Clinical, Laboratory and Instrumental Characteristics of Myocardial Infarction in Young Patients Depending on the Prevalence of Coronary Atherosclerosis
Abstract
1. Introduction
2. Materials and Methods
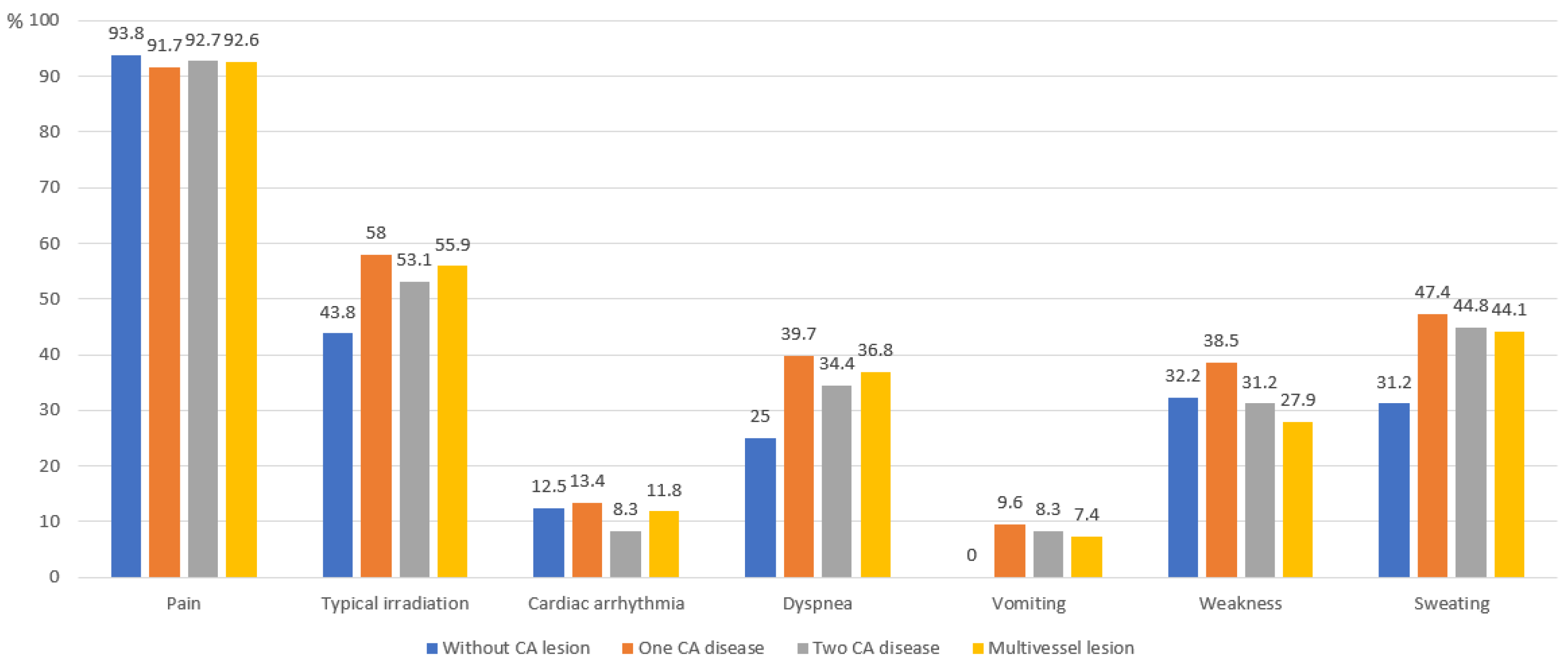
3. Results
4. Discussion
5. Conclusions
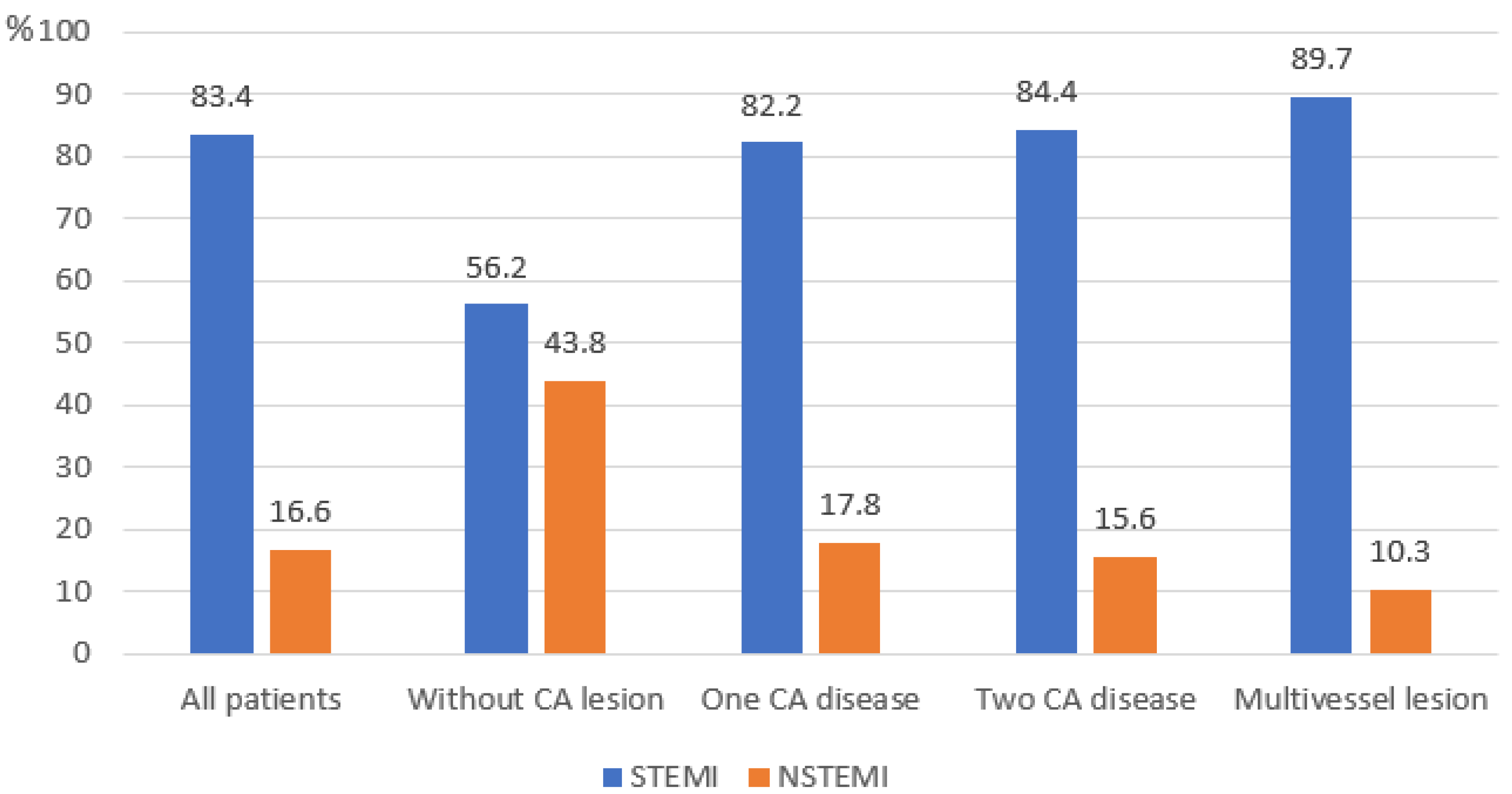
- MI in young Russians is characterized by an extremely high prevalence of modifiable risk factors (smoking, obesity, dyslipidemia), a significant proportion of extensive atherosclerosis (43.9%), and a high frequency of STEMI (83.4%). However, this high prevalence may also reflect referral bias to a specialized cardiology center, where classic STEMI cases are more frequently admitted. This rate exceeds other studies and requires validation in prospective, population-based cohorts.
- Alongside atherosclerotic forms, a clinically significant MINOCA subgroup (4.3%) was identified. Its lower prevalence compared to international data requires further investigation.
- It is necessary to strengthen both primary prevention, aimed at risk factor control among youth, and secondary prevention.
