Abstract
This study assessed the association between multimorbidity and mortality from COVID-19 in the Middle East and North Africa region, where such data are scarce. We conducted a cross-sectional study using data of all cases with COVID-19 reported to the Ministry of Public Health of Qatar from March to September 2020. Data on pre-existing comorbidities were collected using a questionnaire and multimorbidity was defined as having at least two comorbidities. Proportions of deaths were compared by comorbidity and multimorbidity status and multivariable logistic regression analyses were carried out. A total of 92,426 participants with a mean age of 37.0 years (SD 11.0) were included. Mortality due to COVID-19 was associated with gastrointestinal diseases (aOR 3.1, 95% CI 1.16–8.30), respiratory diseases (aOR 2.9, 95% CI 1.57–5.26), neurological diseases (aOR 2.6, 95% CI 1.19–5.54), diabetes (aOR 1.8, 95% CI 1.24–2.61), and CVD (aOR 1.5, 95% CI 1.03–2.22). COVID-19 mortality was strongly associated with increasing multimorbidity; one comorbidity (aOR 2.0, 95% CI 1.28–3.12), two comorbidities (aOR 2.8, 95% CI 1.79–4.38), three comorbidities (aOR 6.0, 95% 3.34–10.86) and four or more comorbidities (aOR 4.15, 95% 1.3–12.88). This study demonstrates a strong association between COVID-19 mortality and multimorbidity in Qatar.
1. Introduction
Mortality from the COVID-19 pandemic has fallen due to the effects of an unprecedented global vaccination campaign [1] and rising population immunity due to previous infection [2]. However, despite this fall in mortality, some individuals are still at high risk of death from COVID-19. Evidence from several countries suggests that individuals with pre-existing comorbidities are at a greater risk of death from COVID-19 [3,4].
Some of the pre-existing comorbidities that have been associated with a higher risk of death from COVID-19 are malignancies, chronic renal disease (CKDs), some respiratory diseases, including chronic obstructive pulmonary disease (COPD), diabetes mellitus (DM), and cardiovascular diseases (CVDs), such as heart failure or coronary artery disease [5]. The Middle East and North Africa (MENA) region consists of large multicultural expatriate populations and is among the regions with high proportions of people with chronic diseases such as diabetes [6]. Notably, many countries in this region, with some exceptions, have good health systems which seem to have fared well during the COVID-19 pandemic [7]. In this region, not many studies have been carried out on the association between comorbidities and mortality from COVID-19.
Multimorbidity is defined as having two or more chronic illnesses [8]. While chronic diseases are linked to a higher risk of hospitalization and death, emerging research suggests that the presence of several comorbidities simultaneously can further increase the risk of mortality [9]. In one study, individuals with three or more long-term illnesses had an increased risk of death than those who did not present with any [10]. Notably, studies on multimorbidity and mortality from COVID-19 are scarce in the MENA region.
Given the low number of deaths from COVID-19 and the relatively good health systems in countries such as Qatar, it is still not known whether the relative contribution of pre-existing comorbidities and multimorbidity to COVID-19 mortality is similar to that observed in other settings. Thus, our study aims to determine the association between multimorbidity and COVID-19 mortality in Qatar.
