Abstract
Background: Appendiceal diverticulitis is a rare and poorly understood condition of the appendix. The diagnosis of appendiceal diverticulitis is challenging due to its rarity and a clinical presentation that often mimics other ileocecal disorders. Unlike acute appendicitis, appendiceal diverticulitis may be associated with a higher risk of perforation, increased mortality, and a potential link to neoplasms. However, further research is necessary to enhance our understanding of its epidemiology, risk factors, clinical presentation, and outcomes. Case Report: A 53-year-old male presented to the emergency department with right lower abdominal pain. On physical examination, tenderness was noted in the right lower quadrant, without rebound tenderness or muscle guarding. Laboratory tests revealed leukocytosis and elevated C-reactive protein (CRP) levels. Ultrasonographic imaging of the ileocecal region suggested acute appendicitis, leading to a decision for surgical intervention. Laparoscopic exploration revealed multiple cylindrical, red, and edematous herniations, up to 4 mm in size, on the surface of the vermiform appendix. An appendectomy was performed. Histopathological examination confirmed appendiceal diverticulitis with surrounding peridiverticulitis. The surgery and early postoperative course were uneventful. Literature review: The study included 5 retrospective studies and 30 case reports, analyzing a total of 112 patients with appendiceal diverticulitis. Of these, 65.5% were male and 34.5% were female, with a median age of 49 years (IQR: 39–59). The most commonly reported clinical findings included pain in the right iliac fossa or right lower abdominal quadrant (56.5%), nausea (18.9%), vomiting (9.8%), rebound tenderness (24.6%), fever (15.6%), leukocytosis (25.4%), and elevated C-reactive protein levels (16.4%). Diagnosis was confirmed histopathologically in 86.9% of the cases via computed tomography imaging in 4.1% and ultrasonography in 1.6%. A histopathological analysis identified five neoplasms (4.1%), including two sessile serrated adenomas, two neuroendocrine carcinoids, and one mucinous tumor. Appendectomy was the treatment of choice, with no intraoperative or postoperative complications recorded and no mortality reported. The median hospital stay was 6.8 days (IQR: 3.0–6.8). Conclusions: Appendiceal diverticulitis should be considered as a differential diagnosis in patients presenting with symptoms resembling acute appendicitis. Early diagnosis and treatment are essential to reduce morbidity and mortality. Appendectomy is a safe and effective treatment approach for appendiceal diverticulitis.
1. Introduction
The vermiform appendix, a small tubular structure attached to the cecum in the lower right quadrant of the abdomen, has been a subject of anatomical, physiological, and pathophysiological interest for centuries [1]. Among the spectrum of appendiceal pathologies, acute appendicitis stands out as the condition with the highest incidence, representing one of the most common surgical emergencies [2,3]. The clinical presentation of acute appendicitis typically includes right lower quadrant abdominal pain, fever, and leukocytosis [4]. However, the diagnosis is not always straightforward due to the variability in clinical presentation and the broad spectrum of potential differential diagnoses of acute appendicitis, which underscores the clinical challenges in accurately diagnosing appendiceal disorders [5,6].
One of the clinical entities that may mimic acute appendicitis is appendiceal diverticulitis. Studies estimate the prevalence of appendiceal diverticulosis in appendectomy specimens to range from 0.004% to 2.1% [7]. Despite being first described by the pathologist T.H. Kelynack in 1893, appendiceal diverticulitis remains a poorly understood and infrequently studied entity [8].
In this article, we present a case report of a 53-year-old male patient diagnosed with appendiceal diverticulitis whose clinical presentation resembled that of acute appendicitis. Furthermore, a review of the literature describing appendiceal diverticulitis is provided.
2. Methods
A literature search (by S.V.) on appendiceal diverticulitis was conducted on 10 December 2024 using the following four electronic databases: PubMed, Scopus, Web of Science, and ScienceDirect. Boolean logical operator expressions were used to search within the databases, as follows:
PubMED: (“appendice”[All Fields] OR “appendiceal”[All Fields] OR “appendices”[All Fields]) AND (“diverticulitis”[MeSH Terms] OR “diverticulitis”[All Fields]) AND (“appendix”[MeSH Terms] OR “appendix”[All Fields] OR “appendix s”[All Fields] OR “appendixes”[All Fields]) AND (“diverticulitis”[MeSH Terms] OR “diverticulitis”[All Fields]).
Scopus: ((appendiceal AND diverticulitis) AND (appendix)) AND (diverticulitis). AND (LIMIT-TO (SUBJAREA, “MEDI”)) AND (LIMIT-TO (DOCTYPE, “ar”)) AND (LIMIT-TO (EXACTKEYWORD, “Human”)) AND (LIMIT-TO (LANGUAGE, “English”)) AND (LIMIT-TO (SRCTYPE, “j”)).
