Role of Final Kissing Balloon Inflation in Left Main Distal Bifurcation Single Stenting: Insights from Angiographic Microvascular Resistance
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. AMR and Lesion Measurements
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Lesion Data
3.3. AMR Analyses
3.4. Impact of AMR on Long-Term Angiographic Restenosis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| FKBI | final kissing balloon inflation |
| SB | side branch |
| LMCBL | left main coronary bifurcation lesion |
| IMR | index of microcirculatory resistance |
| PCI | percutaneous coronary intervention |
| AMR | angiography-derived index of microcirculatory resistance |
| PSM | propensity score matching |
| LM | left main |
| LAD | left anterior descending |
| POT | proximal optimization technique |
| LCX | left circumflex |
| DS% | percent diameter stenosis |
| BMI | body mass index |
| LDL-C | low-density lipoprotein cholesterol |
| HDL-C | high-density lipoprotein cholesterol |
| LVEF | left ventricular ejection fraction |
| IVUS/OCT | intravascular ultrasound/optical coherence tomography |
| DS%-long | long-term DS% |
| MV | main vessel |
| MLD | minimal lumen diameters |
| TLR | target lesion revascularization |
| STEMI | ST elevation myocardial infarction |
References
- Dérimay, F.; Rioufol, G.; Aminian, A.; Maillard, L.; Finet, G. Toward a sequential provisional coronary bifurcation stenting technique. From kissing balloon to re-POT sequence. Arch. Cardiovasc. Dis. 2020, 113, 199–208. [Google Scholar] [CrossRef]
- Gao, Z.; Xu, B.; Yang, Y.-J.; Qiao, S.-B.; Wu, Y.-J.; Chen, T.; Xu, L.; Yuan, J.-Q.; Chen, J.; Qin, X.-W.; et al. Effect of final kissing balloon dilatation after one-stent technique at left-main bifurcation: A single center data. Chin. Med. J. 2015, 128, 733–739. [Google Scholar] [CrossRef]
- Ahn, J.-M.; Lee, P.H.; Park, D.-W.; Kang, S.-J.; Lee, S.-W.; Kim, Y.-H.; Lee, C.W.; Park, S.-W.; Park, S.-J. Benefit of Final Kissing Balloon Inflation Mandatory After Simple Crossover Stenting for Left Main Bifurcation Narrowing. Am. J. Cardiol. 2017, 119, 528–534. [Google Scholar] [CrossRef]
- Liu, G.; Ke, X.; Wang, L.; Huang, Z.; Guo, Y.; Long, M.; Liao, X. Final kissing balloon inflation for coronary bifurcation lesions treated with single-stent technique : A meta-analysis. Herz 2019, 44, 354–362. [Google Scholar] [CrossRef]
