Abstract
Background and Objectives: Triage systems help provide the right care at the right time for patients presenting to emergency departments (EDs). Triage systems are generally used to subdivide patients into three to five categories according to the system used, and their performance must be carefully monitored to ensure the best care for patients. Materials and Methods: We examined ED accesses in the context of 4-level (4LT) and 5-level triage systems (5LT), implemented from 1 January 2014 to 31 December 2020. This study assessed the effects of a 5LT on wait times and under-triage (UT) and over-triage (OT). We also examined how 5LT and 4LT systems reflected actual patient acuity by correlating triage codes with severity codes at discharge. Other outcomes included the impact of crowding indices and 5LT system function during the COVID-19 pandemic in the study populations. Results: We evaluated 423,257 ED presentations. Visits to the ED by more fragile and seriously ill individuals increased, with a progressive increase in crowding. The length of stay (LOS), exit block, boarding, and processing times increased, reflecting a net raise in throughput and output factors, with a consequent lengthening of wait times. The decreased UT trend was observed after implementing the 5LT system. Conversely, a slight rise in OT was reported, although this did not affect the medium-high-intensity care area. Conclusions: Introducing a 5LT improved ED performance and patient care.
1. Introduction
Modern intra-hospital triage involves selecting and evaluating patients upon their arrival to an emergency department (ED) to determine their clinical status, diagnoses, and severity ratings to prioritize treatment access. Triage aims to place patients in the right area at the right time for the most appropriate treatment and to distribute medical resources according to the needs of patients. Trained triage nurses usually assign a triage level to patients using an established triage system. These systems seek to promote safe and efficient utilization of ED resources [1,2].
Triage systems recommend a “time to treatment” in EDs and measure service quality. These systems aim to standardize, create reproducible evaluation procedures, and regulate patient access to increasingly crowded EDs. Standardization increases patient safety and ED access equity by ensuring the quality of care for the community [3,4,5,6,7,8].
In EDs organized by areas of care intensity, patients are prioritized and channeled toward low- or medium-high-intensity care areas at triage [9,10]. Worldwide, triage models are distinguished mainly by the number of priority codes. A 3-level triage system (3LT) defines three priority codes for medical examination; there are also 4-level (4LT) and 5-level (5LT) triage systems [8,11,12].
In the 1980s, the number of 3- and 4LTs increased [8,11,12,13,14]. Gerald Fitzgerald introduced Australia’s first 5LT in 1986 [15]. This system, originally called the National Triage Scale, became the Australian Triage Scale (ATS) in 2000. The ATS demonstrated a superior correlation with patients’ acuity and adequate inter- and intra-observer reproducibility [3,13,16,17,18,19,20,21,22]. Three other 5LT systems followed in the 1990s: the Manchester Triage Scale (MTS), Canadian Triage and Acuity Scale (CTAS), and Emergency Severity Index (ESI) [23,24].
5LTs are considered a “gold standard” for their greater validity and reliability compared to 3LT or 4LT systems. Reliability, i.e., the degree of agreement on code assignment, has been demonstrated both inter and intra-observer: inter-rater agreement and intra-rater agreement. Validity, the ability to correlate with the true acuity of the patient, requires indirect indicators: such as correlation with the need for hospitalization, hospitalization in an intensive environment, the study of over- and under-triage, mortality [3,7,8,12,16,17,18,19,20,23,24,25]. The implementation of 5LT shows a clear correlation between the categories and indirect indices such as time to treatment, resource usage, intra-hospital mortality, hospitalization index, transfer frequency, and time spent in intensive care [3,8,11,12,16,17,18,19,20]. Triage systems also improve estimates of resource usage, hospital costs, the likelihood of hospitalization, and the risk of short-term mortality [17,18,26,27,28,29,30,31,32,33,34,35,36].
With 56.9% of hospitals responding, the most commonly used triage system in the USA is the 5LT ESI, followed by 3LT systems (25.2%) [37]. Unpublished 2021 data from SIMEU (Italian Scientific Society of Emergency Medicine) show that, in Italy, 40% of EDs use 5LT, 57% use 4LT, and 3% use 3LT systems [38]. 3LT and 4LT systems should be upgraded where possible.
