholar] [CrossRef]
- Adair, L.S.; Martorell, R.; Stein, A.D.; Hallal, P.C.; Sachdev, H.S.; Prabhakaran, D.; Wills, A.K.; Norris, S.A.; Dahly, D.L.; Lee, N.R.; et al. Size at Birth, Weight Gain in Infancy and Childhood, and Adult Blood Pressure in 5 Low- and Middle-Income-Country Cohorts: When Does Weight Gain Matter? Am. J. Clin. Nutr. 2009, 89, 1383–1392. [Google Scholar] [CrossRef]
- Adair, L.S.; Fall, C.H.D.; Osmond, C.; Stein, A.D.; Martorell, R.; Ramirez-Zea, M.; Sachdev, H.S.; Dahly, D.L.; Bas, I.; Norris, S.A.; et al. Associations of Linear Growth and Relative Weight Gain during Early Life with Adult Health and Human Capital in Countries of Low and Middle Income: Findings from Five Birth Cohort Studies. Lancet 2013, 382, 525–534. [Google Scholar] [CrossRef]
- Victora, C.G.; Adair, L.; Fall, C.; Hallal, P.C.; Martorell, R.; Richter, L.; Sachdev, H.S. Maternal and Child Undernutrition Study Group Maternal and Child Undernutrition: Consequences for Adult Health and Human Capital. Lancet 2008, 371, 340–357. [Google Scholar] [CrossRef]
- Martins, P.A.; Hoffman, D.J.; Fernandes, M.T.B.; Nascimento, C.R.; Roberts, S.B.; Sesso, R.; Sawaya, A.L. Stunted Children Gain Less Lean Body Mass and More Fat Mass than Their Non-Stunted Counterparts: A Prospective Study. Br. J. Nutr. 2004, 92, 819–825. [Google Scholar] [CrossRef]
- Papier, K.; Williams, G.M.; Luceres-Catubig, R.; Ahmed, F.; Olveda, R.M.; McManus, D.P.; Chy, D.; Chau, T.N.P.; Gray, D.J.; Ross, A.G.P. Childhood Malnutrition and Parasitic Helminth Interactions. Clin. Infect. Dis. 2014, 59, 234–243. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishna, K.V.; Kulkarni, B.; Balakrishna, N.; Rajkumar, H.; Omkar, C.; Shatrugna, V. Composition of Weight Gain during Nutrition Rehabilitation of Severely under Nourished Children in a Hospital Based Study from India. Asia Pac. J. Clin. Nutr. 2010, 19, 8–13. [Google Scholar] [PubMed]
- Rajoo, Y.; Ambu, S.; Lim, Y.A.L.; Rajoo, K.; Tey, S.C.; Lu, C.W.; Ngui, R. Neglected Intestinal Parasites, Malnutrition and Associated Key Factors: A Population Based Cross-Sectional Study among Indigenous Communities in Sarawak, Malaysia. PLoS ONE 2017, 12, e0170174. [Google Scholar] [CrossRef]
- Stephenson, L.S. Helminth Parasites, a Major Factor in Malnutrition. World Health Forum 1994, 15, 169–172. [Google Scholar]
- Campos Ponce, M.; Incani, R.N.; Pinelli, E.; Ten Kulve, N.; Ramak, R.; Polman, K.; Doak, C.M. Are Intestinal Parasites Fuelling the Rise in Dual Burden Households in Venezuela? Trans. R. Soc. Trop. Med. Hyg. 2013, 107, 119–123. [Google Scholar] [CrossRef]
- Zavala, G.A.; García, O.P.; Campos-Ponce, M.; Ronquillo, D.; Caamaño, M.C.; Doak, C.M.; Rosado, J.L. Children with Moderate-High Infection with Entamoeba Coli Have Higher Percentage of Body and Abdominal Fat than Non-Infected Children. Pediatr. Obes. 2016, 11, 443–449. [Google Scholar] [CrossRef]
- Global Nutrition Transition and the Pandemic of Obesity in Developing Countries—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/22221213/ (accessed on 16 December 2020).
