Associations of Serum Magnesium with Brain Morphology and Subclinical Cerebrovascular Disease: The Atherosclerosis Risk in Communities-Neurocognitive Study
Abstract
1. Introduction
2. Materials and Methods
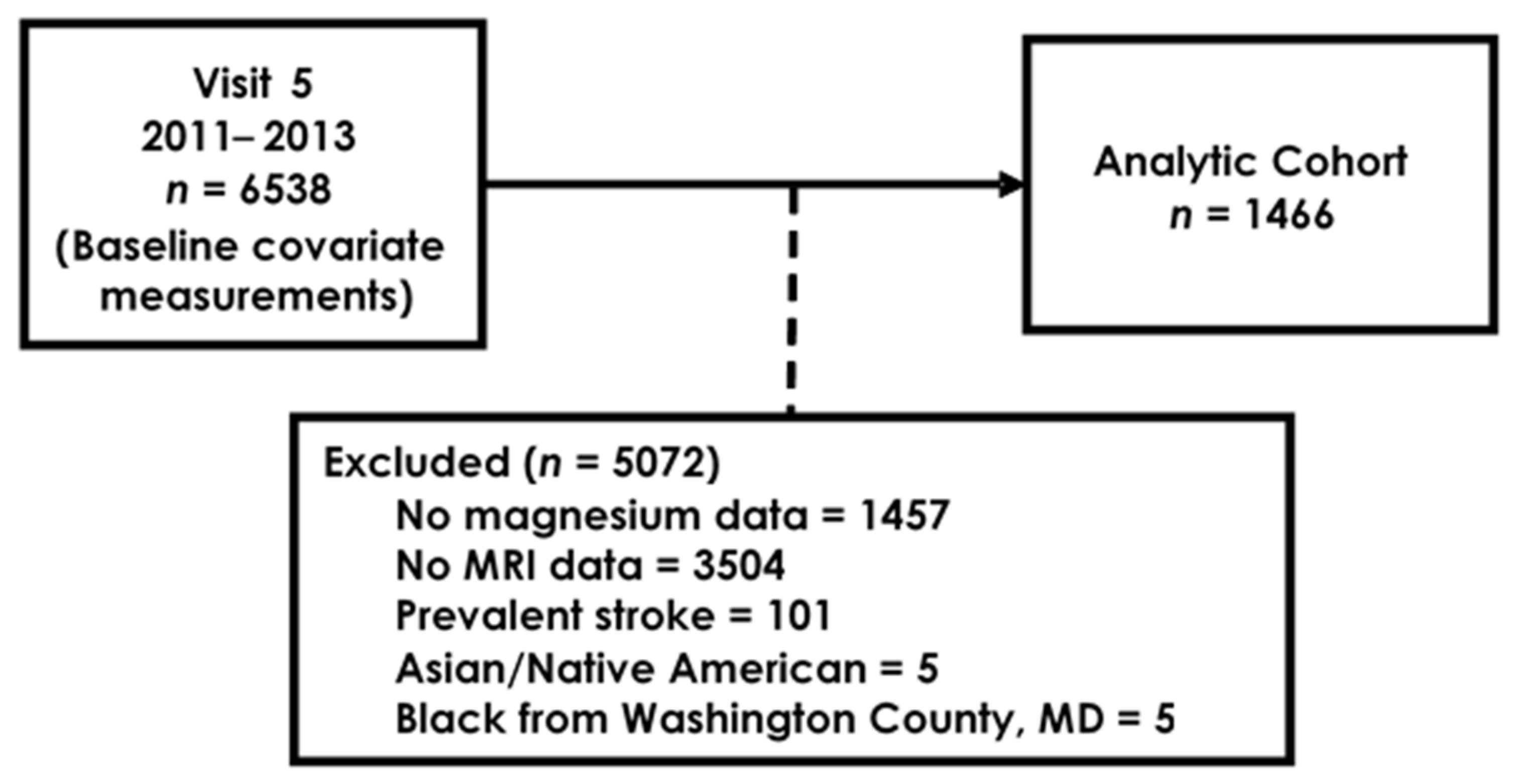
2.1. Study Population
2.2. Brain Imaging
2.3. Serum Magnesium
2.4. Covariates
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alam, A.B.; Lutsey, P.L.; Gottesman, R.F.; Tin, A.; Alonso, A. Low Serum Magnesium is Associated with Incident Dementia in the ARIC-NCS Cohort. Nutrients 2020, 12, 3074. [Google Scholar] [CrossRef] [PubMed]
- Kieboom, B.C.T.; Licher, S.; Wolters, F.J.; Ikram, M.K.; Hoorn, E.J.; Zietse, R.; Stricker, B.H. Serum magnesium is associated with the risk of dementia. Neurology 2017, 89, 1716–1722. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Yu, J.; Liu, Y.; Huang, X.; Abumaria, N.; Zhu, Y.; Huang, X.; Xiong, W.; Ren, C.; Liu, X.-G.; et al. Elevation of brain magnesium prevents synaptic loss and reverses cognitive deficits in Alzheimer’s disease mouse model. Mol. Brain 2014, 7, 65. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Huang, X.; Zhang, L.; Han, F.; Pang, K.L.; Li, X.; Shen, J.Y. Magnesium boosts the memory restorative effect of environmental enrichment in Alzheimer’s disease mice. CNS Neurosci. Ther. 2018, 24, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Flink, E.B. Magnesium deficiency. Etiology and clinical spectrum. Acta Med. Scand Suppl. 1981, 647, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Rayssiguier, Y. Role of magnesium and potassium in the pathogenesis of arteriosclerosis. Magnesium 1984, 3, 226–238. [Google Scholar] [PubMed]
- Shechter, M.; Merz, C.N.; Rude, R.K.; Paul Labrador, M.J.; Meisel, S.R.; Shah, P.K.; Kaul, S. Low intracellular magnesium levels promote platelet-dependent thrombosis in patients with coronary artery disease. Am. Heart J. 2000, 140, 212–218. [Google Scholar] [CrossRef]
- Gottesman, R.F.; Albert, M.S.; Alonso, A.; Coker, L.H.; Coresh, J.; Davis, S.M.; Deal, J.A.; McKhann, G.M.; Mosley, T.H.; Sharrett, A.R.; et al. Associations Between Midlife Vascular Risk Factors and 25-Year Incident Dementia in the Atherosclerosis Risk in Communities (ARIC) Cohort. JAMA Neurol. 2017, 74, 1246–1254. [Google Scholar] [CrossRef]
- Gragossian, A.; Bashir, K.; Friede, R. Hypomagnesemia; StatPearls: Treasure Island, FL, USA, 2021. [Google Scholar]
