Abstract
The COVID-19 outbreak was first reported in 2019, causing massive morbidity and mortality. The majority of the COVID-19 patients survived and developed Post-COVID-19 Syndrome (PC19S) of varying severity. Currently, the diagnosis of PC19S is achieved through history and symptomatology that cannot be explained by an alternative diagnosis. However, the heavy reliance on subjective reporting is prone to reporting errors. Besides, there is no unified diagnostic assessment tool to classify the clinical severity of patients. This leads to significant difficulties when managing patients in terms of public resource utilization, clinical progression monitorization and rehabilitation plan formulation. This narrative review aims to review current evidence of diagnosis based on triple assessment: clinical symptomatology, biochemical analysis and imaging evidence. Further assessment tools can be developed based on triple assessment to monitor patient’s clinical progression, prognosis and intervals of monitoring. It also highlights the high-risk features of patients for closer and earlier monitoring. Rehabilitation programs and related clinical trials are evaluated; however, most of them focus on cardiorespiratory fitness and psychiatric presentations such as anxiety and depression. Further research is required to establish an objective and comprehensive assessment tool to facilitate clinical management and rehabilitation plans.
1. Introduction
The COVID-19 outbreak was first reported in 2019, causing massive morbidity and mortality. Though various vaccine trials have shown good safety and efficacy for different populations, vaccination does not completely prevent infection and re-infection [1,2]. Though the majority of infected patients recover, a significant proportion develop Post-COVID-19 Syndrome (PC19S, aka Long-COVID-19 Condition) of varying severity. In October 2021, the WHO published the definition of Post-COVID-19 Syndrome (PC19S) as patients with a history of probable or confirmed SARS-CoV-2 infection 3 months from the onset of COVID-19 with at least 2 months of new-onset symptoms which cannot be explained by an alternative diagnosis. Currently, there are 12 documented domains of PC19S symptoms to define its diagnosis. However, the heavy reliance on subjective reporting is prone to reporting errors. Thus, an objective diagnostic tool set is required to define the diagnosis and facilitate future treatment.
Over 40–70% of COVID-19 survivors may develop PC19S [3,4]. This has a significant impact on their quality of life, mental health and employment. The effect of PC19S may last years or longer [5]. The impact of PC19S is enormous for patients, the healthcare system and economic development [6,7]. Multidisciplinary care aimed at identifying high-risk individuals and supporting long-term rehabilitation to maximize functional capacity is required [8]. Currently, the NHS has established a three-tier service model to provide targeted individualized interventions with a specific set of outcome measures outlined in the COVID-19 Yorkshire Rehabilitation Scale [9]. Similar clinical questionnaires are under research [10]. However, there is no unified assessment tool to diagnose and quantify the severity of PC19S, leading to consequences of underdiagnosis or overdiagnosis. Medical practitioners know little about its diagnosis and rehabilitation pathways [11,12]. Thus, standardized assessment and treatment tools should be provided according to resource availability in local healthcare systems to maximally safeguard the best interests of COVID-19 survivors.
Some survivors develop subclinical multi-organ impairment, which warrants further screening to guide its management [13]. Figure 1 shows the proposed pathogenesis from previous authors [8,14]. This review aims to define possible assessment tools for the diagnosis and monitoring of the progression in terms of clinical, radiological and biochemical parameters. It also defines high-risk populations for frequent follow-up, follow-up schedules and rehabilitation details for patients with PC19S.
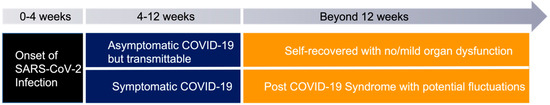
Figure 1.
Proposed Pathogenesis model of PC19S [8,14].
2. Current Diagnosis of PC19S
The WHO definition of PC19S is based on symptom duration, onset and category of symptoms. Figure 2 shows the most common PC19S symptoms. Various clinical questionnaires have been proposed with reference to the incidence of clinical presentations [14]. The initial questionnaire is used to screen the severity of PC19S. The change of symptoms score is used for patients with mild symptoms for outpatient monitoring [15,16]. The initial screening tool, “the long covid Symptom and Impact Tool”, was constructed and validated in France, with a passing score of 30 for self-reported, acceptable symptom control state (95% CI, 28–33) [16]. Non-hospitalized patients are more likely to be associated with neuropsychiatric symptoms [17], while hospitalized patients have more respiratory symptoms (p < 0.05) [18]. Three months is set as the duration necessary for diagnosis, since over 70% of COVID-19 survivors experienced symptom resolution by 12 weeks [19].
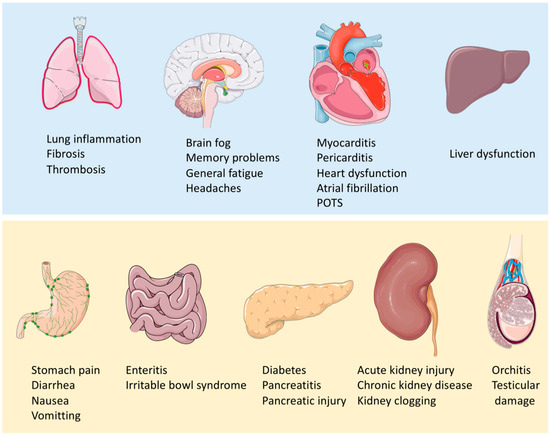
Figure 2.
Common clinical presentations of PC19S. (Parts of the Figure was drawn and adapted using pictures from Servier Medical Art (http://smart.servier.com/) (accessed on 10 July 2022), licensed under a Creative Commons Attribution 3.0 Unported License (https://creativecommons.org/licenses/by/3.0/) (accessed on 4 February 2023).
Another validated clinical assessment tool in the UK is the “Post-Acute (Long) COVID-19 Quality of Life (PAC-19QoL) Instrument”. It identified 35/44 quality of life indicators for those with PC19S (p < 0.05) [20]. Several other clinical tools are used for the assessment of PC19S, such as the Short-Form-36 Health Survey (SF-36), EQ-5D-5L Assessment Tool and Health-Related Quality of Life Scale (HRQoL) [21].
It may be difficult to accurately define PC19S as different assessment schemes emerge. Exertional intolerance and dyspnea with preserved or deteriorated lung function have both been reported [22]. It is important to divide the diagnostic/monitoring pathway into asymptomatic or symptomatic pathways first, followed by a triple assessment if available (clinical, radiological and biochemical). Table 1 shows an updated review summary of PC19S on various body systems.

Table 1.
Summary of PC19S effect on various systems [8], an updated review.
3. Imaging Diagnosis of PC19S
Persistent lung injury has been reported in PC19S due to persistent shedding of the virus, the prothrombotic state and the ongoing inflammatory state [66]. Possible image findings include ground glass opacification, consolidation, crazy paving, vacuole sign, pulmonary nodules, lobar pneumonia, tractional bronchiectasis, vascular thickening, lung cavitations and fibrosis, predominantly at the peripheral/subpleural locations [67]. The CT severity score can be used to calculate the extent of pathological involvement in each of the 5 lobes [68,69]:
- Score of 0: no involvement;
- Score of 1: <5% involvement;
- Score of 2: 5–25% involvement;
- Score of 3: 26–50% involvement;
- Score of 4: 51–75% involvement; and
- Score of 5: >75% involvement.
The sum of each individual lobar score is added to give a global CT score to quantify the severity and predict the probability of PC19S [70]. A cut-off value of 7 is proposed with a sensitivity of 95.9%, specificity of 96%, positive predictive value of 95.92%, negative predictive value of 96% and accuracy of 95.96% [67].
4. Biochemical Diagnosis of PC19S
Understanding the inflammatory, immunological and metabolic activity biomarkers is required for the detailed assessment of PC19S [71].
Post-COVID postural tachycardia syndrome is one of the documented PC19S complications. Its diagnosis is based on clinical symptoms and an excessive orthostatic tachycardia (with a heart rate increase of >30 beats per minute in adults and 40 beats per minute in adolescents) within 10 min of upright posture in the absence of orthostatic hypotension and associated symptoms of orthostatic intolerance for at least 3 months [72,73].
In view of the various clinical manifestations of PC19S on the neurological system, some studies have investigated the effect of biomarkers on the central nervous system, such as myelin oligodendrocyte glycoprotein (MOG) and CCL-11 [74]. In patients with a neurological presentation of PC19S, reactive microglia with astrocyte reactivity, alteration of hippocampal neurogenesis, myelinated axons and oligodendrocytes have been reported in literature [75,76,77,78,79,80,81]. In view of this, several mechanisms have been proposed:
- (1)
- Cytokine-associated immune dysregulation disrupts myelin hemostasis and plasticity, impairing hippocampal neurogenesis with neurotoxic astrocyte reactivity. This results in an impairment of neural circuit function and cognition.
- (2)
- Anti-neural antibodies cause autoimmune encephalitis leading to immune-mediated brain injury
- (3)
- Neuroinvasive infection
- (4)
- COVID-19 triggers reactivation of latent virus infection, such as EBV, which can further trigger inflammation cascades and impairment of brain function
- (5)
- Neurovascular dysfunction of the blood–brain barrier leading to proinflammatory molecules and thrombosis. Neural inflammation accounts for the disseminated brain injury
- (6)
- Hypoxia and metabolic disturbances cause central nervous system injury
Other biochemical research on PC19S have been in progress. Persistent clotting protein pathology has been reported with increased levels of antiplasmin [82]. Microclots with inflammatory molecules have been detected in plasma samples of patients with acute COVID-19 infection and PC19S. Consideration of anticlotting therapy to support fibrinolytic system dysfunction can be considered in clinically symptomatic survivors [31]. Anticoagulation can be effective in improving outcomes as persistent systemic vascular inflammation and dysfunction by thrombosis are key factors driving various complications in PC19S [83].
Several biomarkers have been identified as having prognostic significance. PC19S is associated with long-term inflammation, thus the persistence of interleukin-6 (IL-6) and tumor necrosis factor-alpha have been shown to be of prognostic value [84,85]. The magnitude of early CD4+ T cell immune responses correlate with the severity of initial infection; thus, it can be used as a tracker of PC19S severity [85]. Inflammatory dysbiosis of the oral microbiome is associated with the duration of symptoms of PC19S [86]. Thyroid dysfunction has been observed in PC19S patients. The presence of anti-thyroid peroxidase (Anti-TPO) is a positive prognostic finding for symptom resolution in earlier stage [87].
Detection of superantigens is a proposed hypothesis requiring validation. Persistent viral RNA shedding by superantigens could overstimulate the anti-virus immune response and induce negative feedback loops [88]. Immunologically, reduced CD4+ and CD8+ memory cells are associated with PC19S. Persistent T-cell perturbations up to several months are common in mild COVID-19 survivors [89]. Immunomodulation by mesenchymal cells could be a treatment option for these patients due to their immunomodulatory and regenerative properties [90].
Biochemically, an elevated taurine and reduced glutamine/glutamate ratio in plasma samples (p < 0.05) have been found in patients with PC19S, indicating possible liver and muscle damage and the related energy-demanding process of recovery and tissue repair [40]. Asymptomatic patients during follow-up display a spectrum of multiple biochemical pathophysiology. The metabolic phenotyping approach for multisystem functional assessment has been recommended [91].
The association between gut microbiota disruption and PC19S severity is under investigation [71].
5. Prognosis of PC19S Tools
Ongoing research on PC19S prognosis has aroused interest in the field. Table 2 shows a summary of useful investigation tools for patients with PC19S. A Bangladesh cohort study showed a persistence of PC19S symptoms at 9 months ranging from 16.1% to 50% [92,93]. The mean duration of PC19S symptoms was 21.8 weeks and the length of PC19S was projected with a structural equation based on age, gender, smoking and prior functional limitations [92]. Table 3 shows a summary of the clinical assessment of the prognosis and severity of PC19S in various studies in terms of triple assessment: clinical, biochemical and radiological.

Table 2.
Useful investigation tools for patients with Post-COVID-19 Syndrome [8].

Table 3.
Summary of PC19S clinical, imaging and biochemical markers for diagnosis and prognosis in various studies (Toolbox).
6. Interval of Monitoring
Figure 3 shows the clinical follow-up schedule suggested according to the summary of existing evidence. Table 4 shows the persistence of the most common symptoms across different time periods after initial COVID-19 infection. The order of first ranked symptoms varies in different studies but the top 3 ranked problems are similar: ongoing respiratory problems, persistent fatigue and cognitive deficit (brain fog) [3,102,127]. The initial follow-up schedule should be set at 28 days, 3 months and 9 months. Further follow-up sessions can be arranged if there is a progression of symptoms or abnormal imaging or laboratory findings. Screening should be done based on clinical suspicion. COVID-19-associated acute kidney injury is associated with a good prognosis: over 70% can live without renal replacement therapy and over half with complete resolution of acute kidney injury [128].