In 2012, professionals and scientific societies gathered at the National Triage Coordination Conference and proposed a coding system with five priority codes. After a review of the literature on triage, in 2015, our research group began using a 5LT system that considers each patient’s symptoms, vital signs, and necessary treatment resources, as with other 5LTs [11,13,15,39].
Progressive increases in ED crowding are negatively linked to patient outcomes and satisfaction. However, crowding effects on triage wait times and the frequency of under- (UT) and over-triage (OT) are unclear and under-investigated. In addition, few studies have examined outcomes associated with 5LT systems and ED management in real-life settings [40,41,42].
In this special issue, we focus on ED management, re-engineering the triage system, and the influence of crowding in triage.
2. Methods
2.1. Study Design
This observational study was based on a retrospective review of the epidemiologic and clinical records of patients who visited the Foundation IRCCS Policlinic San Matteo from 1 January 2014 to 31 December 2020. We analyzed all ED visits that occurred during the 4LT period, from the inauguration of the new ED arranged by care intensity (from 1 January 2014 to 30 November 2015). These were compared to ED visits that occurred during the 5LT period (from 30 November 2015 to 31 December 2020).
Before 1 January 2014, our ED had a smaller layout, fewer resources, and no divisions by care intensity. We, therefore, do not believe that comparisons can be made with the period before 1 January 2014.
The data were extracted using PiEsse software, used to manage patients in our ED. Upon presentation, blood tests, imaging, and consultations are required; based on the results of these examinations, patients are hospitalized or discharged. We estimated changes in UT, OT, and crowding indices. The San Matteo Hospital Foundation provided data on all ED services. An ad hoc query was performed to obtain the data of interest. The patients’ names were anonymized to ensure confidentiality. All patients consented to have their data used for medical and research purposes and health data processing upon arrival to the ED, as required by the local ethics committee.
2.2. Endpoints
This analysis was carried out on the total ED accesses during two periods: 4LT and 5LT. We sought to determine the effects of introducing a 5LT on wait times. The secondary aim was to evaluate the impact of introducing a 5LT on validity, measured as UT, and OT. We also sought to determine if the 5LT system codes were better correlated (in comparison to 4LT system codes) to patients’ actual acuity; we verified this outcome by measuring the correlation between the triage code and severity code at discharge.
Other outcomes included the impact of triage on crowding indices such as the length of ED stay, total access block time, and rate of access block. Finally, we analyzed the functioning of the 5LT during the COVID-19 pandemic.
2.3. Inclusion and Exclusion Criteria
All non-pediatric patients (>14 years old) who visited the ED during the study periods were eligible for inclusion.
2.4. Study Population
Demographic data (sex and age), vital parameters (blood pressure, heart rate, oxygen saturation, Glasgow Coma Scale score, respiratory rate), signs and symptoms, waiting time, length of stay (LOS) in the ED, mode of ED access, priority codes for medical examination, exit codes for severity, total access block time, and rate of access block were collected for each patient. All medical records, including computed tomography data, were thoroughly reviewed. All collected data were entered into Microsoft Excel and used for statistical analysis.
The 5LT group consisted of 307,198 patients who accessed the ED between 30 November 2015 and 31 December 2020. The 4LT group consisted of 116,060 patients who accessed the ED during the control period between 1 January 2014 (inauguration of the new ED organized into areas of the care intensity) and 30 November 2015.
2.5. The Organizational Experience of Our ED
Since 2010, triage in our ED has been carried out with guided grids to determine triage codes (guided code attribution algorithms). These grids provide a calculated code but allow the operator to indicate the most appropriate code based on the overall patient assessment. These internal protocols were revised in 2015, according to Ministerial Recommendation No. 15, to adapt the triage activity to a new ED structure (organized by care intensity) and to implement a 5LT system. In 2019, at the same time the ED director retired, various internal reorganizations occurred. These included a shift from 7 to 12 h for doctors and nurses and the dissolution of the intensive short observation (OBI) team. Our region’s healthcare system is organized as a “hub-and-spoke” model. The terms “hub” and “spoke” are borrowed from the airline industry, where the “hub” represents the airport where most flights are concentrated. In medicine, the hub-and-spoke model assumes that, for certain complex pathologies, specialist practitioners and expensive equipment are needed. These resources cannot be guaranteed at every location. Consequently, more-complex patients are routed to regional or macro-area Centers of Excellence (“hubs”) for treatment. Peripheral medical centers (“spokes”) provide fewer and less-specialized services; therefore, less-complex patients are routed to these facilities. The hub-and-spoke model improves healthcare service provision [43].