- Key directions for future work include organizing prospective multicenter studies utilizing modern imaging methods for an in-depth investigation of pathophysiology, including MINOCA, and for assessing long-term outcomes in this patient category.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MI | Myocardial infarction |
| RF | Risk factors |
| CA | Coronary artery |
| CAD | Coronary artery disease |
| PCI | Percutaneous coronary intervention |
| MINOCA | Myocardial infarction with non-obstructive coronary arteries |
| CAG | Coronary angiography |
| RR | Respiratory rate |
| SBP | Systolic blood pressure |
| DBP | Diastolic blood pressure |
| HR | Heart rate |
| AST | Aspartate aminotransferase |
| ALT | Alanine aminotransferase |
| APTT | Activated partial thromboplastin time |
| PTI | The prothrombin index |
| CK-MB | Creatine phosphokinase-MB |
| TC | Total cholesterol |
| LDL | Low-density lipoproteins |
| HDL | High-density lipoproteins |
| TG | Triglycerides |
| EchoCG | Echocardiography |
| LVEF | Left ventricle ejection fraction |
| LVIDd | Left ventricle diastolic dimension |
| LVIDs | Left ventricle systolic dimension |
| LA | Left atrium |
| LVPWT | Left ventricular posterior wall thickness |
| RV | Right ventricle |
| LV | Left ventricle |
| STEMI | Myocardial infarction with ST segment elevation |
| NSTEMI | Myocardial infarction without ST segment elevation |
| PCI & CAS | Percutaneous coronary intervention and coronary artery stenting |
| BAB | Beta-blockers |
| ACE inhibitors | Angiotensin-converting enzyme inhibitors |
| ARBs | Angiotensin II receptor blockers |
References
- Averkov, O.V.; Harutyunyan, G.K.; Duplyakov, D.V.; Konstantinova, E.V.; Konstantinova, N.N.; Shakhnovich, R.M.; Yavelov, I.S.; Yakovlev, A.N.; Abugov, S.A.; Alekyan, B.G.; et al. 2024 Clinical practice guidelines for Acute myocardial infarction with ST segment elevation electrocardiogram. Russ. J. Cardiol. 2025, 30, 6306. [Google Scholar] [CrossRef]
- Arora, S.; Stouffer, G.A.; Kucharska-newton, A.M.; Qamar, A.; Vaduganathan, M.; Pandey, A.; Mph, D.L.B.; Caughey, M.C. Twenty Year Trends and Sex Differences in Young Adults Hospitalized with Acute Myocardial Infarction: The ARIC Community Surveillance Study. Circulation 2019, 139, 1047–1056. [Google Scholar] [CrossRef]
- Ponomarenko, I.V.; Sukmanova, I.A.; Elykomov, V.A. Acute coronary syndrome in young patients: Clinical features and risk factors. Cardiovasc. Ther. Prev. 2018, 17, 13–19. [Google Scholar] [CrossRef]
- Karetnikova, V.N.; Neeshpapa, A.G.; Peganova, K.A. Traditional and non-traditional risk factors for myocardial infarction in young adults. Russ. Med. Inq. 2024, 8, 26–30. [Google Scholar] [CrossRef]