2. Materials and Methods
2.1. Study Design and Participants
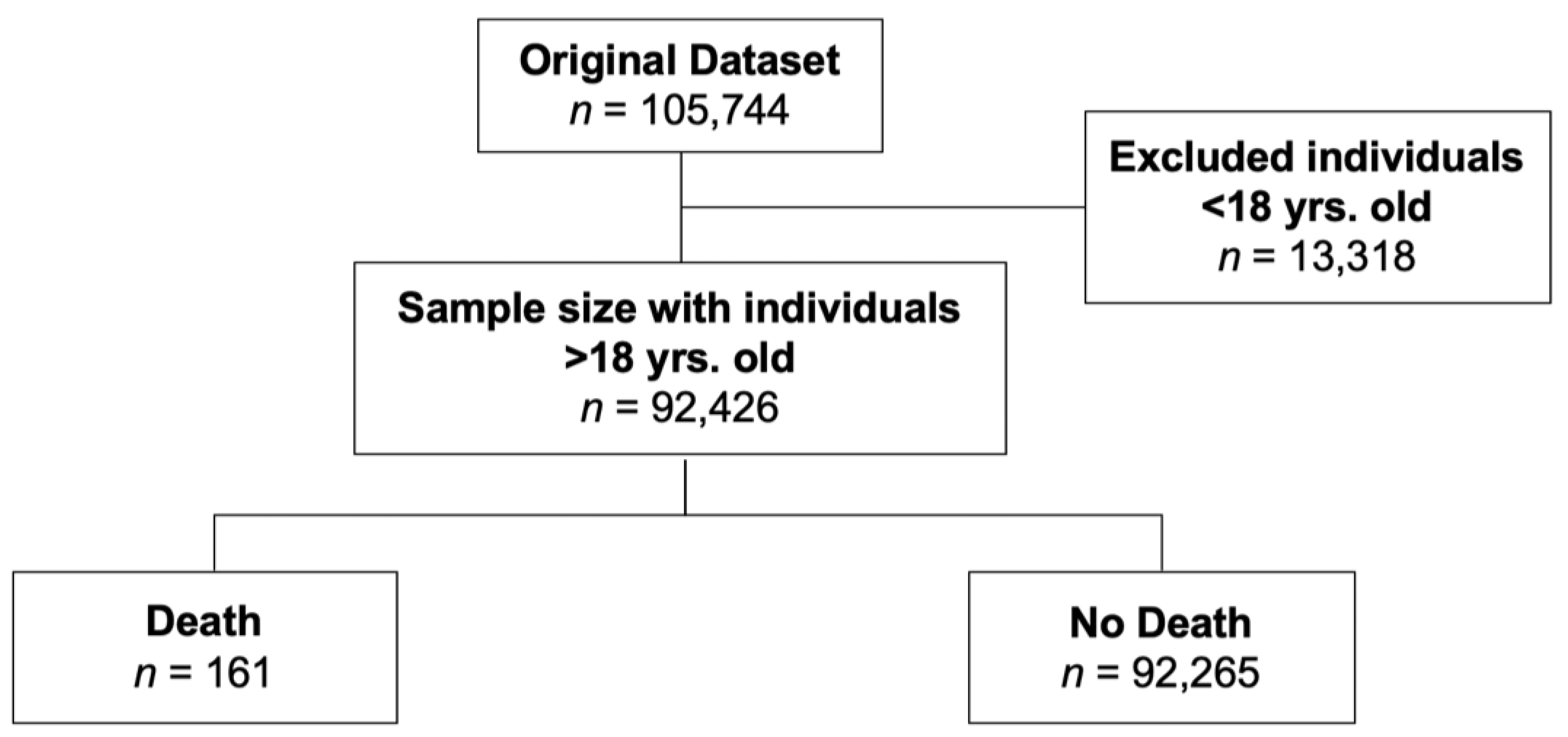
This study is a cross-sectional study of all individuals with confirmed COVID-19 in the state of Qatar in the period March 2020 to September 2020. The data were collected by the Ministry of Public Health (MoPH) in Qatar. During the aforementioned period, 105,744 individuals were confirmed to have COVID-19 using real-time reverse transcriptase-polymerase reaction assay (RT-PCR) of pharyngeal swabs and/or nasal swabs. In this study, we excluded 13,318 individuals who were below the age of 18 years because of the low prevalence of pre-existing comorbidities and given that no deaths were reported in this age group during the study period. After the exclusion, 92,426 participants were included, out of which 161 died.