- Global, Regional, and National Prevalence of Overweight and Obesity in Children and Adults during 1980–2013: A Systematic Analysis for the Global Burden of Disease Study 2013—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/24880830/ (accessed on 16 December 2020).
- Wojcicki, J.M. The Double Burden Household in Sub-Saharan Africa: Maternal Overweight and Obesity and Childhood Undernutrition from the Year 2000: Results from World Health Organization Data (WHO) and Demographic Health Surveys (DHS). BMC Public Health 2014, 14, 1124. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO Growth Reference for School-Aged Children and Adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Site Home Page|Joanna Briggs Institute. Available online: https://jbi.global/ (accessed on 23 September 2021).
- Amare, B.; Ali, J.; Moges, B.; Yismaw, G.; Belyhun, Y.; Gebretsadik, S.; Woldeyohannes, D.; Tafess, K.; Abate, E.; Endris, M.; et al. Nutritional Status, Intestinal Parasite Infection and Allergy among School Children in Northwest Ethiopia. BMC Pediatr. 2013, 13, 7. [Google Scholar] [CrossRef]
- Casapía, M.; Joseph, S.A.; Núñez, C.; Rahme, E.; Gyorkos, T.W. Parasite and Maternal Risk Factors for Malnutrition in Preschool-Age Children in Belen, Peru Using the New WHO Child Growth Standards. Br. J. Nutr. 2007, 98, 1259–1266. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chu, C.-H.; Wang, J.-H.; Jan, R.-H.; Huang, C.-H.; Cheng, C.-F. Association between Health Examination Items and Body Mass Index among School Children in Hualien, Taiwan. BMC Public Health 2013, 13, 975. [Google Scholar] [CrossRef] [PubMed]
- Geltman, P.L.; Radin, M.; Zhang, Z.; Cochran, J.; Meyers, A.F. Growth Status and Related Medical Conditions among Refugee Children in Massachusetts, 1995-1998. Am. J. Public Health 2001, 91, 1800–1805. [Google Scholar] [CrossRef] [PubMed]
- Gerber, M.; Müller, I.; Walter, C.; du Randt, R.; Adams, L.; Gall, S.; Joubert, N.; Nqweniso, S.; Smith, D.; Steinmann, P.; et al. Physical Activity and Dual Disease Burden among South African Primary Schoolchildren from Disadvantaged Neighbourhoods. Prev. Med. 2018, 112, 104–110. [Google Scholar] [CrossRef]
- Jardim-Botelho, A.; Brooker, S.; Geiger, S.M.; Fleming, F.; Souza Lopes, A.C.; Diemert, D.J.; Corrêa-Oliveira, R.; Bethony, J.M. Age Patterns in Undernutrition and Helminth Infection in a Rural Area of Brazil: Associations with Ascariasis and Hookworm. Trop. Med. Int. Health 2008, 13, 458–467. [Google Scholar] [CrossRef]
- Kurscheid, J.; Laksono, B.; Park, M.J.; Clements, A.C.A.; Sadler, R.; McCarthy, J.S.; Nery, S.V.; Soares-Magalhaes, R.; Halton, K.; Hadisaputro, S.; et al. Epidemiology of Soil-Transmitted Helminth Infections in Semarang, Central Java, Indonesia. PLoS Negl. Trop. Dis. 2020, 14, e0008907. [Google Scholar] [CrossRef]
