Abstract
Background and Objectives: A novel synthetic self-assembling peptide, PuraStat, has been introduced as a hemostatic agent. This case series aimed to evaluate the clinical efficacy of PuraStat for gastrointestinal bleeding during emergency endoscopy. Cases: Twenty-five patients with gastrointestinal bleeding who had undergone emergency endoscopy with PuraStat between August 2021 and December 2022 were retrospectively examined. Six patients were receiving antithrombotic agents, and ten patients with refractory gastrointestinal bleeding had undergone at least one endoscopic hemostatic procedure. The breakdown of bleeding was gastroduodenal ulcer/erosion in 12 cases, bleeding after gastroduodenal or colorectal endoscopic resection in 4 cases, rectal ulcer in 2 cases, postoperative anastomotic ulcer in 2 cases, and gastric cancer, diffuse antral vascular ectasia, small intestinal ulcer, colonic diverticular bleeding, and radiation proctitis in each case. The method of hemostasis was only PuraStat application in six cases, and hemostasis in combination with high-frequency hemostatic forceps, hemostatic clip, argon plasma coagulation, and hemostatic agents (i.e., thrombin) in the remaining cases. Rebleeding was observed in three cases. Hemostatic efficiency was observed in 23 cases (92%). Conclusions: PuraStat has the expected hemostatic effect on gastrointestinal bleeding during emergency endoscopy. The use of PuraStat should be considered in emergency endoscopic hemostasis of gastrointestinal bleeding.
1. Introduction
A novel synthetic self-assembling peptide, PuraStat (3-D Matrix Ltd., Tokyo, Japan), has been introduced as a surgical or endoscopic hemostatic agent [1,2]. PuraStat is indicated for the hemostasis of oozing bleeding in the parenchyma of solid organs, vascular anastomoses, and capillaries of the gastrointestinal tract [2,3,4,5]. The peptide molecule in PuraStat consists of a repeating sequence of three types of amino acids: Arginine, Alanine, and Aspartic Acid, and has a β-sheet structure [3]. The peptide self-assembles into an extracellular scaffold matrix when activated by a pH change associated with exposure to the blood. The matrix sticks to and seals the blood vessels, thereby achieving hemostasis as a mechanical barrier. In addition, the activated matrix promotes tissue proliferation and facilitates effective mucosa healing [2]. Therefore, excluding spurting bleeding, general cases of gastrointestinal bleeding are indicated for hemostasis with PuraStat.
Gastrointestinal bleeding is a medical emergency associated with elevated morbidity and mortality and significant costs to the healthcare system. However, there have been few studies on the efficacy of PuraStat for gastrointestinal bleeding during emergency endoscopic hemostasis. The aim of our study was to assess the safety, efficacy, and technical feasibility of PuraStat as a primary hemostat during emergency endoscopy. Herein, we report a case series of endoscopic hemostasis using PuraStat for gastrointestinal bleeding during an emergency endoscopy.
2. Case Descriptions
This retrospective observational study was conducted at the Juntendo University Hospital in Tokyo, Japan. This study included all patients who underwent emergency endoscopic hemostasis using PuraStat for gastrointestinal bleeding between August 2021 and December 2022. Cases in which PuraStat was used during scheduled endoscopic procedures were excluded. Five experienced endoscopists performed all procedures. Patient clinical data, including age; sex; symptoms; underlying disease; use of antithrombotic drugs; necessity of blood transfusion; hemoglobin levels; refractoriness/intractability; causes of gastrointestinal bleeding; and endoscopic procedure data, including the location of the bleeding, types of bleeding, presence or absence of visible vessels, endoscopic hemostasis method, the clinical effectiveness of endoscopic hemostasis, and presence or absence of rebleeding were reviewed. In this study, rebleeding was defined as the development of fresh hematemesis or hematochezia, shock (defined as a systolic blood pressure of ≤90 mmHg or a pulse rate of ≥110 beats per minute) with melena after stabilization, or a drop in hemoglobin of more than 2 g/dL within 24 h. Refractory/intractable bleeding was defined as rebleeding requiring emergency endoscopic hemostasis after failing at least one treatment with endoscopic hemostatic therapy. Clinical effectiveness was defined as achieving no rebleeding within one week after the procedure. All patients were followed up for at least one month after the procedure.