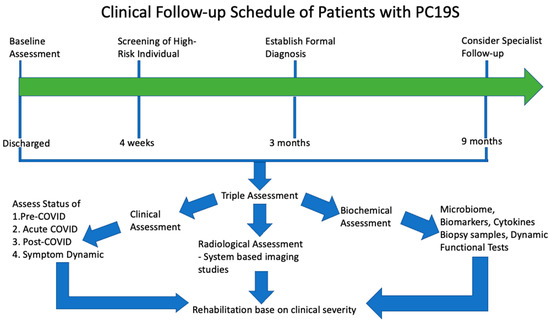
Figure 3.
Clinical Follow-up Schedule of PC19S. Patients are recommended to have an initial clinical assessment at the time of discharge and follow-up for at least 3 months for persistent symptoms/patients with high-risk factors. Patients with persistence/progression of symptoms beyond 9 months should consider specialist referral as most symptoms disappear by 9 months. Triple assessment is recommended based on clinical, radiological and biochemical assessment for a comprehensive review. Rehabilitation programs are provided to patients, stratified by clinical severity to optimize resource usage and rehabilitation progress [8].

Table 4.
Prevalence of PC19S symptoms at different follow-up periods [3,102,127,129].
Hospital admission (odd ratio 2.28) and persistence of symptoms at day 28 (odd ratio 2.21) and month 9 (odd ratio 5.16) are independent predictors of suboptimal physical health and psychological stress [130]. However, another 9-month follow-up study showed no association between acute COVID-19 infection severity state and the number of PC19S symptoms and cognitive dysfunction [131].
There is no increase in inflammatory markers in blood tests at the subacute stage, and no association of the symptoms to biochemical parameters [132]. COVID-19-related persistent symptoms improve over time, but neurological symptoms last longer than other symptoms [98].
A 9-month grace period should be seen as a cut-off interval for top-up rehabilitation services since most PC19S symptoms should decrease after 9 months, while fatigue and somnipathy can persist for over a year [133].
7. Features of High-Risk Individuals for Screening
Some common features of high-risk individuals include a history of hospitalization, concomitant active cancer, medical comorbidities, use of supplemental oxygen and ventilatory support [5,67,134,135,136]. Review of clinical profiles before discharge and planning of rehabilitation schedules are recommended for hospitalized patients. These should include: patients aged over 50 (odd ratio 8.5, 95% CI 1.9–38, p = 0.01), longer duration of hospital stay (odd ratio 5.5, 95% CI 1.5–21, p = 0.01), presence of acute respiratory distress syndrome during the acute phase (odd ratio 13, 95% CI 3.3–55, p < 0.001), non-invasive ventilation (odd ratio 6.3, 95% CI 1.3–30, p = 0.02) and initial CT score more than 18 (odd ratio 4.2, 95% CI 1.2–14, p = 0.02) [137]. One multicenter prospective cohort study shows a higher propensity of PC19S in patients with previous lung disease and tobacco consumption [136].
PC19S has also been reported in non-hospitalized, asymptomatic patients [138]. However, continued interval monitoring for PC19S should be adopted before aggressive treatment since the longitudinal study in Faroe Islands showed symptom resolution took several months [139].
Another more recent study has shown that the number of initial symptoms is more related to PC19S than the severity of the acute infection [140].
Physicians in charge of pediatric populations should also look out for PC19S as it has been widely reported in various literature in children who demonstrate similar symptoms as adults, with an estimated incidence of over 40% [141,142,143]. Various clinical presentations have been documented such as myocarditis, postural tachycardia syndrome, mast cell disorder and mast cell activation [41,144,145,146]. Patients with these complications should be screened and followed-up every 4 weeks or sooner for close monitoring.
PC19S is common among people living with HIV and moderate to severe acute COVID-19 illness. Over 20% reported PC19S at a median follow-up of 6 months, with the most prevalent symptoms being asthenia (80%), shortness of breath (50%) and recurrent headache (25%) [147]. Integrated assessment of PC19S and anti-retroviral therapy clinical visits should be considered [148].
8. Persistent and Clinically Significant Symptoms to Address
Most PC19S symptoms improve over time, particularly after 9 months. A significant proportion of patients reported persistent neuropsychiatric symptoms, which indicates a bad prognosis [133]. Brain fog has been reported frequently as a notable symptom of PC19S. There is an association of brain fog with abnormal FDG-PET findings, highlighted by a hypometabolic cingulate cortex [115]. FDG-PET imaging may also show hypometabolism in the parahippocampal gyrus, cerebellum, brainstem, olfactory gyrus, temporal lobe and thalamus, which corresponds to patients with persistent anosmia/ageusia, fatigue and vascular uptake (uncorrected p < 0.005) [149,150]. This corresponds to cerebral hypoxia, leading to compromised neuronal cell energy metabolism and, eventually, mitochondrial dysfunction [151]. The hypoxic condition favors persistent viral shedding and compromised cognitive change, which induces brain fog and related behavioral changes [151]. The UK Biobank MRI brain cohort study showed a greater reduction in grey matter thickness and tissue damage in the orbitofrontal cortex, parahippocampal gyrus and primary olfactory area at 4 months after infection, leading to multiple clinical presentations such as fatigue, olfactory dysfunction and brain fog [152]. Similar functional changes have been validated whole brain functional analyses performed at 11 months [103]. Another long-term follow-up study of dynamic brain changes in patients who recovered from COVID-19 without neurological manifestation showed there is a co-existence of recoverable and long-term unrecoverable changes after 10 months [153]. Cognitive decline in some patients may spontaneously improve over time [154].
Clinically, the assessment can be done using various scales such as the personality assessment inventory to assess somatic preoccupation and depression [116]. In patients with persistent neurocognitive symptoms, ANA titer elevations should be checked since autoimmunity could be a cofactor in the etiology of PC19S [155]. In patients with baseline motor dysfunction, PC19S with worsening motor symptoms requires a high dosage of levodopa for disease management [156].
9. Rehabilitation Program
The goals of rehabilitation should be individualized based on cardiorespiratory fitness, muscle function, bone and joint health, functional capacity and quality of life [157]. In terms of rehabilitation progress, clinically significant pulmonary function improvement may take a longer time, while muscle strength, walking capacity, sit-to-stand performance and quality of life usually improve earlier [158]. The initial lower physical composite score from the Short-Form Survey (SF-12) is associated with a prolonged recovery [99]. Figure 4 shows a suggested rehabilitation framework for patients with PC19S, and Table 5 shows clinicians’ global research progress related to rehabilitation programs for PC19S.
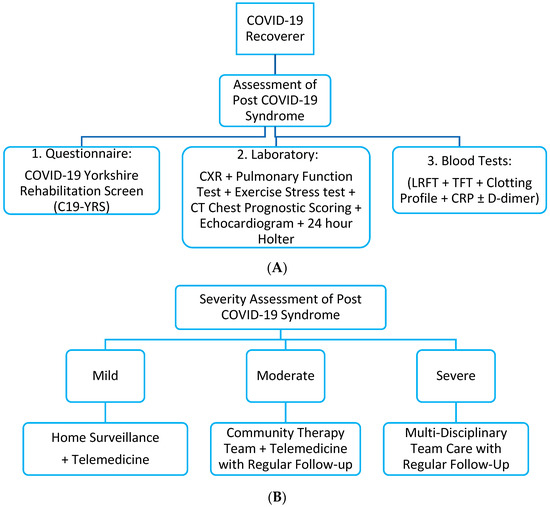
Figure 4.
Recommended rehabilitation model for patients with Post-COVID-19 Syndrome [8], as previously suggested by other authors. However, the key point lies in the severity assessment of Post-COVID-19 Syndrome and its classification. The limitation with this classification system is that there has not been a unified classification system for clinical severity. (A) Basic screening assessment of Post-COVID-19 Syndrome with prognostic scoring. (B) Recommended rehabilitation model based on initial assessment. CXR: Chest X-Ray. LRFT: Liver Renal Function Test. CRP: C-Reactive Protein. CT: Computed Tomography.

Table 5.
Rehabilitation programs and clinical studies showed efficacy for clinical improvement of PC19S.
Moderate impairment of physical capacity caused by muscle deconditioning has been observed in post-COVID-19 patients. Immobilization during its acute episodes further aggravates muscle deconditioning. Sarcopenia incidence is high, complicated by physical inactivity, lockdown, quarantine or acute hospitalization with bed rest [179]. Several small-scale studies have highlighted the importance of cardiopulmonary rehabilitation [180,181,182,183]. A recent clinical trial, the “COVID-Rehab Study”, recruited post-COVID-19 survivors for rehabilitation. This study equips them with aerobic exercise, muscle strengthening and respiratory exercise 3 times per week over 8 weeks with the aim to measure the effect of exercise on various parameters in patients with PC19S, such as cardiorespiratory fitness, neuropsychological assessment, physical strength and functional capacity of body balance and inflammatory markers [167]. The use of oxygen–ozone autohemotherapy has been shown to induce a significant reduction in chronic fatigue in a trial of 100 patients (H = 148.4786, p < 0.01) [136]. The underlying reason for exercise rehabilitation for PC19S is related to the mediation of the anti-inflammatory response, the support of brain homeostasis and the increase in insulin sensitivity to counteract the neuropsychiatric and endocrine sequelae of PC19S [184].
Optimization of comorbidities is a key to rehabilitation. Diabetes mellitus and underlying cardiovascular risk factors play vital roles in disease management [149]. Strict control of diabetes with an optimization of comorbidities, supervised rehabilitation with physical exercise and an optimization of nutrition is recommended for the management of PC19S [185,186]. There is some evidence that the adoption of a plant-based diet could benefit PC19S management due to a reduction of pro-inflammatory mediators [187].
A 7-week psychologist-led interdisciplinary virtual rehabilitation program showed significant improvements in health-related quality of life in terms of mobility, self-care, activities of daily living, pain/discomfort and anxiety/depression [188]. Another 6-week interdisciplinary individualized pulmonary rehabilitation program showed promising findings including an improvement in the 6-min walking distance, pulmonary function test, post-COVID-19 functional status, Borg dyspnea scale, Fatigue Assessment Scale and quality of life [168]. Recent studies have also recommended the role of erectile dysfunction as a biomarker for systemic complications of PC19S, and rehabilitation of sexual health should also be included [189].
A multidisciplinary model showed effective improvement of self-reported symptom scores [190]. Primary care physicians are crucial to curb preventable adverse events through the use of clinical questionnaires, imaging assessments and serial biomarker monitoring to detect early complications and provide timely treatment [191].
In view of the growing number of PC19S cases globally, early identification of affected individuals to provide appropriate and efficient treatment is required [192]. The use of telemedicine for rehabilitation is suitable for long-term PC19S monitoring [193]. It provides a reliable and flexible assessment of patient’s health status through remote monitoring, and identification of disorders and complications through long-term monitoring of health parameters. It also reduces patient’s anxiety toward PC19S. Mental health video consultations is a useful alternative to screen patients with PC19S-related psychiatric symptoms in primary care [194]. Peer support groups are another trend which fills professional care gaps, raises societal awareness and increases public engagement [195].
Neuropsychiatric complaints are a major reason for consultation after 9 months. Several models have been proposed for these patients [196] such as the UT Southwestern Medical Centre COVIER Recover Program, UT Health San Antonio Program, VA Greater Los Angeles Healthcare System, Hennepin Healthcare and University of Florida Model. All of these are designed based on population characteristics, complication prevalence at different periods and resource availability. Baseline assessment for medical need is the first step in order to differentiate those who require self-management, acute hospitalization, community rehabilitation and more advanced rehabilitation based on their physical, cognitive and behavioral symptoms, and the relevant assessment scoring system. Multidisciplinary rehabilitation teams and specialist care will be provided for those with moderate/severe complications.
In view of long-lasting symptoms with a strong probability of progression in PC19S, various clinical studies focusing on symptom trajectory and rehabilitation progress have been published/are in progress. A brief summary has been documented in Table 5. Most of these studies primarily focus on cardiorespiratory fitness and neuropsychiatric symptoms such as chronic fatigue syndrome, depression, anxiety and functional independence measures. Yet, there is no unified rehabilitation program that has shown superior efficacy compared to others since individualized programs may be more efficacious than group training in terms of cardiorespiratory outcomes [82].
PC19S-related fatigue is a common symptom reported in literature. Rehabilitation has shown great efficacy in reducing fatigue. A systematic review and meta-analysis showed that over 80% patients reported no persistent fatigue after rehabilitation [197]. Several studies worldwide have shown that rehabilitation results in a statistically significant improvement in walking tests and the Borg Dyspnea Scale [166,198,199,200,201,202].