- Pham, P.C.; Pham, P.A.; Pham, S.V.; Pham, P.T.; Pham, P.M.; Pham, P.T. Hypomagnesemia: A clinical perspective. Int. J. Nephrol. Renov. Dis. 2014, 7, 219–230. [Google Scholar] [CrossRef]
- Maier, J.A.; Bernardini, D.; Rayssiguier, Y.; Mazur, A. High concentrations of magnesium modulate vascular endothelial cell behaviour in vitro. Biochim. Biophys. Acta 2004, 1689, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Zipfel, G.J.; Babcock, D.J.; Lee, J.M.; Choi, D.W. Neuronal apoptosis after CNS injury: The roles of glutamate and calcium. J. Neurotrauma 2000, 17, 857–869. [Google Scholar] [CrossRef]
- Larsson, S.C.; Traylor, M.; Burgess, S.; Boncoraglio, G.B.; Jern, C.; Michaelsson, K.; Markus, H.; MEGASTROKE Project Of The International Stroke Genetics Consortium. Serum magnesium and calcium levels in relation to ischemic stroke: Mendelian randomization study. Neurology 2019, 92, e944–e950. [Google Scholar] [CrossRef]
- Feng, P.; Niu, X.; Hu, J.; Zhou, M.; Liang, H.; Zhang, Y.; Tong, W.; Xu, T. Relationship of serum magnesium concentration to risk of short-term outcome of acute ischemic stroke. Blood Press. 2013, 22, 297–301. [Google Scholar] [CrossRef] [PubMed]
- Amighi, J.; Sabeti, S.; Schlager, O.; Mlekusch, W.; Exner, M.; Lalouschek, W.; Ahmadi, R.; Minar, E.; Schillinger, M. Low serum magnesium predicts neurological events in patients with advanced atherosclerosis. Stroke 2004, 35, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.D.; Folsom, A.R.; Coresh, J.; Sharrett, A.R.; Couper, D.; Wagenknecht, L.E.; Mosley, T.H., Jr.; Ballantyne, C.M.; Boerwinkle, E.A.; Rosamond, W.D.; et al. The ARIC (Atherosclerosis Risk in Communities) Study: JACC Focus Seminar 3/8. J. Am. Coll. Cardiol. 2021, 77, 2939–2959. [Google Scholar] [CrossRef] [PubMed]
- Knopman, D.S.; Gottesman, R.F.; Sharrett, A.R.; Wruck, L.M.; Windham, B.G.; Coker, L.; Schneider, A.L.; Hengrui, S.; Alonso, A.; Coresh, J.; et al. Mild Cognitive Impairment and Dementia Prevalence: The Atherosclerosis Risk in Communities Neurocognitive Study (ARIC-NCS). Alzheimers Dement. 