Postoperative Lifestyle of Patients with Liver Cancer: An Exploratory Study in a Single Center in Taiwan
Abstract
:1. Introduction
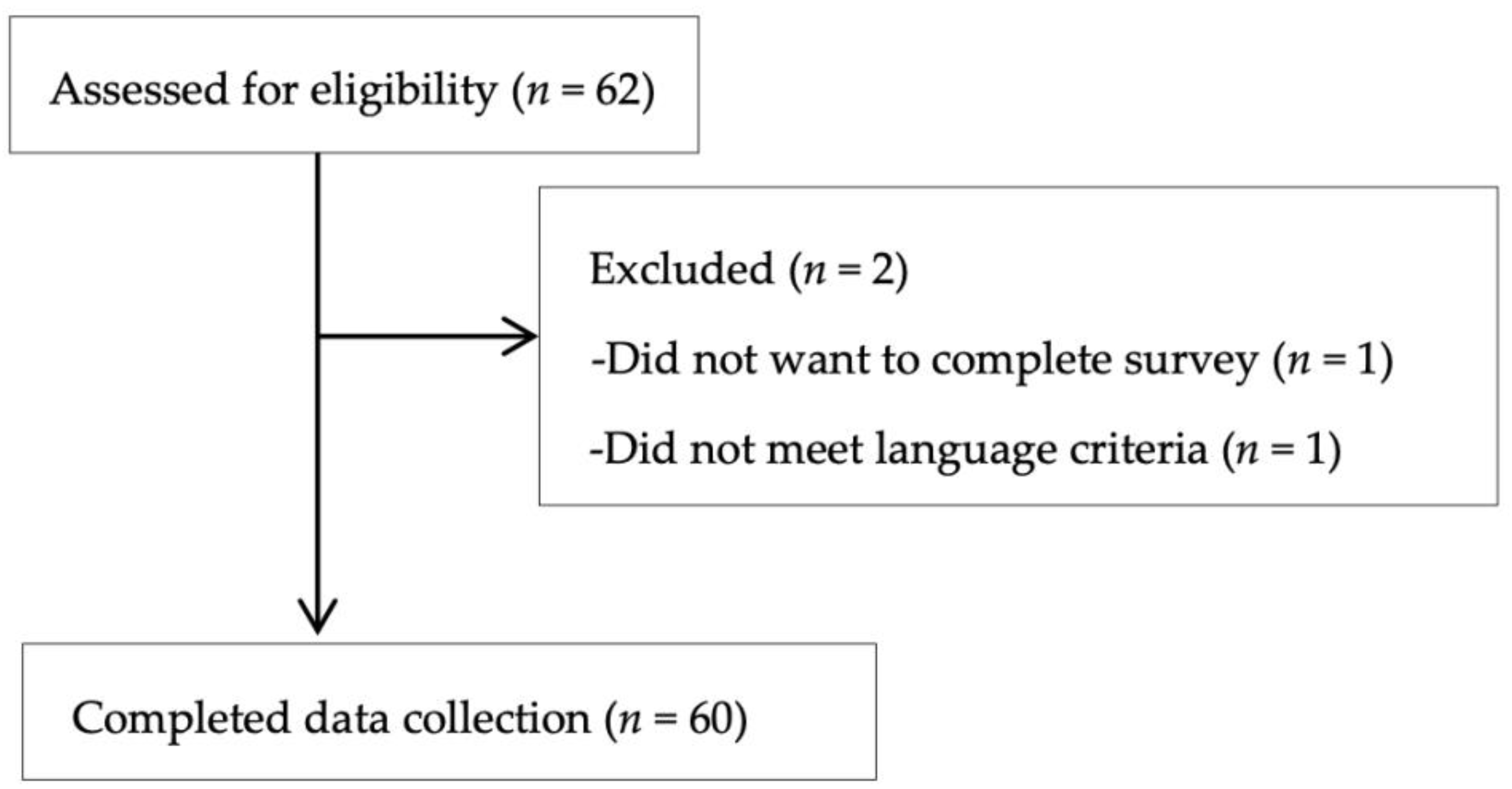
2. Materials and Methods
2.1. Study Design and Setting
2.2. Ethical Considerations
2.3. Measurements
2.4. Data Analyses
3. Results
3.1. Participant Demographics
3.2. Demography of Participants and HELP-C Scores
3.3. Lifestyle Differences between Sexes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- 2020 Cause of Death Statistics. Available online: https://www.mohw.gov.tw/cp-5256-63399-2.html (accessed on 2 April 2022).
