Effectiveness of Nickel–Titanium Files for Retreatment of Molars Filled with Single-Cone Hydraulic Technique Using Bioceramic Sealers: An In Vitro Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Selection of Teeth
2.2. Root Canal Preparation and Obturation
2.3. Endodontic Retreatment and Group Designation
2.4. Scanning Electron Microscope (SEM) Evaluation
2.5. Statistical Analysis
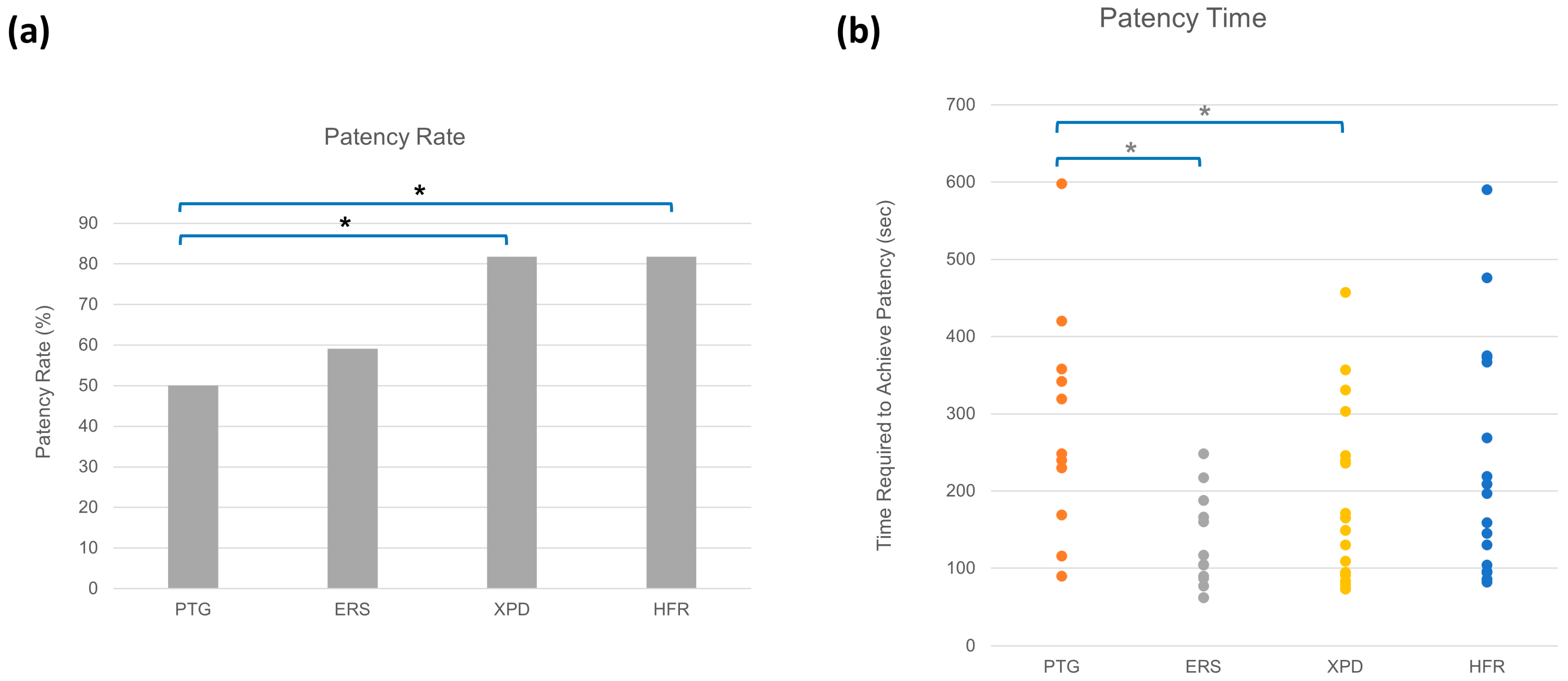
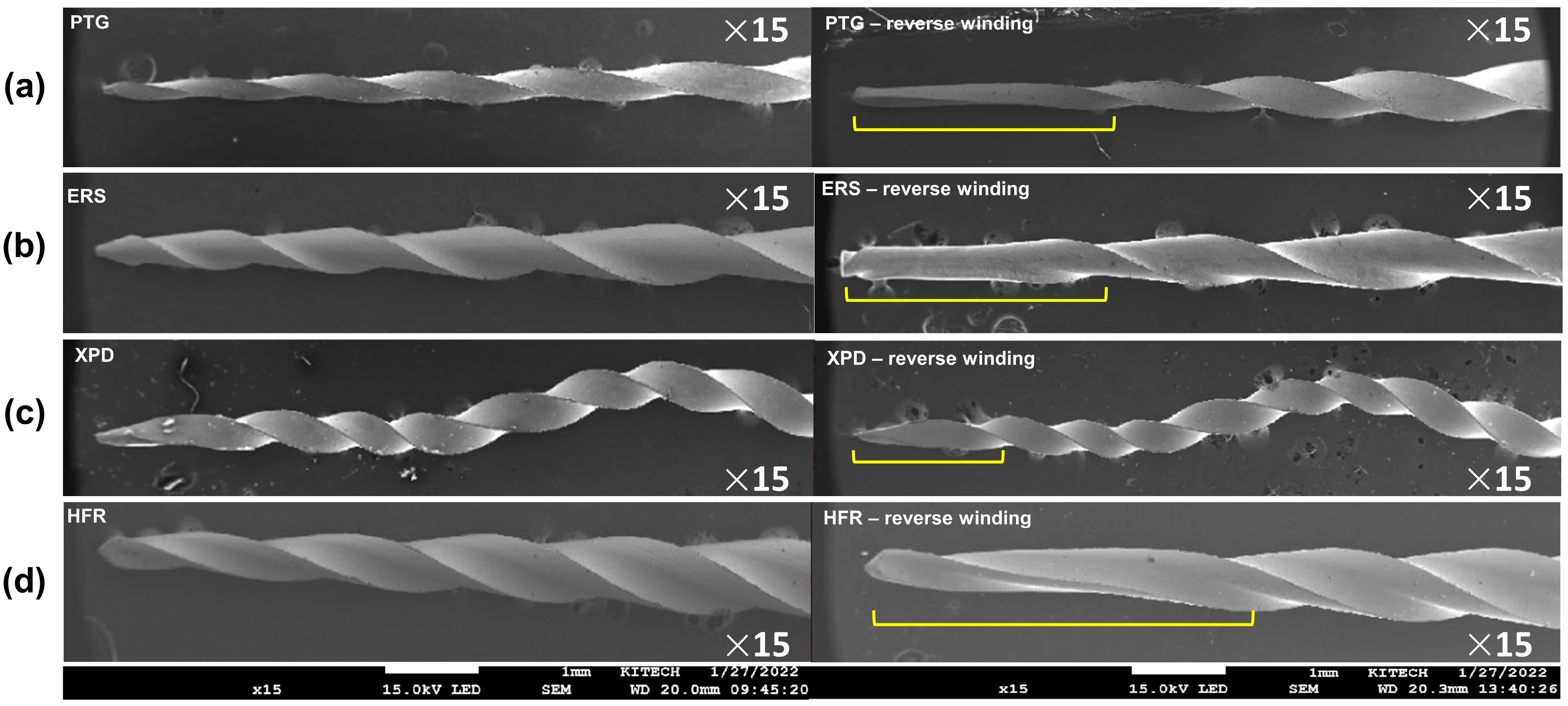
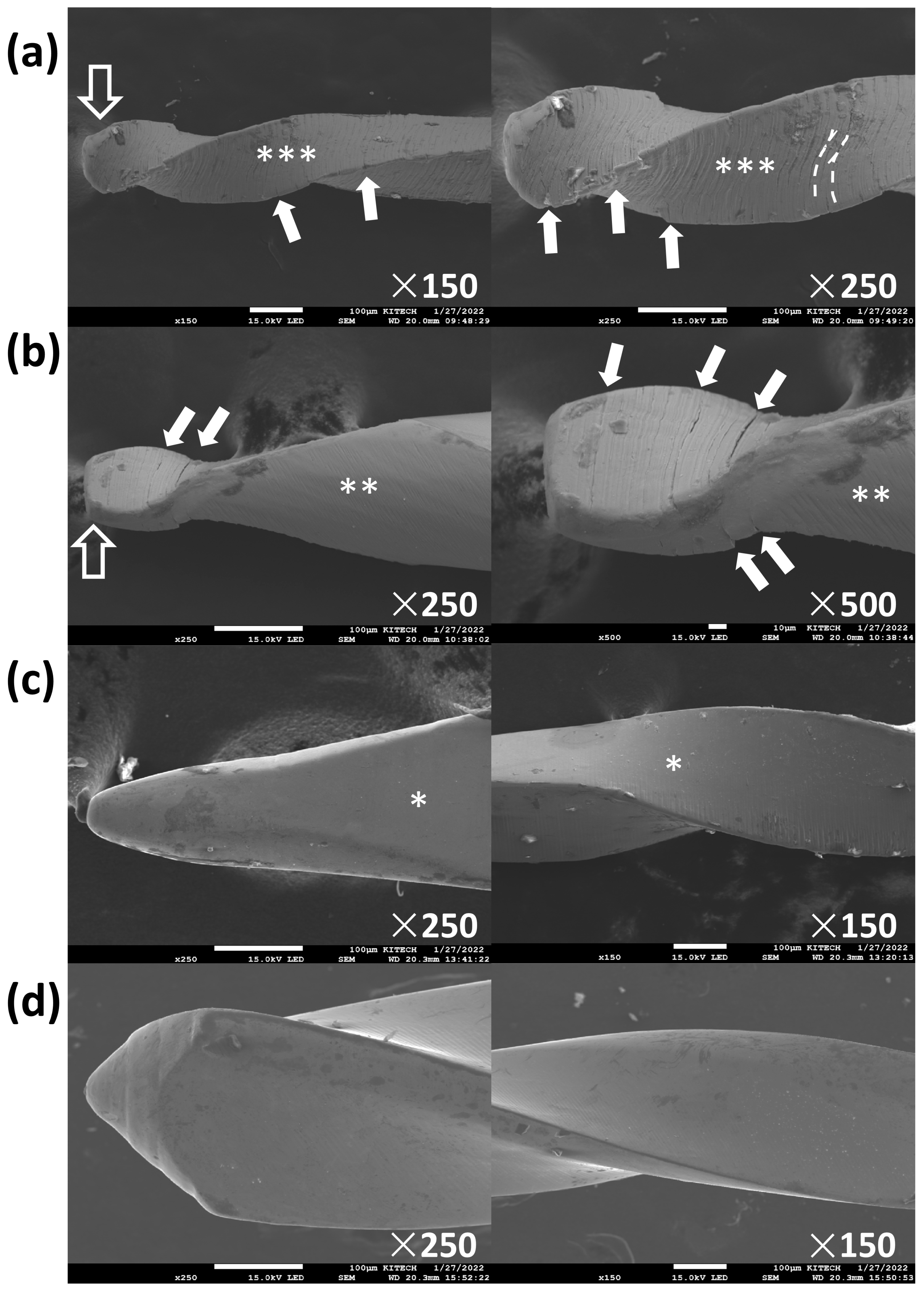
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Retx | retreatment |
| GP | gutta-percha |
| BCSs | bioceramic root canal sealers |
| NiTi | nickel–titanium |
| PTG | ProTaper Gold |
| ERS | Endo ReStart |
| XPD | XP Endo 3D Shaper |
| HFR | HyFlex Remover |
References
- Sundqvist, G.; Figdor, D.; Persson, S.; Sjogren, U. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative re-treatment. Oral Sur. Oral Med. Oral Pathol. Oral Radiol. Endod. 1988, 85, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Friedman, S.; Stabholz, A.; Tamse, A. Endodontic retreatment—Case selection and technique. Part 3. Retreatment techniques. J. Endod. 1990, 16, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Unal, G.C.; Kaya, B.U.; Tac, A.G.; Kececi, A.D. A comparison of the efficacy of conventional and new retreatment instruments to remove gutta-percha in curved root canals: An ex vivo study. Int. Endod. J. 2009, 42, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Guivarc’h, M.; Jeanneau, C.; Giraud, T.; Pommel, L.; About, I.; Azim, A.A.; Bukiet, F. An international survey on the use of calcium silicate-based sealers in non-surgical endodontic treatment. Clin. Oral Investig. 2020, 24, 417–424. [Google Scholar] [CrossRef]