2016, 2, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Knopman, D.S.; Griswold, M.E.; Lirette, S.T.; Gottesman, R.F.; Kantarci, K.; Sharrett, A.R.; Jack, C.R., Jr.; Graff-Radford, J.; Schneider, A.L.; Windham, B.G.; et al. Vascular imaging abnormalities and cognition: Mediation by cortical volume in nondemented individuals: Atherosclerosis risk in communities-neurocognitive study. Stroke 2015, 46, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Fischl, B.; Salat, D.H.; Busa, E.; Albert, M.; Dieterich, M.; Haselgrove, C.; van der Kouwe, A.; Killiany, R.; Kennedy, D.; Klaveness, S.; et al. Whole brain segmentation: Automated labeling of neuroanatomical structures in the human brain. Neuron 2002, 33, 341–355. [Google Scholar] [CrossRef]
- Wardlaw, J.M.; Smith, E.; Biessels, G.J.; Cordonnier, C.; Fazekas, F.; Frayne, R.; Lindley, R.; O’Brien, J.; Barkhof, F.; Benavente, O.R.; et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013, 12, 822–838. [Google Scholar] [CrossRef]
- Alonso, A.; Rooney, M.R.; Chen, L.Y.; Norby, F.; Saenger, A.K.; Soliman, E.Z.; O’Neal, W.T.; Hootman, K.C.; Selvin, E.; Lutsey, P.L. Circulating electrolytes and the prevalence of atrial fibrillation and supraventricular ectopy: The Atherosclerosis Risk in Communities (ARIC) study. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- Newcomer, J.W.; Farber, N.B.; Olney, J.W. NMDA receptor function, memory, and brain aging. Dialogues Clin. Neurosci. 2000, 2, 219–232. [Google Scholar] [PubMed]
- De Lores Arnaiz, G.R.; Bersier, M.G. Relationship between Na+, K+-ATPase and NMDA receptor at central synapses. Curr. Protein Pept. Sci. 2014, 15, 761–777. [Google Scholar] [CrossRef] [PubMed]
- Olivares, D.; KDeshpande, V.; Shi, Y.; KLahiri, D.; HGreig, N.; TRogers, J.; Huang, X. N-methyl D-aspartate (NMDA) receptor antagonists and memantine treatment for Alzheimer’s disease, vascular dementia and Parkinson’s disease. Curr. Alzheimer Res. 2012, 9, 746–758. [Google Scholar] [CrossRef]
- Hynd, M.R.; Scott, H.L.; Dodd, P.R. Glutamate-mediated excitotoxicity and neurodegeneration in Alzheimer’s disease. Neurochem. Int. 2004, 45, 583–595. [Google Scholar] [CrossRef] [PubMed]
- Suri, S.; Mackay, C.E.; Kelly, M.E.; Germuska, M.; Tunbridge, E.M.; Frisoni, G.B.; Matthews, P.M.; Ebmeier, K.P.; Bulte, D.P.; Filippini, N. Reduced cerebrovascular reactivity in young adults carrying the APOE epsilon4 allele. Alzheimers Dement. 2015, 11, 648–657.e1. [Google Scholar] [CrossRef] [PubMed]