- Dattoli-García, C.A.; Jackson-Pedroza, C.N.; Gallardo-Grajeda, A.L.; Gopar-Nieto, R.; Araiza-Garaygordobil, D.; Arias-Mendoza, A. Acute myocardial infarction: Review on risk factors, etiologies, angiographic characteristics and outcomes in young patients. Arch. Cardiol. Mex. 2021, 91, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Shah, N.; Kelly, A.-M.; Cox, N.; Wong, C.; Soon, K. Myocardial Infarction in the “Young”: Risk Factors, Presentation, Management and Prognosis. Hear. Lung Circ. 2016, 25, 955–960. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; The Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth universal definition of myocardial infarction (2018). Circulation 2018, 138, e618–e651, Erratum in Circulation 2018, 39, e652. https://doi.org/10.1161/CIR.0000000000000632. [Google Scholar] [CrossRef]
- Yang, J.; Biery, D.W.; Singh, A.; Divakaran, S.; DeFilippis, E.M.; Wu, W.Y.; Klein, J.; Hainer, J.; Ramsis, M.; Natarajan, P.; et al. Risk Factors and Outcomes of Very Young Adults Who Experience Myocardial Infarction: The Partners YOUNG-MI Registry. Am. J. Med. 2020, 133, 605–612. [Google Scholar] [CrossRef] [PubMed]
- Andreenko, E.Y.; Yavelov, I.S.; Loukianov, M.M.; Vernohaeva, A.N.; Drapkina, O.M.; A Boytsov, S. Ischemic heart disease in subjects of young age: Current state of the problem: Prevalence and cardio-vascular risk factors. Kardiologiya 2018, 58, 53–58. [Google Scholar] [CrossRef]
- Barbarash, O.L.; Sedykh, D.Y.; Bykova, I.S.; Kashtalap, V.V.; Erlich, A.D. Risk factors, clinical features of the course of myocardial infarction and treatment of young patients based on two hospital registries. Ration. Pharmacother. Cardiol. 2020, 16, 250–257. [Google Scholar] [CrossRef]
- Hambraeus, K.; Tydén, P.; Lindahl, B. Time trends and gender differences in prevention guideline adherence and outcome after myocardial infarction: Data from the SWEDEHEART registry. Eur. J. Prev. Cardiol. 2016, 23, 340–348. [Google Scholar] [CrossRef]
- Lee, S.H.; Kim, J.H.; Jeong, M.H.; Park, H.; Jeong, Y.A.; Ahn, Y.; Kim, J.H.; Chae, S.C.; Kim, Y.J.; Hur, S.H.; et al. Clinical characteristics and outcomes of acute st-segment elevation myocardial infarction in younger Korean adults. Korean Circ. J. 2015, 45, 275–284. [Google Scholar] [CrossRef]
- Tian, X.; Chen, S.; Zuo, Y.; Zhang, Y.; Zhang, X.; Xu, Q.; Luo, Y.; Wu, S.; Wang, A. Association of lipid, inflammatory, and metabolic biomarkers with age at onset for incident cardiovascular disease. BMC Med. BioMed Cent. 2022, 20, 383. [Google Scholar] [CrossRef]
- Ishida, M.; Sakai, C.; Kobayashi, Y.; Ishida, T. Cigarette Smoking and Atherosclerotic Cardiovascular Disease. J. Atheroscler. Thromb. 2024, 31, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Addisu, B.; Bekele, S.; Wube, T.B.; Hirigo, A.T.; Cheneke, W. Dyslipidemia and its associated factors among adult cardiac patients at Ambo university referral hospital, Oromia region, west Ethiopia. BMC Cardiovasc. Disord. BioMed Cent. 2023, 23, 321. [Google Scholar] [CrossRef]
- Lee, S.-E.; Chang, H.-J.; Sung, J.M.; Park, H.-B.; Heo, R.; Rizvi, A.; Lin, F.Y.; Kumar, A.; Hadamitzky, M.; Kim, Y.J.; et al. Effects of Statins on Coronary Atherosclerotic Plaques: The PARADIGM Study. JACC Cardiovasc. Imaging 2018, 11, 1475–1484. [Google Scholar] [CrossRef]
