A Group Intervention to Promote Resilience in Nursing Professionals: A Randomised Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedure and Recruitment
2.2. Outcome Measures
2.3. Intervention
2.4. Statistical Analysis
3. Results
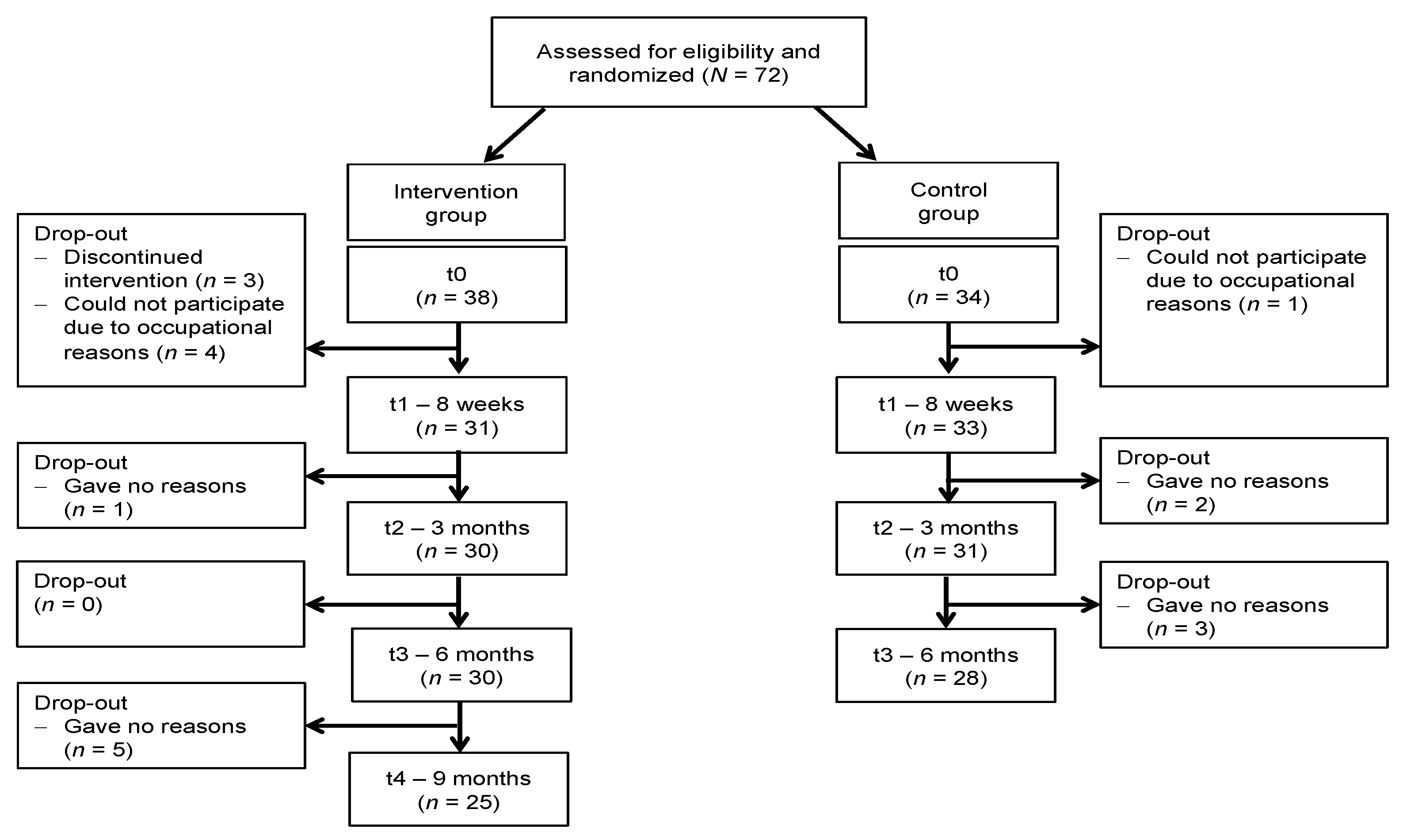
3.1. Participants
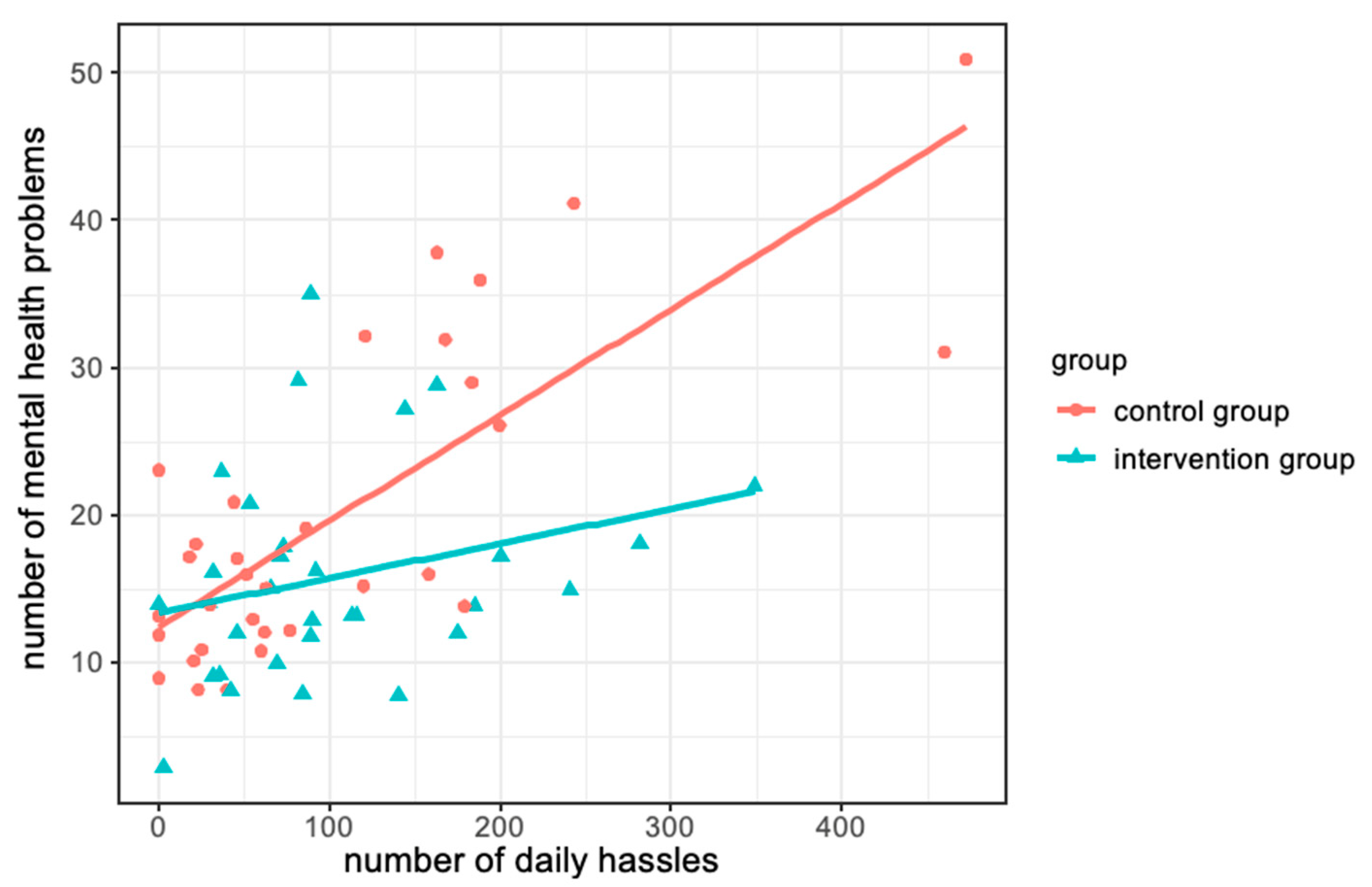
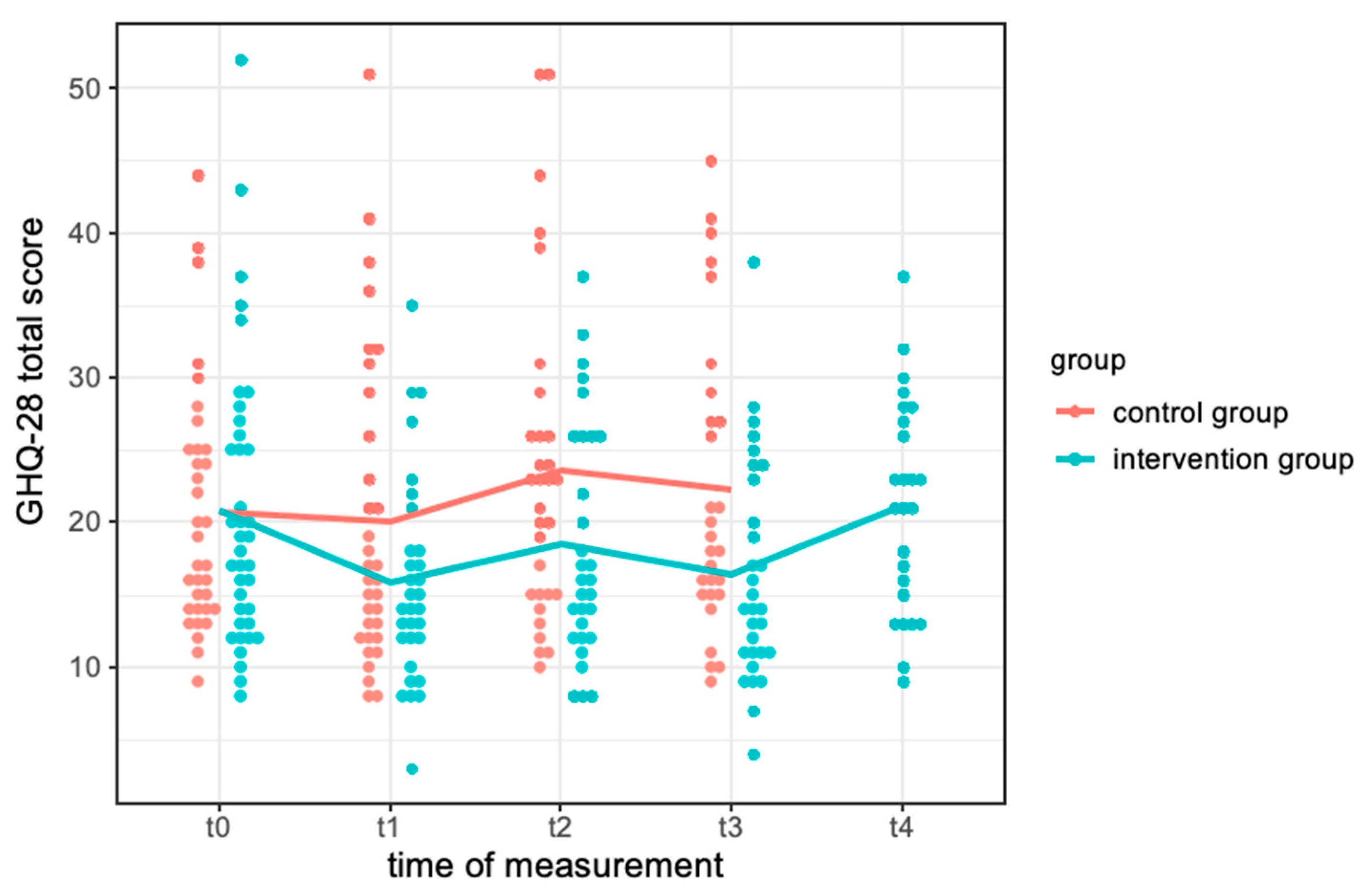
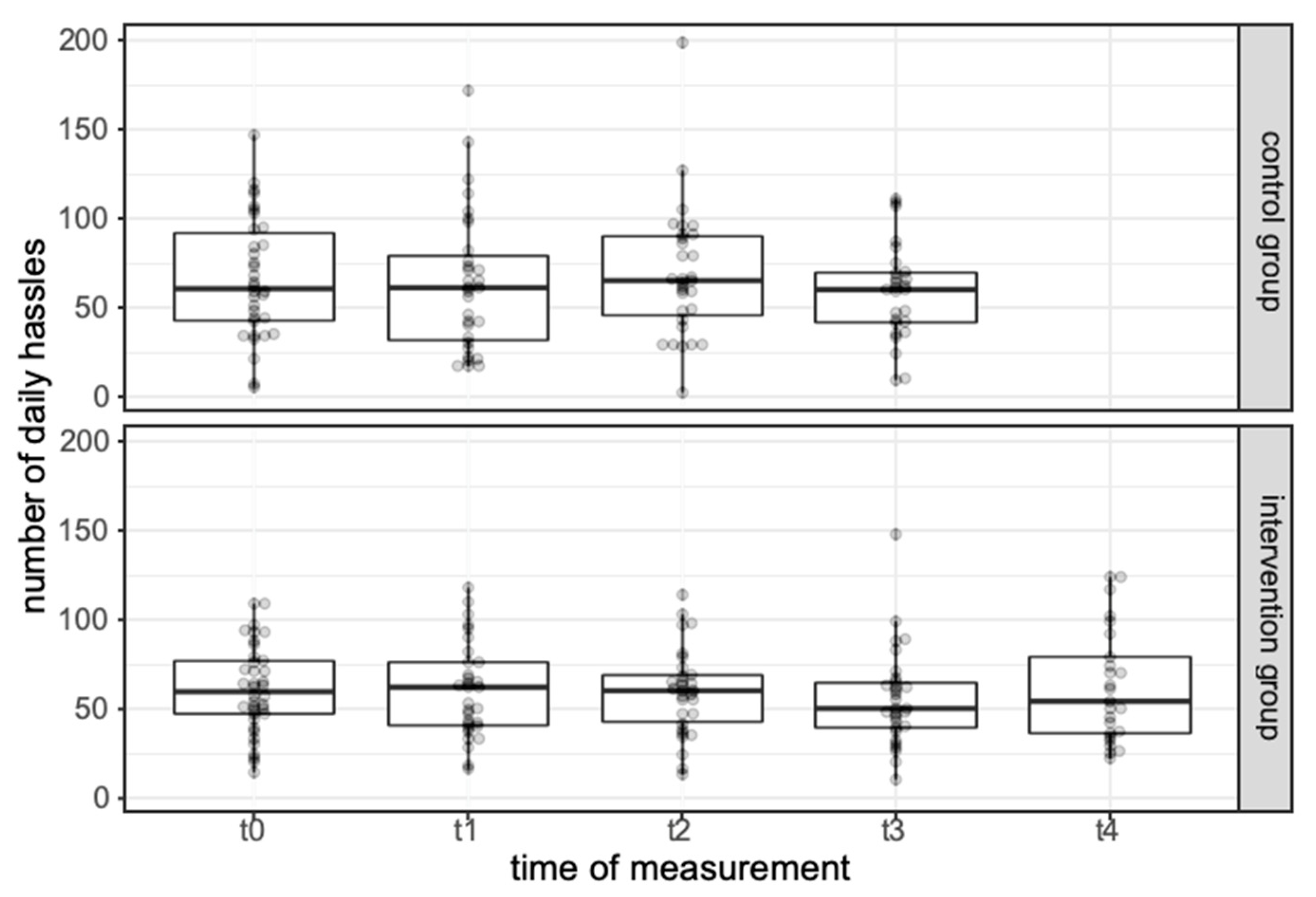
3.2. Primary Outcome
3.3. Secondary Outcomes
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Topic | Training Content |
|---|---|
| Week 1. The starting point: get to know resilience and understand your problems |
|
| Week 2. On the way to resilience: give up maladaptive behaviour and set new goals |
|
| Week 3. The resilient mind control: Train cognitive flexibility and coping skills |
|
| Week 4. Be a good friend to yourself: Train self-care and mindfulness |
|
| Week 5. Be resilient in tough times: Train self-efficacy and self-esteem |
|
| Week 6. Tackle the problem in a resilient way: Use resilience strategies for problem-solving (part 1) |
|
| Week 7. From problem analysis to solution design: Use resilience strategies for problem-solving (part 2) |
|
| Week 8. The new growth: Reflect on your own development |
|
Appendix B
References
- Hart, P.L.; Brannan, J.D.; De Chesnay, M. Resilience in nurses: An integrative review. J. Nurs. Manag. 2014, 22, 720–734. [Google Scholar] [CrossRef] [Green Version]
- World Health Organisation Nursing and Midwifery: Fact Sheet. Available online: https://www.who.int/news-room/fact-sheets/detail/nursing-and-midwifery (accessed on 14 November 2021).