- Chang, S.W.; Lee, S.Y.; Kang, S.K.; Kum, K.Y.; Kim, E.C. In vitro biocompatibility, inflammatory response, and osteogenic potential of 4 root canal sealers: Sealapex, Sankin apatite root sealer, MTA Fillapex, and iRoot SP root canal sealer. J. Endod. 2014, 40, 1642–1648. [Google Scholar] [CrossRef]
- Xue, K.; Hu, G.; Wu, L.; Han, H.; Sun, Y.; Gan, K.; Zhu, J.; Du, T. The bioceramic sealer iRoot SP promotes osteogenic differentiation of human stem cells from apical papilla via miR-141-3p/SPAG9/MAPK signalling pathway. Int. Endod. J. 2023, 56, 1241–1253. [Google Scholar] [CrossRef]
- Yang, R.; Tian, J.; Huang, X.; Lei, S.; Cai, Y.; Xu, Z.; Wei, X. A comparative study of dentinal tubule penetration and the retreatability of EndoSequence BC Sealer HiFlow, iRoot SP, and AH Plus with different obturation techniques. Clin. Oral Investig. 2021, 25, 4163–4173. [Google Scholar] [CrossRef]
- Chybowski, E.A.; Glickman, G.N.; Patel, Y.; Fleury, A.; Solomon, E.; He, J. Clinical outcome of non-surgical root canal treatment using a single-cone technique with Endosequence Bioceramic sealer: A retrospective analysis. J. Endod. 2018, 44, 941–945. [Google Scholar] [CrossRef]
- Zavattini, A.; Knight, A.; Foschi, F.; Mannocci, F. Outcome of root canal treatments using a new calcium silicate root canal sealer: A non-randomized clinical trial. J. Clin. Med. 2020, 9, 782. [Google Scholar] [CrossRef]
- Romeiro, K.; de Almeida, A.; Cassimiro, M.; Gominho, L.; Dantas, E.; Chagas, N.; Velozo, C.; Freire, L.; Albuquerque, D. Reciproc and Reciproc Blue in the removal of bioceramic and resin-based sealers in retreatment procedures. Clin. Oral Investig. 2020, 24, 405–416. [Google Scholar] [CrossRef]