- Kashtalap, V.; Barbarash, O.; Hryachkova, O.; Novitskaya, A. Relationship between lipid disorders and severity and nature of coronary artery lesions in patients with coronary artery disease. Med. Kuzbass. 2016, 15, 63–68. [Google Scholar] [CrossRef]
- Qiao, Y.N.; Zou, Y.L.; Guo, S.D. Low-density lipoprotein particles in atherosclerosis. Front. Physiol. 2022, 13, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Malekmohammad, K.; Bezsonov, E.E.; Rafieian-Kopaei, M. Role of lipid accumulation and inflammation in atherosclerosis: Focus on molecular and cellular mechanisms. Front. Cardiovasc. Med. 2021, 8, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Sim, D.S.; Jeong, M.H. Twenty-Year Clinical Experience of the Korea Acute Myocardial Infarction Registry. Korean Circ. J. 2025, 55, 757. [Google Scholar] [CrossRef]
- Peerwani, G.; Hanif, B.; Rahim, K.A.; Kashif, M.; Virani, S.S.; Sheikh, S. Presentation, management, and early outcomes of young acute coronary syndrome patients- analysis of 23,560 South Asian patients from 2012 to 2021. BMC Cardiovasc. Disord. 2024, 24, 378. [Google Scholar] [CrossRef] [PubMed]
- Zasada, W.; Bobrowska, B.; Plens, K.; Dziewierz, A.; Siudak, Z.; Surdacki, A.; Dudek, D.; Bartuś, S. Acute myocardial infarction in young patients. Kardiol. Pol. 2021, 79, 1093–1098. [Google Scholar] [CrossRef]
- Tamis-Holland, J.E.; Jneid, H.; Reynolds, H.R.; Agewall, S.; Brilakis, E.S.; Brown, T.M.; Lerman, A.; Cushman, M.; Kumbhani, D.J.; Arslanian-Engoren, C.; et al. Contemporary Diagnosis and Management of Patients with Myocardial Infarction in the Absence of Obstructive Coronary Artery Disease: A Scientific Statement from the American Heart Association. Circulation 2019, 139, E891–E908. [Google Scholar] [CrossRef]
- Barr, P.R.; Harrison, W.; Smyth, D.; Flynn, C.; Lee, M.; Kerr, A.J. Myocardial Infarction Without Obstructive Coronary Artery Disease is Not a Benign Condition (ANZACS-QI 10). Heart Lung Circ. 2018, 27, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Gulati, R.; Behfar, A.; Narula, J.; Kanwar, A.; Lerman, A.; Cooper, L.; Singh, M. Acute Myocardial Infarction in Young Individuals. Mayo Clin. Proc. 2020, 95, 136–156. [Google Scholar] [CrossRef] [PubMed]
- Canton, L.; Fedele, D.; Bergamaschi, L.; Foà, A.; Di Iuorio, O.; Tattilo, F.P.; Rinaldi, A.; Angeli, F.; Armillotta, M.; Sansonetti, A.; et al. Sex- and age-related differences in outcomes of patients with acute myocardial infarction: MINOCA vs. MIOCA. Eur. Heart J. Acute Cardiovasc. Care 2023, 12, 604–614. [Google Scholar] [CrossRef]
- Rakowski, T.; De Luca, G.; Siudak, Z.; Plens, K.; Dziewierz, A.; Kleczyński, P.; Tokarek, T.; Węgiel, M.; Sadowski, M.; Dudek, D. Characteristics of patients presenting with myocardial infarction with non-obstructive coronary arteries (MINOCA) in Poland: Data from the ORPKI national registry. J. Thromb. Thrombolysis 2019, 47, 931931. [Google Scholar] [CrossRef]