2.2. Data Collection
Data were collected through a case investigation form, developed by the MOPH based on the WHO protocol on COVID-19 cases, version 2 [11]. All cases that were reported to primary health care centers (PHCCs) or hospitals were reported to the MoPH. Data on mortality was ascertained from MOPH records, and data on comorbidities were self-reported from telephone calls, due to non-contact COVID-19 disease control protocols at that time. Other data collected were demographic and clinical data such as nationality, age, gender, date of birth, symptoms, comorbidities, and mortality status. Comorbidities were categorized according to the latest International Classification of Diseases 11th Revision (ICD-11)—Version: 09/2020. However, because of the known association between diabetes and COVID-19 mortality, diabetes data were collected separately from other endocrine diseases. The other categories of comorbidities were neurological diseases, respiratory diseases, gastrointestinal diseases, diabetes, cancer, thyroid diseases, renal diseases, cardiovascular diseases, and dyslipidemia. Supplementary Materials Table S1 shows the diseases and the category corresponding to each disease. Nationality data were collected and then individuals were classified per the 6 WHO regions (African Region, Region of the Americas, South-East Asia Region, European Region, Eastern Mediterranean Region (EMR), and Western Pacific Region), and we combined South-East Asia and Western Pacific into one category and named it “Asia Pacific”. The number of comorbidities that the patient had was converted into a comorbidity score, which was then categorized. Multimorbidity was defined as having at least two pre-existing comorbidities and measured as having two, three, or at least four pre-existing comorbidities as very few people had more than 4 comorbidities. Proportions of deaths were compared by comorbidity status and multivariable logistic regression analyses were carried out adjusting for confounders.
2.3. Exposure and Outcome Variables
The exposures of interest were pre-existing comorbidities, and the main outcome was death from COVID-19.
2.4. Statistical Analysis
We described categorical data using frequencies and percentages and reported mean age and its standard deviation since age was normally distributed. Pearson X2 tests were used to compare categorical data by death status and a t-test was used for age.
Multiple variable logistic regression was used to obtain adjusted odds ratios (OR) and their 95% confidence intervals (95% CI) to assess the strength of the association between comorbidities (predictor variables) and COVID-19 mortality (binary outcome), and the same done for assessing the association between mortality and multimorbidity (categorized as 2 comorbidities, 3 comorbidities, and ≥4 comorbidities). All the comorbidities were included in one model and adjusted for age and gender. The exact p-value was reported and used to indicate the degree of evidence against the model hypothesis (OR = 1) at the current sample size. We used STATA 16.0. for all analysis.
2.5. Ethics
This study received ethical approval and waiver of informed consent from the Institutional Review Board (IRB) (QU-IRB 1413-E/20) at Qatar University (QU) and permission from the MoPH (ERC-826-3-2020). This study was conducted according to the ethical guidelines of the Declaration of Helsinki [12].
The study is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline (Supplementary Materials Table S2).
3. Results
3.1. Characteristics of Included Participants
Out of the total of 105,744 cases during the study period, 92,426 participants were included after the exclusion of those below 18 years of age. (Figure 1). There were 161 deaths from COVID-19.
Figure 1.
Flow chart showing how participants were included.
As expected, the mean age of the participants who died was significantly older than that of those who were alive during the study period (65.4 years (SD 14.5) vs. 37.0 (SD 11.0), respectively, p < 0.001). Approximately 80% of the cohort were males, reflecting the gender distribution in the country, with no statistical difference in the distribution of females and males between participants who died and those who were alive during the study period (Table 1). Approximately 72% of the individuals who died had at least one comorbidity, compared to 13.6% of controls (Table 1).

Table 1.
Description of the cohort.
3.2. Comparison of Proportions of Comorbidities between Individuals Who Died and Those Who Did Not Die from COVID-19
In general, individuals who died were more likely to have comorbidities, compared to those who were alive, as shown in Table 2.

Table 2.
Association between pre-existing comorbidities and mortality from COVID-19—multivariable-logistic regression.