- Lander, R.L.; Williams, S.M.; Costa-Ribeiro, H.; Mattos, A.P.; Barreto, D.L.; Houghton, L.A.; Bailey, K.B.; Lander, A.G.; Gibson, R.S. Understanding the Complex Determinants of Height and Adiposity in Disadvantaged Daycare Preschoolers in Salvador, NE Brazil through Structural Equation Modelling. BMC Public Health 2015, 15, 1086. [Google Scholar] [CrossRef]
- Li, X.-X.; Chen, J.-X.; Wang, L.-X.; Tian, L.-G.; Zhang, Y.-P.; Dong, S.-P.; Hu, X.-G.; Liu, J.; Wang, F.-F.; Wang, Y.; et al. Prevalence and Risk Factors of Intestinal Protozoan and Helminth Infections among Pulmonary Tuberculosis Patients without HIV Infection in a Rural County in P. R. China. Acta Trop. 2015, 149, 19–26. [Google Scholar] [CrossRef]
- Orden, A.B.; Apezteguía, M.C.; Ciarmela, M.L.; Molina, N.B.; Pezzani, B.C.; Rosa, D.; Minvielle, M.C. Nutritional Status in Parasitized and Nonparasitized Children from Two Districts of Buenos Aires, Argentina. Am. J. Hum. Biol. 2014, 26, 73–79. [Google Scholar] [CrossRef]
- Patel, P.K.; Khandekar, R. Intestinal Parasitic Infections among School Children of the Dhahira Region of Oman. Saudi. Med. J. 2006, 27, 627–632. [Google Scholar]
- Rivero, M.R.; De Angelo, C.; Nuñez, P.; Salas, M.; Liang, S. Intestinal Parasitism and Nutritional Status among Indigenous Children from the Argentinian Atlantic Forest: Determinants of Enteroparasites Infections in Minority Populations. Acta Trop. 2018, 187, 248–256. [Google Scholar] [CrossRef]
- Quihui-Cota, L.; Lugo-Flores, C.M.; Ponce-Martínez, J.A.; Morales-Figueroa, G.G. Cryptosporidiosis: A Neglected Infection and Its Association with Nutritional Status in Schoolchildren in Northwestern Mexico. J. Infect. Dev. Ctries. 2015, 9, 878–883. [Google Scholar] [CrossRef][Green Version]
- Sanchez, A.L.; Gabrie, J.A.; Usuanlele, M.-T.; Rueda, M.M.; Canales, M.; Gyorkos, T.W. Soil-Transmitted Helminth Infections and Nutritional Status in School-Age Children from Rural Communities in Honduras. PLoS Negl. Trop. Dis. 2013, 7, e2378. [Google Scholar] [CrossRef]
- Sayasone, S.; Utzinger, J.; Akkhavong, K.; Odermatt, P. Multiparasitism and Intensity of Helminth Infections in Relation to Symptoms and Nutritional Status among Children: A Cross-Sectional Study in Southern Lao People’s Democratic Republic. Acta Trop. 2015, 141, 322–331. [Google Scholar] [CrossRef]
- Stephenson, L.S.; Latham, M.C.; Kurz, K.M.; Kinoti, S.N.; Brigham, H. Treatment with a Single Dose of Albendazole Improves Growth of Kenyan Schoolchildren with Hookworm, Trichuris Trichiura, and Ascaris Lumbricoides Infections. Am. J. Trop. Med. Hyg. 1989, 41, 78–87. [Google Scholar] [CrossRef]
- Verhagen, L.M.; Incani, R.N.; Franco, C.R.; Ugarte, A.; Cadenas, Y.; Sierra Ruiz, C.I.; Hermans, P.W.M.; Hoek, D.; Campos Ponce, M.; de Waard, J.H.; et al. High Malnutrition Rate in Venezuelan Yanomami Compared to Warao Amerindians and Creoles: Significant Associations with Intestinal Parasites and Anemia. PLoS ONE 2013, 8, e77581. [Google Scholar] [CrossRef]