10. Role of Vaccination in PC19S Rehabilitation
Vaccination confers partial protection from PC19S. An earlier study showed vaccination may contribute to a reduction in the population health burden of PC19S: the first dose reduces the odds of PC19S by 12.8% and the second dose reduces the odds by 8.8 (p < 0.01) [203]. However, in patients who already have PC19S, a delay of vaccination should be considered since a study showed that increases in antibody titers in patients with diagnosed PC19S might significantly worsen clinical symptoms [204].
The COVID-19 vaccine reduces PC19S sequelae by 15% (HR 0.85, 95% CI 0.82–0.89), including cardiovascular, hematological, gastrointestinal, mental health, musculoskeletal and neuropsychiatric sequelae [205]. Owing to the, at best partial, protection of PC19S resulting from COVID-19 vaccines, it is not an optimal strategy to reduce PC19S sequelae [205]. Vaccinated individuals are recommended to take effective infection control measures and booster vaccinations since vaccinated individuals reported less frequent and shorter PC19S symptoms in the British study [206].
11. Future Trends
In spite of the enormous population with PC19S, only 7% received PC19S care in the public sector and among those requiring additional help for PC19S, over half prefer assistance by digital health interventions (DHI) [207]. DHI-related research is under progress worldwide to understand its application in the remote monitoring of PC19S as it is seen as an economical rehabilitation model [208,209,210]. Future directions should include restructuring of PC19S rehabilitation services including both face-to-face consultations and digital interventions to allow flexibility.
The pathophysiology, prognostication scoring system and correlations with underlying comorbidities in different diseased populations are currently under investigation [211]. Mapping of clinical symptoms to the Human Phenotype Ontology for unification of PC19S reporting has been recommended to improve the stratification, diagnosis, treatment and scientific research of PC19S [212]. Different diagnostic criteria have been proposed, but further research into imaging and biochemical diagnosis is required for a definitive approach [213].
Multidisciplinary collaboration with a clear pathway for the diagnosis and management of PC19S is required globally in view of the surging number of patients with PC19S. A clear and integrated care system consisting of holistic healthcare pathways, detection of system-specific complications, management of mild symptoms and tailored rehabilitation services should be planned for in the future.
Author Contributions
Literature search, study designs, figures, data collections, data analysis, data interpretation and manuscript writing were done by M.Z.Y., M.Y. and C.-L.L., M.Z.Y. and M.Y. contribute equally to this work. All authors have read and agreed to the published version of the manuscript.
Funding
The authors did not receive funding for this project.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
There is no conflict of interest.
References
- Yan, Z.P.; Yang, M.; Lai, C.L. COVID-19 Vaccines: A Review of the Safety and Efficacy of Current Clinical Trials. Pharmaceuticals 2021, 14, 406. [Google Scholar] [CrossRef] [PubMed]
- Yan, Z.; Yang, M.; Lai, C.L. COVID-19 Vaccinations: A Comprehensive Review of Their Safety and Efficacy in Special Populations. Vaccines 2021, 9, 1097. [Google Scholar] [CrossRef]
- Chen, C.; Haupert, S.R.; Zimmermann, L.; Shi, X.; Fritsche, L.G.; Mukherjee, B. Global Prevalence of Post COVID-19 Condition or Long COVID: A Meta-Analysis and Systematic Review. J. Infect. Dis. 2022, 226, 1593–1607. [Google Scholar] [CrossRef]
- Seang, S.; Itani, O.; Monsel, G.; Abdi, B.; Marcelin, A.G.; Valantin, M.A.; Palich, R.; Faycal, A.; Pourcher, V.; Katlama, C.; et al. Long COVID-19 symptoms: Clinical characteristics and recovery rate among non-severe outpatients over a six-month follow-up. Infect. Dis. Now. 2022, 52, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Munblit, D.; Bobkova, P.; Spiridonova, E.; Shikhaleva, A.; Gamirova, A.; Blyuss, O.; Nekliudov, N.; Bugaeva, P.; Andreeva, M.; DunnGalvin, A.; et al. Incidence and risk factors for persistent symptoms in adults previously hospitalized for COVID-19. Clin. Exp. Allergy 2021, 51, 1107–1120. [Google Scholar] [CrossRef]
- Martin, C.; Luteijn, M.; Letton, W.; Robertson, J.; McDonald, S. A model framework for projecting the prevalence and impact of Long-COVID in the UK. PLoS ONE 2021, 16, e0260843. [Google Scholar] [CrossRef]
- Smith, M.P. Estimating total morbidity burden of COVID-19: Relative importance of death and disability. J. Clin. Epidemiol. 2022, 142, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Yan, Z.; Yang, M.; Lai, C.L. Long COVID-19 Syndrome: A Comprehensive Review of Its Effect on Various Organ Systems and Recommendation on Rehabilitation Plans. Biomedicines 2021, 9, 966. [Google Scholar] [CrossRef]
- O’Connor, R.J.; Preston, N.; Parkin, A.; Makower, S.; Ross, D.; Gee, J.; Halpin, S.J.; Horton, M.; Sivan, M. The COVID-19 Yorkshire Rehabilitation Scale (C19-YRS): Application and psychometric analysis in a post-COVID-19 syndrome cohort. J. Med. Virol. 2022, 94, 1027–1034. [Google Scholar] [CrossRef]
- Hughes, S.E.; Haroon, S.; Subramanian, A.; McMullan, C.; Aiyegbusi, O.L.; Turner, G.M.; Jackson, L.; Davies, E.H.; Frost, C.; McNamara, G.; et al. Development and validation of the symptom burden questionnaire for long covid (SBQ-LC): Rasch analysis. BMJ 2022, 377, e070230. [Google Scholar] [CrossRef]
- Taylor, A.K.; Kingstone, T.; Briggs, T.A.; O’Donnell, C.A.; Atherton, H.; Blane, D.N.; Chew-Graham, C.A. ‘Reluctant pioneer’: A qualitative study of doctors’ experiences as patients with long COVID. Health Expect. 2021, 24, 833–842. [Google Scholar] [CrossRef] [PubMed]
- Doherty, A.M.; Colleran, G.C.; Durcan, L.; Irvine, A.D.; Barrett, E. A pilot study of burnout and long covid in senior specialist doctors. Ir. J. Med. Sci. 2022, 191, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Petersen, E.L.; Gossling, A.; Adam, G.; Aepfelbacher, M.; Behrendt, C.A.; Cavus, E.; Cheng, B.; Fischer, N.; Gallinat, J.; Kuhn, S.; et al. Multi-organ assessment in mainly non-hospitalized individuals after SARS-CoV-2 infection: The Hamburg City Health Study COVID programme. Eur. Heart J. 2022, 43, 1124–1137. [Google Scholar] [CrossRef] [PubMed]
- Funke-Chambour, M.; Bridevaux, P.O.; Clarenbach, C.F.; Soccal, P.M.; Nicod, L.P.; von Garnier, C.; Swiss, C.L.S.G.; on behalf of the Swiss COVID Lung Study Group and the Swiss Society of Pulmonology. Swiss Recommendations for the Follow-Up and Treatment of Pulmonary Long COVID. Respiration 2021, 100, 826–841. [Google Scholar] [CrossRef]
- Van Herck, M.; Goertz, Y.M.J.; Houben-Wilke, S.; Machado, F.V.C.; Meys, R.; Delbressine, J.M.; Vaes, A.W.; Burtin, C.; Posthuma, R.; Franssen, F.M.E.; et al. Severe Fatigue in Long COVID: Web-Based Quantitative Follow-up Study in Members of Online Long COVID Support Groups. J. Med. Internet Res. 2021, 23, e30274. [Google Scholar] [CrossRef]
- Tran, V.T.; Riveros, C.; Clepier, B.; Desvarieux, M.; Collet, C.; Yordanov, Y.; Ravaud, P. Development and Validation of the Long Coronavirus Disease (COVID) Symptom and Impact Tools: A Set of Patient-Reported Instruments Constructed From Patients’ Lived Experience. Clin. Infect. Dis. 2022, 74, 278–287. [Google Scholar] [CrossRef] [PubMed]
- Titze-de-Almeida, R.; da Cunha, T.R.; Dos Santos Silva, L.D.; Ferreira, C.S.; Silva, C.P.; Ribeiro, A.P.; de Castro Moreira Santos Junior, A.; de Paula Brandao, P.R.; Silva, A.P.B.; da Rocha, M.C.O.; et al. Persistent, new-onset symptoms and mental health complaints in Long COVID in a Brazilian cohort of non-hospitalized patients. BMC Infect. Dis 2022, 22, 133. [Google Scholar] [CrossRef]
- Mohamed-Hussein, A.A.R.; Amin, M.T.; Makhlouf, H.A.; Makhlouf, N.A.; Galal, I.; Abd-Elaal, H.K.; Abdeltawab, D.; Kholief, K.M.S.; Hashem, M.K. Non-hospitalised COVID-19 patients have more frequent long COVID-19 symptoms. Int. J. Tuberc. Lung Dis. 2021, 25, 732–737. [Google Scholar] [CrossRef]
- Naik, S.; Haldar, S.N.; Soneja, M.; Mundadan, N.G.; Garg, P.; Mittal, A.; Desai, D.; Trilangi, P.K.; Chakraborty, S.; Begam, N.N.; et al. Post COVID-19 sequelae: A prospective observational study from Northern India. Drug Discov. Ther. 2021, 15, 254–260. [Google Scholar] [CrossRef]
- Jandhyala, R. Design, validation and implementation of the post-acute (long) COVID-19 quality of life (PAC-19QoL) instrument. Health Qual. Life Outcomes 2021, 19, 229. [Google Scholar] [CrossRef]
- Poudel, A.N.; Zhu, S.; Cooper, N.; Roderick, P.; Alwan, N.; Tarrant, C.; Ziauddeen, N.; Yao, G.L. Impact of Covid-19 on health-related quality of life of patients: A structured review. PLoS ONE 2021, 16, e0259164. [Google Scholar] [CrossRef] [PubMed]
- Lam, G.Y.; Befus, A.D.; Damant, R.W.; Ferrara, G.; Fuhr, D.P.; Stickland, M.K.; Varughese, R.A.; Wong, E.Y.; Smith, M.P. Exertional intolerance and dyspnea with preserved lung function: An emerging long COVID phenotype? Respir. Res. 2021, 22, 222. [Google Scholar] [CrossRef]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020, 8, 420–422. [Google Scholar] [CrossRef] [PubMed]
- Mo, X.; Jian, W.; Su, Z.; Chen, M.; Peng, H.; Peng, P.; Lei, C.; Chen, R.; Zhong, N.; Li, S. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. Eur. Respir. J. 2020, 55, 2001217. [Google Scholar] [CrossRef] [PubMed]
- Froidure, A.; Mahsouli, A.; Liistro, G.; De Greef, J.; Belkhir, L.; Gerard, L.; Bertrand, A.; Koenig, S.; Pothen, L.; Yildiz, H.; et al. Integrative respiratory follow-up of severe COVID-19 reveals common functional and lung imaging sequelae. Respir. Med. 2021, 181, 106383. [Google Scholar] [CrossRef]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Sonnweber, T.; Sahanic, S.; Pizzini, A.; Luger, A.; Schwabl, C.; Sonnweber, B.; Kurz, K.; Koppelstatter, S.; Haschka, D.; Petzer, V.; et al. Cardiopulmonary recovery after COVID-19: An observational prospective multicentre trial. Eur. Respir. J. 2021, 57, 2003481. [Google Scholar] [CrossRef] [PubMed]