- Gong, H.; Takami, Y.; Amemiya, T. Ultrastructure of the optic nerve in magnesium-deficient rats. Ophthalmic Res. 2003, 35, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Shadman, J.; Sadeghian, N.; Moradi, A.; Bohlooli, S.; Panahpour, H. Magnesium sulfate protects blood-brain barrier integrity and reduces brain edema after acute ischemic stroke in rats. Metab. Brain Dis. 2019, 34, 1221–1229. [Google Scholar] [CrossRef] [PubMed]
- Dalal, P.J.; Muller, W.A.; Sullivan, D.P. Endothelial Cell Calcium Signaling during Barrier Function and Inflammation. Am. J. Pathol. 2020, 190, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Adebamowo, S.N.; Jimenez, M.C.; Chiuve, S.E.; Spiegelman, D.; Willett, W.C.; Rexrode, K.M. Plasma magnesium and risk of ischemic stroke among women. Stroke 2014, 45, 2881–2886. [Google Scholar] [CrossRef]
- Shechter, M.; Sharir, M.; Labrador, M.J.; Forrester, J.; Silver, B.; Bairey Merz, C.N. Oral magnesium therapy improves endothelial function in patients with coronary artery disease. Circulation 2000, 102, 2353–2358. [Google Scholar] [CrossRef]
- Elin, R.J. Assessment of magnesium status. Clin. Chem. 1987, 33, 1965–1970. [Google Scholar] [CrossRef] [PubMed]
- Elin, R.J. Magnesium metabolism in health and disease. Dis. Mon. 1988, 34, 161–218. [Google Scholar] [CrossRef]
- Kusuhara, H.; Sugiyama, Y. Efflux transport systems for drugs at the blood-brain barrier and blood-cerebrospinal fluid barrier (Part 1). Drug Discov. Today. 2001, 6, 150–156. [Google Scholar] [CrossRef]
- Nischwitz, V.; Berthele, A.; Michalke, B. Speciation analysis of selected metals and determination of their total contents in paired serum and cerebrospinal fluid samples: An approach to investigate the permeability of the human blood-cerebrospinal fluid-barrier. Anal. Chim. Acta. 2008, 627, 258–269. [Google Scholar] [CrossRef] [PubMed]
- Bush, A.I. The metallobiology of Alzheimer’s disease. Trends Neurosci. 2003, 26, 207–214. [Google Scholar] [CrossRef]
- Vink, R.; McIntosh, T.K.; Demediuk, P.; Weiner, M.W.; Faden, A.I. Decline in intracellular free Mg2+ is associated with irreversible tissue injury after brain trauma. J. Biol. Chem. 1988, 263, 757–761. [Google Scholar] [CrossRef]
- Nayak, R.; Attry, S.; Ghosh, S.N. Serum Magnesium as a Marker of Neurological Outcome in Severe Traumatic Brain Injury Patients. Asian J. Neurosurg. 2018, 13, 685–688. [Google Scholar] [CrossRef] [PubMed]