The choice of the hemostasis method was left to the endoscopist. Endoscopic hemostasis using PuraStat was attempted in all cases. When a large amount of blood accumulated in the intestinal tract, it was washed thoroughly with water to identify the bleeding points. PuraStat was applied at the bleeding point using a delivery catheter inserted through the endoscope accessory channel. The procedure was completed after confirming that effective hemostasis was achieved after the wound was covered with a transparent jelly substance of PuraStat.
Twenty-five patients were recruited and treated with PuraStat. The clinical characteristics of the patients are summarized in Table 1. The median age was 73.0 years (range, 40–91 years), and there were twenty men and five women. All but one patient had some underlying medical condition, including cancer, heart disease, diabetes, kidney disease, liver disease, or hypertension, and six were taking antithrombotic drugs. The median hemoglobin level immediately prior to the endoscopic procedure was 7.4 (range 5.0–14.5) g/dL, and 17 patients required red blood cell transfusions. Fifteen of the twenty-five patients had initial bleeding, while the remaining ten patients had refractory or intractable bleeding in which at least one endoscopic hemostasis had been performed before this treatment and resulted in failure.

Table 1.
The Clinical Characteristics of the Studied Patients.
The endoscopic data of the study patients are summarized in Table 2, and the case numbers in Table 2 correspond to those in Table 1. The breakdown of bleeding was gastroduodenal ulcer or erosion, which was the most common type of bleeding; in 12 cases, bleeding after gastroduodenal or colorectal endoscopic resection was observed in 4 cases, acute hemorrhagic rectal ulcer in 2 cases, postoperative anastomotic ulcer in 2 cases, and gastric cancer, diffuse antral vascular ectasia, small intestinal ulcer, colonic diverticular bleeding, and radiation proctitis in each case. Bleeding occurred in various gastrointestinal tracts, including the stomach, duodenum, small intestine, colon, and rectum. The types of bleeding included oozing, bleeding in 22 cases, and spurting bleeding in 3 cases. Five cases had visible vessels. The method of hemostasis was only PuraStat application in six cases, and hemostasis in combination with high-frequency hemostatic forceps, hemostatic clip, argon plasma coagulation, and hemostatic agents (i.e., thrombin) in the remaining nineteen cases. Rebleeding was observed in only three cases, one of which occurred 10 days after endoscopic hemostasis. Hemostasis was clinically effective in 23 cases (92%), including the aforementioned. All three rebleeding cases underwent endoscopic hemostasis using high-frequency hemostatic forceps and PuraStat and achieved complete hemostasis. No procedure-related side effects were observed in the studied cases.

Table 2.
Endoscopic Data of the Studied Patients.
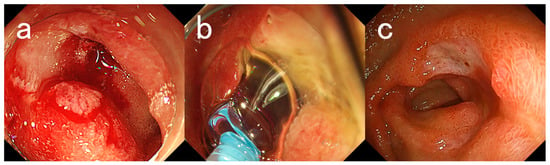
Figure 1.
Endoscopic images for Case #13. A 76-year-old woman with a history of myasthenia and diabetes mellitus presented with melena and underwent emergency endoscopy. (a) An ulcer with bleeding oozing in the duodenal bulb. (b) Application of PuraStat. Hemostasis was achieved by applying 3 mL of PuraStat. (c) Endoscopic image taken 2 weeks later. There was a reduction in the size of the ulcer and healing was observed. The patient has not presented with melena for 4 months after her last endoscopy.
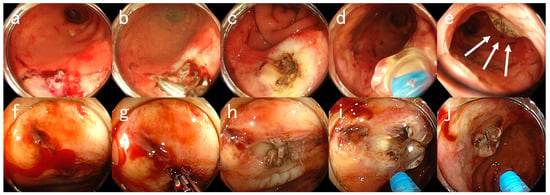
Figure 2.