- Barber, F.D.; Nelson, J.P. Liver Cancer: Looking to the future for better detection and treatment. Am. J. Nurs. 2000, 100, 41–46. [Google Scholar] [CrossRef]
- Shun, S.C.; Lai, Y.H.; Jing, T.T.; Jeng, C.; Lee, F.Y.; Hu, L.S.; Cheng, S.Y. Fatigue patterns and correlates in male liver cancer patients receiving transcatheter hepatic arterial chemoembolization. Support Care Cancer 2005, 13, 311–317. [Google Scholar] [CrossRef]
- Forner, A.; Hessheimer, A.J.; Real, M.I.; Bruix, J. Treatment of hepatocellular carcinoma. Crit. Rev. Oncol. Hematol. 2006, 60, 89–98. [Google Scholar] [CrossRef]
- Eileen, K.; DSc, R.; Susan, E. Healthy lifestyles for healthy Americans: Report USDA’s year 2000 behavioral nutrition roundtable. Nutr. Today 2000, 35, 84–88. [Google Scholar]
- Liu, H.Q.; Li, X.L. Effect of Nursing Intervention on Liver Cancer Patients Undergoing Interventional Therapy. Available online: https://www.alliedacademies.org/articles/effect-of-nursing-intervention-on-liver-cancer-patients-undergoing-interventional-therapy.html (accessed on 30 December 2017).
- Zhao, Q. Complications in Patients with Hepatocellular Carcinoma after Interventional Observation and Nursing Care. Nurs. Sci. 2014, 3, 61–64. [Google Scholar] [CrossRef]
- Robotin, M.C.; Wallace, J.; Gallego, G.; George, J. Hepatitis B and Liver Cancer: Community Awareness, Knowledge and Beliefs of Middle Eastern Migrants in Sydney, Australia. Int. J. Environ. Res. Public Health. Available online: https://www.mdpi.com/1660-4601/18/16/8534 (accessed on 30 December 2021).
- Ghasemi Yngyknd, S.; Asghari Jafarabadi, M.; Ghanbari-Homayi, S.; Laghousi, D.; Mirghafourvand, M. A systematic review of social determinants of healthy lifestyle among Iranian women. Nurs. Open 2021, 8, 2007–2017. [Google Scholar] [CrossRef]
- Jackiewicz, S.; James, R.; Campbell, C. Is the term ‘lifestyle’ appropriate to use in health promotion today? Health Promot. J. Aust. 2005, 16, 179–183. [Google Scholar] [CrossRef]
- Cheng, M.L.; Lin, H.Y.; Hsieh, C.F. The Correlation between age of Death and Life Habits in Patients with Liver Cirrhosis or Liver Cancer in Hualien Area. J. Intern. Med. Taiwan 2022, 33, 57–63. [Google Scholar]
- Bin Wei, W.W.; Yunquan, L.; Shibing, S. Advances in Traditional Chinese Medical Treatment Research in Liver Cancer Postoperation. Tradit. Chin. Med. 2014, 3, 38–46. [Google Scholar]
- Tsai, S.J.; Chen, M.J.; Chang, W.H.; Shin, S.C.; Wang, H.Y.; Wang, T.E. Analysis of Risk Factors of Early Recurrence of Hepatocellular Carcinoma after Surgical Resection. Taiwan Oncol. Soc. 2009, 25, 114–122. [Google Scholar]
- Chen, J.J.; Hsu, C.Y. To Compare of the Radio Frequency Ablation and Transcatheter Arterial Embolization on the Postoperative Complications, Health Problems and Quality of Life in Pateints with Early Liver Cancer; Issue Brief No. 10601-L07; Chi Mei Medical Center: Tainan, Taiwan, 2017. [Google Scholar]
- Ali, M.A.M.; Harmsen, W.S.; Morsy, K.H.; Galal, G.M.K.; Therneau, T.M.; Roberts, L.R. Prognostic utility of systemic inflammatory markers and chronic hepatitis C virus infection status in hepatocellular carcinoma patients treated with local ablation. BMC Cancer 2022, 22, 221. [Google Scholar] [CrossRef]