Web of Science: TS = ((appendiceal diverticulitis) AND (appendix)) AND (diverticulitis)).
ScienceDirect: ((appendiceal diverticulitis) AND (appendix)) AND (diverticulitis). The search was restricted to papers in English and with the access type Open Access and Open Archive.
The inclusion and exclusion criteria for the selection of the studies are noted in Table 1.

Table 1.
Inclusion and exclusion criteria for the study.
A search of the databases identified 812 records. After removing 160 duplicates before the screening phase, 652 records remained. During screening, 516 records were excluded based on titles and abstracts. Subsequently, 136 full-text papers were assessed, of which 101 were excluded based on the inclusion and exclusion criteria (Table 1) due to insufficient data or because the reported outcome was either missing or irrelevant. Ultimately, 35 studies were included in the study. A flow diagram of the literature search is presented in Figure 1.
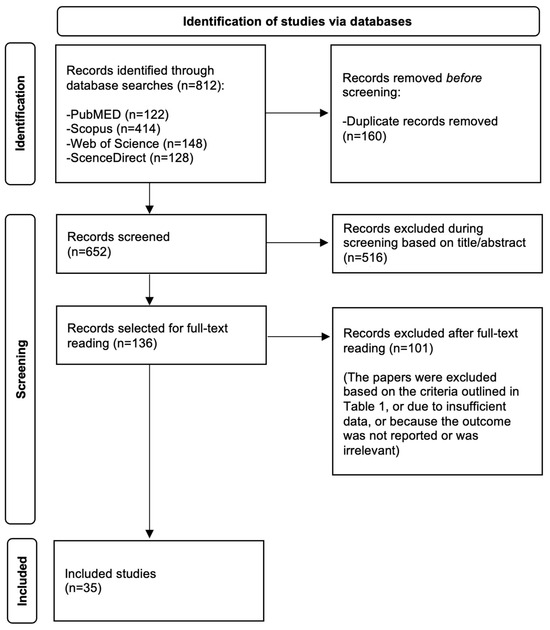
Figure 1.
A flow diagram of the literature search.
The data extraction, performed by S.V. and Z.P., focused on studies of appendiceal diverticulitis and included the following variables: the first author of the article, year of publication, study design, total number of participants, gender distribution, study period, reported symptoms, findings from physical examinations and laboratory tests, diagnostic methods, associated neoplasms, management strategies, intraoperative and postoperative complications, length of hospital stay, and mortality rates.
3. Case Report
A 53-year-old male patient presented to an emergency department with pain in the right hemiabdomen. The pain had begun earlier that morning, localized in the right lower quadrant of the abdomen, and it progressively intensified throughout the day. That morning, the patient experienced mild nausea without vomiting. Prior to this, the patient had not experienced any similar episodes or pain in this region. Furthermore, the patient reported no history of chronic illnesses or prior surgeries.
Upon admission, the patient was afebrile, and his vital signs were normal. Abdominal palpation revealed pain (8/10) without guarding, and it was most intense in the right lower quadrant of abdomen. The Blumberg sign, Rovsing sign, and obturator sign were negative. Hematological tests revealed leukocytosis (20.9 × 109/L), while biochemical tests showed elevated C-reactive protein (CRP) levels (22.4 mg/L). An ultrasound of the abdomen revealed a tubular, non-compressible structure with dorsal enhancement adjacent to the ileocecal region at the cecal base, measuring up to 25 mm in diameter, surrounded by mesenteric fat. There was no evidence of free fluid, diffuse peritonitis, or appendicolith.
The Appendicitis Inflammatory Response (AIR) score was 6, indicating a mild probability of acute appendicitis [9]. Based on the patient’s overall symptoms, physical examination findings, laboratory results, and ultrasound findings, laparoscopic exploration was indicated and carried out without further diagnostic evaluation.The laparoscopic exploration revealed cylindrical, red, and edematous herniations on the surface of the appendix (Figure 2A). An appendectomy was performed, and the appendix was sent for histopathological examination. Regarding histopathological findings, the appendix measured 6 cm in length macroscopically, with surrounding fatty tissue, having a diameter of 5.5 cm. The wall exhibited focal protrusions, up to 0.4 cm in diameter, located on the mesenteric edge of the appendix (Figure 2B).
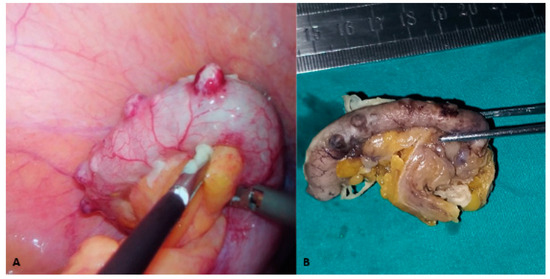
Figure 2.