- Ambardar, S.R.; Hightower, S.L.; Huprikar, N.A.; Chung, K.K.; Singhal, A.; Collen, J.F. Post-COVID-19 Pulmonary Fibrosis: Novel Sequelae of the Current Pandemic. J. Clin. Med. 2021, 10, 2452. [Google Scholar] [CrossRef]
- Wang, Y.; Dong, C.; Hu, Y.; Li, C.; Ren, Q.; Zhang, X.; Shi, H.; Zhou, M. Temporal Changes of CT Findings in 90 Patients with COVID-19 Pneumonia: A Longitudinal Study. Radiology 2020, 296, E55–E64. [Google Scholar] [CrossRef]
- Deng, L.; Khan, A.; Zhou, W.; Dai, Y.; Md, E.; Chen, R.; Cheng, G. Follow-up study of clinical and chest CT scans in confirmed COVID-19 patients. Radiol. Infect. Dis. 2020, 7, 106–113. [Google Scholar] [CrossRef]
- Barisione, E.; Grillo, F.; Ball, L.; Bianchi, R.; Grosso, M.; Morbini, P.; Pelosi, P.; Patroniti, N.A.; De Lucia, A.; Orengo, G.; et al. Fibrotic progression and radiologic correlation in matched lung samples from COVID-19 post-mortems. Virchows Arch. 2021, 478, 471–485. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Wu, Q.; Chen, Z.; Xiong, Z.; Wang, K.; Tian, J.; Zhang, S. The potential indicators for pulmonary fibrosis in survivors of severe COVID-19. J. Infect. 2021, 82, e5–e7. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.Y.; Qiao, K.; Liu, F.; Wu, B.; Xu, X.; Jiao, G.Q.; Lu, R.G.; Li, H.X.; Zhao, J.; Huang, J.; et al. Lung transplantation as therapeutic option in acute respiratory distress syndrome for coronavirus disease 2019-related pulmonary fibrosis. Chin. Med. J. (Engl.) 2020, 133, 1390–1396. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wu, J.; Wang, S.; Li, X.; Zhou, J.; Huang, B.; Luo, D.; Cao, Q.; Chen, Y.; Chen, S.; et al. Progression to fibrosing diffuse alveolar damage in a series of 30 minimally invasive autopsies with COVID-19 pneumonia in Wuhan, China. Histopathology 2021, 78, 542–555. [Google Scholar] [CrossRef] [PubMed]
- Baker, J.R.; Mahdi, M.; Nicolau, D.V., Jr.; Ramakrishnan, S.; Barnes, P.J.; Simpson, J.L.; Cass, S.P.; Russell, R.E.K.; Donnelly, L.E.; Bafadhel, M. Early Th2 inflammation in the upper respiratory mucosa as a predictor of severe COVID-19 and modulation by early treatment with inhaled corticosteroids: A mechanistic analysis. Lancet Respir. Med. 2022, 10, 545–556. [Google Scholar] [CrossRef] [PubMed]
- Ostergaard, L. SARS CoV-2 related microvascular damage and symptoms during and after COVID-19: Consequences of capillary transit-time changes, tissue hypoxia and inflammation. Physiol. Rep. 2021, 9, e14726. [Google Scholar] [CrossRef]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in COVID-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef]
- Liu, P.P.; Blet, A.; Smyth, D.; Li, H. The Science Underlying COVID-19: Implications for the Cardiovascular System. Circulation 2020, 142, 68–78. [Google Scholar] [CrossRef]
- Giamarellos-Bourboulis, E.J.; Netea, M.G.; Rovina, N.; Akinosoglou, K.; Antoniadou, A.; Antonakos, N.; Damoraki, G.; Gkavogianni, T.; Adami, M.E.; Katsaounou, P.; et al. Complex Immune Dysregulation in COVID-19 Patients with Severe Respiratory Failure. Cell Host Microbe 2020, 27, 992–1000.e3. [Google Scholar] [CrossRef] [PubMed]
- Mitrani, R.D.; Dabas, N.; Goldberger, J.J. COVID-19 cardiac injury: Implications for long-term surveillance and outcomes in survivors. Heart Rhythm 2020, 17, 1984–1990. [Google Scholar] [CrossRef] [PubMed]
- Raman, B.; Bluemke, D.A.; Luscher, T.F.; Neubauer, S. Long COVID: Post-acute sequelae of COVID-19 with a cardiovascular focus. Eur. Heart J. 2022, 43, 1157–1172. [Google Scholar] [CrossRef] [PubMed]
- Townsend, L.; Fogarty, H.; Dyer, A.; Martin-Loeches, I.; Bannan, C.; Nadarajan, P.; Bergin, C.; O’Farrelly, C.; Conlon, N.; Bourke, N.M.; et al. Prolonged elevation of D-dimer levels in convalescent COVID-19 patients is independent of the acute phase response. J. Thromb. Haemost. 2021, 19, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Roncon, L.; Zuin, M.; Zonzin, P. Age-adjusted D-dimer cut-off levels to rule out venous thromboembolism in COVID-19 patients. Thromb. Res. 2020, 190, 102. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; de Oliveira, M.H.S.; Benoit, S.; Plebani, M.; Lippi, G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): A meta-analysis. Clin. Chem. Lab. Med. 2020, 58, 1021–1028. [Google Scholar] [CrossRef]
- Yang, X.; Jin, Y.; Li, R.; Zhang, Z.; Sun, R.; Chen, D. Prevalence and impact of acute renal impairment on COVID-19: A systematic review and meta-analysis. Crit. Care 2020, 24, 356. [Google Scholar] [CrossRef]
- Ng, J.H.; Hirsch, J.S.; Hazzan, A.; Wanchoo, R.; Shah, H.H.; Malieckal, D.A.; Ross, D.W.; Sharma, P.; Sakhiya, V.; Fishbane, S.; et al. Outcomes Among Patients Hospitalized With COVID-19 and Acute Kidney Injury. Am. J. Kidney Dis. 2021, 77, 204–215. [Google Scholar] [CrossRef]
- Post, A.; den Deurwaarder, E.S.G.; Bakker, S.J.L.; de Haas, R.J.; van Meurs, M.; Gansevoort, R.T.; Berger, S.P. Kidney Infarction in Patients With COVID-19. Am. J. Kidney Dis. 2020, 76, 431–435. [Google Scholar] [CrossRef]
- Pei, G.; Zhang, Z.; Peng, J.; Liu, L.; Zhang, C.; Yu, C.; Ma, Z.; Huang, Y.; Liu, W.; Yao, Y.; et al. Renal Involvement and Early Prognosis in Patients with COVID-19 Pneumonia. J. Am. Soc. Nephrol. 2020, 31, 1157–1165. [Google Scholar] [CrossRef]
- Monkemuller, K.; Fry, L.; Rickes, S. COVID-19, coronavirus, SARS-CoV-2 and the small bowel. Rev. Esp. Enferm. Dig. 2020, 112, 383–388. [Google Scholar] [CrossRef]
- Wu, Y.; Guo, C.; Tang, L.; Hong, Z.; Zhou, J.; Dong, X.; Yin, H.; Xiao, Q.; Tang, Y.; Qu, X.; et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol. Hepatol. 2020, 5, 434–435. [Google Scholar] [CrossRef]
- Xu, Y.; Li, X.; Zhu, B.; Liang, H.; Fang, C.; Gong, Y.; Guo, Q.; Sun, X.; Zhao, D.; Shen, J.; et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat. Med. 2020, 26, 502–505. [Google Scholar] [CrossRef] [PubMed]
- Effenberger, M.; Grabherr, F.; Mayr, L.; Schwaerzler, J.; Nairz, M.; Seifert, M.; Hilbe, R.; Seiwald, S.; Scholl-Buergi, S.; Fritsche, G.; et al. Faecal calprotectin indicates intestinal inflammation in COVID-19. Gut 2020, 69, 1543–1544. [Google Scholar] [CrossRef] [PubMed]
- Barbara, G.; Feinle-Bisset, C.; Ghoshal, U.C.; Quigley, E.M.; Santos, J.; Vanner, S.; Vergnolle, N.; Zoetendal, E.G. The Intestinal Microenvironment and Functional Gastrointestinal Disorders. Gastroenterology 2016, 150, 1305–1318.e8. [Google Scholar] [CrossRef] [PubMed]
- De-Madaria, E.; Siau, K.; Cardenas-Jaen, K. Increased Amylase and Lipase in Patients With COVID-19 Pneumonia: Don’t Blame the Pancreas Just Yet! Gastroenterology 2021, 160, 1871. [Google Scholar] [CrossRef]
- Pribadi, R.R.; Simadibrata, M. Increased serum amylase and/or lipase in coronavirus disease 2019 (COVID-19) patients: Is it really pancreatic injury? JGH Open 2021, 5, 190–192. [Google Scholar] [CrossRef]
- Nordvig, A.S.; Fong, K.T.; Willey, J.Z.; Thakur, K.T.; Boehme, A.K.; Vargas, W.S.; Smith, C.J.; Elkind, M.S.V. Potential Neurologic Manifestations of COVID-19. Neurol. Clin. Pract. 2021, 11, e135–e146. [Google Scholar] [CrossRef]
- Fotuhi, M.; Mian, A.; Meysami, S.; Raji, C.A. Neurobiology of COVID-19. J. Alzheimers Dis. 2020, 76, 3–19. [Google Scholar] [CrossRef]
- Garrigues, E.; Janvier, P.; Kherabi, Y.; Le Bot, A.; Hamon, A.; Gouze, H.; Doucet, L.; Berkani, S.; Oliosi, E.; Mallart, E.; et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J. Infect. 2020, 81, e4–e6. [Google Scholar] [CrossRef] [PubMed]
- Miners, S.; Kehoe, P.G.; Love, S. Cognitive impact of COVID-19: Looking beyond the short term. Alzheimers Res. Ther. 2020, 12, 170. [Google Scholar] [CrossRef]
- Lee, M.H.; Perl, D.P.; Nair, G.; Li, W.; Maric, D.; Murray, H.; Dodd, S.J.; Koretsky, A.P.; Watts, J.A.; Cheung, V.; et al. Microvascular Injury in the Brains of Patients with COVID-19. N. Engl. J. Med. 2021, 384, 481–483. [Google Scholar] [CrossRef]
- Kaseda, E.T.; Levine, A.J. Post-traumatic stress disorder: A differential diagnostic consideration for COVID-19 survivors. Clin. Neuropsychol. 2020, 34, 1498–1514. [Google Scholar] [CrossRef] [PubMed]
- Chee, Y.J.; Ng, S.J.H.; Yeoh, E. Diabetic ketoacidosis precipitated by COVID-19 in a patient with newly diagnosed diabetes mellitus. Diabetes Res. Clin. Pract. 2020, 164, 108166. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, X.; Chen, J.; Zuo, X.; Zhang, H.; Deng, A. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes. Metab. 2020, 22, 1935–1941. [Google Scholar] [CrossRef]
- Ren, H.; Yang, Y.; Wang, F.; Yan, Y.; Shi, X.; Dong, K.; Yu, X.; Zhang, S. Association of the insulin resistance marker TyG index with the severity and mortality of COVID-19. Cardiovasc. Diabetol. 2020, 19, 58. [Google Scholar] [CrossRef] [PubMed]
- Suwanwongse, K.; Shabarek, N. Newly diagnosed diabetes mellitus, DKA, and COVID-19: Causality or coincidence? A report of three cases. J. Med. Virol. 2021, 93, 1150–1153. [Google Scholar] [CrossRef] [PubMed]
- Xiang, M.; Jing, H.; Wang, C.; Novakovic, V.A.; Shi, J. Persistent Lung Injury and Prothrombotic State in Long COVID. Front. Immunol. 2022, 13, 862522. [Google Scholar] [CrossRef]
- Saad, M.A.; El Khateeb, A.F.; Ahmed, M.I.; Magdy, A.M. Semi-quantitative CT severity scoring as a predictor of development of post-COVID syndrome. Egypt. J. Radiol. Nucl. Med. 2021, 52, 102. [Google Scholar] [CrossRef]
- Yang, R.; Li, X.; Liu, H.; Zhen, Y.; Zhang, X.; Xiong, Q.; Luo, Y.; Gao, C.; Zeng, W. Chest CT Severity Score: An Imaging Tool for Assessing Severe COVID-19. Radiol. Cardiothorac. Imaging 2020, 2, e200047. [Google Scholar] [CrossRef]
- Pan, F.; Ye, T.; Sun, P.; Gui, S.; Liang, B.; Li, L.; Zheng, D.; Wang, J.; Hesketh, R.L.; Yang, L.; et al. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology 2020, 295, 715–721. [Google Scholar] [CrossRef]
- Francone, M.; Iafrate, F.; Masci, G.M.; Coco, S.; Cilia, F.; Manganaro, L.; Panebianco, V.; Andreoli, C.; Colaiacomo, M.C.; Zingaropoli, M.A.; et al. Chest CT score in COVID-19 patients: Correlation with disease severity and short-term prognosis. Eur. Radiol. 2020, 30, 6808–6817. [Google Scholar] [CrossRef]