- Li, C.F.; Feng, S.H.; Chien, L.Y. Relationship between Symptom Distress and Fatigue in Hepatocellular Carcinoma Patients Who Received Transcatheter Arterial Embolization. J. Nurs. 2015, 62, 57–65. [Google Scholar]
- Guibal, A.; Seiller, I.; Khemissa, F.; Aufranc, V.; Rehim, M.A.; Fryder, I.; Chevallier, P. Recommandations opérationnelles en radiologie interventionnelle: Destruction tumorale percutanée des tumeurs hépatiques. J. Dimagerie Diagn. Interv. 2021, 4, 231–237. [Google Scholar] [CrossRef]
- Brunello, F.; Veltri, A.; Carucci, P.; Pagano, E.; Ciccone, G.; Moretto, P.; Rizzetto, M. Radiofrequency ablation versus ethanol injection for early hepatocellular carcinoma: A randomized controlled trial. Scand. J. Gastroenterol. 2008, 43, 727–735. [Google Scholar] [CrossRef]
- WHOQOL Group. Development of the world health organization WHOQOL BREF quality of life assessment. Psychol. Med. 1998, 28, 551–558. [Google Scholar] [CrossRef] [Green Version]
- Hsu, W.C.; Chan, S.C.; Chen, Y.C.; Chung, N.N.; Wang, P.M. Analysis of Nutritional Status Assessment and Quality of Life for the Patients with Hepatocellular Carcinoma. Ther. Radiol. Oncol. 2011, 18, 299–310. [Google Scholar]
- Chiu, Y.R.; Hsu, H.C.; Huang, H.P. The impact of depression and care burden on quality of life among primary caregivers of advanced liver cancer patients. Formos. J. Med. 2021, 25, 580–591. [Google Scholar]
- Peng, C.Y.; Yu, M.C.; Wang, Y.W.; Weng, L.C. Exploring the Quality of Life and Its Influencing Factors in Patients with Recurrent Liver Cancer. Chang. Gung Nurs. 2020, 31, 315–328. [Google Scholar]
- Polit, D.F.; Beck, C.T. Nursing Research: Generating and Assessing Evidence for Nursing Practice, 9th ed.; Wolters Kluwer Health/Lippincott Williams & Wilkins: New York, NY, USA, 2012. [Google Scholar]
- Lin, Y.J.; Wu, H.C.; Buo, B.M.; Chang, C.S.; Chang, Y.F.; Liu, P.Y.; Wu, C.H. Nutritional Status and Associated Factors of the Elderly in a Remote Community. Taiwan Geriatr. Gerontol. 2013, 8, 186–201. [Google Scholar]
- Chiang, Y.; Wu, T.H. The Aarticulation of Healthism and the Beauty Myth: Consumerism in Taiwanese Women’s Practices of Leisure Sports (1990–2010). J. Sport Cult. 2021, 38, 73–107. [Google Scholar]
- Lo, J.L. Sex Differences in the Correlations of Daily Affective Occupational Experiences and Subjective Well-Being Measures. J. Taiwan Occup. Ther. Assoc. 1994, 12, 21–39. [Google Scholar]
- WHOQOL Group. The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Soc. Sci. Med. 1995, 41, 1403–1409. [Google Scholar] [CrossRef]

| Variable | n | % | ||
|---|---|---|---|---|
| Age | Mean age (SD): 67.28 (10.01) | |||
| Gender | Male | 39 | 65.0 | |
| Female | 21 | 35.0 | ||
| Ethnicity | Hoklo Taiwanese | 56 | 93.3 | |
| Chinese | 4 | 6.7 | ||
| Education | None | 1 | 1.7 | |
| Primary school | 6 | 10 | ||
| Junior high school | 8 | 13.3 | ||
| High school | 15 | 25 | ||
| College/university | 28 | 46.7 | ||
| Research institute | 2 | 3.3 | ||