This pattern was also true when the number of comorbidities was compared between those who died and those who were alive at the end of the study period. Individuals who died were more likely to have at least one co-morbidity (26.1% vs. 8.9%, respectively, p < 0.001). The cases who died were also more likely to have multimorbidity. For example, the proportion of individuals with two comorbidities was higher in those who died compared to those who did not (29.8% vs. 3.8%, respectively, p < 0.001). The percentage of individuals with three comorbidities was also higher in those who died compared to those who did not (12.4% vs. 0.8%, respectively, p < 0.001). Similarly, the proportion of individuals with four or more comorbidities was higher in those who died compared to those who did not (2.5% vs. 0.1%, respectively, p < 0.001) (Table 3).

Table 3.
Association between Number of comorbidities and COVID-19 mortality—Multivariable logistic regression.
3.3. Association between Comorbidities and Mortality from COVID-19–Multivariable Logistic Regression
After multivariable logistic regression, mortality due to COVID-19 was strongly associated with gastrointestinal diseases (aOR 3.1, 95% CI 1.16–8.30, p = 0.024), respiratory diseases (aOR 2.9, 95% CI 1.57–5.26, p 0.001), neurological diseases (aOR 2.6, 95% CI 1.19–5.54, p = 0.016), diabetes (aOR 1.8, 95% CI 1.24–2.61, p 0.002), and CVD (aOR 1.5, 95% CI 1.03–2.22, p = 0.036). Renal diseases (aOR 2.1, 95% CI 0.56–8.02, p = 0.270), thyroid diseases (aOR 2.1, 95% CI 0.85–5.41, p = 0.106), and cancer (aOR 2.6, 95% CI 0.76–8.66, p = 0.130) were associated with increased odds of mortality but with weak evidence against the null hypothesis (Table 2).
3.4. Association between Multimorbidity and Mortality from COVID-19–Multivariable Logistic Regression
There was a strong association between multimorbidity and odds of mortality (Table 3). Mortality from COVID-19 was strongly associated with multimorbidity, with increased odds of death observed as the number of multimorbidity increased. Having any comorbidity increased the odds of mortality two-fold (aOR 2.0, 95% CI 1.28–3.12, p = 0.002), any two comorbidities increased the odds of mortality by almost three-fold (aOR 2.8, 95% CI 1.79–4.38, p < 0.001), any three comorbidities increased the odds of mortality by six-fold (aOR 6.0, 95% 3.34–10.86, p < 0.001) and having four or more comorbidities increased the odds of mortality by four times (aOR 4.15, 95% 1.3–12.88, p = 0.014).
4. Discussion
Our findings confirmed the association between comorbidities and COVID-19 mortality in a region where data have been scarce on this topic. Further, this study showed that multimorbidity was associated with higher odds of mortality and demonstrated a graded increase in the odds of mortality as the number of comorbidities increased in an individual.
While our findings affirmed the associations between mortality from COVID-19 comorbidities, such as cardiovascular diseases [13,14,15], thyroid diseases [16], renal diseases [15,16], and diabetes [15,17], our research adds to the body of knowledge for the MENA region. Further, our findings suggest that neurological diseases are a risk factor for COVID-19 mortality. Deleterious autosomal recessive diseases have been reported to be the leading consequence of consanguinity in South Asia and the Middle East regions and the main cause of disabilities in Arab countries [17,18]. Individuals with various muscular dystrophies, including myotonic dystrophy, and those who have ventilatory muscle weakness or cardiomyopathy have been found to have a higher risk of severe COVID-19, in one study [19]. It is, therefore, possible that neurological diseases lead to several complications of which muscular atrophy is the most prominent, which will lead to acute respiratory failure and eventually death [20]. Moreover, our findings imply diabetes as one of the major contributing comorbidities to COVID-19 mortality given the high population prevalence of diabetes in Qatar and the region [21]. More protection and closer monitoring for people with neurological comorbidities and diabetes may therefore be warranted.