Care Areas of the ED
Since December 2013, our ED has been divided into low- and medium-high-intensity areas. In addition to examination and shock rooms, the medium-intensity care area also includes an observation unit that functions as a holding area. The medium-high-intensity care area consists of a resuscitation area for triage code 1 (4 beds) and a level 2 critical monitoring area (6 beds). There is also a trauma area for more stable patients with fractures [9,10].
Incoming patients are first triaged by specialized nurses with basic and advanced triage education training. First, the nurses gather information about the main symptom(s) that led the patient to the ED, including a brief medical history. Second, they collect vital parameters and perform a visual inspection. Patients are then assigned a priority code for medical examination and are redirected toward a specific care intensity area. The triage process is based on written protocols (“triage grids” drawn up mainly based on the evolution of the main symptom) as well as the patient’s medical history and vital parameters.
Patients assigned to the medium-high-intensity area should demonstrate impairment of a vital parameter, an altered state of consciousness, be at increased evolutionary risk of any symptoms (e.g., typical chest pain), need specialized care (such as non-invasive ventilation), or multi-parameter monitoring. Once in the ED, the doctor establishes the patient’s diagnostic and therapeutic pathways. The two areas of the care intensity flow to a stabilization area for OBI (Figure 1).
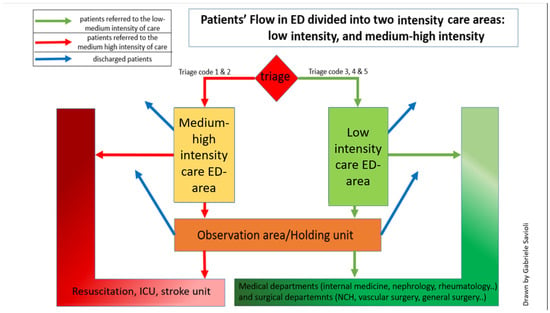
Figure 1.
Our ED is divided into two areas according to care intensity. A medium-high-intensity area (shown on the right in the figure) includes a shock room for cases to be isolated and medium-high-intensity beds. Patients at high developmental risk and requiring high care intensity (codes 1 and 2) are routed here. In a second area, patients with low-intensity care are managed, and some patients with medium-intensity care (codes 3, 4, and 5) can be managed. The two areas are physically separated while remaining connected through two corridors so that low- and high-intensity patient flows do not cross. Patients can be sent to the observation unit—where patients are stabilized, monitored, and observed—from both areas. Our observation unit also functions as a holding unit from the observation unit; patients can be hospitalized, transferred to other hospitals, or discharged. Admission and discharge are directly possible from both areas.
2.6. The Two Triage Systems Are 4LT and 5LT Grids
The priority codes for medical examination in our ED are shown in the graph below. A triage code (the new Code 3) was introduced for patients requiring faster medical examination or therapy than other patients in the low-intensity care area. The secondary reason for the new Code 3 was to relieve patients who would have previously been assigned a Code 2 (area of medium intensity) because they needed urgent medical examination but did not require a medium-high-intensity care area (Figure 2).
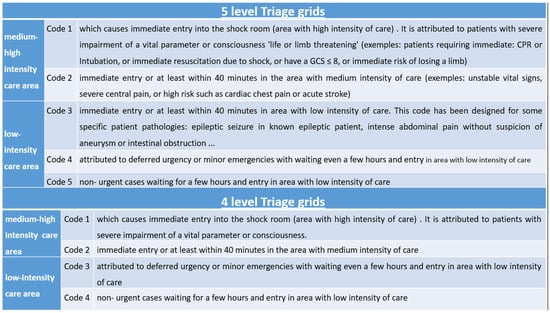
Figure 2.
4LT and 5LT grids.