- Keller, S.M.; Berryman, P.; Lukes, E. Effects of extended work shifts and shift work on patient safety, productivity, and employee health. Aaohn J. 2009, 57, 497–504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lo, W.Y.; Chien, L.Y.; Hwang, F.M.; Huang, N.; Chiou, S.T. From job stress to intention to leave among hospital nurses: A structural equation modelling approach. J. Adv. Nurs. 2018, 74, 677–688. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Cheng, B.; Zhu, X.P. Quantification of burnout in emergency nurses: A systematic review and meta-analysis. Int. Emerg. Nurs. 2018, 39, 46–54. [Google Scholar] [CrossRef]
- Ross, C.A.; Berry, N.S.; Smye, V.; Goldner, E.M. A critical review of knowledge on nurses with problematic substance use: The need to move from individual blame to awareness of structural factors. Nurs. Inq. 2018, 25, e12215. [Google Scholar] [CrossRef]
- Booker, L.A.; Sletten, T.L.; Alvaro, P.K.; Barnes, M.; Collins, A.; Chai-Coetzer, C.L.; Naqvi, A.; McMahon, M.; Lockley, S.W.; Rajaratnam, S.M. Exploring the associations between shift work disorder, depression, anxiety and sick leave taken amongst nurses. J. Sleep Res. 2020, 29, e12872. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Lee, E.; Lee, H. Association between workplace bullying and burnout, professional quality of life, and turnover intention among clinical nurses. PLoS ONE 2019, 14, e0226506. [Google Scholar] [CrossRef]
- Salyers, M.P.; Bonfils, K.A.; Luther, L.; Firmin, R.L.; White, D.A.; Adams, E.L.; Rollins, A.L. The relationship between professional burnout and quality and safety in healthcare: A meta-analysis. J. Gen. Intern. Med. 2017, 32, 475–482. [Google Scholar] [CrossRef]
- Yu, F.; Raphael, D.; Mackay, L.; Smith, M.; King, A. Personal and work-related factors associated with nurse resilience: A systematic review. Int. J. Nurs. Stud. 2019, 93, 129–140. [Google Scholar] [CrossRef]
- Bonanno, G.A.; Diminich, E.D. Annual Research Review: Positive adjustment to adversity–trajectories of minimal–impact resilience and emergent resilience. J. Child Psychol. Psychiatry 2013, 54, 378–401. [Google Scholar] [CrossRef] [Green Version]
- Kalisch, R.; Baker, D.G.; Basten, U.; Boks, M.P.; Bonanno, G.A.; Brummelman, E.; Chmitorz, A.; Fernàndez, G.; Fiebach, C.J.; Galatzer-Levy, I. The resilience framework as a strategy to combat stress-related disorders. Nat. Hum. Behav. 2017, 1, 784–790. [Google Scholar] [CrossRef] [Green Version]
- Rutten, B.P.; Hammels, C.; Geschwind, N.; Menne-Lothmann, C.; Pishva, E.; Schruers, K.; Van Den Hove, D.; Kenis, G.; van Os, J.; Wichers, M. Resilience in mental health: Linking psychological and neurobiological perspectives. Acta Psychiatr. Scand. 2013, 128, 3–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stainton, A.; Chisholm, K.; Kaiser, N.; Rosen, M.; Upthegrove, R.; Ruhrmann, S.; Wood, S.J. Resilience as a multimodal dynamic process. Early Interv. Psychiatry 2019, 13, 725–732. [Google Scholar] [CrossRef] [Green Version]
- Southwick, S.M.; Charney, D.S. Resilience: The Science of Mastering Life’s Greatest Challenges; Cambridge University Press: Cambridge, UK, 2018. [Google Scholar]
- Fritz, J.; Fried, E.I.; Goodyer, I.M.; Wilkinson, P.O.; van Harmelen, A.-L. A network model of resilience factors for adolescents with and without exposure to childhood adversity. Sci. Rep. 2018, 8, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bengel, J.; Lyssenko, L. Resilienz und psychologische Schutzfaktoren im Erwachsenenalter: Stand der Forschung zu Psychologischen Schutzfaktoren von Gesundheit im Erwachsenenalter; BZgA Bundeszentrale für Gesundheitliche Aufklärung: Köln, Germany, 2012. [Google Scholar]
- Cleary, M.; Kornhaber, R.; Thapa, D.K.; West, S.; Visentin, D. The effectiveness of interventions to improve resilience among health professionals: A systematic review. Nurse Educ. Today 2018, 71, 247–263. [Google Scholar] [CrossRef]
- Kunzler, A.M.; Helmreich, I.; Chmitorz, A.; König, J.; Binder, H.; Wessa, M.; Lieb, K. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Syst. Rev. 2020, 7, Cd012527. [Google Scholar] [PubMed]
- Kunzler, A.M.; Helmreich, I.; König, J.; Chmitorz, A.; Wessa, M.; Binder, H.; Lieb, K. Psychological interventions to foster resilience in healthcare students. Cochrane Database Syst. Rev. 2020, 7, Cd013684. [Google Scholar]
- Chmitorz, A.; Kunzler, A.; Helmreich, I.; Tüscher, O.; Kalisch, R.; Kubiak, T.; Wessa, M.; Lieb, K. Intervention studies to foster resilience—A systematic review and proposal for a resilience framework in future intervention studies. Clin. Psychol. Rev. 2018, 59, 78–100. [Google Scholar] [CrossRef]