| Indicator | All Patients (n = 374) | No CA Lesion (n = 16) | Single-Vessel Disease (n = 157) | Two-Vessel Disease (n = 96) | Multi-Vessel Disease (n = 68) | p |
|---|---|---|---|---|---|---|
| Age, years, Me (IQR) | 41.0 [37.0; 43.0] | 40.0 [36.0; 41.0] | 41.0 [37.0; 43.0] | 41.0 [37.8; 44.0] | 41.0 [38.0; 43.0] | 0.282 |
| Male, n (%) | 341 (91.2) | 15 (93.8) | 141 (89.8) | 90 (93.8) | 63 (92.6) | 0.697 |
| Pre-obesity, n (%) | 159 (42.5) | 7 (43.8) | 70 (44.6) | 33 (34.4) | 35 (51.5) | 0.052 |
| Obesity class I, n (%) | 95 (25.4) | 1 (6.2) | 36 (22.9) | 26 (27.1) | 21 (30.9) | |
| Obesity class II, n (%) | 34 (9.1) | 1 (6.2) | 20 (12.7) | 9 (9.4) | 3 (4.4) | |
| Obesity class III, n (%) | 9 (2.4) | 0 (0.0) | 3 (1.9) | 3 (3.1) | 2 (2.9) | |
| Smoking, n (%) | 290 (77.5) | 8 (50.0) | 129 (82.2) | 73 (76.0) | 52 (76.5) | 0.028 p1–2 = 0.015 |
| Burdened heredity 1, n (%) | 172 (46.0) | 4 (25.0) | 68 (43.3) | 46 (47.9) | 34 (50.0) | 0.286 |
| Arterial hypertension, n (%) | 277 (74.1) | 12 (75.0) | 116 (73.9) | 72 (75.0) | 55 (80.9) | 0.729 |
| Diabetes mellitus or impaired glucose tolerance, n (%) | 69 (18.4) | 1 (6.2) | 26 (16.6) | 20 (20.8) | 17 (25.0) | 0.251 |
| STEMI 2, n (%) | 312 (83.4) | 9 (56.2) | 129 (82.2) | 81 (84.4) | 61 (89.7) | 0.015 p1–3 = 0.044 p1–4 = 0.007 |
| NSTEMI 3, n (%) | 62 (16.6) | 7 (43.8) | 28 (17.8) | 15 (15.6) | 7 (10.3) |
| Indicator | All Patients (n = 374) | No CA Lesion (n = 16) | Single-Vessel Disease (n = 157) | Two-Vessel Disease (n = 96) | Multi-Vessel Disease (n = 68) | p |
|---|---|---|---|---|---|---|
| RR 1, breath per min | 16.0 [16.0; 17.0] | 17.0 [16.0; 17.0] | 16.0 [16.0; 17.0] | 16.0 [16.0; 17.0] | 16.0 [16.0; 18.0] | 0.326 |
| SBP 2 at admission, mmHg. | 132.0 [120.0; 150.0] | 140.0 [130.0; 162.5] | 130.0 [120.0; 150.0] | 140.0 [120.0; 150.0] | 140.0 [128.8; 150.0] | 0.536 |
| DBP 3 at admission, mmHg. | 80.0 [80.0; 90.0] | 82.5 [80.0; 92.5] | 80.0 [80.0; 90.0] | 84.5 [80.0; 90.0] | 90.0 [80.0; 90.0] | 0.545 |
| HR 4, bpm | 78.0 [70.0; 89.0] | 85.5 [73.0; 90.5] | 76.0 [67.0; 85.0] | 80.0 [72.0; 90.0] | 78.0 [70.0; 88.0] | 0.006 p2–3 = 0.012 |
| Indicator | All Patients (n = 374) | No CA Lesion (n = 16) | Single-Vessel Disease (n = 157) | Two-Vessel Disease (n = 96) | Multi-Vessel Disease (n = 68) | p |
|---|---|---|---|---|---|---|
| Hemoglobin max, g/L | 155.0 [147.0; 163.3] | 150.00 [143.75; 159.50] | 155.00 [148.00; 164.00] | 154.50 [149.75; 166.00] | 157.00 [148.50; 162.00] | 0.484 |
| White blood cells max, 109/L | 12.3 [9.7; 15.7] | 9.73 [7.77; 12.50] | 13.00 [10.20; 16.20] | 12.20 [9.85; 15.94] | 12.07 [9.62; 14.45] | 0.010 p1–2. 1–3 < 0.05 |
| AST 1 max, U/L | 86.0 [40.6; 223.7] | 66.67 [41.65; 109.12] | 84.80 [46.00; 230.80] | 108.00 [48.25; 248.00] | 106.70 [42.51; 247.50] | 0.500 |