- Alharbi, K.S.; Singh, Y.; Hassan Almalki, W.; Rawat, S.; Afzal, O.; Alfawaz Altamimi, A.S.; Kazmi, I.; Al-Abbasi, F.A.; Alzarea, S.I.; Singh, S.K.; et al. Gut Microbiota Disruption in COVID-19 or Post-COVID Illness Association with severity biomarkers: A Possible Role of Pre/Pro-biotics in manipulating microflora. Chem. Biol. Interact. 2022, 358, 109898. [Google Scholar] [CrossRef] [PubMed]
- Raj, S.R.; Guzman, J.C.; Harvey, P.; Richer, L.; Schondorf, R.; Seifer, C.; Thibodeau-Jarry, N.; Sheldon, R.S. Canadian Cardiovascular Society Position Statement on Postural Orthostatic Tachycardia Syndrome (POTS) and Related Disorders of Chronic Orthostatic Intolerance. Can. J. Cardiol. 2020, 36, 357–372. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, D.S. The possible association between COVID-19 and postural tachycardia syndrome. Heart Rhythm 2021, 18, 508–509. [Google Scholar] [CrossRef]
- Monje, M.; Iwasaki, A. The neurobiology of long COVID. Neuron 2022, 110, 3484–3496. [Google Scholar] [CrossRef] [PubMed]
- de Paula, J.J.; Paiva, R.; Souza-Silva, N.G.; Rosa, D.V.; Duran, F.L.S.; Coimbra, R.S.; Costa, D.S.; Dutenhefner, P.R.; Oliveira, H.S.D.; Camargos, S.T.; et al. Selective visuoconstructional impairment following mild COVID-19 with inflammatory and neuroimaging correlation findings. Mol. Psychiatry 2023, 28, 553–563. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Castaneda, A.; Lu, P.; Geraghty, A.C.; Song, E.; Lee, M.H.; Wood, J.; O’Dea, M.R.; Dutton, S.; Shamardani, K.; Nwangwu, K.; et al. Mild respiratory COVID can cause multi-lineage neural cell and myelin dysregulation. Cell 2022, 185, 2452–2468.e16. [Google Scholar] [CrossRef] [PubMed]
- Geraghty, A.C.; Gibson, E.M.; Ghanem, R.A.; Greene, J.J.; Ocampo, A.; Goldstein, A.K.; Ni, L.; Yang, T.; Marton, R.M.; Pasca, S.P.; et al. Loss of Adaptive Myelination Contributes to Methotrexate Chemotherapy-Related Cognitive Impairment. Neuron 2019, 103, 250–265.e8. [Google Scholar] [CrossRef]
- Thakur, K.T.; Miller, E.H.; Glendinning, M.D.; Al-Dalahmah, O.; Banu, M.A.; Boehme, A.K.; Boubour, A.L.; Bruce, S.S.; Chong, A.M.; Claassen, J.; et al. COVID-19 neuropathology at Columbia University Irving Medical Center/New York Presbyterian Hospital. Brain 2021, 144, 2696–2708. [Google Scholar] [CrossRef] [PubMed]
- Frere, J.J.; Serafini, R.A.; Pryce, K.D.; Zazhytska, M.; Oishi, K.; Golynker, I.; Panis, M.; Zimering, J.; Horiuchi, S.; Hoagland, D.A.; et al. SARS-CoV-2 infection in hamsters and humans results in lasting and unique systemic perturbations after recovery. Sci. Transl. Med. 2022, 14, eabq3059. [Google Scholar] [CrossRef]
- Soung, A.L.; Vanderheiden, A.; Nordvig, A.S.; Sissoko, C.A.; Canoll, P.; Mariani, M.B.; Jiang, X.; Bricker, T.; Rosoklija, G.B.; Arango, V.; et al. COVID-19 induces CNS cytokine expression and loss of hippocampal neurogenesis. Brain 2022, 145, 4193–4201. [Google Scholar] [CrossRef]
- Guttenplan, K.A.; Weigel, M.K.; Prakash, P.; Wijewardhane, P.R.; Hasel, P.; Rufen-Blanchette, U.; Munch, A.E.; Blum, J.A.; Fine, J.; Neal, M.C.; et al. Neurotoxic reactive astrocytes induce cell death via saturated lipids. Nature 2021, 599, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Vlok, M.; Venter, C.; Bezuidenhout, J.A.; Laubscher, G.J.; Steenkamp, J.; Kell, D.B. Persistent clotting protein pathology in Long COVID/Post-Acute Sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc. Diabetol. 2021, 20, 172. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Yu, C.; Jing, H.; Wu, X.; Novakovic, V.A.; Xie, R.; Shi, J. Long COVID: The Nature of Thrombotic Sequelae Determines the Necessity of Early Anticoagulation. Front. Cell. Infect. Microbiol. 2022, 12, 861703. [Google Scholar] [CrossRef] [PubMed]
- Kappelmann, N.; Dantzer, R.; Khandaker, G.M. Interleukin-6 as potential mediator of long-term neuropsychiatric symptoms of COVID-19. Psychoneuroendocrinology 2021, 131, 105295. [Google Scholar] [CrossRef]
- Peluso, M.J.; Lu, S.; Tang, A.F.; Durstenfeld, M.S.; Ho, H.E.; Goldberg, S.A.; Forman, C.A.; Munter, S.E.; Hoh, R.; Tai, V.; et al. Markers of Immune Activation and Inflammation in Individuals With Postacute Sequelae of Severe Acute Respiratory Syndrome Coronavirus 2 Infection. J. Infect. Dis. 2021, 224, 1839–1848. [Google Scholar] [CrossRef]
- Haran, J.P.; Bradley, E.; Zeamer, A.L.; Cincotta, L.; Salive, M.C.; Dutta, P.; Mutaawe, S.; Anya, O.; Meza-Segura, M.; Moormann, A.M.; et al. Inflammation-type dysbiosis of the oral microbiome associates with the duration of COVID-19 symptoms and long COVID. JCI Insight 2021, 6, e152346. [Google Scholar] [CrossRef] [PubMed]
- Lui, D.T.W.; Lee, C.H.; Chow, W.S.; Lee, A.C.H.; Tam, A.R.; Pang, P.; Ho, T.Y.; Fong, C.H.Y.; Law, C.Y.; Leung, E.K.H.; et al. Long COVID in Patients With Mild to Moderate Disease: Do Thyroid Function and Autoimmunity Play a Role? Endocr. Pract. 2021, 27, 894–902. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.J.L. Persistent SARS-2 infections contribute to long COVID-19. Med. Hypotheses 2021, 149, 110538. [Google Scholar] [CrossRef]
- Glynne, P.; Tahmasebi, N.; Gant, V.; Gupta, R. Long COVID following mild SARS-CoV-2 infection: Characteristic T cell alterations and response to antihistamines. J. Investig. Med. 2022, 70, 61–67. [Google Scholar] [CrossRef]
- Loke, X.Y.; Imran, S.A.M.; Tye, G.J.; Wan Kamarul Zaman, W.S.; Nordin, F. Immunomodulation and Regenerative Capacity of MSCs for Long-COVID. Int. J. Mol. Sci. 2021, 22, 12421. [Google Scholar] [CrossRef]
- Holmes, E.; Wist, J.; Masuda, R.; Lodge, S.; Nitschke, P.; Kimhofer, T.; Loo, R.L.; Begum, S.; Boughton, B.; Yang, R.; et al. Incomplete Systemic Recovery and Metabolic Phenoreversion in Post-Acute-Phase Nonhospitalized COVID-19 Patients: Implications for Assessment of Post-Acute COVID-19 Syndrome. J. Proteome Res. 2021, 20, 3315–3329. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.A.; Hossain, K.M.A.; Saunders, K.; Uddin, Z.; Walton, L.M.; Raigangar, V.; Sakel, M.; Shafin, R.; Hossain, M.S.; Kabir, M.F.; et al. Prevalence of Long COVID symptoms in Bangladesh: A prospective Inception Cohort Study of COVID-19 survivors. BMJ Glob. Health 2021, 6, e006838. [Google Scholar] [CrossRef]
- Nune, A.; Durkowski, V.; Titman, A.; Gupta, L.; Hadzhiivanov, M.; Ahmed, A.; Musat, C.; Sapkota, H.R. Incidence and risk factors of long COVID in the UK: A single-centre observational study. J. R. Coll. Physicians Edinb. 2021, 51, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Dhawan, R.T.; Gopalan, D.; Howard, L.; Vicente, A.; Park, M.; Manalan, K.; Wallner, I.; Marsden, P.; Dave, S.; Branley, H.; et al. Beyond the clot: Perfusion imaging of the pulmonary vasculature after COVID-19. Lancet Respir. Med. 2021, 9, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Patel, B.V.; Arachchillage, D.J.; Ridge, C.A.; Bianchi, P.; Doyle, J.F.; Garfield, B.; Ledot, S.; Morgan, C.; Passariello, M.; Price, S.; et al. Pulmonary Angiopathy in Severe COVID-19: Physiologic, Imaging, and Hematologic Observations. Am. J. Respir. Crit. Care Med. 2020, 202, 690–699. [Google Scholar] [CrossRef]
- Puntmann, V.O.; Carerj, M.L.; Wieters, I.; Fahim, M.; Arendt, C.; Hoffmann, J.; Shchendrygina, A.; Escher, F.; Vasa-Nicotera, M.; Zeiher, A.M.; et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 1265–1273. [Google Scholar] [CrossRef]
- Diaz, A.; Bujnowski, D.; McMullen, P.; Lysandrou, M.; Ananthanarayanan, V.; Husain, A.N.; Freeman, R.; Vigneswaran, W.T.; Ferguson, M.K.; Donington, J.S.; et al. Pulmonary Parenchymal Changes in COVID-19 Survivors. Ann. Thorac. Surg. 2022, 114, 301–310. [Google Scholar] [CrossRef]
- Kim, Y.; Bitna, H.; Kim, S.W.; Chang, H.H.; Kwon, K.T.; Bae, S.; Hwang, S. Post-acute COVID-19 syndrome in patients after 12 months from COVID-19 infection in Korea. BMC Infect. Dis. 2022, 22, 93. [Google Scholar] [CrossRef]
- O’Kelly, B.; Vidal, L.; Avramovic, G.; Broughan, J.; Connolly, S.P.; Cotter, A.G.; Cullen, W.; Glaspy, S.; McHugh, T.; Woo, J.; et al. Assessing the impact of COVID-19 at 1-year using the SF-12 questionnaire: Data from the Anticipate longitudinal cohort study. Int. J. Infect. Dis. 2022, 118, 236–243. [Google Scholar] [CrossRef]
- Philip, K.E.; Lewis, A.; Jeffery, E.; Buttery, S.; Cave, P.; Cristiano, D.; Lound, A.; Taylor, K.; Man, W.D.; Fancourt, D.; et al. Moving singing for lung health online in response to COVID-19: Experience from a randomised controlled trial. BMJ Open Respir. Res. 2020, 7, e000737. [Google Scholar] [CrossRef]
- Soejima, Y.; Otsuka, Y.; Tokumasu, K.; Nakano, Y.; Harada, K.; Nakamoto, K.; Sunada, N.; Sakurada, Y.; Hasegawa, K.; Hagiya, H.; et al. Late-Onset Hypogonadism in a Male Patient with Long COVID Diagnosed by Exclusion of ME/CFS. Medicina 2022, 58, 536. [Google Scholar] [CrossRef]
- Global Burden of Disease Long, C.C.; Wulf Hanson, S.; Abbafati, C.; Aerts, J.G.; Al-Aly, Z.; Ashbaugh, C.; Ballouz, T.; Blyuss, O.; Bobkova, P.; Bonsel, G.; et al. Estimated Global Proportions of Individuals With Persistent Fatigue, Cognitive, and Respiratory Symptom Clusters Following Symptomatic COVID-19 in 2020 and 2021. JAMA 2022, 328, 1604–1615. [Google Scholar] [CrossRef]
- Diez-Cirarda, M.; Yus, M.; Gomez-Ruiz, N.; Polidura, C.; Gil-Martinez, L.; Delgado-Alonso, C.; Jorquera, M.; Gomez-Pinedo, U.; Matias-Guiu, J.; Arrazola, J.; et al. Multimodal neuroimaging in post-COVID syndrome and correlation with cognition. Brain 2022, awac384. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A.; Niloofa, R.; Jayarajah, U.; De Mel, S.; Abeysuriya, V.; Seneviratne, S.L. Hematological Abnormalities in COVID-19: A Narrative Review. Am. J. Trop. Med. Hyg. 2021, 104, 1188–1201. [Google Scholar] [CrossRef] [PubMed]
- Agbuduwe, C.; Basu, S. Haematological manifestations of COVID-19: From cytopenia to coagulopathy. Eur. J. Haematol. 2020, 105, 540–546. [Google Scholar] [CrossRef] [PubMed]
- Minami, T.; Iwata, Y.; Wada, T. Renal complications in coronavirus disease 2019: A systematic review. Inflamm. Regen. 2020, 40, 31. [Google Scholar] [CrossRef]
- Smith, S.M.; Boppana, A.; Traupman, J.A.; Unson, E.; Maddock, D.A.; Chao, K.; Dobesh, D.P.; Brufsky, A.; Connor, R.I. Impaired glucose metabolism in patients with diabetes, prediabetes, and obesity is associated with severe COVID-19. J. Med. Virol. 2021, 93, 409–415. [Google Scholar] [CrossRef]