- Bernburg, M.; Groneberg, D.A.; Mache, S. Mental Health Promotion Intervention for Nurses Working in German Psychiatric Hospital Departments: A Pilot Study. Issues Mental Health Nur. 2019, 40, 706–711. [Google Scholar] [CrossRef] [PubMed]
- Lebares, C.C.; Hershberger, A.O.; Guvva, E.V.; Desai, A.; Mitchell, J.; Shen, W.; Reilly, L.M.; Delucchi, K.L.; O’Sullivan, P.S.; Ascher, N.L.; et al. Feasibility of Formal Mindfulness-Based Stress-Resilience Training Among Surgery Interns: A Randomized Clinical Trial. JAMA Surg. 2018, 153, e182734. [Google Scholar] [CrossRef] [PubMed]
- Zarbo, C.; Tasca, G.A.; Cattafi, F.; Compare, A. Integrative Psychotherapy Works. Front. Psychol. 2016, 6, 2021. [Google Scholar] [CrossRef] [Green Version]
- Lazarus, R.S. Coping theory and research: Past, present, and future. Psychosom. Med. 1993, 55, 234–247. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.; Bogossian, F.; Ahern, K. Stress and coping in Australian nurses: A systematic review. Int. Nurs. Rev. 2010, 57, 22–31. [Google Scholar] [CrossRef]
- Ren, Y.; Zhou, Y.; Wang, S.; Luo, T.; Huang, M.; Zeng, Y. Exploratory study on resilience and its influencing factors among hospital nurses in Guangzhou, China. Int. J. Nurs. Sci. 2018, 5, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-F.; Kuo, C.-C.; Chien, T.-W.; Wang, Y.-R. A meta-analysis of the effects of coping strategies on reducing nurse burnout. Appl. Nurs. Res. 2016, 31, 100–110. [Google Scholar] [CrossRef]
- Diamond, A. Executive functions. Annu. Rev. Psychol. 2013, 64, 135–168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and commitment therapy: Model, processes and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef] [Green Version]
- Beck, J.S.; Beck, A.T. Cognitive Therapy: Basics and Beyond; Guilford Press: New York, NY, USA, 1995. [Google Scholar]
- Bateman, A.; Fonagy, P. Psychotherapy for Borderline Personality Disorder: Mentalization Based Treatment; Oxford University Press: Oxford, UK, 2004. [Google Scholar]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change; Guilford Press: New York, NY, USA, 1999. [Google Scholar]
- Luszczynska, A.; Gutiérrez-Doña, B.; Schwarzer, R. General self-efficacy in various domains of human functioning: Evidence from five countries. Int. J. Psychol. 2005, 40, 80–89. [Google Scholar] [CrossRef]
- Lee, J.H.; Nam, S.K.; Kim, A.R.; Kim, B.; Lee, M.Y.; Lee, S.M. Resilience: A meta-analytic approach. J. Couns. Dev. 2013, 91, 269–279. [Google Scholar] [CrossRef]
- Nielsen, K.; Yarker, J.; Randall, R.; Munir, F. The mediating effects of team and self-efficacy on the relationship between transformational leadership, and job satisfaction and psychological well-being in healthcare professionals: A cross-sectional questionnaire survey. Int. J. Nurs. Stud. 2009, 46, 1236–1244. [Google Scholar] [CrossRef]
- Lee, T.W.; Ko, Y.K. Effects of self-efficacy, affectivity and collective efficacy on nursing performance of hospital nurses. J. Adv. Nurs. 2010, 66, 839–848. [Google Scholar] [CrossRef]
- Yang, Y.-K. A study on burnout, emotional labor, and self-efficacy in nurses. J. Korean Acad. Nurs. Adm. 2011, 17, 423–431. [Google Scholar] [CrossRef] [Green Version]
- Baumeister, R.F.; Campbell, J.D.; Krueger, J.I.; Vohs, K.D. Does high self-esteem cause better performance, interpersonal success, happiness, or healthier lifestyles? Psychol. Sci. Public Interest 2003, 4, 1–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferring, D.; Filipp, S.-H. Messung des Selbstwertgefühls: Befunde zu Reliabilität, Validität und Stabilität der Rosenberg-Skala. Diagnostica 1996, 42, 284–292. [Google Scholar]
- Besser, A.; Weinberg, M.; Zeigler-Hill, V.; Neria, Y. Acute symptoms of posttraumatic stress and dissociative experiences among female Israeli civilians exposed to war: The roles of intrapersonal and interpersonal sources of resilience. J. Clin. Psychol. 2014, 70, 1227–1239. [Google Scholar] [CrossRef]
- Hayter, M.; Dorstyn, D. Resilience, self-esteem and self-compassion in adults with spina bifida. Spinal Cord 2014, 52, 167–171. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.; Yu, Q.; Zhang, Q.; Guo, Y.; Chen, J. The relationship between explicit self-esteem and subjective well-being: The moderating effect of implicit self-esteem. J. Gen. Psychol. 2020, 147, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Levin, L.S.; Idler, E.L. Self-care in health. Annu. Rev. Public Health 1983, 4, 181–201. [Google Scholar] [CrossRef]
- Richards, K. Self-care is a lifelong journey. Nurs. Econ. 2013, 31, 198. [Google Scholar]
- Grafton, E.; Gillespie, B.; Henderson, S. Resilience: The power within. Oncol. Nurs. Forum 2010, 37, 698–705. [Google Scholar] [CrossRef] [PubMed]