In transitioning from a 4LT to a 5LT system, the triage codes for the medium-high care intensity remained unchanged: Code 1 indicates life-threatening conditions, and Code 2 indicates very urgent conditions. In the 5LT system, patients with Codes 3, 4, or 5 are allocated to the low-intensity care area. Previously, in the 4LT system, there were only two levels of triage code (Codes 3 and 4). Thus, an extra triage code was created for patients destined for the low-intensity area. Patients previously assigned to the triage code 2, who urgently needed to be seen by the doctor (high visit priority) but could otherwise be treated in a low-intensity care area, were assigned to this additional level of triage (e.g., pain due to renal colic).
2.7. UT and OT Definitions
The UT rate is defined as the proportion of patients who have a lower-than-appropriate triage code, are not attended to in time, or are not assigned to an adequate intensive care area. UT poses a serious risk and is associated with increased mortality and adverse outcomes. Calculation of UT using a two-entry contingency table corresponds to a false negative rate. These patients experienced low triage activation (assigned a triage code lower than necessary, assignment to an intensive care area lower than necessary, with reduced resource allocation) relative to all patients with that condition.
The OT rate is defined as the proportion of unnecessarily applied hospital resources to patients without a particular condition (resource overuse). Therefore, the calculation of OT using a two-entry contingency table corresponds to False Discovery Rate (FDR) = 1 − Positive Predictive Value. That is, it represents the ratio between those who had a high triage activation (assigned a triage code higher than necessary, assignment to an intensive care area higher than necessary; with an increased resource overuse) but did not have acute pathology compared to all those who had a high triage activation (both those with and without acute pathology). Figure 3 describes how the UT and OT are calculated.
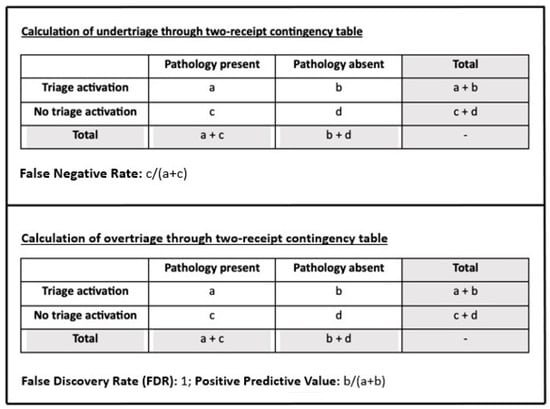
Figure 3.
Calculation of UT and OT.
2.8. Measurement of Crowding
Several widely validated indices for measuring crowding have been proposed [44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67]. The most used indices are:
Input crowding indices: wait times, number of patients visiting the ED, disease severity and complexity (e.g., number of patients at each acuity level), and number of people who left without being seen (LWBS).
Throughput Crowding Indices: LOS
Output crowding indices: mean number or percentage of admissions, patients in the ED (number or percentage), access block and boarding (mean number or percentage of patients who have experienced it), and access block or boarding times (such as the total access block time).
“Wait time” was defined as the total time from initial registration or triage to the time the patient was first seen by a doctor. The overall ED-LOS was the time from arrival at triage or registration until discharge or hospital transfer. LOS reflected the total patient experience, including care and waiting. Access block was defined as >8 h in the ED from presentation to admission [68]. Total access block time thus represented access block duration [69].
Boarding was the time that elapsed between the medical decision to admit the patient to the hospital and the patient’s arrival at the hospital bed; a boarding time in the ED of 6 h is considered high [70,71,72]. Thus, boarding time represented the duration of boarding [64,66,73,74].
We used indices that concerned both inputs and throughputs and output factors to account for the complexity of the crowding phenomenon. Among these we have chosen waiting time; ED-LOS; boarding and access block time.