- Lecrux, C.; McCabe, C.; Weir, C.J.; Gallagher, L.; Mullin, J.; Touzani, O.; Muir, K.W.; Lees, K.R.; Macrae, I.M. Effects of magnesium treatment in a model of internal capsule lesion in spontaneously hypertensive rats. Stroke 2008, 39, 448–454. [Google Scholar] [CrossRef][Green Version]
- Aslanyan, S.; Weir, C.J.; Muir, K.W.; Lees, K.R.; IMAGES Study Investigators. Magnesium for treatment of acute lacunar stroke syndromes: Further analysis of the IMAGES trial. Stroke 2007, 38, 1269–1273. [Google Scholar] [CrossRef]
- Lutsey, P.L.; Chen, L.Y.; Eaton, A.; Jaeb, M.; Rudser, K.D.; Neaton, J.D.; Alonso, A. A Pilot Randomized Trial of Oral Magnesium Supplementation on Supraventricular Arrhythmias. Nutrients 2018, 10, 884. [Google Scholar] [CrossRef]
| Q1 | Q2 | Q3 | Q4 | Q5 | |
|---|---|---|---|---|---|
| Magnesium, mmol/L | <0.76 | 0.76–0.80 | 0.81–0.84 | 0.85–0.88 | >0.88 |
| N | 277 | 226 | 296 | 351 | 316 |
| Age, years | 75.3 (5.1) | 76.9 (5.1) | 76.0 (5.5) | 76.1 (5.0) | 76.7 (5.5) |
| Female, % | 71.1 | 58.4 | 56.1 | 55.3 | 60.8 |
| Black, % | 39.0 | 36.3 | 28.7 | 23.9 | 19.9 |
| More than high school, % | 38.3 | 42.9 | 44.3 | 45.3 | 46.5 |
| HDL cholesterol, mg/dL | 51.3 (14.7) | 52.8 (13.4) | 53.6 (14.1) | 52.8 (13.7) | 53.5 (14.5) |
| Total cholesterol, mg/dL | 174.9 (42.0) | 176.0 (38.5) | 184.3 (42.5) | 184.3 (42.4) | 188.2 (41.7) |
| BMI, kg/m2 | 30.3 (6.3) | 29.1 (6.0) | 28.2 (5.6) | 27.6 (4.8) | 27.3 (5.0) |
| Sodium, mmol/L | 138.3 (3.2) | 138.9 (2.8) | 139.1 (2.6) | 139.1 (2.4) | 139.6 (2.5) |
| Potassium, mmol/L | 4.0 (0.4) | 4.0 (0.3) | 4.0 (0.3) | 4.1 (0.3) | 4.1 (0.4) |
| Calcium, mg/dL | 9.5 (0.4) | 9.4 (0.3) | 9.3 (0.4) | 9.4 (0.4) | 9.4 (0.4) |
| Current smoking, % | 7.2 | 5.8 | 4.7 | 4.3 | 4.1 |
| Hypertension, % | 87.7 | 82.7 | 72.3 | 67.0 | 63.9 |
| Hypertension medication, % | 81.2 | 77.4 | 63.5 | 59.0 | 55.1 |
| Diabetes, % | 56.0 | 34.5 | 26.7 | 27.4 | 19.9 |
| Coronary heart disease, % | 7.6 | 12.0 | 8.1 | 8.0 | 10.1 |
| Heart failure, % | 9.8 | 14.2 | 9.8 | 6.3 | 8.9 |
| eGFR, mL/min/1.73m2 | 66.1 (19.3) | 66.0 (17.4) | 67.8 (17.7) | 67.4 (16.5) | 62.9 (17.7) |
| C-reactive protein, mg/L | 4.7 (8.1) | 3.9 (6.7) | 3.8 (5.4) | 3.4 (4.9) | 3.4 (6.5) |
| APOE ɛ4 allele, % | 26.4 | 31.0 | 30.1 | 29.6 | 28.5 |
| Markers of subclinical cerebrovascular disease | |||||
| Cortical infarcts, % | 9.8 | 10.2 | 8.8 | 9.4 | 7.3 |
| Subcortical infarcts, % | 21.7 | 20.4 | 15.2 | 16.2 | 13.6 |
| Lacunar infarcts, % | 21.3 | 19.5 | 15.2 | 16.0 | 12.7 |