- Agrafioti, A.; Koursoumis, A.D.; Kontakiotis, E.G. Re-establishing apical patency after obturation with Gutta-percha and two novel calcium silicate-based sealers. Eur. J. Dent. 2015, 9, 457–461. [Google Scholar] [CrossRef] [PubMed]
- Hess, D.; Solomon, E.; Spears, R.; He, J. Retreatability of a bioceramic root canal sealing material. J. Endod. 2011, 37, 1547–1549. [Google Scholar] [CrossRef] [PubMed]
- Ng, Y.L.; Mann, V.; Gulabivala, K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1: Periapical health. Int. Endod. J. 2011, 44, 583–609. [Google Scholar] [CrossRef]
- Garrib, M.; Camilleri, J. Retreatment efficacy of hydraulic calcium silicate sealers used in single cone obturation. J. Dent. 2020, 98, 103370. [Google Scholar] [CrossRef] [PubMed]
- Rezaei, G.; Liu, X.; Jalali, P. Efficacy of different Solvents for achieving patency in teeth obturated using bioceramic sealer. J. Endod. 2023, 49, 219–223. [Google Scholar] [CrossRef]
- Carrillo, C.A.; Kirkpatrick, T.; Freeman, K.; Makins, S.R.; Aldabbagh, M.; Jeong, J.W. Retrievability of calcium silicate-based root canal sealers during retreatment: An ex vivo study. J. Endod. 2022, 48, 781–786. [Google Scholar] [CrossRef]
- Kaval, M.E.; Capar, I.D.; Ertas, H. Evaluation of the cyclic fatigue and torsional resistance of novel nickel-titanium rotary files with various alloy properties. J. Endod. 2016, 42, 1840–1843. [Google Scholar] [CrossRef]
- Silva, E.; Vieira, V.T.L.; Hecksher, F.; Dos Santos Oliveira, M.R.S.; Dos Santos Antunes, H.; Moreira, E.J.L. Cyclic fatigue using severely curved canals and torsional resistance of thermally treated reciprocating instruments. Clin. Oral Investig. 2018, 22, 2633–2638. [Google Scholar] [CrossRef]