- Ross, A.; Touchton-Leonard, K.; Perez, A.; Wehrlen, L.; Kazmi, N.; Gibbons, S. Factors that influence health-promoting self-care in registered nurses: Barriers and facilitators. Adv. Nurs. Sci. 2019, 42, 358–373. [Google Scholar] [CrossRef]
- Rizo-Baezea, M.; Mendiola-Infante, S.V.; Sepehri, A.; Palazón-Bru, A.; Gil-Guillén, V.F.; Cortés-Castell, E. Burnout syndrome in nurses working in palliative care units: An analysis of associated factors. J. Nurs. Manag. 2018, 26, 19–25. [Google Scholar] [CrossRef]
- Alexander, G.K.; Rollins, K.; Walker, D.; Wong, L.; Pennings, J. Yoga for Self-Care and Burnout Prevention among Nurses. Workplace Health Saf. 2015, 63, 462–470. [Google Scholar] [CrossRef]
- Erisman, S.M.; Roemer, L. A preliminary investigation of the process of mindfulness. Mindfulness 2012, 3, 30–43. [Google Scholar] [CrossRef]
- Tang, Y.-Y.; Hölzel, B.K.; Posner, M.I. The neuroscience of mindfulness meditation. Nat. Rev. Neurosci. 2015, 16, 213–225. [Google Scholar] [CrossRef]
- Benada, N.; Chowdhry, R. A correlational study of happiness, resilience and mindfulness among nursing student. Indian J. Posit. Psychol. 2017, 8, 105–107. [Google Scholar]
- Guillaumie, L.; Boiral, O.; Champagne, J. A mixed-methods systematic review of the effects of mindfulness on nurses. J. Adv. Nurs. 2017, 73, 1017–1034. [Google Scholar] [CrossRef]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2012, 10, 28–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ackenheil, M.; Stotz-Ingenlath, G.; Dietz-Bauer, R.; Vossen, A. MINI Mini International Neuropsychiatric Interview, German Version 5.0.0 DSM IV; Psychiatric University Clinic: München, Germany, 1999. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Hillier, V.F. A scaled version of the General Health Questionnaire. Psychol. Med. 1979, 9, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, D.P.; Oldehinkel, T.; Ormel, J. Why GHQ threshold varies from one place to another. Psychol. Med. 1998, 28, 915–921. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, D.P.; Gater, R.; Sartorius, N.; Ustun, T.B.; Piccinelli, M.; Gureje, O.; Rutter, C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 1997, 27, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Chmitorz, A.; Kurth, K.; Mey, L.K.; Wenzel, M.; Lieb, K.; Tüscher, O.; Kubiak, T.; Kalisch, R. Assessment of Microstressors in Adults: Questionnaire Development and Ecological Validation of the Mainz Inventory of Microstressors. JMIR Ment. Health 2020, 7, e14566. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef]
- Chmitorz, A.; Wenzel, M.; Stieglitz, R.; Kunzler, A.; Bagusat, C.; Helmreich, I.; Gerlicher, A.; Kampa, M.; Kubiak, T.; Kalisch, R.; et al. Population-based validation of a German version of the Brief Resilience Scale. PLoS ONE 2018, 13, e0192761. [Google Scholar] [CrossRef] [Green Version]
- Kunzler, A.M.; Chmitorz, A.; Bagusat, C.; Kaluza, A.J.; Hoffmann, I.; Schäfer, M.; Quiring, O.; Rigotti, T.; Kalisch, R.; Tüscher, O.; et al. Construct Validity and Population-Based Norms of the German Brief Resilience Scale (BRS). Eur. J. Health Psychol. 2018, 25, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Connor, K.M.; Davidson, J.R.T. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Bech, P. Measuring the dimension of psychological general well-being by the WHO-5. Qual. Life Newsl. 2004, 32, 15–16. [Google Scholar]
- Schwarzer, R.; Jerusalem, M. Skalen zur Erfassung von Lehrer-und Schülermerkmalen; Freie Universität Berlin: Berlin, Germany, 1999. [Google Scholar]
- Rosenberg, M. Society and the Adolescent Self-Image; Princeton university Press: Princeton, NJ, USA, 1965. [Google Scholar]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The satisfaction with life scale. J. Personal. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Berking, M.; Znoj, H. Entwicklung und Validierung eines Fragebogens zur standardisierten Selbsteinschätzung emotionaler Kompetenzen (SEK-27). Z. Für Psychiatr. Psychol. Und Psychother. 2008, 56, 141–153. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Schneider, E.E.; Schönfelder, S.; Domke-Wolf, M.; Wessa, M. Measuring stress in clinical and nonclinical subjects using a German adaptation of the Perceived Stress Scale. Int. J. Clin. Health Psychol. 2020, 20, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S. You want to measure coping but your protocol’too long: Consider the brief cope. Int. J. Behav. Med. 1997, 4, 92. [Google Scholar] [CrossRef]
- Bates, D.; Maechler, M.; Bolker, B. Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing. Available online: https://www.R-project.org/ (accessed on 14 November 2021).