Macroscopic visualizations of the vermiform appendix: (A) the intraoperative findings for the vermiform appendix, with multiple cylindrical, red, and edematous herniations on its surface; and (B) the macroscopic appearance after embedding the appendix in 4% buffered formalin, with several visible focal protrusions measuring up to 0.4 cm in diameter.
Microscopically, herniation of the mucosal and submucosal layers through a defect in the muscular layer was observed. Additionally, lymphoid follicular hyperplasia, along with an abundance of granulocytes and mononuclear cells, was identified within the wall, extending into the described diverticular protrusions (Figure 3). Overall, these findings were indicative of appendiceal diverticulitis.
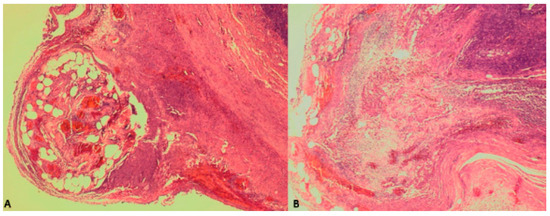
Figure 3.
The histopathological findings: (A) herniation of the mucosal and submucosal layers through a defect in the muscular layer of the appendix; and (B) localized lymphoid follicular hyperplasia and an abundance of granulocytes and mononuclear cells, collectively indicating appendiceal diverticulitis.
The surgery and early postoperative course proceeded without complications. During his hospital stay, the patient was treated with crystalloid infusions, antiemetics, and analgesics. He recovered well, tolerated oral feeding, and he had normal bowel movements. On postoperative day two, the patient was discharged home in good general and local condition. In the follow-up period of three months, the patient remained in good overall and local condition.
4. Discussion
Diverticulitis is most commonly described in the colon and, very rarely, in the appendix, as in our case [10]. Appendiceal diverticulitis can be classified as either congenital or acquired. In the congenital form, the mucosa, submucosa, and muscular layer herniate through the wall, whereas in the acquired form, only the mucosa and submucosa are involved [8]. Additionally, in the acquired form, herniations are typically more numerous, smaller (2–5 mm), and located on the mesenteric edge, whereas the congenital form is usually solitary, larger, and found on the antimesenteric edge of the appendix [11,12,13,14]. In our case, macroscopically, the diverticula measured up to 4 mm and were located on the mesenteric edge of the appendix. A histopathological examination revealed herniation of the mucosal and submucosal layers through a defect in the muscular layer, suggesting that our specimens were acquired diverticula. The acquired type is more common than the congenital type, which has an incidence of 0.014%, constituting approximately 3% of all appendiceal diverticula [7].
The classification of appendiceal diverticular disease was introduced by Phillips et al., who defined five distinct microscopic types of appendiceal diverticulitis (Table 2) [15]. Histopathologically, our specimen met the criteria for type one.

Table 2.
Types of appendiceal diverticular disease according to classification by Phillips et al. [15].
4.1. Review of the Literature
Following a review of the literature, the study included and analyzed 5 retrospective studies and 30 case reports, encompassing a total of 112 patients with appendiceal diverticulitis. Of these, 65.5% were male and 34.5% were female, with a median age of 49 years (IQR: 39–59). The most commonly reported symptoms were pain in the right iliac fossa or right lower abdominal quadrant (56.5%), nausea (18.9%), and vomiting (9.8%). Additionally, the most frequently observed physical examination and laboratory findings included rebound tenderness (24.6%), fever (15.6%), leukocytosis (25.4%), and elevated CRP levels (16.4%). The diagnosis was confirmed histopathologically in 86.9% of cases via CT imaging in 4.1% and through ultrasonography in 1.6%. A histopathological analysis identified five neoplasms (4.1%), including two sessile serrated adenomas, two neuroendocrine carcinoids, and one mucinous tumor. Table 3 presents the main characteristics and clinical findings of the patients with appendiceal diverticulitis.

Table 3.
Main characteristics and clinical findings of the patients with appendiceal diverticulitis.
The risk factors for appendiceal diverticulitis include chronic appendicitis, Hirschsprung’s disease, cystic fibrosis, an age of over 30 years, and being of male sex. In our case, the patient was older than 30 and male. Findings from case reports and retrospective studies also indicated that patients predominantly tended to be over 30 years old (Table 4). Additionally, a higher prevalence of appendiceal diverticulitis among men was reported in retrospective studies by Ergenç and Uprak, Yardimci et al., and Yamana et al. [20,36,40]. Moreover, Philips et al. provided a tabular overview of the symptomatology of appendiceal diverticulitis (Table 4), which largely aligned with the clinical presentations described in case reports presented in Table 2 [15]. Our patient also exhibited leukocytosis and elevated CRP levels, findings that were consistent with a majority of the case reports and retrospective studies on appendiceal diverticulitis (Table 3).