We found that individuals with multiple comorbidities were highly at risk of mortality from COVID-19. Our findings of a strong and graded increase in the odds of mortality with increasing multimorbidity are similar to findings reported elsewhere [22]. Another study also showed that patients who are diagnosed with three or more long-term illnesses had an increased risk of death than those who did not present with any. Together, these findings suggest the need to consider the individual comorbidities when triaging the risk of mortality from COVID-19 and factor in the total comorbidity burden per individual. This shows that individuals with multimorbidity would need to be prioritized and closely monitored and will benefit from increased protections such as booster doses if they get COVID-19.
Notably, the highest age mortality was in the age group of 60–69 years. This could likely have been due to the combined effect of comorbidities and age since both are associated with a higher risk of death from COVID-19, with older age perhaps playing a larger role [22,23]. There is also the possibility that there could have been a higher force of infection (higher proportion of cases) in this age group, but this could not be verified as population denominators in this age group were not available at the time of this study.
A limitation of this study is that the data on comorbidities were self-reported and collected using telephonic calls, to avoid COVID-19 spreading from confirmed cases. Measured data on confounders, such as body mass index (BMI), were therefore not available. We were also not able to categorize cancer using validated tools, such as the CORONET Predictive Score, or to measure the Charlson comorbidity index, due to the way our data were collected. Therefore, the adjustment for confounders may not have been optimal. A strength of this study is the rigorous design, the total sample size, and the analysis which enabled us to minimize the effect of confounding variables. This research, due to the multinational nature of Qatar’s population, may apply to different populations, especially in Asia.
5. Conclusions
This study affirms the strong association between preexisting comorbidities with COVID-19 mortality and demonstrates a very strong and graded increase in the odds of mortality with increasing multimorbidity in Qatar.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/microbiolres14010023/s1, Table S1: Comorbidities’ categories and the respective diseases within each category; Table S2: STROBE Checklist.
Author Contributions
Conceptualization, K.A., B.E., M.E., M.K., R.T., F.A., A.A., M.E.H., T.C. and M.M.E.; Data Curation, K.A., B.E., M.E., M.K., R.T., F.A., A.A., M.E.H., S.S.A., J.A., M.A.H.S., M.H.M.A.-S., H.E.A.-R., D.B., O.A.H.M., E.F. and M.H.J.A.-T.; Formal Analysis, K.A., B.E., M.E., M.K., T.C. and M.M.E.; Methodology, K.A., B.E., M.E., M.K., R.T., F.A., A.A., M.E.H., T.C. and M.M.E.; Project Management, K.A.; Supervision, K.A., T.C. and M.M.E.; Validation, T.C. and M.M.E.; Visualization, K.A., B.E., M.E. and M.K.; Writing-original draft, K.A., B.E., M.E., M.K., R.T., F.A., A.A., M.E.H., T.C. and M.M.E.; Writing-review & editing, K.A., B.E., M.E., M.K., R.T., F.A., A.A., M.E.H., S.S.A., J.A., M.A.H.S., M.H.M.A.-S., H.E.A.-R., D.B., O.A.H.M., E.F., M.H.J.A.-T., T.C. and M.M.E. All authors have read and agreed to the published version of the manuscript.
Funding
Funding was received from the Ministry of Public Health (MoPH) in Qatar for the publish of this research.
Data Availability Statement
Restrictions apply to the availability of these data as it was obtained from the ministry of public health in Qatar and are not publicly available due to the maintenance of individuals’ confidentiality.