2.9. Statistics
Continuous variables are described as means, medians, and interquartile ranges; qualitative variables are expressed as the number of observations and appropriate proportions. Between-group comparisons for continuous variables were made using the non-parametric Mann–Whitney test, according to their non-normal distributions. Associations between the qualitative variables were studied using the χ2 test. Statistical analyses were conducted using appropriate logistic multivariate regression models to test the association between time variables while accounting for crowding, exit block, and the different triage periods. The test of proportions was used to examine the differences in UT and OT by year of observation. In particular, for each record the presence/absence of over-triage and under-triage was modeled as a dichotomous variable, as described in the Methods section, and the risk of undergoing to either over- or under-triage was described as the odds ratio (OR) resulting from multiple regression analysis adjusted by age, gender and year of observation. This analysis has been carried out for the whole population and for subgroups in which boarding or exit block was present. The significance level was set at alpha 0.05 (statistical significance at p < 0.05), and all tests were two-tailed.
The analyzes were conducted with STATA software (version 14; Stata Corporation, College Station, TX, USA, 2015). The ethics committee submitted and approved the study (Protocol number 20200114609). The analyses were made on data from the PIESSE software (Piesse SRL, Latina, Italy).
3. Results
3.1. Overall (Table 1)
In the 5LT system period, there was a statistically significant increase in older patients (p < 0.001). During the same period, the number of patients that arrived at our ED by personal transport (so-called ambulatory arrivals) decreased significantly (39.1% vs. 20.8%, p < 0.001). Simultaneously, more patients presented by ambulance (27.6% vs. 37.2%, p < 0.001), and required specialized nursing staff (30.5% vs. 39.1%, p < 0.001) and medical assistance (2.5% vs. 2.7%, p < 0.001). A progressive increase in patients requiring higher triage codes was also reported (p < 0.001). The need for hospitalization progressively increased (32.6% vs. 55.5%; p < 0.001), transfers to spoke hospitals decreased (2.8% vs. 2.1%, p < 0.001), and the number of patients discharged decreased (64.2% vs. 42.1%, p < 0.001). Analyzing the correlation based on the care intensity in the two periods, the correlation between the triage code and the severity code at hospital discharge increased from 0.266 in 4LT to 0.319 in 5LT for the low-medium-intensity care area. For the medium-high care intensity area, the correlation improved from 0.277 in 4LT to 0.304 in 5LT.


Table 1.
(a) Principal personal and ED presentation features of patients included in the study, by period of observation. The 4LT period (T4) spanned 1 January 2014 to 30 November 2015; the 5LT period (T5) spanned 1 December 2015 to 31 December 2020. a: χ2 test. (b) Pathology at admission for the patients included in the study, by period of observation.
Table 1.
(a) Principal personal and ED presentation features of patients included in the study, by period of observation. The 4LT period (T4) spanned 1 January 2014 to 30 November 2015; the 5LT period (T5) spanned 1 December 2015 to 31 December 2020. a: χ2 test. (b) Pathology at admission for the patients included in the study, by period of observation.
| (a) | |||
| 1-1-2014/30-11-2015 | 1-12-2015/31-12-2020 | ||
| Sex | 4LT n (%) | 5LT n (%) | p a |
| Male | 59,432 (51.2) | 158,914 (51.7) | |
| Female | 56,628 (48.8) | 148,283 (48.3) | 0.002 |
| Age | |||
| <18 | 11,333 (9.8) | 27,267 (8.9) | |