- Rodig, T.; Reicherts, P.; Konietschke, F.; Dullin, C.; Hahn, W.; Hulsmann, M. Efficacy of reciprocating and rotary NiTi instruments for retreatment of curved root canals assessed by micro-CT. Int. Endod. J. 2014, 47, 942–948. [Google Scholar] [CrossRef]
- Schneider, S.W. A comparison of canal preparations in straight and curved root canals. Oral Surg. Oral Med. Oral Pathol. 1971, 32, 271–275. [Google Scholar] [CrossRef]
- Crozeta, B.M.; Lopes, F.C.; Menezes Silva, R.; Silva-Sousa, Y.T.C.; Moretti, L.F.; Sousa-Neto, M.D. Retreatability of BC Sealer and AH Plus root canal sealers using new supplementary instrumentation protocol during non-surgical endodontic retreatment. Clin. Oral Investig. 2021, 25, 891–899. [Google Scholar] [CrossRef] [PubMed]
- Hassan, R.; Elzahar, S. Cleaning efficiency of XP Finisher, XP Finisher R and passive ultrasonic irrigation following retreatment of teeth obturated with TotalFill HiFlow bioceramic sealer. Eur. Endod. J. 2022, 7, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Mamootil, K.; Messer, H.H. Penetration of dentinal tubules by endodontic sealer cements in extracted teeth and in vivo. Int. Endod. J. 2007, 40, 873–881. [Google Scholar] [CrossRef]
- Gergi, R.; Sabbagh, C. Effectiveness of two nickel-titanium rotary instruments and a hand file for removing gutta-percha in severely curved root canals during retreatment: An ex vivo study. Int. Endod. J. 2007, 40, 532–537. [Google Scholar] [CrossRef] [PubMed]
- Goo, H.J.; Kwak, S.W.; Ha, J.H.; Pedulla, E.; Kim, H.C. Mechanical properties of various heat-treated nickel-titanium rotary instruments. J. Endod. 2017, 43, 1872–1877. [Google Scholar] [CrossRef]