- Kini, A.S.; Dangas, G.D.; Baber, U.; Vengrenyuk, Y.; Kandzari, D.E.; Leon, M.B.; Morice, M.-C.; Serruys, P.W.; Kappetein, A.P.; Sabik, J.F.; et al. Influence of final kissing balloon inflation on long-term outcomes after PCI of distal left main bifurcation lesions in the EXCEL trial. EuroIntervention 2020, 16, 218–224. [Google Scholar] [CrossRef]
- Sanz-Sánchez, J.; Calderón, A.T.; Neves, D.; Villar, C.C.; Lukic, A.; González, E.R.; Sánchez-Elvira, G.; Patricio, L.; Díez-Gil, J.L.; García-García, H.M.; et al. Culprit-Lesion Drug-Coated-Balloon Percutaneous Coronary Intervention in Patients Presenting with ST-Elevation Myocardial Infarction (STEMI). J. Clin. Med. 2025, 14, 869. [Google Scholar] [CrossRef]
- Li, W.; Takahashi, T.; Rios, S.A.; Latib, A.; Lee, J.M.; Fearon, W.F.; Kobayashi, Y. Diagnostic performance and prognostic impact of coronary angiography-based Index of Microcirculatory Resistance assessment: A systematic review and meta-analysis. Catheter. Cardiovasc. Interv. 2022, 99, 286–292. [Google Scholar] [CrossRef]
- Huang, M.; Chen, W.; Liu, D.; Zheng, M.; Lin, L.; Jiang, H.; Lin, K.; Zheng, X.; Lin, N.; Lin, F.; et al. Impact of post-dilatation on post-procedural physiology, microcirculatory resistance, and target vessel failure in STEMI patients undergoing PPCI: A single-center experience. Int. J. Cardiol. 2024, 399, 131685. [Google Scholar] [CrossRef] [PubMed]
- Lu, G.; Zhao, L.; Hui, K.; Lu, Z.; Zhang, X.; Gao, H.; Ma, X. Angiography-Derived Microcirculatory Resistance in Detecting Microvascular Obstruction and Predicting Heart Failure After STEMI. Circ. Cardiovasc. Imaging 2025, 18, e017506. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Liu, S.; Wang, J.; Liu, Z.; Qi, C. Analysis of Metabolic Risk Factors for Microcirculation Disorders Post-Percutaneous Coronary Intervention and Predictive Model Construction: A Study on Patients with Unstable Angina. Rev. Cardiovasc. Med. 2025, 26, 25739. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Fezzi, S.; Sun, P.; Ding, N.; Li, X.; Hu, X.; Wang, S.; Wijns, W.; Lu, Z.; Tu, S. In Vivo Validation of a Novel Computational Approach to Assess Microcirculatory Resistance Based on a Single Angiographic View. J. Pers. Med. 2022, 12, 1798. [Google Scholar] [CrossRef]