Table 4.
Clinical presentation of appendiceal diverticulitis.
Studies have reported a high prevalence of perforation in appendiceal diverticulitis, ranging from 30% to 70%, which is four times higher than in appendicitis [15,20,36,38,45]. This increased incidence of perforation is primarily attributed to the thin-walled diverticulum, which serves as a weak point prone to rupture. Consequently, patients with appendiceal diverticulitis face a 30-fold higher mortality risk compared to those with simple appendicitis [15,45]. In our patient, no perforation was observed.
In the context of preoperative diagnosis, studies have indicated that ultrasound and CT imaging can be useful in identifying appendiceal diverticulitis, with a diagnostic accuracy of 86% in pathologically confirmed cases [46,47,48]. Furthermore, studies suggest that, when interpreted by experienced radiologists, most cases of appendiceal diverticulitis can be differentiated from acute appendicitis using CT imaging. This differentiation is based on the characteristic appearance of inflamed diverticula, which present as small cystic protrusions within the appendix, accompanied by an increased contrast enhancement of the diverticular wall [46,47,49]. However, other research has highlighted that these radiological techniques lack specificity for this condition [49,50,51].
Several studies have described an association between the presence of appendiceal diverticulosis and neoplasms such as carcinoid tumors and mucinous adenomas [49,50,51,52,53,54]. In our case, no neoplasm was identified.
A review of the literature and an analysis of the included studies established that appendectomies were performed in 98 patients with appendiceal diverticulitis. Among these, 20 laparoscopic and 14 open appendectomies were performed, while the type of appendectomy was unspecified in the remaining cases. Furthermore, no intraoperative or postoperative complications were recorded, and no mortality was reported. The median hospital stay was 6.8 days (IQR: 3.0–6.8) (Table 5). Notably, the studies indicated that prophylactic appendectomy was recommended for all patients in whom appendiceal diverticula were identified as an intraoperative finding due to the increased risk of perforation, malignancy, and associated mortality [12,52,53].

Table 5.
Management, intraoperative and postoperative complications, length of hospital stay, and mortality in patients with appendiceal diverticulitis.
4.2. Comparison Between the Clinical and Laboratory Findings of Acute Appendicitis and Appendiceal Diverticulitis
Appendiceal diverticulitis should be considered in the differential diagnosis of patients presenting with right lower quadrant pain suggestive of acute appendicitis. The importance of this distinction lies in its clinical implications. Studies report a perforation risk of up to 70% in appendiceal diverticulitis compared to approximately 10–20% in acute appendicitis, leading to a significantly increased risk of sepsis and mortality [15,20,36,38,45]. Additionally, there is a well-documented association between appendiceal diverticulosis and neoplasms, particularly mucinous neoplasms, and carcinoid tumors, which may necessitate further surgery or postoperative surveillance [49,50,51,52,53,54,55,56,57,58]. Although imaging findings in appendiceal diverticulitis can be subtle, preoperative detection may require the use of contrast-enhanced computed tomography, which has demonstrated up to 86% accuracy in distinguishing this condition from acute appendicitis [46,47,48]. Given these considerations, identifying appendiceal diverticulitis preoperatively could lead to earlier surgical intervention, a reduced risk of complications, and more targeted postoperative follow-up, particularly in cases where histopathological findings indicate neoplastic changes.
Although appendiceal diverticulitis and acute appendicitis share similar clinical presentations, retrospective studies suggest subtle differences that may aid in diagnosis. Unlike acute appendicitis, appendiceal diverticulitis often presents with insidious pain that can persist for 2 to 14 days before hospitalization [15]. Furthermore, appendiceal diverticulitis is more frequently observed in patients over 30 years of age, whereas acute appendicitis is typically diagnosed in younger individuals [15,36,38]. Laboratory findings, such as leukocytosis and elevated CRP levels, occur in both conditions; however, appendiceal diverticulitis is more commonly associated with leukocytosis (>15 × 109/L) and significantly higher CRP levels [38,45]. Moreover, appendiceal diverticulitis is four times more likely to result in perforation, further increasing the risk of postoperative complications and mortality [15,38,45]. Table 6 summarizes the key distinguishing features between these two conditions.

Table 6.
Key distinguishing features between appendiceal diverticulitis and acute appendicitis.
4.3. Limitations
This systematic review included 35 studies, of which 6 were retrospective studies and 29 were case reports, and all were single-centered and had relatively small sample sizes. Additionally, no retrospective cohort studies, prospective studies, or randomized controlled trials on appendiceal diverticulitis were identified. Moreover, numerous studies did not report or sufficiently describe the variables of interest, further limiting the comprehensiveness of the analysis, increasing the potential for bias, and restricting the generalizability of the findings. Due to the small number of studies and limited sample sizes, a meta-analytic approach to data synthesis was not undertaken. This further constrained the possibility of quantitative synthesis, increased subjectivity, made it more challenging to identify patterns, and prevented the assessment of heterogeneity.