| Marriage | Married | 50 | 83.3 | |
| Single | 1 | 1.7 | ||
| Widowed | 9 | 15 | ||
| Chronic diseases | Yes | 39 | 65 | |
| No | 21 | 35 | ||
| Drug allergy | Yes | 7 | 11.7 | |
| No | 53 | 88.3 | ||
| Main treatment | RFA | 30 | 50 | |
| TAE | 30 | 50 | ||
| Postoperative complications | No | 40 | 66.7 | |
| Yes | 20 | 33.3 | ||
| Items | HELP-C | ||
|---|---|---|---|
| Mean ± SD | F | p-Value | |
| Age | - | 3.39 | 0.00 * |
| Gender | 0.06 | 0.79 | |
| Male | 54.52 ± 12.23 | ||
| Female | 53.61 ± 14.45 | ||
| Ethnicity | 8.84 | 0.00 * | |
| Hoklo Taiwanese | 55.47 ± 12.38 | ||
| Chinese | 36.75 ± 6.89 | ||
| Education | 9.84 | 0.00 * | |
| None | 37.00 ± - | ||
| Primary school | 40.50 ± 8.91 | ||
| Junior high school | 38.87 ± 6.55 | ||
| High school | 56.33 ± 13.27 | ||
| College/university | 60.33 ± 7.88 | ||
| Research institute | 66.50 ± 16.26 | ||
| Marriage | 12.77 | 0.00 * | |
| Married | 56.59 ± 11.34 | ||
| Single | 78.00 ± - | ||
| Widowed | 38.55 ± 12.95 | ||
| Chronic diseases | 14.57 | 0.00 * | |
| Yes | 49.89 ± 12.89 | ||
| No | 62.00 ± 8.93 | ||
| Drug allergy | 0.07 | 0.79 | |
| Yes | 55.42 ± 12.47 | ||
| No | 54.03 ± 13.12 | ||
| Main treatment | 0.00 | 0.99 | |
| RFA | 54.20 ± 12.67 | ||
| TAE | 54.20 ± 13.43 | ||
| Postoperative complications | 16.77 | 0.00 * | |
| No | 58.58 ± 11.12 | ||
| Yes | 45.65 ± 12.17 |
| Items | Male | Female | ||
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | F | p-Value | |
| Exercise | 2.89 ± 2.50 | 3.00 ± 3.53 | 0.01 | 0.89 |
| Diet | 13.13 ± 4.98 | 9.66 ± 4.21 | 7.27 | 0.00 * |
| Social and productive activities | 5.69 ± 3.01 | 5.33 ± 2.97 | 0.19 | 0.66 |
| Leisure | 6.17 ± 2.37 | 4.33 ± 2.03 | 9.10 | 0.00 * |
| ADL | 13.48 ± 2.56 | 17.90 ± 5.15 | 19.76 | 0.00 * |
| Stress management and spiritual participation | 8.94 ± 3.84 | 8.38 ± 4.08 | 0.28 | 0.59 |
| Other health promotion and risks behaviors | 4.30 ± 2.42 | 5.00 ± 1.87 | 1.28 | 0.26 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yan, S.-L.; Hu, C.-J.; Tsai, L.-Y.; Hsu, C.-Y. Postoperative Lifestyle of Patients with Liver Cancer: An Exploratory Study in a Single Center in Taiwan. Int. J. Environ. Res. Public Health 2022, 19, 9883. https://doi.org/10.3390/ijerph19169883
Yan S-L, Hu C-J, Tsai L-Y, Hsu C-Y. Postoperative Lifestyle of Patients with Liver Cancer: An Exploratory Study in a Single Center in Taiwan. International Journal of Environmental Research and Public Health. 2022; 19(16):9883. https://doi.org/10.3390/ijerph19169883
Chicago/Turabian StyleYan, Sheng-Lei, Chia-Jung Hu, Li-Yun Tsai, and Chen-Yuan Hsu. 2022. "Postoperative Lifestyle of Patients with Liver Cancer: An Exploratory Study in a Single Center in Taiwan" International Journal of Environmental Research and Public Health 19, no. 16: 9883. https://doi.org/10.3390/ijerph19169883
APA StyleYan, S.-L., Hu, C.-J., Tsai, L.-Y., & Hsu, C.-Y. (2022). Postoperative Lifestyle of Patients with Liver Cancer: An Exploratory Study in a Single Center in Taiwan. International Journal of Environmental Research and Public Health, 19(16), 9883. https://doi.org/10.3390/ijerph19169883