| ALT 2 max, U/L | 56.3 [37.2; 83.9] | 60.75 [36.67; 72.55] | 56.30 [39.20; 83.30] | 60.80 [39.85; 91.19] | 51.80 [37.05; 81.64] | 0.696 |
| Total bilirubin max, μmol/L | 12.5 [8.9; 17.1] | 16.34 [12.20; 20.18] | 12.20 [8.60; 16.30] | 12.50 [8.98; 18.06] | 12.70 [9.50; 16.10] | 0.171 |
| APTT 3, s | 31.4 [27.9; 37.7] | 32.15 [27.73; 35.77] | 31.30 [28.00; 36.45] | 31.90 [28.00; 41.60] | 31.50 [27.30; 37.00] | 0.730 |
| PTI 4, % | 0.9 [0.9; 1.0] | 0.99 [0.88; 1.00] | 0.93 [0.88; 1.00] | 0.93 [0.88; 1.00] | 0.93 [0.87; 1.00] | 0.774 |
| Troponin I max, ng/mL | 10.7 [1.0; 50.0] | 4.68 [1.00; 358.02] | 13.80 [1.00; 50.00] | 13.40 [1.00; 50.00] | 9.16 [1.00; 44.95] | 0.788 |
| CK-MB 5 max, U/L | 132.7 [41.0; 329.9] | 48.00 [28.60; 131.38] | 177.72 [51.00; 328.50] | 157.00 [54.50; 469.50] | 143.00 [66.50; 341.00] | 0.036 p1–2. 1–3. 1–4 < 0.05 |
| Fasting glucose max, mmol/L | 5.8 [5.1; 6.8] | 6.05 [5.40; 6.90] | 5.68 [5.10; 6.74] | 6.03 [5.30; 6.89] | 5.86 [5.12; 6.79] | 0.233 |
| Creatinine max, μmol/L | 94.0 [83.0; 105,1] | 101.25 [78.17; 116.15] | 96.00 [81.50; 103.30] | 94.00 [82.50; 105.85] | 93.00 [85.50; 102.70] | 0.958 |
| TC 6 max, mmol/L | 5.3 [4.5; 6.2] | 4.65 [3.68; 5.21] | 5.29 [4.51; 6.19] | 5.32 [4.37; 6.37] | 5.70 [5.04; 6.51] | 0.004 p1–4 = 0.003 |
| LDL 7 max, mmol/L | 3.1 [2.4; 3.8] | 2.57 [1.92; 2.79] | 3.13 [2.48; 3.80] | 3.12 [2.41; 3.83] | 3.33 [2.62; 4.29] | 0.005 p1–2. 1–3. 1–4 < 0.05 |
| HDL 8 max, mmol/L | 1.1 [0.9; 1.3] | 1.15 [1.02; 1.48] | 1.04 [0.89; 1.25] | 1.12 [0.90; 1.34] | 1.03 [0.90; 1.21] | 0.292 |
| TG 9 max, mmol/L | 1.8 [1.1; 2.5] | 1.68 [0.82; 2.50] | 1.85 [1.15; 2.75] | 1.55 [1.07; 2.23] | 1.88 [1.27; 2.30] | 0.286 |
| Indicator | All Patients (n = 374) | No CA Lesion (n = 16) | Single-Vessel Disease (n = 157) | Two-Vessel Disease (n = 96) | Multi-Vessel Disease (n = 68) | p |
|---|---|---|---|---|---|---|
| LVIDd 1, Me [IQR] | 5.4 [5.1; 5.7] | 5.54 [5.28; 5.63] | 5.30 [5.00; 5.60] | 5.50 [5.20; 5.80] | 5.50 [5.10; 5.70] | 0.010 p2–3 = 0.019 |
| LVIDs 2, Me [IQR] | 3.8 [3.6; 4.2] | 3.84 [3.60; 4.24] | 3.70 [3.50; 4.00] | 3.90 [3.62; 4.28] | 3.90 [3.60; 4.22] | 0.018 p2–3 = 0.035 |
| LA 3, Me [IQR] | 3.9 [3.6; 4.1] | 3.90 [3.50; 3.98] | 3.85 [3.60; 4.10] | 4.00 [3.60; 4.13] | 3.90 [3.65; 4.14] | 0.623 |
| Interventricular septum thickness, Me [IQR] | 1.1 [1.0; 1.2] | 1.00 [0.97; 1.10] | 1.06 [1.00; 1.18] | 1.10 [0.98; 1.19] | 1.08 [1.00; 1.17] | 0.646 |
| LVPWT 4, Me [IQR] | 1.0 [0.9; 1.1] | 1.00 [0.90; 1.00] | 1.00 [0.90; 1.02] | 1.00 [0.90; 1.10] | 1.00 [0.90; 1.08] | 0.782 |
| RV 5, Me [IQR] | 2.5 [2.3; 2.7] | 2.55 [2.20; 2.79] | 2.50 [2.40; 2.70] | 2.50 [2.30; 2.68] | 2.50 [2.31; 2.60] | 0.795 |
| LVEF 6, Me [IQR] | 52.0 [47.0; 60.0] | 54.50 [50.00; 61.25] | 53.00 [48.00; 60.00] | 51.00 [46.25; 57.00] | 52.00 [48.00; 58.50] | 0.195 |
| LVEF, abs. (%) | 0.407 | |||||
| -LVEF ≤ 50% | 150 (41.1) | 6 (37.5) | 56 (36.4) | 44 (46.8) | 29 (43.3) | |
| -LVEF > 50% | 214 (58.9) | 10 (62.5) | 98 (63.6) | 50 (53.2) | 38 (56.7) | |