Further retrospective cohort studies, prospective studies, and randomized controlled trials, preferably multi-centered and with a larger sample size, are needed to provide more comprehensive and unbiased evidence on appendiceal diverticulitis. Standardizing methodologies and reporting key variables across studies would enable more thorough analyses and facilitate meta-analyses. Such research could enhance the understanding of this still insufficiently characterized pathology.
5. Conclusions
This case report highlights the incidental discovery of appendiceal diverticulitis, which clinically mimicked acute appendicitis and was successfully treated with laparoscopic appendectomy. We emphasize the importance of considering appendiceal diverticulitis as a differential diagnosis in patients presenting with symptoms suggestive of acute appendicitis. Moreover, additional research is needed to better understand the risk factors, clinical manifestations, disease progression, and optimal treatment strategies for this condition.
Author Contributions
S.V. and Z.P., conceptualization, visualization, writing—original draft preparation, editing, and literature review; N.Č., I.Š. and M.U., data collection, writing—original draft preparation, and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. Institutional Review Board permission was waived due to the fact that patient received standard treatments, and the study did not include experimental interventions for the patients.
Informed Consent Statement
The patient provided written informed consent with regard to including his case details and imaging studies.
Data Availability Statement
The data are not publicly available since they contain information that could compromise the privacy of the research participant.
Conflicts of Interest
There are no conflicts to be declared.
References
- Constantin, M.; Petrescu, L.; Mătanie, C.; Vrancianu, C.O.; Niculescu, A.-G.; Andronic, O.; Bolocan, A. The Vermiform Appendix and Its Pathologies. Cancers 2023, 15, 3872. [Google Scholar] [CrossRef] [PubMed]
- Jukić, M.; Nizeteo, P.; Matas, J.; Pogorelić, Z. Trends and Predictors of Pediatric Negative Appendectomy Rates: A Single-Centre Retrospective Study. Children 2023, 10, 887. [Google Scholar] [CrossRef] [PubMed]
- Han, H.; Letourneau, I.D.; Abate, Y.H.; Abdelmasseh, M.; Abu-Gharbieh, E.; Adane, T.D.; Ahinkorah, B.O.; Ahmad, A.; Ahmadi, A.; Ahmed, A.; et al. Trends and Levels of the Global, Regional, and National Burden of Appendicitis between 1990 and 2021: Findings from the Global Burden of Disease Study 2021. Lancet Gastroenterol. Hepatol. 2024, 9, 825–858. [Google Scholar] [CrossRef] [PubMed]
- Pogorelić, Z.; Janković Marendić, I.; Čohadžić, T.; Jukić, M. Clinical outcomes of daytime versus nighttime laparoscopic appendectomy in children. Children 2023, 10, 750. [Google Scholar] [CrossRef]
- Lamm, R.; Kumar, S.S.; Collings, A.T.; Haskins, I.N.; Abou-Setta, A.; Narula, N.; Nepal, P.; Hanna, N.M.; Athanasiadis, D.I.; Scholz, S.; et al. Diagnosis and Treatment of Appendicitis: Systematic Review and Meta-Analysis. Surg. Endosc. 2023, 37, 8933–8990. [Google Scholar] [CrossRef]
- Males, I.; Boban, Z.; Kumric, M.; Vrdoljak, J.; Berkovic, K.; Pogorelic, Z.; Bozic, J. Applying an explainable machine learning model might reduce the number of negative appendectomies in pediatric patients with a high probability of acute appendicitis. Sci. Rep. 2024, 14, 12772. [Google Scholar] [CrossRef]
- AbdullGaffar, B. Diverticulosis and Diverticulitis of the Appendix. Int. J. Surg. Pathol. 2009, 17, 231–237. [Google Scholar] [CrossRef]