- Fezzi, S.; Ding, D.; Scarsini, R.; Huang, J.; Del Sole, P.A.; Zhao, Q.; Pesarini, G.; Simpkin, A.; Wijns, W.; Ribichini, F.; et al. Integrated Assessment of Computational Coronary Physiology from a Single Angiographic View in Patients Undergoing TAVI. Circ. Cardiovasc. Interv. 2023, 16, e013185. [Google Scholar] [CrossRef]
- Shi, W.; Zhang, H.; Song, L.; Zou, T.; Xie, L.; Guan, C.; Wang, M.; Wu, Y. Angiographic Microvascular Resistance Is an Independent Predictor of Adverse Clinical Outcomes After Transcatheter Aortic Valve Replacement. J. Am. Heart Assoc. 2025, 14, e039346. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.W.; Yang, J.H.; Bin Song, Y.; Hahn, J.-Y.; Choi, S.-H.; Choi, J.-H.; Lee, H.J.; Oh, J.H.; Koo, B.-K.; Rha, S.W.; et al. Long-Term Clinical Outcomes of Final Kissing Ballooning in Coronary Bifurcation Lesions Treated With the 1-Stent Technique: Results from the COBIS II Registry (Korean Coronary Bifurcation Stenting Registry). JACC Cardiovasc. Interv. 2015, 8, 1297–1307. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gwon, H.-C.; Hahn, J.-Y.; Koo, B.-K.; Bin Song, Y.; Choi, S.-H.; Choi, J.-H.; Lee, S.H.; Jeong, M.-H.; Kim, H.-S.; Seong, I.-W.; et al. Final kissing ballooning and long-term clinical outcomes in coronary bifurcation lesions treated with 1-stent technique: Results from the COBIS registry. Heart 2011, 98, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Nam, C.-W.; Cho, Y.-K.; Yoon, H.-J.; Kim, K.-B.; Gwon, H.-C.; Kim, H.-S.; Chun, W.J.; Han, S.H.; Rha, S.-W.; et al. 5-Year Outcome of Simple Crossover Stenting in Coronary Bifurcation Lesions Compared with Side Branch Opening. JACC Asia 2021, 1, 53–64. [Google Scholar] [CrossRef]
- He, L.; Robb, J.F.; Martinez-Camblor, P.; Andrus, B.W.; Greene, L.J.; Gongal, P.; Reddy, D.S.; DeVries, J.T. Longitudinal outcomes of final kissing balloon inflation in coronary bifurcation lesions treated with a single stent. Front. Cardiovasc. Med. 2023, 10, 1290024. [Google Scholar] [CrossRef]
- Watanabe, Y.; Murasato, Y.; Yamawaki, M.; Kinoshita, Y.; Okubo, M.; Yumoto, K.; Masuda, N.; Otake, H.; Aoki, J.; Nakazawa, G.; et al. Proximal optimisation technique versus final kissing balloon inflation in coronary bifurcation lesions: The randomised, multicentre PROPOT trial. EuroIntervention 2021, 17, 747–756. [Google Scholar] [CrossRef]