- Kuznetsova, A.; Brockhoff, P.B.; Christensen, R.H. lmerTest package: Tests in linear mixed effects models. J. Stat. Softw. 2017, 82, 1–26. [Google Scholar] [CrossRef] [Green Version]
- Halekoh, U.; Højsgaard, S. A kenward-roger approximation and parametric bootstrap methods for tests in linear mixed models–the R package pbkrtest. J. Stat. Softw. 2014, 59, 1–30. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Steinhardt, M.; Dolbier, C. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. J. Am. Coll. Health 2008, 56, 445–453. [Google Scholar] [CrossRef]
- Castro, C.A.; Adler, A.B.; McGurk, D.; Bliese, P.D. Mental health training with soldiers four months after returning from Iraq: Randomization by platoon. J. Trauma. Stress 2012, 25, 376–383. [Google Scholar] [CrossRef]
- Schroeder, D.A.; Stephens, E.; Colgan, D.; Hunsinger, M.; Rubin, D.; Christopher, M.S. A brief mindfulness-based intervention for primary care physicians: A pilot randomized controlled trial. Am. J. Lifestyle Med. 2018, 12, 83–91. [Google Scholar] [CrossRef] [Green Version]
- Chesak, S.S.; Bhagra, A.; Schroeder, D.R.; Foy, D.A.; Cutshall, S.M.; Sood, A. Enhancing resilience among new nurses: Feasibility and efficacy of a pilot intervention. Ochsner J. 2015, 15, 38–44. [Google Scholar]
- Sood, A.; Prasad, K.; Schroeder, D.; Varkey, P. Stress management and resilience training among Department of Medicine faculty: A pilot randomized clinical trial. J. Gen. Intern. Med. 2011, 26, 858–861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalisch, R.; Köber, G.; Binder, H.; Ahrens, K.F.; Basten, U.; Chmitorz, A.; Fiebach, C.; Goldbach, N.; Horstmann, R.; Kampa, M. A generic solution for the operationalization and measurement of resilience and resilience processes in longitudinal observations: Rationale and basic design of the MARP and LORA studies. 2020. Available online: https://psyarxiv.com/jg238/ (accessed on 14 November 2021).
- Morrison-Beedy, D.; Visovsky, C. Participant Recruitment and Retention. In Intervention Research and Evidence-Based Quality Improvement: Designing, Conducting, Analyzing, and Funding; Melnyk, B.M., Morrison-Beedy, D., Eds.; Springer: Berlin/Heidelberg, Germany, 2018; p. 225. [Google Scholar]
- Galantino, M.L.; Baime, M.; Maguire, M.; Szapary, P.O.; Farrar, J.T. Association of psychological and physiological measures of stress in health-care professionals during an 8-week mindfulness meditation program: Mindfulness in practice. Stress Health J. Int. Soc. Investig. Stress 2005, 21, 255–261. [Google Scholar] [CrossRef]
- Luthar, S.S.; Curlee, A.; Tye, S.J.; Engelman, J.C.; Stonnington, C.M. Fostering resilience among mothers under stress:”Authentic Connections Groups” for medical professionals. Women’s Health Issues 2017, 27, 382–390. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Intervention Group (n = 38) | Control Group (n = 34) | Test-Statistic | p |
|---|---|---|---|---|
| age in years, M (SD) | 47.4 (10.8) | 46.5 (10.4) | 618 1 | 0.76 |
| gender, n (%) | 0.89 3 | |||
| female | 35 (92.1) | 31 (91.2) | ||
| male | 3 (7.9) | 3 (8.8) | ||
| marital status, n (%) | 4 2 | 0.17 | ||
| single | 11 (29.0) | 17 (50.0) | ||
| married | 19 (50.0) | 13 (38.2) | ||
| divorced | 5 (13.2) | 3 (8.8) | ||
| living separately | 1 (2.6) | 1 (2.9) | ||
| widowed | 2 (5.3) | 0 (0.0) | ||
| weekly working hours, M (SD) | 34.3 (7.6) | 33.4 (7.9) | 546 1 | 0.24 |
| Stressorload 4, M (SD) | 60.82 (24.63) | 66.29 (34.07) | 693 1 | 0.60 |
| medical department, n (%) | ||||
| anaesthesia, intensive care, surgery, emergency medicine, cardiology | 11 (30.0) | 12 (35.3) | ||
| ophthalmology | 3 (7.9) | 4 (11.8) | ||
| dermatology | 1 (2.6) | 1 (2.9) | ||
| gynaecology, urology | 3 (7.9) | 1 (2.9) | ||
| oral and maxillofacial surgery, ear, nose, and throat medicine | 4 (10.5) | 3 (8.8) | ||
| neurology, stroke unit | 8 (21.1) | 8 (23.5) | ||
| nuclear medicine | 1 (2.6) | 1 (2.9) | ||
| paediatrics | 2 (5.3) | 0 (0.0) | ||
| psychiatry, psychosomatic medicine | 2 (5.3) | 1 (2.9) | ||
| OR management | 3 (7.9) | 3 (8.8) |
| Intervention Group | Control Group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| t0 (n = 38) | t1 (n = 31) | t0 (n = 34) | t1 (n = 33) | ||||||||
| Outcome Measure | M | SD | M | SD | M | SD | M | SD | t | p | η2 |
| mental health (GHQ-28) | 20.79 | 9.85 | 15.81 | 7.13 | 20.68 | 8.48 | 20.03 | 10.69 | −2.25 | 0.03 | 0.08 |