- Kelynack, T.N. A Contribution to the Pathology of the Vermiform Appendix; Lewis: London, UK, 1893. [Google Scholar]
- Pogorelić, Z.; Mihanović, J.; Ninčević, S.; Lukšić, B.; Elezović Baloević, S.; Polašek, O. Validity of Appendicitis Inflammatory Response Score in Distinguishing Perforated from Non-Perforated Appendicitis in Children. Children 2021, 8, 309. [Google Scholar] [CrossRef]
- Dupre, M.P.; Jadavji, I.; Matshes, E.; Urbanski, S.J. Diverticular Disease of the Vermiform Appendix: A Diagnostic Clue to Underlying Appendiceal Neoplasm. Hum. Pathol. 2008, 39, 1823–1826. [Google Scholar] [CrossRef]
- Williams, J.M.; Adamo, D.A.; Olson, M.C. Acute Appendiceal Diverticulitis: A Case Report. Radiol. Case Rep. 2021, 16, 1072–1074. [Google Scholar] [CrossRef]
- Altieri, M.L.; Piozzi, G.N.; Salvatori, P.; Mirra, M.; Piccolo, G.; Olivari, N. Appendiceal Diverticulitis, a Rare Relevant Pathology: Presentation of a Case Report and Review of the Literature. Int. J. Surg. Case Rep. 2017, 33, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Zubieta-O’Farrill, G.; Guerra-Mora, J.R.; Gudiño-Chávez, A.; Gonzalez-Alvarado, C.; Cornejo-López, G.B.; Villanueva-Sáenz, E. Appendiceal Diverticulum Associated with Chronic Appendicitis. Int. J. Surg. Case Rep. 2014, 5, 961–963. [Google Scholar] [CrossRef] [PubMed]
- Fiordaliso, M.; De Marco, A.F.; Costantini, R. A Case of Type 2 Appendiceal Diverticulum Perforated and a Review of the Literature. Int. J. Surg. Case Rep. 2020, 77, 450–453. [Google Scholar] [CrossRef] [PubMed]
- Phillips, B.J.; Perry, C.W. Appendiceal Diverticulitis. Mayo Clin. Proc. 1999, 74, 890–892. [Google Scholar] [CrossRef]
- Abdelrahim, A.; Yusuf, Y.; Ali, O.; Abudeeb, H. Acute Diverticulitis of the Appendix. BMJ Case Rep. 2024, 17, e259552. [Google Scholar] [CrossRef]
- Cadena, M.; López, R.; Cardoso, L.; García, D.; Cabrera-Vargas, L.F.; Velásquez-Candamil, D.; Lozada Martinez, I.D. Acute Diverticulitis of the Appendix: A Case Report. Ann. Mediterr. Surg. 2023, 6, 17–22. [Google Scholar] [CrossRef]
- Laamiri, G.; Ezzine, R.; Feriani, N.; Rchidi, J.; Debbiche, A.; Hedfi, M. Appendiceal Diverticulitis: A Case Report. Clin. Case Rep. Int. 2023, 7, 1586. [Google Scholar]
- Bonomo, L.D.; Zago, M.; Quirico, C.; Ottinetti, A.; Panzera, F.; Galli, A.; Gattoni, L.; Canova, G.; Nicotera, A. Surgical Rarities: Case Report of Appendicular Diverticulitis and Literature Review. J. Surg. Case Rep. 2022, 2022, rjac319. [Google Scholar] [CrossRef]
- Ergenç, M.; Uprak, T.K. Appendiceal Diverticulitis Presenting as Acute Appendicitis and Diagnosed After Appendectomy. Cureus 2022, 14, e23050. [Google Scholar] [CrossRef]
- Elkhawaga, M.; Mundasad, B.; Hampton, J.; Alam, A.S. Appendiceal Diverticulitis Presenting as Acute Appendicitis: A Case Report. Cureus 2022, 14, e32626. [Google Scholar] [CrossRef]
- Abdulmomen, A.A.; AlZahrani, A.S.; Al Mulla, L.A.; Alaqeel, F.O. Acute Perforated Appendicitis Associated with Appendiceal Diverticulitis in a Young Man: A Case Report with Literature Review. Am. J. Case Rep. 2021, 23, e934838-1. [Google Scholar] [CrossRef] [PubMed]
- Onafowokan, O.O.; Khairat, A.; Bonatti, H.J.R. Appendiceal Diverticulitis in a Young Female Diagnosed on Pathology after Laparoscopic Appendectomy for Acute Appendicitis. Case Rep. Med. 2021, 2021, 2508956. [Google Scholar] [CrossRef] [PubMed]
- Bujold-Pitre, K.; Mailloux, O. Diverticulitis of the Appendix—Case Report and Literature Review. J. Surg. Case Rep. 2021, 2021, rjab488. [Google Scholar] [CrossRef] [PubMed]
- Memon, A.; Stoeckle, D.B. Incidental Finding of Diverticulosis of the Appendix with Sessile Serrated Adenoma. Cureus 2020, 12, e8230. [Google Scholar] [CrossRef]