- Bianchini, F.; Cangemi, S.; DeVos, A.; Bielecki, M.; Aurigemma, C.; Romagnoli, E.; Trani, C.; Iaizzo, P.A.; Burzotta, F. Multimodal Comparisons of Results Achieved by Different Side Branch Ballooning Techniques for Bifurcation Provisional Stenting. Circ. Cardiovasc. Interv. 2023, 16, 111–120. [Google Scholar] [CrossRef]
- Gdowski, M.A.; Murthy, V.L.; Doering, M.; Monroy-Gonzalez, A.G.; Slart, R.; Brown, D.L. Association of Isolated Coronary Microvascular Dysfunction with Mortality and Major Adverse Cardiac Events: A Systematic Review and Meta-Analysis of Aggregate Data. J. Am. Heart Assoc. 2020, 9, e014954. [Google Scholar] [CrossRef]
- Fearon, W.F.; Balsam, L.B.; Farouque, H.M.O.; Robbins, R.C.; Fitzgerald, P.J.; Yock, P.G.; Yeung, A.C. Novel index for invasively assessing the coronary microcirculation. Circulation 2003, 107, 3129–3132. [Google Scholar] [CrossRef]
- Maznyczka, A.M.; Oldroyd, K.G.; McCartney, P.; McEntegart, M.; Berry, C. The Potential Use of the Index of Microcirculatory Resistance to Guide Stratification of Patients for Adjunctive Therapy in Acute Myocardial Infarction. JACC Cardiovasc. Interv. 2019, 12, 951–966. [Google Scholar] [CrossRef]
- Nishi, T.; Murai, T.; Ciccarelli, G.; Shah, S.V.; Kobayashi, Y.; Derimay, F.; Waseda, K.; Moonen, A.; Hoshino, M.; Hirohata, A.; et al. Prognostic Value of Coronary Microvascular Function Measured Immediately After Percutaneous Coronary Intervention in Stable Coronary Artery Disease: An International Multicenter Study. Circ. Cardiovasc. Interv. 2019, 12, e007889. [Google Scholar] [CrossRef] [PubMed]
- A Montone, R.; Galiuto, L.; Meucci, M.C.; Del Buono, M.G.; Vergni, F.; Camilli, M.; Sanna, T.; Pedicino, D.; Buffon, A.; D’AMario, D.; et al. Coronary slow flow is associated with a worse clinical outcome in patients with Takotsubo syndrome. Heart 2020, 106, 923–930. [Google Scholar] [CrossRef]
- Belmonte, M.; Gallinoro, E.; Pijls, N.H.; Bertolone, D.T.; Keulards, D.C.; Viscusi, M.M.; Storozhenko, T.; Mizukami, T.; Mahendiran, T.; Seki, R.; et al. Measuring Absolute Coronary Flow and Microvascular Resistance by Thermodilution: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2024, 83, 699–709. [Google Scholar] [CrossRef]