- Fresard, I.; Genecand, L.; Altarelli, M.; Gex, G.; Vremaroiu, P.; Vremaroiu-Coman, A.; Lawi, D.; Bridevaux, P.O. Dysfunctional breathing diagnosed by cardiopulmonary exercise testing in ‘long COVID’ patients with persistent dyspnoea. BMJ Open Respir. Res. 2022, 9, e001126. [Google Scholar] [CrossRef]
- Kersten, J.; Wolf, A.; Hoyo, L.; Hull, E.; Tadic, M.; Andress, S.; d’Almeida, S.; Scharnbeck, D.; Roder, E.; Beschoner, P.; et al. Symptom burden correlates to impairment of diffusion capacity and exercise intolerance in long COVID patients. Sci. Rep. 2022, 12, 8801. [Google Scholar] [CrossRef]
- Mayer, K.P.; Steele, A.K.; Soper, M.K.; Branton, J.D.; Lusby, M.L.; Kalema, A.G.; Dupont-Versteegden, E.E.; Montgomery-Yates, A.A. Physical Therapy Management of an Individual With Post-COVID Syndrome: A Case Report. Phys. Ther. 2021, 101, pzab098. [Google Scholar] [CrossRef]
- McNarry, M.A.; Berg, R.M.G.; Shelley, J.; Hudson, J.; Saynor, Z.L.; Duckers, J.; Lewis, K.; Davies, G.A.; Mackintosh, K.A. Inspiratory muscle training enhances recovery post-COVID-19: A randomised controlled trial. Eur. Respir. J. 2022, 60, 2103101. [Google Scholar] [CrossRef] [PubMed]
- Kayaaslan, B.; Eser, F.; Kalem, A.K.; Kaya, G.; Kaplan, B.; Kacar, D.; Hasanoglu, I.; Coskun, B.; Guner, R. Post-COVID syndrome: A single-center questionnaire study on 1007 participants recovered from COVID-19. J. Med. Virol. 2021, 93, 6566–6574. [Google Scholar] [CrossRef]
- Singh, I.; Joseph, P.; Heerdt, P.M.; Cullinan, M.; Lutchmansingh, D.D.; Gulati, M.; Possick, J.D.; Systrom, D.M.; Waxman, A.B. Persistent Exertional Intolerance After COVID-19: Insights From Invasive Cardiopulmonary Exercise Testing. Chest 2022, 161, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Morrow, A.; Gray, S.R.; Bayes, H.K.; Sykes, R.; McGarry, E.; Anderson, D.; Boiskin, D.; Burke, C.; Cleland, J.G.F.; Goodyear, C.; et al. Prevention and early treatment of the long-term physical effects of COVID-19 in adults: Design of a randomised controlled trial of resistance exercise-CISCO-21. Trials 2022, 23, 660. [Google Scholar] [CrossRef]
- Hugon, J.; Msika, E.F.; Queneau, M.; Farid, K.; Paquet, C. Long COVID: Cognitive complaints (brain fog) and dysfunction of the cingulate cortex. J. Neurol. 2022, 269, 44–46. [Google Scholar] [CrossRef]
- Whiteside, D.M.; Naini, S.M.; Basso, M.R.; Waldron, E.J.; Holker, E.; Porter, J.; Niskanen, N.; Melnik, T.E.; Taylor, S.E. Outcomes in post-acute sequelae of COVID-19 (PASC) at 6 months post-infection part 2: Psychological functioning. Clin. Neuropsychol. 2022, 36, 829–847. [Google Scholar] [CrossRef] [PubMed]
- Anderson, A.M.; Letendre, S.L.; Ances, B.M. CROI 2022: Neurologic complications of HIV-1, SARS-CoV-2, and other pathogens. Top. Antivir. Med. 2022, 30, 475–489. [Google Scholar]
- Weiner, L.; Berna, F.; Nourry, N.; Severac, F.; Vidailhet, P.; Mengin, A.C. Efficacy of an online cognitive behavioral therapy program developed for healthcare workers during the COVID-19 pandemic: The REduction of STress (REST) study protocol for a randomized controlled trial. Trials 2020, 21, 870. [Google Scholar] [CrossRef]
- Liu, Z.; Qiao, D.; Xu, Y.; Zhao, W.; Yang, Y.; Wen, D.; Li, X.; Nie, X.; Dong, Y.; Tang, S.; et al. The Efficacy of Computerized Cognitive Behavioral Therapy for Depressive and Anxiety Symptoms in Patients With COVID-19: Randomized Controlled Trial. J. Med. Internet Res. 2021, 23, e26883. [Google Scholar] [CrossRef]
- Wahlund, T.; Mataix-Cols, D.; Olofsdotter Lauri, K.; de Schipper, E.; Ljotsson, B.; Aspvall, K.; Andersson, E. Brief Online Cognitive Behavioural Intervention for Dysfunctional Worry Related to the COVID-19 Pandemic: A Randomised Controlled Trial. Psychother. Psychosom. 2021, 90, 191–199. [Google Scholar] [CrossRef]
- Kedor, C.; Freitag, H.; Meyer-Arndt, L.; Wittke, K.; Hanitsch, L.G.; Zoller, T.; Steinbeis, F.; Haffke, M.; Rudolf, G.; Heidecker, B.; et al. A prospective observational study of post-COVID-19 chronic fatigue syndrome following the first pandemic wave in Germany and biomarkers associated with symptom severity. Nat. Commun. 2022, 13, 5104. [Google Scholar] [CrossRef] [PubMed]
- Courel-Ibanez, J.; Buendia-Romero, A.; Pallares, J.G.; Garcia-Conesa, S.; Martinez-Cava, A.; Izquierdo, M. Impact of Tailored Multicomponent Exercise for Preventing Weakness and Falls on Nursing Home Residents’ Functional Capacity. J. Am. Med. Dir. Assoc. 2022, 23, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Blackett, J.W.; Sun, Y.; Purpura, L.; Margolis, K.G.; Elkind, M.S.V.; O’Byrne, S.; Wainberg, M.; Abrams, J.A.; Wang, H.H.; Chang, L.; et al. Decreased Gut Microbiome Tryptophan Metabolism and Serotonergic Signaling in Patients With Persistent Mental Health and Gastrointestinal Symptoms After COVID-19. Clin. Transl. Gastroenterol. 2022, 13, e00524. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Spranger, L.; Soll, D.; Beer, F.; Brachs, M.; Spranger, J.; Mai, K. Metabolic impact of weight loss induced reduction of adipose ACE-2—Potential implication in COVID-19 infections? Metabolism 2020, 113, 154401. [Google Scholar] [CrossRef]
- Soll, D.; Beer, F.; Spranger, L.; Li, L.; Spranger, J.; Mai, K. Effects of Weight Loss on Adipose and Muscular Neuropilin 1 mRNA Expression in Obesity: Potential Implication in SARS-CoV-2 Infections? Obes. Facts 2022, 15, 90–98. [Google Scholar] [CrossRef]
- Deftereos, S.G.; Giannopoulos, G.; Vrachatis, D.A.; Siasos, G.D.; Giotaki, S.G.; Gargalianos, P.; Metallidis, S.; Sianos, G.; Baltagiannis, S.; Panagopoulos, P.; et al. Effect of Colchicine vs. Standard Care on Cardiac and Inflammatory Biomarkers and Clinical Outcomes in Patients Hospitalized With Coronavirus Disease 2019: The GRECCO-19 Randomized Clinical Trial. JAMA Netw. Open 2020, 3, e2013136. [Google Scholar] [CrossRef] [PubMed]
- O’Mahoney, L.L.; Routen, A.; Gillies, C.; Ekezie, W.; Welford, A.; Zhang, A.; Karamchandani, U.; Simms-Williams, N.; Cassambai, S.; Ardavani, A.; et al. The prevalence and long-term health effects of Long Covid among hospitalised and non-hospitalised populations: A systematic review and meta-analysis. EClinicalMedicine 2023, 55, 101762. [Google Scholar] [CrossRef]
- Chand, S.; Kapoor, S.; Naqvi, A.; Thakkar, J.; Fazzari, M.J.; Orsi, D.; Dieiev, V.; Lewandowski, D.C.; Dicpinigaitis, P.V. Long-Term Follow up of Renal and Other Acute Organ Failure in Survivors of Critical Illness Due to COVID-19. J. Intensive Care Med. 2022, 37, 736–742. [Google Scholar] [CrossRef]
- Alkodaymi, M.S.; Omrani, O.A.; Fawzy, N.A.; Shaar, B.A.; Almamlouk, R.; Riaz, M.; Obeidat, M.; Obeidat, Y.; Gerberi, D.; Taha, R.M.; et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2022, 28, 657–666. [Google Scholar] [CrossRef]
- Righi, E.; Mirandola, M.; Mazzaferri, F.; Dossi, G.; Razzaboni, E.; Zaffagnini, A.; Ivaldi, F.; Visentin, A.; Lambertenghi, L.; Arena, C.; et al. Determinants of persistence of symptoms and impact on physical and mental wellbeing in Long COVID: A prospective cohort study. J. Infect. 2022, 84, 566–572. [Google Scholar] [CrossRef]
- Mirfazeli, F.S.; Sarabi-Jamab, A.; Pereira-Sanchez, V.; Kordi, A.; Shariati, B.; Shariat, S.V.; Bahrami, S.; Nohesara, S.; Almasi-Dooghaee, M.; Faiz, S.H.R. Chronic fatigue syndrome and cognitive deficit are associated with acute-phase neuropsychiatric manifestations of COVID-19: A 9-month follow-up study. Neurol. Sci. 2022, 43, 2231–2239. [Google Scholar] [CrossRef] [PubMed]
- Taskiran-Sag, A.; Eroglu, E.; Canlar, S.; Poyraz, B.M.; Ozulken, K.; Mumcuoglu, T.; Numanoglu, N. Subacute neurological sequelae in mild COVID-19 outpatients. Tuberk Toraks 2022, 70, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Yan, M.Z.; Li, X.; Lau, E.H.Y. Sequelae of COVID-19 among previously hospitalized patients up to 1 year after discharge: A systematic review and meta-analysis. Infection 2022, 50, 1067–1109. [Google Scholar] [CrossRef] [PubMed]
- Pinato, D.J.; Tabernero, J.; Bower, M.; Scotti, L.; Patel, M.; Colomba, E.; Dolly, S.; Loizidou, A.; Chester, J.; Mukherjee, U.; et al. Prevalence and impact of COVID-19 sequelae on treatment and survival of patients with cancer who recovered from SARS-CoV-2 infection: Evidence from the OnCovid retrospective, multicentre registry study. Lancet Oncol. 2021, 22, 1669–1680. [Google Scholar] [CrossRef]
- Crook, H.; Raza, S.; Nowell, J.; Young, M.; Edison, P. Long covid-mechanisms, risk factors, and management. BMJ 2021, 374, n1648. [Google Scholar] [CrossRef]
- Perez-Gonzalez, A.; Araujo-Ameijeiras, A.; Fernandez-Villar, A.; Crespo, M.; Poveda, E.; the Cohort COVID-19 of the Galicia Sur Health Research Institute. Long COVID in hospitalized and non-hospitalized patients in a large cohort in Northwest Spain, a prospective cohort study. Sci. Rep. 2022, 12, 3369. [Google Scholar] [CrossRef]
- Han, X.; Fan, Y.; Alwalid, O.; Li, N.; Jia, X.; Yuan, M.; Li, Y.; Cao, Y.; Gu, J.; Wu, H.; et al. Six-month Follow-up Chest CT Findings after Severe COVID-19 Pneumonia. Radiology 2021, 299, E177–E186. [Google Scholar] [CrossRef]
- Doykov, I.; Hallqvist, J.; Gilmour, K.C.; Grandjean, L.; Mills, K.; Heywood, W.E. ‘The long tail of COVID-19’—The detection of a prolonged inflammatory response after a SARS-CoV-2 infection in asymptomatic and mildly affected patients. F1000Res 2020, 9, 1349. [Google Scholar] [CrossRef]
- Petersen, M.S.; Kristiansen, M.F.; Hanusson, K.D.; Danielsen, M.E.; Steig, B.; Gaini, S.; Strøm, M.; Weihe, P. Long COVID in the Faroe Islands: A Longitudinal Study Among Nonhospitalized Patients. Clin. Infect. Dis. 2021, 73, e4058–e4063. [Google Scholar] [CrossRef]
- Chan Sui Ko, A.; Candellier, A.; Mercier, M.; Joseph, C.; Schmit, J.L.; Lanoix, J.P.; Andrejak, C. Number of initial symptoms is more related to long COVID-19 than acute severity of infection: A prospective cohort of hospitalized patients. Int. J. Infect. Dis. 2022, 118, 220–223. [Google Scholar] [CrossRef]
- Asadi-Pooya, A.A.; Nemati, H.; Shahisavandi, M.; Akbari, A.; Emami, A.; Lotfi, M.; Rostamihosseinkhani, M.; Barzegar, Z.; Kabiri, M.; Zeraatpisheh, Z.; et al. Long COVID in children and adolescents. World J. Pediatr. 2021, 17, 495–499. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, P.; Pittet, L.F.; Curtis, N. How Common is Long COVID in Children and Adolescents? Pediatr. Infect. Dis. J. 2021, 40, e482–e487. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.F. Case report and systematic review suggest that children may experience similar long-term effects to adults after clinical COVID-19. Acta Paediatr. 2021, 110, 914–921. [Google Scholar] [CrossRef]