- Albeeshi, M.Z.; Alwanyan, A.A.; Salim, A.A.; Albabtain, I.T. Appendiceal Diverticulitis Presenting as Acute Appendicitis Diagnosed Postoperatively. J. Surg. Case Rep. 2019, 2019, rjz332. [Google Scholar] [CrossRef]
- Hwala, S.; Aoun, C.; El Hajj, I.; Malek, A.; Saber, T.; Farhat, S.; Asmar, A.E.; Saad, J.; Khoury, M.E. Appendiceal Diverticulitis Presenting with Clinical Features of Acute Appendicitis: Case Report and Literature Review. World J. Surg. Surg. Res. 2019, 2, 1137. [Google Scholar]
- Vass, T.; Zaránd, A.; Horányi, D.; Harsányi, L. A féregnyúlvány diverticulosisa, diverticulitise. Esetismertetés És Irod. Áttekintés. Orv. Hetil. 2018, 159, 768–772. [Google Scholar] [CrossRef]
- Singh-Ranger, D.; Mangalika, M. Appendix Diverticula—A Serious Diagnosis: Case Report and Literature Review. Clin. Surg. 2018, 3, 2270. [Google Scholar]
- Ogawa, Y.; Asayama, N.; Nagata, S. Acute Gastrointestinal Bleeding from Appendiceal Diverticulitis Diagnosed Preoperatively by Combined Short-interval Computed Tomography and Colonoscopy: A Case Report. Dig. Endosc. 2018, 30, 392–394. [Google Scholar] [CrossRef]
- Lourenço, R.B.; Pinho, M.D.C.; Schraibman, V.; Macedo, A.L.D.V.; Francisco Neto, M.J.; Funari, M.B.D.G. Perforated Diverticulitis of the Appendix: Ultrasonographic Diagnosis. Einstein São Paulo 2011, 9, 75–77. [Google Scholar] [CrossRef]
- Fernández Gómez-Cruzado, L.; Prieto Calvo, M.; Pérez González, C.; Larrea Oleaga, J. Diverticulitis of the Appendix as Debut of Appendicular Cystadenoma and Carcinoid Tumor. Rev. Esp. Enferm. Dig. 2017, 109, 145–146. [Google Scholar] [PubMed]
- El-Saady, A. Diverticulitis of the Appendix: Is It Clinically Significant? Egypt. J. Surg. 2016, 35, 150. [Google Scholar] [CrossRef]
- Lange, J.; Bachmann, R.; Königsrainer, A.; Zdichavsky, M. Appendiceal Diverticulitis Shortly after a Performed Laparoscopic Sigma Resection. J. Surg. Case Rep. 2015, 2015, rjv086. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, M.; Chawla, A.; Chokkappan, K.; Liu, H. Diverticulitis of the Appendix, a Distinctive Entity: Preoperative Diagnosis by Computed Tomography. Emerg. Radiol. 2015, 22, 609–612. [Google Scholar] [CrossRef]
- Yardimci, A.H.; Bektas, C.T.; Pasaoglu, E.; Kinaci, E.; Ozer, C.; Sevinc, M.M.; Mahmutoglu, A.S.; Kilickesmez, O. Retrospective Study of 24 Cases of Acute Appendiceal Diverticulitis: CT Findings and Pathological Correlations. Jpn. J. Radiol. 2017, 35, 225–232. [Google Scholar] [CrossRef]
- Patil, A.Y.; Levine, M.S.; Grujic, E.; Goren, R.A. Clinical and CT Findings in Appendiceal Diverticulitis. Clin. Imaging 2014, 38, 350–352. [Google Scholar] [CrossRef]
- Sohn, T.J.; Chang, Y.S.; Kang, J.H.; Kim, D.H.; Lee, T.S.; Han, J.K.; Kim, S.H.; Hong, Y.O. Clinical Characteristics of Acute Appendiceal Diverticulitis. J. Korean Surg. Soc. 2013, 84, 33. [Google Scholar] [CrossRef]
- Heffernan, D.S.; Saqib, N.; Terry, M. A Case of Appendiceal Diverticulitis, and a Review of the Literature. Ir. J. Med. Sci. 2009, 178, 519–521. [Google Scholar] [CrossRef]
- Yamana, I.; Kawamoto, S.; Inada, K.; Nagao, S.; Yoshida, T.; Yamashita, Y. Clinical Characteristics of 12 Cases of Appendiceal Diverticulitis: A Comparison with 378 Cases of Acute Appendicitis. Surg. Today 2012, 42, 363–367. [Google Scholar] [CrossRef]
- Käser, S.A.; Willi, N.; Maurer, C.A. Prevalence and Clinical Implications of Diverticulosis of the Vermiform Appendix. J. Int. Med. Res. 2013, 41, 1350–1356. [Google Scholar] [CrossRef]
- Kubota, T. Sonographic Findings of Acute Appendiceal Diverticulitis. World J. Gastroenterol. 2006, 12, 4104. [Google Scholar] [CrossRef] [PubMed]