Endoscopic Images for Case #23. An 80-year-old man with a history of diabetes, chronic kidney disease (on hemodialysis), foot gangrene, and hypertension presented with hematochezia. The patient was taking aspirin. (a–e) First emergency endoscopic views. (a) Ulcers with visible blood vessels in the rectum. (b) High-frequency hemostasis using hemostatic forceps. (c) An ulcer after coagulation. (d) Application of PuraStat. (e) An ulcer attached with PuraStat (arrows). However, 10 days later, massive hematochezia recurred. (f–j) Second emergency endoscopy at rebleeding. (f) An ulcer with active oozing bleeding in the rectum. (g) Re-hemostasis using hemostatic forceps. (h) An ulcer after coagulation. (i) Application of PuraStat. (j) An ulcer attached with PuraStat. Hemostasis was achieved by applying 3 mL of PuraStat. It has been a month since the last endoscopy and the patient has yet to present with hematochezia for one month.
3. Discussion
Endoscopic procedures, surgery, and radiological angiography are the main therapeutic options available for managing gastrointestinal bleeding. Owing to the increasing number of successful endoscopic applications and recent advances in technology, endoscopic procedures are the current standard for hemostasis in patients with gastrointestinal bleeding. In this study, we used PuraStat to treat various gastrointestinal bleeding episodes. The high clinical hemostatic effectiveness of PuraStat was confirmed in patients with underlying disease and/or bleeding diathesis who were taking antithrombotic drugs. It is interesting that hemostatic efficacy was found in 23 out of 25 cases (92%), including 10 cases of refractory or intractable gastrointestinal bleeding. Rebleeding was observed in three cases, while hemostasis was achieved in all cases via endoscopic treatment using PuraStat. de Nucci et al. described the use of PuraStat in 77 patients treated for acute gastrointestinal bleeding, including bleeding occurring as a complication of a previous endoscopic procedure (endoscopic mucosal resection [EMR] and endoscopic retrograde cholangiopancreatography [ERCP]), peptic ulcers, angiodysplasia, cancer, and surgical anastomoses [5]. In their study, the efficacy of PuraStat in primary hemostasis was 90%, and the rebleeding rate was 10%. These findings are consistent with those of this study. In general, the rebleeding rate in patients with peptic ulcers is expected to be 10–20%, and is thought to be two–three times higher in patients taking antithrombotic drugs [6]. In addition, a previous report on acute gastrointestinal bleeding has also shown that rebleeding was significantly associated with patient comorbidities (i.e., cancer, heart disease, diabetes, kidney disease, liver disease, and hypertension), with an odds ratio of 1.2 (95% confidence interval, 1.0–1.4) [7]. The rebleeding rate in this study was lower than estimated, although it could not be compared with that rate. Therefore, endoscopic treatment using PuraStat is expected to have a high hemostatic efficiency. However, further large-scale analyses are required to determine whether PuraStat is effective in patients taking antithrombotic drugs or those with underlying diseases.
Hemostasis with endoscopic clipping or high-frequency hemostatic forceps has been increasingly adopted as a method for hemostasis of the bleeding vessel at the ulcer base. Conventional hemostatic clips achieve hemostasis over the bleeding vessel at the ulcer base through the application of mechanical force between the two jaws. However, secure application of hemoclips to the fibrotic ulcer base can be technically difficult at times [8]. Furthermore, high-frequency hemostatic forceps are endoscopic coagulation devices developed solely for hemostasis. Unlike biopsy forceps, they have a narrow opening angle, small cup, and dull edge to enable pinpoint holding of the target lesion. However, high-frequency coagulation may cause serious complications, such as perforation, due to tissue damage during or after the procedure [9]. In contrast, hemostasis using PuraStat involves only applying PuraStat from a dedicated catheter, which is extremely simple. Subramaniam S et al. used PuraStat in 100 patients undergoing endoscopic resection and stated that only a small amount (mean 1.76 mL) was required for hemostasis, and it took, on average, 69.5 s to stop a bleed [10]. Soons E et al. also reported that it was easy to apply 3 mL of PuraStat to a post-endoscopic mucosal resection defect with a median duration of 2.0 min, and there were no adverse events related to PuraStat application [11]. Similarly, in comparing the conventional hemostatic technique and PuraStat application in patients who developed bleeding associated with endoscopic sphincterotomy, the hemostatic procedure time was significantly shorter in patients using PuraStat, whereas adverse events were significantly less frequently observed in patients using PuraStat [12]. In addition, applying PuraStat does not cause tissue damage due to thermocoagulation; therefore, there is no risk of perforation associated with the procedure. Subramaniam et al. demonstrated that Purastat was an effective hemostat that could reduce heat therapy using coagulation forceps for bleeding during endoscopic submucosal dissection (ESD), resulting in a significant increase in the proportion of patients achieving complete wound healing in the Purastat group compared with controls [13]. Therefore, hemostasis with PuraStat is a simple and safe procedure. The application of PuraStat can be an option for the hemostasis of gastrointestinal bleeding during an emergency endoscopy.