| Akinesia zones, abs. (%) | 146 (40) | 2 (12.5%) | 60 (39.0%) | 40 (42.6%) | 23 (34.3%) | 0.128 |
| Hypokinesia zones, abs. (%) | 240 (65.8) | 15 (93.8%) | 93 (60.4%) | 62 (66.0%) | 49 (73.1%) | 0.027 p1–2 = 0.050 |
| STEMI 1 | ||||||
|---|---|---|---|---|---|---|
| Indicator | All patients (n = 280) | No CA Lesion (n = 9) | Single-Vessel Disease (n = 129) | Two-Vessel Disease (n = 81) | Multi-Vessel Disease (n = 61) | p |
| Thrombolysis, abs (%) | 10 (3.6) | 3 (33.3) | 5 (3.9) | 0 (0.0) | 2 (3.3) | <0.001 p1–2. 1–3. 1–4 < 0.05 |
| PTCA & CAS 2, abs. (%) | 179 (63.9) | 0 (0.0) | 78 (60.5) | 58 (71.6) | 43 (70.5) | <0.001 p1–2. 1–3. 1–4 < 0.05 |
| Pharmaco-invasive strategy, abs. (%) | 74 (26.4) | 0 (0.0) | 40 (31.0) | 20 (24.7) | 14 (23.0) | 0.163 |
| Without reperfusion, abs. (%) | 17 (6.1) | 6 (66.7) | 6 (4.7) | 3 (3.7) | 2 (3.3) | <0.001 p1–2. 1–3. 1–4 < 0.05 |
| NSTEMI3 | ||||||
| Indicator | All patients(n = 57) | No CA Lesion (n = 7) | Single-Vessel Disease (n = 28) | Two-Vessel Disease (n = 15) | Multi-Vessel Disease (n = 7) | p |
| PTCA & CAS, aбc. (%) | 44 (77.2) | 0 (0.0) | 23 (82.1) | 15 (100.0) | 6 (85.7) | <0.001 p1–2. 1–3. 1–4 < 0.05 |
| Without reperfusion, abs. (%) | 13 (22.8) | 7 (100.0) | 5 (17.9) | 0 (0.0) | 1 (14.3) | <0.001 p1–2. 1–3. 1–4 < 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nozhov, G.V.; Pereverzeva, K.G.; Zagorodniy, S.S.; Yakushin, S.S.; Platonova, E.S.; Sermavbrina, A.V.; Popov, G.M.; Martynova, E.R. Clinical, Laboratory and Instrumental Characteristics of Myocardial Infarction in Young Patients Depending on the Prevalence of Coronary Atherosclerosis. Medicina 2025, 61, 1996. https://doi.org/10.3390/medicina61111996
Nozhov GV, Pereverzeva KG, Zagorodniy SS, Yakushin SS, Platonova ES, Sermavbrina AV, Popov GM, Martynova ER. Clinical, Laboratory and Instrumental Characteristics of Myocardial Infarction in Young Patients Depending on the Prevalence of Coronary Atherosclerosis. Medicina. 2025; 61(11):1996. https://doi.org/10.3390/medicina61111996
Chicago/Turabian StyleNozhov, Gleb Vladimirovich, Kristina Gennadievna Pereverzeva, Sergey Sergeevich Zagorodniy, Sergey Stepanovich Yakushin, Elizaveta Sergeevna Platonova, Angelina Vladimirovna Sermavbrina, German Maksimovich Popov, and Elizaveta Romanovna Martynova. 2025. "Clinical, Laboratory and Instrumental Characteristics of Myocardial Infarction in Young Patients Depending on the Prevalence of Coronary Atherosclerosis" Medicina 61, no. 11: 1996. https://doi.org/10.3390/medicina61111996
APA StyleNozhov, G. V., Pereverzeva, K. G., Zagorodniy, S. S., Yakushin, S. S., Platonova, E. S., Sermavbrina, A. V., Popov, G. M., & Martynova, E. R. (2025). Clinical, Laboratory and Instrumental Characteristics of Myocardial Infarction in Young Patients Depending on the Prevalence of Coronary Atherosclerosis. Medicina, 61(11), 1996. https://doi.org/10.3390/medicina61111996