| 18–29 | 15,975 (13.8) | 39,128 (12.7) | |
| 30–39 | 13,711 (11.8) | 32,049 (10.4) | |
| 40–49 | 16,376 (14.1) | 40,943 (13.3) | |
| 50–59 | 14,132 (12.2) | 41,339 (13.5) | |
| 60–69 | 12,698 (10.9) | 34,955 (11.4) | |
| 70–79 | 14,902 (12.8) | 41,001 (13.4) | |
| 80+ | 16,933 (14.6) | 50,516 (16.4) | <0.001 |
| Triage priority code | |||
| Code 5 | 13,443 (11.6) | 25,748 (8.4) | |
| Code 4 | 78,777 (67.9) | 191,981 (62.5) | |
| Code 3 | 0 (-) | 17,297 (5.6) | |
| Code 2 | 22,711 (19.6) | 67,688 (22.0) | |
| Code 1 | 1129 (0.9) | 4484 (1.5) | <0.001 |
| Priority code at discharge | |||
| Code 5 | 29,240 (25.2) | 43,141 (14.0) | |
| Code 4 | 73,995 (63.8) | 224,039 (72.9) | |
| Code 3 | 0 (-) | 425 (0.1) | |
| Code 2 | 11,952 (10.3) | 36,341 (11.8) | |
| Code 1 | 873 (0.7) | 3252 (1.2) | <0.001 |
| Care intensity | |||
| Low | 92,220 (79.5) | 235,026 (76.5) | |
| Medium-to-high | 23,840 (20.5) | 72,172 (23.5) | <0.001 |
| Outcome | |||
| Discharge | 94,701 (81.6) | 246,413 (80.2) | |
| Hospitalization | 17,347 (14.9) | 51,043 (16.6) | |
| Transfer | 2166 (1.9) | 5746 (1.9) | |
| Left without being seen | 1385 (1.2) | 2933 (0.9) | |
| Other | 461 (0.4) | 1063 (0.4) | <0.001 |
| (b) | |||
| Pathology at ED Access | n | % | |
| 4TL | |||
| Trauma | 39,713 | 34.22 | |
| Major trauma | 271 | 0.23 | |
| Minor symptoms | 25,614 | 22.07 | |
| Dyspnea | 5399 | 4.65 | |
| Thoracic pain | 5870 | 5.06 | |
| Abdominal pain | 9455 | 8.15 | |
| Headache | 4353 | 3.75 | |
| Neurologic symptoms | 1630 | 1.40 | |
| Bleeding | 2024 | 1.74 | |
| Fever/Sepsis | 1 | 0.00 | |
| Other | 28,4811 | 18.73 | |
| 5TL | |||
| Trauma | 12,233 | 5.03 | |
| Major trauma | 933 | 0.38 | |
| Minor symptoms | 35,712 | 14.70 | |
| Dyspnea | 14,117 | 5.81 | |
| Thoracic pain | 17,321 | 7.13 | |
| Abdominal pain | 26,159 | 10.76 | |
| Headache | 3494 | 1.44 | |
| Neurologic symptoms | 14,319 | 5.89 | |
| Bleeding | 5757 | 2.37 | |
| Fever/Sepsis | 8048 | 3.31 | |
| Other | 10,4924 | 43.18 | |
3.2. Wait Time (Table 2)
There was a minimal reduction in wait times for life-threatening triage codes (5 min for Code 1 patients during the 4LT system period vs. 4.3 min during the 5LT system period, p < 0.001). In contrast, wait times rose for very urgent codes (23.5 min for Code 2 patients during the 4LT system period vs. 32.5 min during the 5LT system period, p < 0.001). Comparing the twelve months prior to the introduction of the 5LT with the twelve months that followed 5LT implementation (10,636 cases in T4 and 13,608 in T5), we noted a minimal, non-significant increase of ~3 min. Considering triage code 2 data acquired over various years, we saw a slight (non-significant) yet constant increase in wait times of ~3–4 min per year, corresponding with the increase in the number of triage code 2 patients and crowding at our hospital. More precisely, the year our facility switched from 4LT to 5LT, there was a greater increase in just less than 4 min. This increase continued during the 4LT (just under 4 min from the year 2014–2015) and 5LT (just under 2 min from 2016 to 2017; about 5 min from 2017 to 2018) periods. The wait time increased significantly in 2019.
The wait times for Code 3 in the 5LT system period were similar to those of Code 2 in the 4LT system period (24.3 min for Code 3 during the 5LT system period vs. 23.5 min for Code 2 patients during the 4LT system period). The wait times for Codes 4 and 5 during the 5LT system period were comparable to those of Codes 3 and 4 during the 4LT system period (52.1 min for Code 3 patients during the 4LT system period vs. 57.5 min for Code 4 patients during the 5LT system period and 52.2 min, for Code 4 patients during the 4LT system period vs. 48.4 min for Code 5 patients during the 5LT system period).


Table 2.