- Lopes, H.P.; Elias, C.N.; Vedovello, G.A.; Bueno, C.E.; Mangelli, M.; Siqueira, J.F., Jr. Torsional resistance of retreatment instruments. J. Endod. 2011, 37, 1442–1445. [Google Scholar] [CrossRef]
- Ha, J.H.; Kim, S.R.; Versluis, A.; Cheung, G.S.; Kim, J.W.; Kim, H.C. Elastic limits in torsion of reciprocating nickel-titanium instruments. J. Endod. 2015, 41, 715–719. [Google Scholar] [CrossRef]
- Silva, E.; Vieira, V.T.L.; Belladonna, F.G.; Zuolo, A.S.; Antunes, H.D.S.; Cavalcante, D.M.; Elias, C.N.; De-Deus, G. Cyclic and torsional fatigue resistance of XP-endo Shaper and TRUShape instruments. J. Endod. 2018, 44, 168–172. [Google Scholar] [CrossRef]
- Thomas, J.P.; Lynch, M.; Paurazas, S.; Askar, M. Micro-computed tomographic evaluation of the shaping ability of WaveOne Gold, TRUShape, EdgeCoil, and XP-3D Shaper endodontic files in single, oval-shaped canals: An in vitro study. J. Endod. 2020, 46, 244–251.e1. [Google Scholar] [CrossRef]
- Fife, D.; Gambarini, G.; Britto, L.R. Cyclic fatigue testing of ProTaper NiTi rotary instruments after clinical use. Oral Sur. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 97, 251–256. [Google Scholar] [CrossRef]
- Grande, N.M.; Plotino, G.; Pecci, R.; Bedini, R.; Malagnino, V.A.; Somma, F. Cyclic fatigue resistance and three-dimensional analysis of instruments from two nickel-titanium rotary systems. Int. Endod. J. 2006, 39, 755–763. [Google Scholar] [CrossRef] [PubMed]
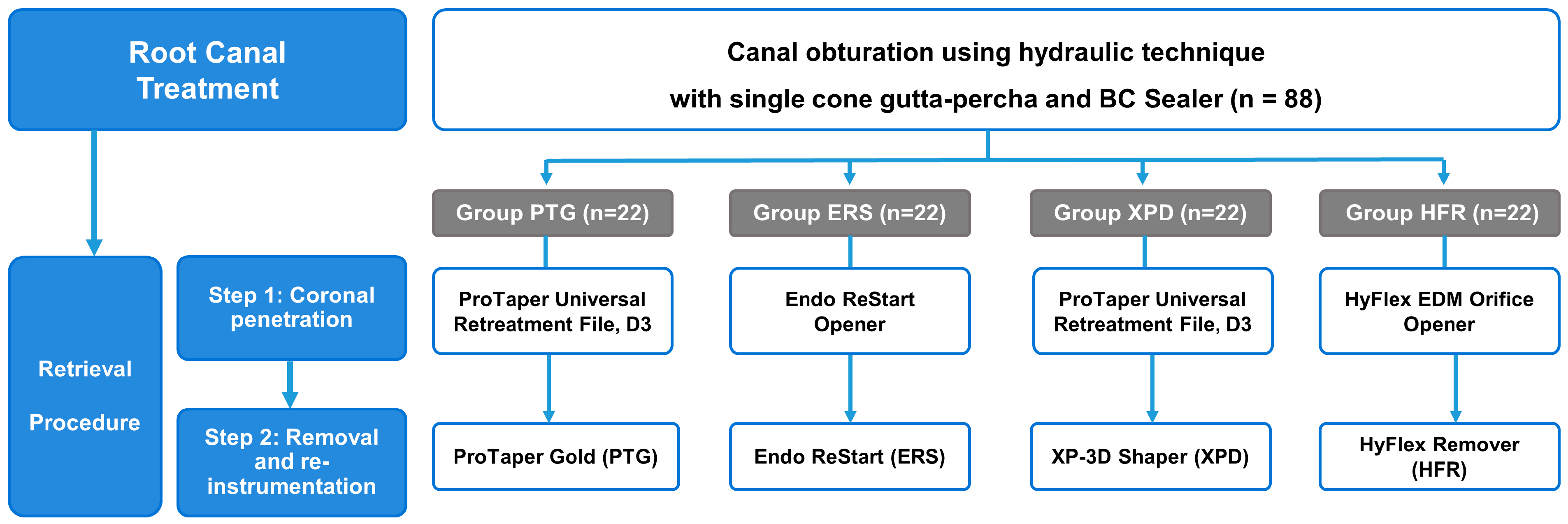
| Group | Step 1: Coronal Penetration | rpm, Ncm | Step 2: Obturation Material Removal | rpm, Ncm |
|---|---|---|---|---|
| PTG | ProTaper Universal Retreatment, D3 (#20/0.07) | 700, 3 | ProTaper Gold, S1 (#18/0.02–0.11) | 700, 3 |
| ERS | Endo ReStart Opener (#30/0.10) | 700, 2.5 | Endo ReStart (#25/0.05) | 700, 2.5 |