| White matter hyperintensity volume (cm3), (SD) | 17 (17) | 19 (18) | 16 (16) | 17 (16) | 19 (20) |
| Brain volume (cm3), (SD) | |||||
| Total brain | 983 (101) | 1007 (106) | 1024 (107) | 1020 (99) | 1019 (118) |
| Frontal | 145 (15) | 149 (16) | 153 (15) | 151 (14) | 151 (17) |
| Temporal | 99 (10) | 101 (12) | 103 (11) | 103 (11) | 102 (13) |
| Occipital | 39 (5) | 40 (6) | 41 (5) | 41 (5) | 41 (6) |
| Parietal | 102 (12) | 105 (12) | 107 (12) | 107 (12) | 107 (14) |
| Deep grey matter | 42 (4) | 42 (4) | 43 (4) | 43 (4) | 43 (5) |
| Q1 | Q2 | Q3 | Q4 | Q5 | 1-SD Mg | |
| Total brain volume | ||||||
| Model 1 * | Ref. | 0.11 (0.02, 0.20) | 0.19 (0.10, 0.28) | 0.15 (0.06, 0.23) | 0.21 (0.12, 0.30) | 0.06 (0.04, 0.09) |
| Model 2 ** | Ref. | 0.09 (0.00, 0.18) | 0.17 (0.08, 0.26) | 0.13 (0.05, 0.22) | 0.19 (0.10, 0.28) | 0.06 (0.03, 0.09) |
| Frontal lobe | ||||||
| Model 1 * | Ref. | 0.08 (−0.04, 0.19) | 0.21 (0.11, 0.32) | 0.11 (0.01, 0.21) | 0.19 (0.08, 0.29) | 0.06 (0.02, 0.09) |
| Model 2 ** | Ref. | 0.07 (−0.05, 0.18) | 0.19 (0.08, 0.30) | 0.09 (−0.02, 0.19) | 0.16 (0.05, 0.27) | 0.05 (0.01, 0.08) |
| Temporal lobe | ||||||
| Model 1 * | Ref. | 0.10 (0.00, 0.23) | 0.10 (−0.01, 0.20) | 0.10 (0.04, 0.20) | 0.15 (0.05, 0.25) | 0.06 (0.02, 0.09) |
| Model 2 ** | Ref. | 0.11 (0.00, 0.22) | 0.09 (−0.02, 0.20) | 0.08 (−0.02, 0.19) | 0.14 (0.03, 0.24) | 0.05 (0.02, 0.09) |
| Occipital lobe | ||||||
| Model 1 * | Ref. | 0.14 (0.01, 0.28) | 0.15 (0.02, 0.28) | 0.15 (0.03, 0.27) | 0.14 (0.02, 0.26) | 0.05 (0.01, 0.09) |
| Model 2 ** | Ref. | 0.12 (−0.02, 0.26) | 0.10 (−0.03, 0.23) | 0.11 (−0.02, 0.23) | 0.08 (−0.05, 0.21) | 0.03 (−0.01, 0.08) |
| Parietal lobe | ||||||
| Model 1 * | Ref. | 0.14 (0.03, 0.25) | 0.16 (0.05, 0.27) | 0.13 (0.03, 0.23) | 0.18 (0.08, 0.29) | 0.06 (0.03, 0.10) |
| Model 2 ** | Ref. | 0.13 (0.02, 0.25) | 0.14 (0.04, 0.25) | 0.12 (0.02, 0.23) | 0.17 (0.06, 0.28) | 0.06 (0.03, 0.10) |
| Deep grey matter | ||||||
| Model 1 * | Ref. | 0.08 (−0.05, 0.21) | 0.09 (−0.02, 0.21) | 0.12 (0.00, 0.23) | 0.14 (0.01, 0.27) | 0.05 (0.00, 0.09) |
| Model 2 ** | Ref. | 0.06 (−0.07, 0.19) | 0.08 (−0.04, 0.20) | 0.11 (−0.01, 0.23) | 0.13 (0.00, 0.26) | 0.05 (0.00, 0.09) |
| Variable | Q1 | Q2 | Q3 | Q4 | Q5 | 1-SD Mg |
|---|---|---|---|---|---|---|
| Odds Ratios (95%CI) | ||||||
| Cortical infarcts | ||||||