Acknowledgments
We acknowledge methodological and statistical support from the Department of Population Medicine, College of Medicine, from Qatar University. We are also grateful to the Ministry of Public Health (MoPH), Qatar for collecting the data used in this study.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2), COVID-19 (coronavirus disease outbreak), COPD (chronic obstructive pulmonary disease), DM (diabetes mellitus), CVDs (cardiovascular diseases), ICU (intensive care unit), UCEC (uterine corpus endometrial carcinoma), ACE2 (angiotensin-converting enzyme), TMPRSS2 (transmembrane protease serine 2), IBD (inflammatory bowel disease), ALD (alcoholic liver disease), HCC (hepatocellular carcinoma), MoPH (ministry of public health of Qatar), RT-PCR (real-time reverse transcriptase-polymerase reaction assay), PHCC (Primary Health Care Center), DAGs (directed acyclic graphs), ICD-11 (international classification of diseases 11th revision), WHO (World Health Organization), EMR (Eastern Mediterranean Region), OR (odds ratios), CI (confidence intervals), IRB (institutional review board), QU (Qatar University), STROBE (strengthening the reporting of observational studies in epidemiology), ACE2 (angiotensin-converting enzyme 2), BMI (body mass index).
References
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Beltekian, D.; Roser, M. Coronavirus Pandemic (COVID-19). Our World in Data, 2020. Available online: https://ourworldindata.org/covid-cases (accessed on 28 August 2022).
- Chivese, T.; Matizanadzo, J.T.; Musa, O.A.H.; Hindy, G.; Furuya-Kanamori, L.; Islam, N.; Al-Shebly, R.; Shalaby, R.; Habibullah, M.; Al-Marwani, T.A.; et al. The prevalence of adaptive immunity to COVID-19 and reinfection after recovery—A comprehensive systematic review and meta-analysis. Pathog. Glob. Health 2022, 116, 269–281. [Google Scholar] [CrossRef] [PubMed]
- Adab, P.; Haroon, S.; O’Hara, E.M.; Jordan, E.R. Comorbidities and Covid-19. BMJ 2022, 377, o1431. [Google Scholar] [CrossRef] [PubMed]
- Dessie, Z.G.; Zewotir, T. Mortality-related risk factors of COVID-19: A systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect. Dis. 2021, 21, 855. [Google Scholar] [CrossRef] [PubMed]
- National Center for Immunization and Respiratory Diseases (NCIRD). CDC COVID-19 Science Briefs; Centers for Disease Control and Prevention (US): Atlanta, GA, USA, 2020. [Google Scholar]
- Wang, H.; Li, N.; Chivese, T.; Werfalli, M.; Sun, H.; Yuen, L.; Hoegfeldt, C.A.; Powe, C.E.; Immanuel, J.; Karuranga, S.; et al. IDF Diabetes Atlas: Estimation of Global and Regional Gestational Diabetes Mellitus Prevalence for 2021 by International Association of Diabetes in Pregnancy Study Group’s Criteria. Diabetes Res. Clin. Pract. 2021, 183, 109050. [Google Scholar] [CrossRef] [PubMed]
- Fang, X.; Li, S.; Yu, H.; Wang, P.; Zhang, Y.; Chen, Z.; Li, Y.; Cheng, L.; Li, W.; Jia, H.; et al. Epidemiological, comorbidity factors with severity and prognosis of COVID-19: A systematic review and meta-analysis. Aging 2020, 12, 12493–12503. [Google Scholar] [CrossRef] [PubMed]
- Prazeres, F.; Castro, L.; Teixeira, A. Sociodemographic and Clinical Determinants of Multimorbidity of Underlying Conditions That Increase the Risk of Severe Illness from COVID-19 in Chronic Adult Individuals. BioMed 2022, 2, 94–103. [Google Scholar] [CrossRef]
- Kansara, N.; Nandapurkar, A.B.; Maniyar, R.; Yadav, A.K. Prediction of mortality by age and multi-morbidities among confirmed COVID-19 patients: Secondary analysis of surveillance data in Pune, Maharashtra, India. Indian J. Public Health 2021, 65, 64–66. [Google Scholar] [PubMed]
- Monterrubio-Flores, E.; Ramírez-Villalobos, M.D.; Espinosa-Montero, J.; Hernandez, B.; Barquera, S.; Villalobos-Daniel, V.E.; Campos-Nonato, I. Characterizing a two-pronged epidemic in Mexico of non-communicable diseases and SARS-Cov-2: Factors associated with increased case-fatality rates. Int. J. Epidemiol. 2021, 50, 430–445. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The First Few X Cases and Contacts (FFX) Investigation Protocol for Coronavirus Disease 2019 (COVID-19), 23 February 2020; WHO/2019-nCoV/FFXprotocol/2020.3; World Health Organization: Geneva, Switzerland, 2020; Available online: https://apps.who.int/iris/handle/10665/332023 (accessed on 28 August 2022).