- Tu, S.; Ding, D.; Chang, Y.; Li, C.; Wijns, W.; Xu, B. Diagnostic accuracy of quantitative flow ratio for assessment of coronary stenosis significance from a single angiographic view: A novel method based on bifurcation fractal law. Catheter. Cardiovasc. Interv. 2021, 97 (Suppl. S2), 1040–1047. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Wu, Q.; Yang, L.; Chen, L.; Liu, W.Z.; Guo, J.; Xu, J.S. Application of AMR in evaluating microvascular dysfunction after ST-elevation myocardial infarction. Clin. Cardiol. 2023, 47, e24196. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Xu, C.; Wang, J.; Teng, Z.; Sha, X.; Xu, K.; Wang, R.; Zhu, L. Triglyceride-glucose index is associated with microcirculatory resistance in patients with type 2 diabetes and STEMI undergoing primary PCI. Sci. Rep. 2025, 15, 4723. [Google Scholar] [CrossRef]
- Gao, B.; Wu, G.; Xie, J.; Ruan, J.; Xu, P.; Qian, Y.; Gu, J.; Li, W.; Jin, X.; Tong, G.; et al. Quantitative Flow Ratio-Derived Index of Microcirculatory Resistance as a Novel Tool to Identify Microcirculatory Function in Patients with Ischemia and No Obstructive Coronary Artery Disease. Cardiology 2023, 149, 14–22. [Google Scholar] [CrossRef]


| Before PSM | After PSM | |||||
|---|---|---|---|---|---|---|
| Simple Crossover (n = 197) | FKBI (n = 70) | p Value | Simple Crossover (n = 61) | FKBI (n = 61) | p Value | |
| Age, years | 65 ± 10.3 | 66.3 ± 8.8 | 0.342 | 68.1 ± 9.6 | 66 ± 9.1 | 0.231 |
| Male gender, n (%) | 160 (81.2%) | 59 (84.3%) | 0.566 | 50 (82%) | 50 (82%) | 1 |
| BMI, kg/m2 | 24.2 (22.1–26.1) | 24.2 (22.4–26.3) | 0.941 | 24.2 (22.7–26.3) | 24.2 (22.7–26.4) | 0.955 |
| Current UA, n (%) | 134 (68%) | 54 (77.1%) | 0.151 | 60 (82%) | 46 (75.4%) | 0.377 |
| Current MI, n (%) | 63 (32%) | 16 (22.9%) | 0.151 | 11 (18%) | 15 (24.6%) | 0.377 |
| Prior MI, n (%) | 27 (13.7%) | 12 (17.1%) | 0.484 | 8 (13.1%) | 8 (13.1%) | 1 |
| Diabetes mellitus, n (%) | 70 (35.5%) | 31 (44.3%) | 0.195 | 25 (41%) | 26 (42.6%) | 0.854 |
| Hypertension, n (%) | 123 (62.4%) | 54 (77.1%) | 0.025 | 47 (77%) | 45 (73.8%) | 0.674 |
| Dyslipidemia, n (%) | 75 (38.1%) | 25 (35.7%) | 0.726 | 25 (41%) | 23 (37.7%) | 0.711 |
| Current smoker, n (%) | 70 (35.5%) | 26 (37.1%) | 0.809 | 26 (42.6%) | 21 (34.4%) | 0.352 |
| LDL-C, mmol/L | 2.6 (2–3.4) | 2.5 (1.9–3.3) | 0.737 | 2.8 (2.1–3.5) | 2.5 (1.9–3.6) | 0.472 |
| HDL-C, mmol/L | 1 (0.8–1.2) | 1 (0.8–1.1) | 0.491 | 1 (0.9–1.1) | 1 (0.8–1.2) | 0.856 |
| Cholesterol, mmol/L | 4 (3.3–4.9) | 3.8 (3.3–4.8) | 0.953 | 4 (3.4–5) | 3.9 (3.3–5.2) | 0.519 |