| Model 1 * | 1 (ref.) | 1.19 (0.60, 2.35) | 1.13 (0.59, 2.18) | 1.03 (0.55, 1.92) | 0.84 (0.43, 1.65) | 1.02 (0.84, 1.24) |
| Model 2 ** | 1 (ref.) | 1.24 (0.61, 2.53) | 1.25 (0.63, 2.49) | 1.22 (0.62, 2.41) | 1.01 (0.49, 2.07) | 1.11 (0.90, 1.37) |
| Subcortical infarcts | ||||||
| Model 1 * | 1 (ref.) | 0.89 (0.52, 1.51) | 0.47 (0.28, 0.78) | 0.56 (0.34, 0.92) | 0.42 (0.25, 0.70) | 0.75 (0.65, 0.88) |
| Model 2 ** | 1 (ref.) | 0.97 (0.56, 1.68) | 0.52 (0.30, 0.90) | 0.58 (0.34, 0.99) | 0.44 (0.25, 0.77) | 0.77 (0.65, 0.91) |
| Lacunar infarcts | ||||||
| Model 1 * | 1 (ref.) | 0.86 (0.51, 1.48) | 0.47 (0.28, 0.78) | 0.55 (0.33, 0.91) | 0.38 (0.22, 0.65) | 0.74 (0.64, 0.86) |
| Model 2 ** | 1 (ref.) | 0.94 (0.54, 1.64) | 0.52 (0.30, 0.90) | 0.57 (0.34, 0.98) | 0.40 (0.22, 0.71) | 0.76 (0.64, 0.89) |
| Beta (95%CI) | ||||||
| Ln(WMH volume) † | ||||||
| Model 1 * | Ref. | −0.01 (−0.13, 0.16) | −0.15 (−0.32, −0.01) | −0.16 (−0.32, 0.00) | −0.12 (−0.26, 0.02) | −0.05 (−0.10, −0.01) |
| Model 2 ** | Ref. | 0.03 (−0.13, 0.18) | −0.10 (−0.25, 0.04) | −0.11 (−0.27, 0.05) | −0.07 (−0.22, 0.08) | −0.03 (−0.08, 0.02) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alam, A.B.; Thomas, D.S.; Lutsey, P.L.; Shrestha, S.; Alonso, A. Associations of Serum Magnesium with Brain Morphology and Subclinical Cerebrovascular Disease: The Atherosclerosis Risk in Communities-Neurocognitive Study. Nutrients 2021, 13, 4496. https://doi.org/10.3390/nu13124496
Alam AB, Thomas DS, Lutsey PL, Shrestha S, Alonso A. Associations of Serum Magnesium with Brain Morphology and Subclinical Cerebrovascular Disease: The Atherosclerosis Risk in Communities-Neurocognitive Study. Nutrients. 2021; 13(12):4496. https://doi.org/10.3390/nu13124496
Chicago/Turabian StyleAlam, Aniqa B., DaNashia S. Thomas, Pamela L. Lutsey, Srishti Shrestha, and Alvaro Alonso. 2021. "Associations of Serum Magnesium with Brain Morphology and Subclinical Cerebrovascular Disease: The Atherosclerosis Risk in Communities-Neurocognitive Study" Nutrients 13, no. 12: 4496. https://doi.org/10.3390/nu13124496
APA StyleAlam, A. B., Thomas, D. S., Lutsey, P. L., Shrestha, S., & Alonso, A. (2021). Associations of Serum Magnesium with Brain Morphology and Subclinical Cerebrovascular Disease: The Atherosclerosis Risk in Communities-Neurocognitive Study. Nutrients, 13(12), 4496. https://doi.org/10.3390/nu13124496