- Weinstock, L.B.; Brook, J.B.; Walters, A.S.; Goris, A.; Afrin, L.B.; Molderings, G.J. Mast cell activation symptoms are prevalent in Long-COVID. Int. J. Infect. Dis. 2021, 112, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Raj, S.R.; Arnold, A.C.; Barboi, A.; Claydon, V.E.; Limberg, J.K.; Lucci, V.M.; Numan, M.; Peltier, A.; Snapper, H.; Vernino, S.; et al. Long-COVID postural tachycardia syndrome: An American Autonomic Society statement. Clin. Auton. Res. 2021, 31, 365–368. [Google Scholar] [CrossRef]
- Afrin, L.B.; Weinstock, L.B.; Molderings, G.J. Covid-19 hyperinflammation and post-Covid-19 illness may be rooted in mast cell activation syndrome. Int. J. Infect. Dis. 2020, 100, 327–332. [Google Scholar] [CrossRef]
- Mazzitelli, M.; Trunfio, M.; Sasset, L.; Leoni, D.; Castelli, E.; Lo Menzo, S.; Gardin, S.; Putaggio, C.; Brundu, M.; Garzotto, P.; et al. Factors Associated with Severe COVID-19 and Post-Acute COVID-19 Syndrome in a Cohort of People Living with HIV on Antiretroviral Treatment and with Undetectable HIV RNA. Viruses 2022, 14, 493. [Google Scholar] [CrossRef]
- Pujari, S.; Gaikwad, S.; Chitalikar, A.; Dabhade, D.; Joshi, K.; Bele, V. Long-coronavirus disease among people living with HIV in western India: An observational study. Immun. Inflamm. Dis. 2021, 9, 1037–1043. [Google Scholar] [CrossRef]
- Sollini, M.; Morbelli, S.; Ciccarelli, M.; Cecconi, M.; Aghemo, A.; Morelli, P.; Chiola, S.; Gelardi, F.; Chiti, A. Long COVID hallmarks on [18F]FDG-PET/CT: A case-control study. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 3187–3197. [Google Scholar] [CrossRef]
- Guedj, E.; Campion, J.Y.; Dudouet, P.; Kaphan, E.; Bregeon, F.; Tissot-Dupont, H.; Guis, S.; Barthelemy, F.; Habert, P.; Ceccaldi, M.; et al. (18)F-FDG brain PET hypometabolism in patients with long COVID. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 2823–2833. [Google Scholar] [CrossRef]
- Stefano, G.B.; Ptacek, R.; Ptackova, H.; Martin, A.; Kream, R.M. Selective Neuronal Mitochondrial Targeting in SARS-CoV-2 Infection Affects Cognitive Processes to Induce ‘Brain Fog’ and Results in Behavioral Changes that Favor Viral Survival. Med. Sci. Monit. 2021, 27, e930886. [Google Scholar] [CrossRef] [PubMed]
- Douaud, G.; Lee, S.; Alfaro-Almagro, F.; Arthofer, C.; Wang, C.; McCarthy, P.; Lange, F.; Andersson, J.L.R.; Griffanti, L.; Duff, E.; et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 2022, 604, 697–707. [Google Scholar] [CrossRef] [PubMed]
- Tian, T.; Wu, J.; Chen, T.; Li, J.; Yan, S.; Zhou, Y.; Peng, X.; Li, Y.; Zheng, N.; Cai, A.; et al. Long-term follow-up of dynamic brain changes in patients recovered from COVID-19 without neurological manifestations. JCI Insight 2022, 7, e155827. [Google Scholar] [CrossRef] [PubMed]
- Del Brutto, O.H.; Rumbea, D.A.; Recalde, B.Y.; Mera, R.M. Cognitive sequelae of long COVID may not be permanent: A prospective study. Eur. J. Neurol. 2022, 29, 1218–1221. [Google Scholar] [CrossRef] [PubMed]
- Seessle, J.; Waterboer, T.; Hippchen, T.; Simon, J.; Kirchner, M.; Lim, A.; Muller, B.; Merle, U. Persistent Symptoms in Adult Patients 1 Year After Coronavirus Disease 2019 (COVID-19): A Prospective Cohort Study. Clin. Infect. Dis. 2022, 74, 1191–1198. [Google Scholar] [CrossRef] [PubMed]
- Leta, V.; Rodriguez-Violante, M.; Abundes, A.; Rukavina, K.; Teo, J.T.; Falup-Pecurariu, C.; Irincu, L.; Rota, S.; Bhidayasiri, R.; Storch, A.; et al. Parkinson’s Disease and Post-COVID-19 Syndrome: The Parkinson’s Long-COVID Spectrum. Mov. Disord. 2021, 36, 1287–1289. [Google Scholar] [CrossRef]
- Arena, R.; Myers, J.; Ozemek, C.; Hall, G.; Severin, R.; La.addu, D.; Kaminsky, L.A.; Stoner, L.; Conners, R.T.; Faghy, M.A.; et al. An Evolving Approach to Assessing Cardiorespiratory Fitness, Muscle Function and Bone and Joint Health in the COVID-19 Era. Curr. Probl. Cardiol. 2022, 47, 100879. [Google Scholar] [CrossRef]
- Fugazzaro, S.; Contri, A.; Esseroukh, O.; Kaleci, S.; Croci, S.; Massari, M.; Facciolongo, N.C.; Besutti, G.; Iori, M.; Salvarani, C.; et al. Rehabilitation Interventions for Post-Acute COVID-19 Syndrome: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5185. [Google Scholar] [CrossRef]
- Lloyd-Evans, P.H.I.; Baldwin, M.M.; Daynes, E.; Hong, A.; Mills, G.; Goddard, A.C.N.; Chaplin, E.; Gardiner, N.; Singh, S.J.; Your, C.R.D.G. Early experiences of the Your COVID Recovery((R)) digital programme for individuals with long COVID. BMJ Open Respir. Res. 2022, 9, e001237. [Google Scholar] [CrossRef]
- Philip, K.E.J.; Owles, H.; McVey, S.; Pagnuco, T.; Bruce, K.; Brunjes, H.; Banya, W.; Mollica, J.; Lound, A.; Zumpe, S.; et al. An online breathing and wellbeing programme (ENO Breathe) for people with persistent symptoms following COVID-19: A parallel-group, single-blind, randomised controlled trial. Lancet Respir. Med. 2022, 10, 851–862. [Google Scholar] [CrossRef]
- Batalik, L.; Dosbaba, F.; Hartman, M.; Konecny, V.; Batalikova, K.; Spinar, J. Long-term exercise effects after cardiac telerehabilitation in patients with coronary artery disease: 1-year follow-up results of the randomized study. Eur. J. Phys. Rehabil. Med. 2021, 57, 807–814. [Google Scholar] [CrossRef] [PubMed]
- Jimeno-Almazan, A.; Franco-Lopez, F.; Buendia-Romero, A.; Martinez-Cava, A.; Sanchez-Agar, J.A.; Sanchez-Alcaraz Martinez, B.J.; Courel-Ibanez, J.; Pallares, J.G. Rehabilitation for post-COVID-19 condition through a supervised exercise intervention: A randomized controlled trial. Scand. J. Med. Sci Sports 2022, 32, 1791–1801. [Google Scholar] [CrossRef] [PubMed]
- Nambi, G.; Abdelbasset, W.K.; Alrawaili, S.M.; Elsayed, S.H.; Verma, A.; Vellaiyan, A.; Eid, M.M.; Aldhafian, O.R.; Nwihadh, N.B.; Saleh, A.K. Comparative effectiveness study of low versus high-intensity aerobic training with resistance training in community-dwelling older men with post-COVID 19 sarcopenia: A randomized controlled trial. Clin. Rehabil. 2022, 36, 59–68. [Google Scholar] [CrossRef]
- Nagy, E.N.; Elimy, D.A.; Ali, A.Y.; Ezzelregal, H.G.; Elsayed, M.M. Influence of Manual Diaphragm Release Technique Combined with Inspiratory Muscle Training on Selected Persistent Symptoms in Men with Post-Covid-19 Syndrome: A Randomized Controlled Trial. J. Rehabil. Med. 2022, 54, jrm00330. [Google Scholar] [CrossRef]
- Brewer, L.C.; Jenkins, S.; Hayes, S.N.; Kumbamu, A.; Jones, C.; Burke, L.E.; Cooper, L.A.; Patten, C.A. Community-based, cluster-randomized pilot trial of a cardiovascular mHealth intervention: Rationale, design, and baseline findings of the FAITH! Trial. Am. Heart J. 2022, 247, 1–14. [Google Scholar] [CrossRef]
- Daynes, E.; Gerlis, C.; Chaplin, E.; Gardiner, N.; Singh, S.J. Early experiences of rehabilitation for individuals post-COVID to improve fatigue, breathlessness exercise capacity and cognition—A cohort study. Chron. Respir. Dis. 2021, 18, 14799731211015691. [Google Scholar] [CrossRef]
- Besnier, F.; Berube, B.; Malo, J.; Gagnon, C.; Gregoire, C.A.; Juneau, M.; Simard, F.; L’Allier, P.; Nigam, A.; Iglesies-Grau, J.; et al. Cardiopulmonary Rehabilitation in Long-COVID-19 Patients with Persistent Breathlessness and Fatigue: The COVID-Rehab Study. Int. J. Environ. Res. Public Health 2022, 19, 4133. [Google Scholar] [CrossRef]
- Nopp, S.; Moik, F.; Klok, F.A.; Gattinger, D.; Petrovic, M.; Vonbank, K.; Koczulla, A.R.; Ay, C.; Zwick, R.H. Outpatient Pulmonary Rehabilitation in Patients with Long COVID Improves Exercise Capacity, Functional Status, Dyspnea, Fatigue, and Quality of Life. Respiration 2022, 101, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Hockele, L.F.; Sachet Affonso, J.V.; Rossi, D.; Eibel, B. Pulmonary and Functional Rehabilitation Improves Functional Capacity, Pulmonary Function and Respiratory Muscle Strength in Post COVID-19 Patients: Pilot Clinical Trial. Int. J. Environ. Res. Public Health 2022, 19, 14899. [Google Scholar] [CrossRef]
- Novak, P.; Cunder, K.; Petrovic, O.; Oblak, T.; Dular, K.; Zupanc, A.; Prosic, Z.; Majdic, N. Rehabilitation of COVID-19 patients with respiratory failure and critical illness disease in Slovenia: An observational study. Int. J. Rehabil. Res. 2022, 45, 65–71. [Google Scholar] [CrossRef]
- Albu, S.; Rivas Zozaya, N.; Murillo, N.; Garcia-Molina, A.; Figueroa Chacon, C.A.; Kumru, H. Multidisciplinary outpatient rehabilitation of physical and neurological sequelae and persistent symptoms of COVID-19: A prospective, observational cohort study. Disabil. Rehabil. 2022, 44, 6833–6840. [Google Scholar] [CrossRef] [PubMed]
- Ogonowska-Slodownik, A.; Labecka, M.K.; Kaczmarczyk, K.; McNamara, R.J.; Starczewski, M.; Gajewski, J.; Maciejewska-Skrendo, A.; Morgulec-Adamowicz, N. Water-Based and Land-Based Exercise for Children with Post-COVID-19 Condition (postCOVIDkids)-Protocol for a Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 14476. [Google Scholar] [CrossRef] [PubMed]
- Turan, Z.; Topaloglu, M.; Ozyemisci Taskiran, O. Is tele-rehabilitation superior to home exercise program in COVID-19 survivors following discharge from intensive care unit?—A study protocol of a randomized controlled trial. Physiother. Res. Int. 2021, 26, e1920. [Google Scholar] [CrossRef] [PubMed]
- Si, M.Y.; Xiao, W.J.; Pan, C.; Wang, H.; Huang, Y.M.; Lian, J.; Mak, W.W.S.; Leng, Z.W.; Su, X.Y.; Tang, Q.P.; et al. Mindfulness-based online intervention on mental health and quality of life among COVID-19 patients in China: An intervention design. Infect. Dis. Poverty 2021, 10, 69. [Google Scholar] [CrossRef]
- Rutsch, M.; Frommhold, J.; Buhr-Schinner, H.; Djeiranachvili, L.; Gross, T.; Schuller, P.O.; Katalinic, A.; Deck, R. Study protocol medical rehabilitation after COVID-19 disease: An observational study with a comparison group with obstructive airway disease/Re_Co. BMC Health Serv. Res. 2021, 21, 373. [Google Scholar] [CrossRef]