| Serum creatinine, mmol/L | 80 (70–93) | 81 (69.8–95) | 0.625 | 80 (70.5–91) | 83 (70.5–95) | 0.527 |
| Fasting blood glucose, mmol/L | 5.6 (4.9–7) | 5.9 (5.2–7.1) | 0.21 | 5.7 (4.9–6.7) | 5.9 (5.3–7.4) | 0.114 |
| LVEF, % | 62.5 (54.9–68.4) | 62.4 (56.6–69.2) | 0.58 | 62.9 (58.4–69) | 62.3 (56.3–69) | 0.822 |
| Follow-up, days | 382 (361–458.5) | 378 (353.8–483.5) | 0.693 | 393 (363–592.5) | 378 (353–456.5) | 0.231 |
| Intermediate coronary artery, n (%) | 32 (16.2%) | 12 (17.1%) | 0.862 | 9 (14.8%) | 10 (16.4%) | 0.803 |
| IVUS/OCT, n (%) | 52 (26.4%) | 35 (50%) | <0.001 | 20 (32.8%) | 28 (45.9%) | 0.138 |
| Before PSM | After PSM | |||||
|---|---|---|---|---|---|---|
| Simple Crossover (n = 197) | FKBI (n = 70) | p Value | Simple Crossover (n = 61) | FKBI (n = 61) | p Value | |
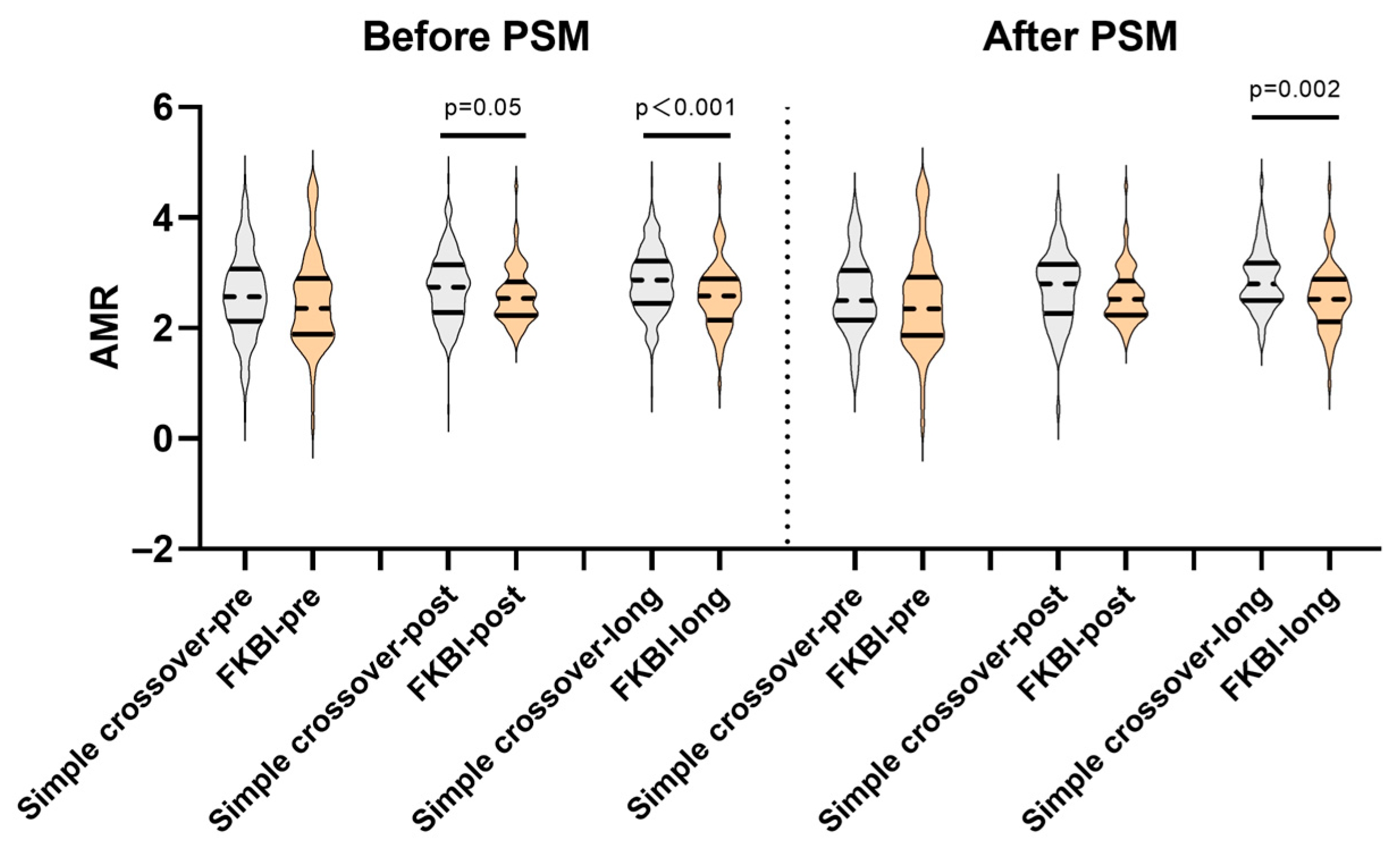
| AMR-pre | 2.57 (2.13–3.07) | 2.36 (1.89–2.9) | 0.178 | 2.5 (2.15–3.04) | 2.35 (1.87–2.93) | 0.275 |
| AMR-post | 2.74 (2.28–3.15) | 2.54 (2.23–2.84) | 0.05 | 2.8 (2.27–3.16) | 2.52 (2.24–2.86) | 0.194 |
| AMR-long | 2.87 (2.45–3.22) | 2.59 (2.15–2.89) | <0.001 | 2.8 (2.5–3.18) | 2.52 (2.12–2.89) | 0.002 |
| DS%-pre in LM | 45.7 (25.3–61.2) | 51.3 (29.3–64.2) | 0.165 | 51.7 (28.9–61.2) | 50.8 (27.8–64.8) | 0.862 |
| DS%-pre in LAD | 63.8 (54.9–68.8) | 58.4 (47–66.4) | 0.012 | 58.8 (51.4–67.4) | 58.6 (48.4–68.1) | 0.737 |
| DS%-pre in LCX | 19.4 (13.2–26.8) | 26.3 (15.6–38) | 0.002 | 25 (17.2–35.7) | 25.8 (15.4–31.1) | 0.63 |
| DS%-post in LM | 3.2 (0–5.7) | 2.5 (0–5) | 0.313 | 4.2 (0–9) | 2.4 (0–5.1) | 0.057 |
| DS%-post in LAD | 5.7 (3.2–8.5) | 6.4 (3.2–10.1) | 0.258 | 7.6 (5.6–11.7) | 6.4 (3.3–10.2) | 0.079 |
| DS%-post in LCX | 25.9 (19.8–33.8) | 25.7 (19.2–37.1) | 0.973 | 29.5 (24.5–36.1) | 25.6 (19.2–34.8) | 0.043 |
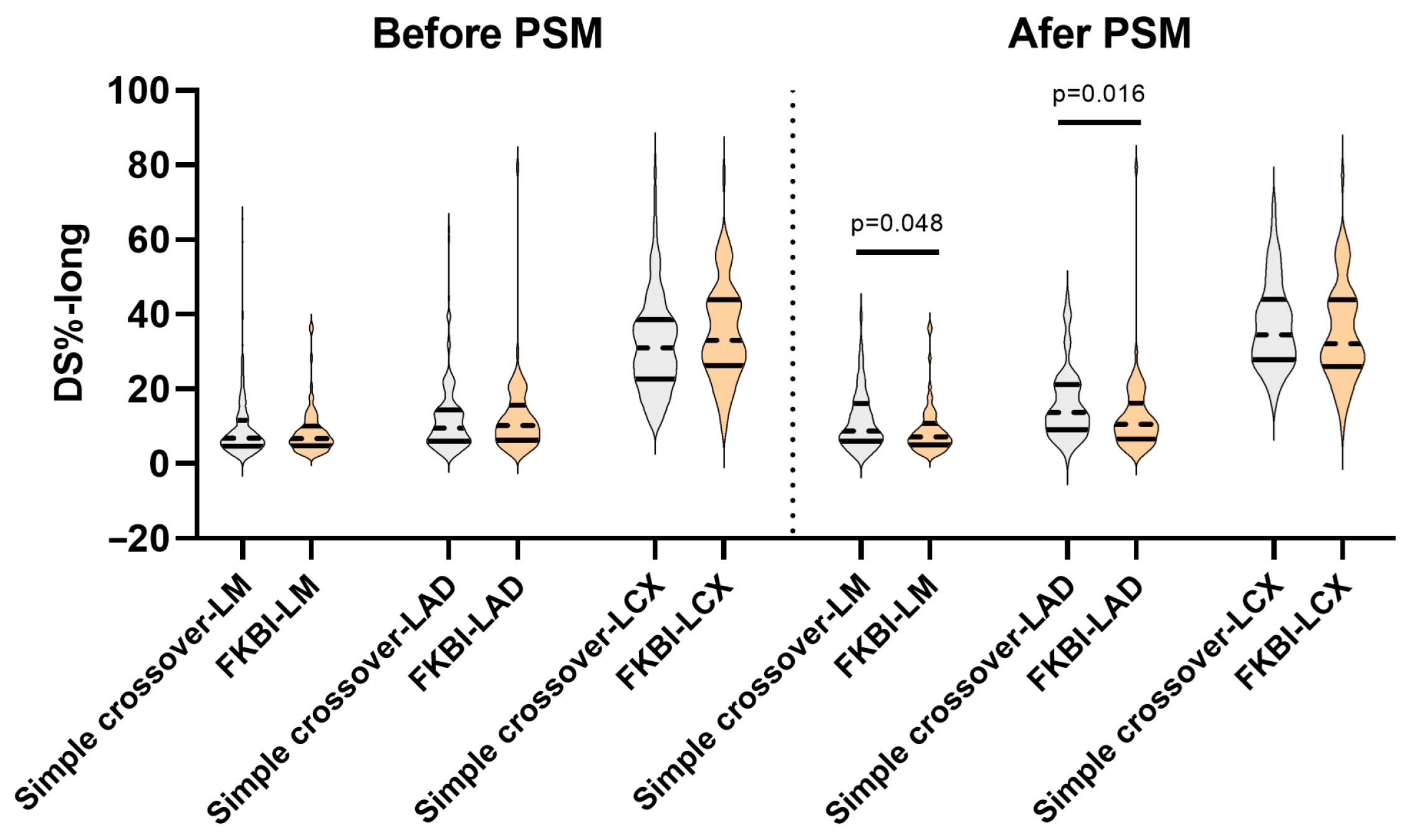
| DS%-long in LM | 6.8 (4.6–11.6) | 6.8 (4.8–10.1) | 0.987 | 8.8 (6–16) | 7.2 (5–10.8) | 0.048 |
| DS%-long in LAD | 9.6 (6–14.4) | 10.2 (6.2–15.6) | 0.656 | 13.7 (9.1–21.2) | 10.6 (6.6–16.2) | 0.016 |
| DS%-long in LCX | 31 (22.6–38.6) | 33.1 (26.2–43.9) | 0.083 | 34.5 (27.9–44) | 32.1 (26–43.9) | 0.293 |
| Pre-Procedure | Post-Procedure | Follow-Up | p Value | ||
|---|---|---|---|---|---|
| Before PSM | Simple crossover | 2.57 (2.13–3.07) | 2.74 (2.28–3.15) | 2.87 (2.45–3.22) | <0.001 |
| FKBI | 2.36 (1.89–2.9) | 2.54 (2.23–2.84) | 2.59 (2.15–2.89) | 0.68 | |