- Wiria, A.E.; Hamid, F.; Wammes, L.J.; Kaisar, M.M.M.; May, L.; Prasetyani, M.A.; Wahyuni, S.; Djuardi, Y.; Ariawan, I.; Wibowo, H.; et al. The Effect of Three-Monthly Albendazole Treatment on Malarial Parasitemia and Allergy: A Household-Based Cluster-Randomized, Double-Blind, Placebo-Controlled Trial. PLoS ONE 2013, 8, e57899. [Google Scholar] [CrossRef]
- Wiria, A.E.; Wammes, L.J.; Hamid, F.; Dekkers, O.M.; Prasetyani, M.A.; May, L.; Kaisar, M.M.M.; Verweij, J.J.; Tamsma, J.T.; Partono, F.; et al. Relationship between Carotid Intima Media Thickness and Helminth Infections on Flores Island, Indonesia. PLoS ONE 2013, 8, e54855. [Google Scholar] [CrossRef]
- Zhou, H.; Watanabe, C.; Ohtsuka, R. Impacts of Dietary Intake and Helminth Infection on Diversity in Growth among Schoolchildren in Rural South China: A Four-Year Longitudinal Study. Am. J. Hum. Biol. 2007, 19, 96–106. [Google Scholar] [CrossRef]
- Zavala, G.A.; Doak, C.M.; Portrait, F.; Seidell, J.C.; García, O.P.; Rosado, J.L.; Jarquín, T.; Polman, K.; Campos-Ponce, M. Are Intestinal Parasites Associated with Obesity in Mexican Children and Adolescents? Parasitol. Int. 2019, 71, 126–131. [Google Scholar] [CrossRef]
- Wasilewska, J.; Kaczmarski, M.G.; Sawicka-Zukowska, M.; Tomaszewska, B.; Majewska, A.; Plewa, K.; Ołdak, E.; Debkowska, K. Analysis of Clinical Symptoms and Selected Hematological Indices in Hospitalized Children with Ascaris Lumbricoides Infection from the Northeastern Region of Poland. Wiad. Parazytol. 2011, 57, 43–51. [Google Scholar]
- Kinung’hi, S.M.; Mazigo, H.D.; Dunne, D.W.; Kepha, S.; Kaatano, G.; Kishamawe, C.; Ndokeji, S.; Angelo, T.; Nuwaha, F. Coinfection of Intestinal Schistosomiasis and Malaria and Association with Haemoglobin Levels and Nutritional Status in School Children in Mara Region, Northwestern Tanzania: A Cross-Sectional Exploratory Study. BMC Res. Notes 2017, 10, 583. [Google Scholar] [CrossRef]
- Grimes, J.E.T.; Tadesse, G.; Gardiner, I.A.; Yard, E.; Wuletaw, Y.; Templeton, M.R.; Harrison, W.E.; Drake, L.J. Sanitation, Hookworm, Anemia, Stunting, and Wasting in Primary School Children in Southern Ethiopia: Baseline Results from a Study in 30 Schools. PLoS Negl. Trop. Dis. 2017, 11, e0005948. [Google Scholar] [CrossRef]
- Welch, V.A.; Ghogomu, E.; Hossain, A.; Awasthi, S.; Bhutta, Z.A.; Cumberbatch, C.; Fletcher, R.; McGowan, J.; Krishnaratne, S.; Kristjansson, E.; et al. Mass Deworming to Improve Developmental Health and Wellbeing of Children in Low-Income and Middle-Income Countries: A Systematic Review and Network Meta-Analysis. Lancet Glob. Health 2017, 5, e40–e50. [Google Scholar] [CrossRef]
- Kadakia, R.; Josefson, J. The Relationship of Insulin-Like Growth Factor 2 to Fetal Growth and Adiposity. Horm. Res. Paediatr. 2016, 85, 75–82. [Google Scholar] [CrossRef]
- Sørensen, K.; Juul, A. BMI Percentile-for-Age Overestimates Adiposity in Early Compared with Late Maturing Pubertal Children. Eur. J. Endocrinol. 2015, 173, 227–235. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).