- McGregor, G.; Sandhu, H.; Bruce, J.; Sheehan, B.; McWilliams, D.; Yeung, J.; Jones, C.; Lara, B.; Smith, J.; Ji, C.; et al. Rehabilitation Exercise and psycholoGical support After COVID-19 InfectioN’ (REGAIN): A structured summary of a study protocol for a randomised controlled trial. Trials 2021, 22, 8. [Google Scholar] [CrossRef]
- Lira, F.S.; Pereira, T.; Guerra Minuzzi, L.; Figueiredo, C.; Olean-Oliveira, T.; Figueira Freire, A.P.C.; Coelho, E.S.M.J.; Caseiro, A.; Thomatieli-Santos, R.V.; Dos Santos, V.R.; et al. Modulatory Effects of Physical Activity Levels on Immune Responses and General Clinical Functions in Adult Patients with Mild to Moderate SARS-CoV-2 Infections-A Protocol for an Observational Prospective Follow-Up Investigation: Fit-COVID-19 Study. Int. J. Environ. Res. Public Health 2021, 18, 13249. [Google Scholar] [CrossRef]
- Carvalho, A.C.; Moreira, J.; Cubelo, P.; Cantista, P.; Aguiar Branco, C.; Guimaraes, B. Multidisciplinary rehabilitation in intensive care for COVID-19: Randomised controlled trial. ERJ Open Res. 2023, 9, 00350–2022. [Google Scholar] [CrossRef]
- Piotrowicz, K.; Gasowski, J.; Michel, J.P.; Veronese, N. Post-COVID-19 acute sarcopenia: Physiopathology and management. Aging Clin. Exp. Res. 2021, 33, 2887–2898. [Google Scholar] [CrossRef]
- Liu, K.; Zhang, W.; Yang, Y.; Zhang, J.; Li, Y.; Chen, Y. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement. Ther. Clin. Pract. 2020, 39, 101166. [Google Scholar] [CrossRef]
- Rooney, S.; Webster, A.; Paul, L. Systematic Review of Changes and Recovery in Physical Function and Fitness After Severe Acute Respiratory Syndrome-Related Coronavirus Infection: Implications for COVID-19 Rehabilitation. Phys. Ther. 2020, 100, 1717–1729. [Google Scholar] [CrossRef] [PubMed]
- Barker-Davies, R.M.; O’Sullivan, O.; Senaratne, K.P.P.; Baker, P.; Cranley, M.; Dharm-Datta, S.; Ellis, H.; Goodall, D.; Gough, M.; Lewis, S.; et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br. J. Sports Med. 2020, 54, 949–959. [Google Scholar] [CrossRef]
- Wang, T.J.; Chau, B.; Lui, M.; Lam, G.T.; Lin, N.; Humbert, S. Physical Medicine and Rehabilitation and Pulmonary Rehabilitation for COVID-19. Am. J. Phys. Med. Rehabil. 2020, 99, 769–774. [Google Scholar] [CrossRef]
- Rebello, C.J.; Axelrod, C.L.; Reynolds, C.F., 3rd; Greenway, F.L.; Kirwan, J.P. Exercise as a Moderator of Persistent Neuroendocrine Symptoms of COVID-19. Exerc Sport Sci Rev. 2022, 50, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Raveendran, A.V.; Misra, A. Post COVID-19 Syndrome (“Long COVID”) and Diabetes: Challenges in Diagnosis and Management. Diabetes Metab. Syndr. 2021, 15, 102235. [Google Scholar] [CrossRef]
- Fumagalli, C.; Zocchi, C.; Tassetti, L.; Silverii, M.V.; Amato, C.; Livi, L.; Giovannoni, L.; Verrillo, F.; Bartoloni, A.; Marcucci, R.; et al. Factors associated with persistence of symptoms 1 year after COVID-19: A longitudinal, prospective phone-based interview follow-up cohort study. Eur. J. Intern. Med. 2022, 97, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Storz, M.A. Lifestyle Adjustments in Long-COVID Management: Potential Benefits of Plant-Based Diets. Curr. Nutr. Rep. 2021, 10, 352–363. [Google Scholar] [CrossRef]
- Harenwall, S.; Heywood-Everett, S.; Henderson, R.; Godsell, S.; Jordan, S.; Moore, A.; Philpot, U.; Shepherd, K.; Smith, J.; Bland, A.R. Post-Covid-19 Syndrome: Improvements in Health-Related Quality of Life Following Psychology-Led Interdisciplinary Virtual Rehabilitation. J. Prim. Care Community Health 2021, 12, 21501319211067674. [Google Scholar] [CrossRef]
- Sansone, A.; Mollaioli, D.; Limoncin, E.; Ciocca, G.; Bac, N.H.; Cao, T.N.; Hou, G.; Yuan, J.; Zitzmann, M.; Giraldi, A.; et al. The Sexual Long COVID (SLC): Erectile Dysfunction as a Biomarker of Systemic Complications for COVID-19 Long Haulers. Sex. Med. Rev. 2022, 10, 271–285. [Google Scholar] [CrossRef]
- Morrow, A.K.; Ng, R.; Vargas, G.; Jashar, D.T.; Henning, E.; Stinson, N.; Malone, L.A. Postacute/Long COVID in Pediatrics: Development of a Multidisciplinary Rehabilitation Clinic and Preliminary Case Series. Am. J. Phys. Med. Rehabil. 2021, 100, 1140–1147. [Google Scholar] [CrossRef]
- Sarfraz, Z.; Sarfraz, A.; Barrios, A.; Garimella, R.; Dominari, A.; Kc, M.; Pandav, K.; Pantoja, J.C.; Retnakumar, V.; Cherrez-Ojeda, I. Cardio-Pulmonary Sequelae in Recovered COVID-19 Patients: Considerations for Primary Care. J. Prim. Care Community Health 2021, 12, 21501327211023726. [Google Scholar] [CrossRef]
- Moghimi, N.; Di Napoli, M.; Biller, J.; Siegler, J.E.; Shekhar, R.; McCullough, L.D.; Harkins, M.S.; Hong, E.; Alaouieh, D.A.; Mansueto, G.; et al. The Neurological Manifestations of Post-Acute Sequelae of SARS-CoV-2 infection. Curr. Neurol. Neurosci. Rep. 2021, 21, 44. [Google Scholar] [CrossRef]
- Romaszko-Wojtowicz, A.; Maksymowicz, S.; Jarynowski, A.; Jaskiewicz, L.; Czekaj, L.; Doboszynska, A. Telemonitoring in Long-COVID Patients-Preliminary Findings. Int. J. Environ. Res. Public Health 2022, 19, 5268. [Google Scholar] [CrossRef] [PubMed]
- Rashid, A. Yonder: Long Covid, mental health video consultations, overactive bladder syndrome, and haematological malignancies. Br. J. Gen. Pract. 2020, 70, 601. [Google Scholar] [CrossRef]
- Day, H.L.S. Exploring Online Peer Support Groups for Adults Experiencing Long COVID in the United Kingdom: Qualitative Interview Study. J. Med. Internet Res. 2022, 24, e37674. [Google Scholar] [CrossRef]
- Fernandez-de-Las-Penas, C.; Florencio, L.L.; Gomez-Mayordomo, V.; Cuadrado, M.L.; Palacios-Cena, D.; Raveendran, A.V. Proposed integrative model for post-COVID symptoms. Diabetes Metab. Syndr. 2021, 15, 102159. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Ramirez, D.C.; Normand, K.; Zhaoyun, Y.; Torres-Castro, R. Long-Term Impact of COVID-19: A Systematic Review of the Literature and Meta-Analysis. Biomedicines 2021, 9, 900. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, I.; Bin Inam, A.; Belli, S.; Ahmad, J.; Khalil, W.; Jafar, M.M. Effectiveness of aerobic exercise training program on cardio-respiratory fitness and quality of life in patients recovered from COVID-19. Eur. J. Physiother. 2022, 24, 358–363. [Google Scholar] [CrossRef]
- Ferraro, F.; Calafiore, D.; Dambruoso, F.; Guidarini, S.; de Sire, A. COVID-19 related fatigue: Which role for rehabilitation in post-COVID-19 patients? A case series. J. Med. Virol. 2021, 93, 1896–1899. [Google Scholar] [CrossRef] [PubMed]
- Tozato, C.; Ferreira, B.F.C.; Dalavina, J.P.; Molinari, C.V.; Alves, V. Cardiopulmonary rehabilitation in post-COVID-19 patients: Case series. Rev. Bras. Ter. Intensiv. 2021, 33, 167–171. [Google Scholar] [CrossRef]
- Wootton, S.L.; King, M.; Alison, J.A.; Mahadev, S.; Chan, A.S.L. COVID-19 rehabilitation delivered via a telehealth pulmonary rehabilitation model: A case series. Respirol. Case Rep. 2020, 8, e00669. [Google Scholar] [CrossRef]
- Bickton, F.M.; Chisati, E.; Rylance, J.; Morton, B. An Improvised Pulmonary Telerehabilitation Program for Postacute COVID-19 Patients Would Be Feasible and Acceptable in a Low-Resource Setting. Am. J. Phys. Med. Rehabil. 2021, 100, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Ayoubkhani, D.; Bermingham, C.; Pouwels, K.B.; Glickman, M.; Nafilyan, V.; Zaccardi, F.; Khunti, K.; Alwan, N.A.; Walker, A.S. Trajectory of long covid symptoms after COVID-19 vaccination: Community based cohort study. BMJ 2022, 377, e069676. [Google Scholar] [CrossRef] [PubMed]
- Tsuchida, T.; Hirose, M.; Inoue, Y.; Kunishima, H.; Otsubo, T.; Matsuda, T. Relationship between changes in symptoms and antibody titers after a single vaccination in patients with Long COVID. J. Med. Virol. 2022, 94, 3416–3420. [Google Scholar] [CrossRef] [PubMed]
- Al-Aly, Z.; Bowe, B.; Xie, Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat. Med. 2022, 28, 1461–1467. [Google Scholar] [CrossRef]
- Antonelli, M.; Penfold, R.S.; Merino, J.; Sudre, C.H.; Molteni, E.; Berry, S.; Canas, L.S.; Graham, M.S.; Klaser, K.; Modat, M.; et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: A prospective, community-based, nested, case-control study. Lancet Infect. Dis. 2022, 22, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Mendelsohn, A.S.; Nath, N.; De Sa, A.; Von Pressentin, K.B. Two months follow-up of patients with non-critical COVID-19 in Cape Town, South Africa. S. Afr. Fam. Pract. (2004) 2022, 64, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Shapira, S.; Yeshua-Katz, D.; Goren, G.; Aharonson-Daniel, L.; Clarfield, A.M.; Sarid, O. Evaluation of a Short-Term Digital Group Intervention to Relieve Mental Distress and Promote Well-Being Among Community-Dwelling Older Individuals During the COVID-19 Outbreak: A Study Protocol. Front. Public Health 2021, 9, 577079. [Google Scholar] [CrossRef]
- Murray, E.; Goodfellow, H.; Bindman, J.; Blandford, A.; Bradbury, K.; Chaudhry, T.; Fernandez-Reyes, D.; Gomes, M.; Hamilton, F.L.; Heightman, M.; et al. Development, deployment and evaluation of digitally enabled, remote, supported rehabilitation for people with long COVID-19 (Living With COVID-19 Recovery): Protocol for a mixed-methods study. BMJ Open 2022, 12, e057408. [Google Scholar] [CrossRef]
- Gomes, M.; Murray, E.; Raftery, J. Economic Evaluation of Digital Health Interventions: Methodological Issues and Recommendations for Practice. Pharmacoeconomics 2022, 40, 367–378. [Google Scholar] [CrossRef]
- Adeloye, D.; Elneima, O.; Daines, L.; Poinasamy, K.; Quint, J.K.; Walker, S.; Brightling, C.E.; Siddiqui, S.; Hurst, J.R.; Chalmers, J.D.; et al. The long-term sequelae of COVID-19: An international consensus on research priorities for patients with pre-existing and new-onset airways disease. Lancet Respir. Med. 2021, 9, 1467–1478. [Google Scholar] [CrossRef] [PubMed]
- Deer, R.R.; Rock, M.A.; Vasilevsky, N.; Carmody, L.; Rando, H.; Anzalone, A.J.; Basson, M.D.; Bennett, T.D.; Bergquist, T.; Boudreau, E.A.; et al. Characterizing Long COVID: Deep Phenotype of a Complex Condition. EBioMedicine 2021, 74, 103722. [Google Scholar] [CrossRef] [PubMed]
- Raveendran, A.V. Long COVID-19: Challenges in the diagnosis and proposed diagnostic criteria. Diabetes Metab. Syndr. 2021, 15, 145–146. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).