- Lanthaler, M.; Nehoda, H. It Is Not Always Appendicitis. Wien. Klin. Wochenschr. 2004, 116, 51–54. [Google Scholar] [CrossRef] [PubMed]
- Iki, K.; Echigo, M.; Nogami, A.; Iwamoto, S.; Takeo, T.; Tsunoda, T.; Eto, T. Preoperative Diagnosis of Acute Appendiceal Diverticulitis by Ultrasonography. Surgery 2001, 130, 87–89. [Google Scholar] [CrossRef] [PubMed]
- Lipton, S.; Estrin, J.; Glasser, I. Diverticular Disease of the Appendix. Surg. Gynecol. Obstet. 1989, 168, 13–16. [Google Scholar]
- Osada, H.; Ohno, H.; Saiga, K.; Watanabe, W.; Okada, T.; Honda, N. Appendiceal Diverticulitis: Multidetector CT Features. Jpn. J. Radiol. 2012, 30, 242–248. [Google Scholar] [CrossRef]
- Lee, K.H.; Lee, H.S.; Park, S.H.; Bajpai, V.; Choi, Y.S.; Kang, S.-B.; Kim, K.J.; Kim, Y.H. Appendiceal Diverticulitis: Diagnosis and Differentiation From Usual Acute Appendicitis Using Computed Tomography. J. Comput. Assist. Tomogr. 2007, 31, 763–769. [Google Scholar] [CrossRef]
- Motos Micó, J.; Ferrer Márquez, M.; Berenguel Ibáñez, M.D.M.; Belda Lozano, R.; Moreno Serrano, A. Appendiceal Diverticulitis: A Possible Diagnosis in Acute Abdomen. Cirugía Esp. Engl. Ed. 2015, 93, e49–e51. [Google Scholar] [CrossRef]
- Nitta, N.; Takahashi, M.; Furukawa, A.; Murata, K.; Mori, M.; Fukushima, M. MR Imaging of the Normal Appendix and Acute Appendicitis. J. Magn. Reson. Imaging 2005, 21, 156–165. [Google Scholar] [CrossRef]
- Jaboury, I.A. Diverticulitis of the vermiform appendix. ANZ J. Surg. 2007, 77, 803–804. [Google Scholar] [CrossRef]
- Simpson, J.; Lobo, D.N.; Spiller, R.C.; Scholefield, J.H. Diverticular Abscess of the Appendix: Report of a Case and Review of the Literature. Dis. Colon Rectum 2003, 46, 832–834. [Google Scholar] [CrossRef]
- Pai, R.K.; Beck, A.H.; Norton, J.A.; Longacre, T.A. Appendiceal Mucinous Neoplasms: Clinicopathologic Study of 116 Cases With Analysis of Factors Predicting Recurrence. Am. J. Surg. Pathol. 2009, 33, 1425–1439. [Google Scholar] [CrossRef] [PubMed]
- Yantiss, R.K.; Shia, J.; Klimstra, D.S.; Hahn, H.P.; Odze, R.D.; Misdraji, J. Prognostic Significance of Localized Extra-Appendiceal Mucin Deposition in Appendiceal Mucinous Neoplasms. Am. J. Surg. Pathol. 2009, 33, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Lamps, L.W.; Gray, G.F.; Dilday, B.R.; Washington, M.K. The Coexistence of Low-Grade Mucinous Neoplasms of the Appendix and Appendiceal Diverticula: A Possible Role in the Pathogenesis of Pseudomyxoma Peritonei. Mod. Pathol. 2000, 13, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Stockl, T.; Ross, J.S.; Walter, O.; Dresser, K.; Lee, H. Appendiceal Mucosal Schwann Cell Proliferation: A Putative Histologic Marker of Appendiceal Diverticular Disease. Int. J. Surg. Pathol. 2013, 21, 603–609. [Google Scholar] [CrossRef]
- Marcacuzco, A.A.; Manrique, A.; Calvo, J.; Loinaz, C.; Justo, I.; Caso, O.; Cambra, F.; Fakih, N.; Sanabria, R.; Jimenez-Romero, L.C. Clinical Implications of Diverticular Disease of the Appendix. Experience Over the Past 10 Years. Cirugía Esp. Engl. Ed. 2016, 94, 44–47. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Ercegović, V.; Bašković, M.; Jukić, M.; Karaman, I.; Mrklić, I. Incidence and Management of Appendiceal Neuroendocrine Tumors in Pediatric Population: A Bicentric Experience with 6285 Appendectomies. Children 2023, 10, 1899. [Google Scholar] [CrossRef]
- Tintor, G.; Jukić, M.; Šupe-Domić, D.; Jerončić, A.; Pogorelić, Z. Diagnostic Accuracy of Leucine-Rich α-2-Glycoprotein 1 as a Non-Invasive Salivary Biomarker in Pediatric Appendicitis. Int. J. Mol. Sci. 2023, 24, 6043. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).