- World Health Organization. Serum and Red Blood Cell Folate Concentrations for Assessing Folate Status in Populations Vitamin and Mineral Nutrition Information System; World Health Organization: Geneva, Switzerland. Available online: http://apps.who.int/iris/bitstream/10665/162114/1/WHO_NMH_NHD_EPG_15.01.pdf?ua=1 (accessed on 28 August 2022).
- Nishiga, M.; Wang, D.W.; Han, Y.; Lewis, D.B.; Wu, J.C. COVID-19 and cardiovascular disease: From basic mechanisms to clinical perspectives. Nat. Rev. Cardiol. 2020, 17, 543–558. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Lin, F.; Tu, W.; Zhang, J.; Choudhry, A.A.; Ahmed, O.; Cheng, J.; Cui, Y.; Liu, B.; Dai, M.; et al. Thyroid dysfunction may be associated with poor outcomes in patients with COVID-19. Mol. Cell. Endocrinol. 2021, 521, 111097. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Arora, A.; Sharma, P.; Anikhindi, S.A.; Bansal, N.; Singla, V.; Khare, S.; Srivastava, A. Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 535–545. [Google Scholar] [CrossRef] [PubMed]
- Oyelade, T.; Alqahtani, J.; Canciani, G. Prognosis of COVID-19 in Patients with Liver and Kidney Diseases: An Early Systematic Review and Meta-Analysis. Trop. Med. Infect. Dis. 2020, 5, 80. [Google Scholar] [CrossRef] [PubMed]
- Pranata, R.; Huang, I.; Lim, M.A.; Wahjoepramono, E.J.; July, J. Impact of cerebrovascular and cardiovascular diseases on mortality and severity of COVID-19–systematic review, meta-analysis, and meta-regression. J. Stroke Cerebrovasc. Dis. 2020, 29, 104949. [Google Scholar] [CrossRef] [PubMed]
- Al-Gazali, L.; Hamamy, H.; Al-Arrayad, S. Genetic disorders in the Arab world. BMJ 2006, 333, 831–834. [Google Scholar] [CrossRef] [PubMed]
- Guidon, A.C.; Amato, A.A. COVID-19 and neuromuscular disorders. Neurology 2020, 94, 959–969. [Google Scholar] [CrossRef] [PubMed]
- Hutchinson, D.; Whyte, K. Neuromuscular disease and respiratory failure. Pract. Neurol. 2008, 8, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Majeed, A.; El-Sayed, A.A.; Khoja, T.; Alshamsan, R.; Millett, C.; Rawaf, S. Diabetes in the Middle-East and North Africa: An update. Diabetes Res. Clin. Pract. 2014, 103, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Tian, W.; Jiang, W.; Yao, J.; Nicholson, C.J.; Li, R.; Sigurslid, H.; Wooster, L.; Rotter, J.I.; Guo, X.; Malhotra, R. Predictors of mortality in hospitalized COVID-19 patients: A systematic review and meta-analysis. J. Med. Virol. 2020, 92, 1875–1883. [Google Scholar] [CrossRef] [PubMed]
- Bonanad, C.; García-Blas, S.; Tarazona-Santabalbina, F.; Sanchis, J.; Bertomeu-González, V.; Fácila, L.; Ariza, A.; Núñez, J.; Cordero, A. The Effect of Age on Mortality in Patients With COVID-19: A Meta-Analysis With 611,583 Subjects. J. Am. Med. Dir. Assoc. 2020, 21, 915–918. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).