Furthermore, endoscopic hemostasis can be challenging in some scenarios, even for the most experienced endoscopists. The presence of hematic residues and clots in the gastrointestinal tract can pose technical difficulties that may prolong the procedure time or make it impossible [14]. One of the characteristics of PuraStat is that it is a transparent jelly-like substance prone to immiscibility with the blood. Therefore, it is possible to secure a visual field after the application, suggesting that it is easy to identify the bleeding point and confirm hemostasis.
The present study had several limitations. First, it was carried out at a single center and the number of cases was small. Second, PuraStat was not originally indicated for spurting bleeding, although in the present analysis, hemostasis was achieved by applying PuraStat after weakening the bleeding pressure with hemostatic clips or hemostatic forceps, even in three spurting bleeding cases. Third, the method of hemostasis was only PuraStat application in 6 cases, whereas hemostasis in combination with high-frequency hemostatic forceps, hemostatic clips, argon plasma coagulation, and hemostatic agents was used in the remaining 19 cases. It is unclear whether hemostasis was achieved using only the PuraStat or other hemostatic methods. These findings suggest that hemostatic efficiency can be enhanced by combining PuraStat with other hemostatic methods. Fourth, this study was a case series and did not include a control group for comparison. Therefore, further investigation is needed to validate our results and to confirm their clinical effectiveness.
4. Conclusions
In this case series, a self-assembling peptide hemostatic hydrogel, PuraStat, was effective in achieving hemostasis of gastrointestinal bleeding during emergency endoscopy. The use of PuraStat should be considered in emergency endoscopic hemostasis of gastrointestinal bleeding.
Author Contributions
T.M. mainly contributed to this work and wrote the manuscript. E.K., K.H., Y.A., H.U., T.S., M.H. and A.N. contributed equally to this work. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board and the Ethical Committee of Juntendo University Hospital (reference number: #E22-0454, approved on 10 March 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets of the current study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Yoshida, M.; Goto, N.; Kawaguchi, M.; Koyama, H.; Kuroda, J.; Kitahora, T.; Iwasaki, H.; Suzuki, S.; Kataoka, M.; Takashi, F.; et al. Initial clinical trial of a novel hemostat, TDM-621, in the endoscopic treatments of the gastric tumors. J. Gastroenterol. Hepatol. 2014, 29 (Suppl. 4), 77–79. [Google Scholar] [CrossRef] [PubMed]
- Uraoka, T.; Ochiai, Y.; Fujimoto, A.; Goto, O.; Kawahara, Y.; Kobayashi, N.; Kanai, T.; Matsuda, S.; Kitagawa, Y.; Yahagi, N. A novel fully synthetic and self-assembled peptide solution for endoscopic submucosal dissection-induced ulcer in the stomach. Gastrointest. Endosc. 2016, 83, 1259–1264. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.F.; Ma, Z.; Ananda, A. A novel haemostatic agent based on self-assembling peptides in the setting of nasal endoscopic surgery, a case series. Int. J. Surg. Case Rep. 2017, 41, 461–464. [Google Scholar] [CrossRef] [PubMed]