| After PSM | Simple crossover | 2.5 (2.15–3.04) | 2.8 (2.27–3.16) | 2.8 (2.5–3.18) | 0.011 |
| FKBI | 2.35 (1.87–2.93) | 2.52 (2.24–2.86) | 2.52 (2.12–2.89) | 0.664 |
| Variables Predicting DS%-Long in LAD | B | SE | β | t | p Value | VIF | R | R2 | D-W | |
|---|---|---|---|---|---|---|---|---|---|---|
| Before PSM | Simple crossover | 0.227 | 0.052 | 2.036 | ||||||
| F = 5.278 | p = 0.006 | |||||||||
| AMR-pre | 2.893 | 0.891 | 0.239 | 3.247 | 0.001 | 1.107 | ||||
| AMR-post | −1.258 | 1.111 | −0.083 | −1.132 | 0.259 | 1.107 | ||||
| FKBI | 0.046 | 0.002 | 1.401 | |||||||
| F = 0.072 | p = 0.931 | |||||||||
| AMR-pre | −0.321 | 1.43 | −0.028 | −0.225 | 0.823 | 1.008 | ||||
| AMR-post | −0.702 | 2.483 | −0.035 | −0.283 | 0.778 | 1.008 | ||||
| After PSM | Simple crossover | 0.398 | 0.158 | 1.887 | ||||||
| F = 5.45 | p = 0.007 | |||||||||
| AMR-pre | 4.921 | 1.75 | 0.36 | 2.811 | 0.007 | 1.13 | ||||
| AMR-post | 1.24 | 1.834 | 0.087 | 0.676 | 0.502 | 1.13 | ||||
| FKBI | 0.075 | 0.006 | 2.03 | |||||||
| F = 0.162 | p = 0.85 | |||||||||
| AMR-pre | −0.645 | 1.525 | −0.056 | −0.423 | 0.674 | 1.005 | ||||
| AMR-post | −0.959 | 2.735 | −0.046 | −0.351 | 0.727 | 1.005 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, E.; Hu, D.; Zheng, H.; Chen, L.; Cai, W. Role of Final Kissing Balloon Inflation in Left Main Distal Bifurcation Single Stenting: Insights from Angiographic Microvascular Resistance. Medicina 2025, 61, 2062. https://doi.org/10.3390/medicina61112062
Chen E, Hu D, Zheng H, Chen L, Cai W. Role of Final Kissing Balloon Inflation in Left Main Distal Bifurcation Single Stenting: Insights from Angiographic Microvascular Resistance. Medicina. 2025; 61(11):2062. https://doi.org/10.3390/medicina61112062
Chicago/Turabian StyleChen, En, Danqing Hu, Hong Zheng, Lianglong Chen, and Wei Cai. 2025. "Role of Final Kissing Balloon Inflation in Left Main Distal Bifurcation Single Stenting: Insights from Angiographic Microvascular Resistance" Medicina 61, no. 11: 2062. https://doi.org/10.3390/medicina61112062
APA StyleChen, E., Hu, D., Zheng, H., Chen, L., & Cai, W. (2025). Role of Final Kissing Balloon Inflation in Left Main Distal Bifurcation Single Stenting: Insights from Angiographic Microvascular Resistance. Medicina, 61(11), 2062. https://doi.org/10.3390/medicina61112062