| XPD | ProTaper Universal Retreatment, D3 (#20/0.07) | 700, 3 | XP-3D Shaper (#30/0.02–0.08) | 1200, 3 |
| HFR | HyFlex EDM Orifice Opener (#25/0.12) | 700, 2.5 | HyFlex Remover (#30/0.07) | 700, 2.5 |
| Frequency of Mechanical Alterations | |||
|---|---|---|---|
| Group (n = 22) | Reverse Winding | Microcrack | Broken Tip |
| PTG | 10 | 4 | 9 |
| ERS | 1 | 1 | 1 |
| XPD | 6 | 0 | 0 |
| HFR | 5 | 0 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Kim, H.-C.; Kirkpatrick, T.; Jaramillo, D.E.; Kwak, S.W.; Jeong, J.W. Effectiveness of Nickel–Titanium Files for Retreatment of Molars Filled with Single-Cone Hydraulic Technique Using Bioceramic Sealers: An In Vitro Study. Materials 2025, 18, 1265. https://doi.org/10.3390/ma18061265
Lee J, Kim H-C, Kirkpatrick T, Jaramillo DE, Kwak SW, Jeong JW. Effectiveness of Nickel–Titanium Files for Retreatment of Molars Filled with Single-Cone Hydraulic Technique Using Bioceramic Sealers: An In Vitro Study. Materials. 2025; 18(6):1265. https://doi.org/10.3390/ma18061265
Chicago/Turabian StyleLee, Jane, Hyeon-Cheol Kim, Timothy Kirkpatrick, David E. Jaramillo, Sang Won Kwak, and Ji Wook Jeong. 2025. "Effectiveness of Nickel–Titanium Files for Retreatment of Molars Filled with Single-Cone Hydraulic Technique Using Bioceramic Sealers: An In Vitro Study" Materials 18, no. 6: 1265. https://doi.org/10.3390/ma18061265
APA StyleLee, J., Kim, H.-C., Kirkpatrick, T., Jaramillo, D. E., Kwak, S. W., & Jeong, J. W. (2025). Effectiveness of Nickel–Titanium Files for Retreatment of Molars Filled with Single-Cone Hydraulic Technique Using Bioceramic Sealers: An In Vitro Study. Materials, 18(6), 1265. https://doi.org/10.3390/ma18061265