- Giritharan, S.; Salhiyyah, K.; Tsang, G.M.; Ohri, S.K. Feasibility of a novel, synthetic, self-assembling peptide for suture-line haemostasis in cardiac surgery. J. Cardiothorac. Surg. 2018, 13, 68. [Google Scholar] [CrossRef] [PubMed]
- de Nucci, G.; Reati, R.; Arena, I.; Bezzio, C.; Devani, M.; Corte, C.D.; Morganti, D.; Mandelli, E.D.; Omazzi, B.; Redaelli, D.; et al. Efficacy of a novel self-assembling peptide hemostatic gel as rescue therapy for refractory acute gastrointestinal bleeding. Endoscopy 2020, 52, 773–779. [Google Scholar] [CrossRef] [PubMed]
- Gralnek, I.M.; Stanley, A.J.; Morris, A.J.; Camus, M.; Lau, J.; Lanas, A.; Laursen, S.B.; Radaelli, F.; Papanikolaou, I.S.; Cúrdia Gonçalves, T.; et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Update 2021. Endoscopy 2021, 53, 300–332. [Google Scholar] [CrossRef] [PubMed]
- Nagata, N.; Sakurai, T.; Moriyasu, S.; Shimbo, T.; Okubo, H.; Watanabe, K.; Yokoi, C.; Yanase, M.; Akiyama, J.; Uemura, N. Impact of INR monitoring, reversal agent use, heparin bridging, and anticoagulant interruption on rebleeding and thromboembolism in acute gastrointestinal bleeding. PLoS ONE 2017, 12, e0183423. [Google Scholar] [CrossRef] [PubMed]
- Grupka, M.J.; Benson, J. Endoscopic clipping. J. Dig. Dis. 2008, 9, 72–78. [Google Scholar] [CrossRef]
- Ninomiya, S.; Shiroshita, H.; Bandoh, T.; Soma, W.; Abe, H.; Arita, T. Delayed perforation 10 days after endoscopic hemostasis using hemostatic forceps for a bleeding Dieulafoy lesion. Endoscopy 2013, 45 (Suppl. 2), E99–E100. [Google Scholar] [CrossRef]
- Subramaniam, S.; Kandiah, K.; Thayalasekaran, S.; Longcroft-Wheaton, G.; Bhandari, P. Haemostasis and prevention of bleeding related to ER: The role of a novel self-assembling peptide. United Eur. Gastroenterol. J. 2019, 7, 155–162. [Google Scholar] [CrossRef]
- Soons, E.; Turan, A.; van Geenen, E.; Siersema, P. Application of a novel self-assembling peptide to prevent hemorrhage after EMR, a feasibility and safety study. Surg. Endosc. 2021, 35, 3564–3571. [Google Scholar] [CrossRef]
- Uba, Y.; Ogura, T.; Ueno, S.; Okuda, A.; Nishioka, N.; Miyano, A.; Yamamoto, Y.; Bessho, K.; Tomita, M.; Nakamura, J.; et al. Comparison of Endoscopic Hemostasis for Endoscopic Sphincterotomy Bleeding between a Novel Self-Assembling Peptide and Conventional Technique. J. Clin. Med. 2022, 12, 79. [Google Scholar] [CrossRef]
- Subramaniam, S.; Kandiah, K.; Chedgy, F.; Fogg, C.; Thayalasekaran, S.; Alkandari, A.; Baker-Moffatt, M.; Dash, J.; Lyons-Amos, M.; Longcroft-Wheaton, G.; et al. A novel self-assembling peptide for hemostasis during endoscopic submucosal dissection: A randomized controlled trial. Endoscopy 2021, 53, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.I.; Kim, S.S.; Park, S.; Han, J.; Kim, J.K.; Han, S.W.; Choi, K.Y.; Chung, I.S.; Chung, K.W.; Sun, H.S. Endoscopic hemoclipping using a transparent cap in technically difficult cases. Endoscopy 2003, 35, 659–662. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).