| wellbeing (WHO-5) | 15.90 | 4.83 | 17.26 | 4.17 | 15.47 | 5.51 | 15.24 | 5.89 | 1.59 | 0.12 | 0.04 |
| resilience (BRS) | 3.08 | 0.34 | 3.12 | 0.32 | 2.89 | 0.36 | 2.85 | 0.50 | 1.43 | 0.16 | 0.03 |
| satisfaction with life (SWLS) | 24.21 | 5.28 | 26.71 | 4.49 | 24.94 | 5.06 | 25.15 | 4.90 | 2.05 | 0.05 | 0.07 |
| perceived stress (PSS-10) | 21.91 | 3.68 | 20.03 | 2.94 | 19.34 | 3.37 | 20.06 | 3.34 | −1.52 | 0.13 | 0.04 |
| self-esteem (RSES) | 35.37 | 4.09 | 35.23 | 4.52 | 34.06 | 3.94 | 34.36 | 4.44 | −0.17 | 0.87 | 0.00 |
| self-efficacy (SWE) | 29.95 | 3.48 | 30.71 | 4.02 | 30.03 | 3.91 | 29.73 | 4.02 | 1.93 | 0.06 | 0.06 |
| emotion regulation (SEK-27) | 78.16 | 12.22 | 83.55 | 13.42 | 74.86 | 12.83 | 72.70 | 14.80 | 3.13 | 0.003 | 0.14 |
| resilience (CD-RISC) | 70.40 | 11.84 | 73.36 | 12.38 | 69.88 | 11.85 | 69.33 | 12.35 | 2.36 | 0.02 | 0.08 |
| active coping (Brief-COPE) | 5.18 | 1.47 | 5.84 | 1.46 | 5.35 | 1.37 | 4.94 | 1.46 | 2.94 | 0.01 | 0.12 |
| positive reframing (Brief-COPE) | 5.19 | 1.60 | 5.48 | 1.63 | 5.09 | 1.48 | 5.18 | 1.42 | 1.24 | 0.22 | 0.02 |
| stressor load (MIMI; occurrence) | 60.82 | 24.63 | 60.26 | 26.68 | 66.29 | 34.07 | 63.45 | 39.2 | |||
| Intervention Group | Control Group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| t2 (n = 30) | t3 (n = 30) | t4 (n = 25) | t2 (n = 31) | t3 (n = 28) | ||||||
| Outcome Measure | M | SD | M | SD | M | SD | M | SD | M | SD |
| mental health (GHQ-28) | 18.53 | 8.11 | 16.37 | 7.62 | 21.16 | 7.37 | 23.58 | 11.20 | 22.21 | 10.30 |
| wellbeing (WHO-5) | 17.70 | 4.42 | 18.10 | 4.21 | 14.32 | 5.17 | 14.19 | 5.20 | 13.60 | 5.34 |
| resilience (BRS) | 3.73 | 0.65 | 3.80 | 0.58 | 3.79 | 0.59 | 3.45 | 0.83 | 3.57 | 0.78 |
| satisfaction with life (SWLS) | 26.50 | 4.10 | 27.37 | 4.76 | 26.76 | 4.88 | 25.94 | 4.84 | 25.61 | 5.64 |
| perceived stress (PSS-10) | 19.63 | 3.42 | 19.63 | 3.01 | 20.44 | 3.36 | 20.00 | 3.29 | 18.93 | 3.63 |
| self-esteem (RSES) | 35.67 | 4.28 | 35.23 | 4.60 | 35.76 | 4.35 | 33.39 | 4.43 | 33.86 | 4.44 |
| self-efficacy (SWE) | 29.97 | 4.72 | 31.00 | 3.96 | 30.24 | 4.38 | 30.23 | 4.52 | 30.32 | 4.68 |
| emotion regulation (SEK-27) | 83.13 | 11.76 | 82.90 | 13.11 | 75.96 | 14.80 | 73.87 | 16.47 | 74.43 | 16.05 |
| resilience (CD-RISC) | 72.03 | 11.89 | 73.80 | 12.75 | 71.12 | 12.23 | 69.81 | 13.57 | 69.43 | 13.16 |
| active coping (Brief-COPE) | 5.73 | 1.48 | 5.43 | 1.55 | 5.24 | 1.42 | 5.06 | 1.18 | 5.07 | 1.21 |
| positive reframing (Brief-COPE) | 5.30 | 1.42 | 5.60 | 1.28 | 5.52 | 1.53 | 4.90 | 1.11 | 4.82 | 1.44 |
| stressor load (MIMI; occurrence) | 59.20 | 24.44 | 55.43 | 27.25 | 62.28 | 31.97 | 68.61 | 37.00 | 58.44 | 26.72 |
| Outcome Measure | t | p | η2 | |
|---|---|---|---|---|
| mental health (GHQ-28) | −4.18 | −2.67 | 0.01 | 0.11 |
| wellbeing (WHO-5) | 2.62 | 2.97 | 0.004 | 0.13 |
| resilience (BRS) | 0.07 | 0.66 | 0.51 | 0.01 |
| satisfaction with life (SWLS) | 1.69 | 1.82 | 0.07 | 0.05 |
| perceived stress (PSS-10) | −0.84 | −1.41 | 0.16 | 0.03 |
| self-esteem (RSES) | 0.43 | 0.81 | 0.42 | 0.01 |
| self-efficacy (SWE) | 0.84 | 1.49 | 0.14 | 0.03 |
| emotion regulation (SEK-27) | 5.41 | 2.44 | 0.02 | 0.09 |
| resilience (CD-RISC) | 3.46 | 2.14 | 0.04 | 0.07 |
| active coping (Brief-COPE) | 0.64 | 2.74 | 0.01 | 0.11 |
| positive reframing (Brief-COPE) | 0.59 | 2.61 | 0.01 | 0.10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Janzarik, G.; Wollschläger, D.; Wessa, M.; Lieb, K. A Group Intervention to Promote Resilience in Nursing Professionals: A Randomised Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 649. https://doi.org/10.3390/ijerph19020649
Janzarik G, Wollschläger D, Wessa M, Lieb K. A Group Intervention to Promote Resilience in Nursing Professionals: A Randomised Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(2):649. https://doi.org/10.3390/ijerph19020649
Chicago/Turabian StyleJanzarik, Gesche, Daniel Wollschläger, Michèle Wessa, and Klaus Lieb. 2022. "A Group Intervention to Promote Resilience in Nursing Professionals: A Randomised Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 2: 649. https://doi.org/10.3390/ijerph19020649
APA StyleJanzarik, G., Wollschläger, D., Wessa, M., & Lieb, K. (2022). A Group Intervention to Promote Resilience in Nursing Professionals: A Randomised Controlled Trial. International Journal of Environmental Research and Public Health, 19(2), 649. https://doi.org/10.3390/ijerph19020649