(a1) Selected time variables accounting for crowding, by period. * The 4LT period (T4) spanned 1 January 2014 to 30 November 2015; the 5LT period (T5) spanned 1 December 2015 to 31 December 2020; a: Kruskal–Wallis test. (a2) Wait time, by period and code at presentation. * The 4LT period (T4) spanned 1 January 2014 to 30 November 2015; the 5LT period (T5) spanned 1 December 2015 to 31 December 2020. a: Kruskal–Wallis test. (b) Selected time variables accounting for crowding, by presence of boarding and exit block. a: Kruskal–Wallis test. (c) Wait time (Mean; minutes) for triage code 2 the 12 months before, and the 12 months immediately following, the introduction of the 5LT system. * Kruskal–Wallis test. (d) Wait time (Mean; minutes) for triage code 2 during the seven years of the study. The 4LT period (T4) spanned 1 January 2014 to 30 November 2015; the 5LT period (T5) spanned 1 December 2015 to 31 December 2020.
Table 2.
(a1) Selected time variables accounting for crowding, by period. * The 4LT period (T4) spanned 1 January 2014 to 30 November 2015; the 5LT period (T5) spanned 1 December 2015 to 31 December 2020; a: Kruskal–Wallis test. (a2) Wait time, by period and code at presentation. * The 4LT period (T4) spanned 1 January 2014 to 30 November 2015; the 5LT period (T5) spanned 1 December 2015 to 31 December 2020. a: Kruskal–Wallis test. (b) Selected time variables accounting for crowding, by presence of boarding and exit block. a: Kruskal–Wallis test. (c) Wait time (Mean; minutes) for triage code 2 the 12 months before, and the 12 months immediately following, the introduction of the 5LT system. * Kruskal–Wallis test. (d) Wait time (Mean; minutes) for triage code 2 during the seven years of the study. The 4LT period (T4) spanned 1 January 2014 to 30 November 2015; the 5LT period (T5) spanned 1 December 2015 to 31 December 2020.
| (a1) | |||||||
| Period * | Observations | Median (min) | pa | Interquartile Range (min) | |||
| Wait time | |||||||
| T4 | 116,060 | 43.3 | 16.7–96.1 | ||||
| T5 | 307,198 | 45.5 | <0.001 | 17.7–104.5 | |||
| Process time | |||||||
| T4 | 116,060 | 105.7 | 52.1–194.1 | ||||
| T5 | 307,198 | 118.4 | <0.001 | 57.5–232.2 | |||
| Length of stay (LOS) | |||||||
| T4 | 116,060 | 174.2 | 99.0–290.8 | ||||
| T5 | 307,198 | 195.8 | <0.001 | 108.2–338.1 | |||
| (a2) | |||||||
| Period * | Observations | Median (min) | Interquartile Range (min) | pa | |||
| Wait time | |||||||
| Code 5 | |||||||
| T4 | 13,443 | 52.2 | 18.2–109.1 | ||||
| T5 | 25,748 | 48.4 | 17.5–104.3 | <0.001 | |||
| Code 4 | |||||||
| T4 | 78,777 | 52.1 | 20.7–108.9 | ||||
| T5 | 191,981 | 57.5 | 22.3–122.9 | <0.001 | |||
| Code 3 | |||||||
| T5 | 17,297 | 24.3 | 12.9–44.9 | - | |||
| Code 2 | |||||||
| T4 | 22,711 | 23.5 | 11.4–49.1 | ||||
| T5 | 67,688 | 32.5 | 14.2–73.8 | <0.001 | |||
| Code1 | |||||||
| T4 | 1129 | 5.0 | 2.6–9.8 | ||||
| T5 | 4484 | 4.3 | 2.2–8.5 | <0.001 | |||
| (b) | |||||||
| Observations | Median (min) | Interquartile Range (min) | pa | ||||
| Wait time | Low-intensity care | ||||||
| No boarding | 28,731 | 52.7 | 21.5–114.7 | ||||
| Boarding | 7416 | 62.4 | 24.8–141.1 | <0.001 | |||
| Medium-to-high care intensity | |||||||
| No boarding | 35,225 | 18.7 | 8.0–44.3 | ||||
| Boarding | 4930 | 23.1 | 9.9–54.6 | <0.001 | |||
| Low-intensity care | |||||||
| No exit block | 29,005 | 48.6 | 20.3–105.4 | ||||
| Exit block | 7142 | 94.3 | 34.3–186.5 | <0.001 | |||
| Medium-to-high care intensity | |||||||
| No exit block | 35,907 | 18.4 | 8.0–43.1 | ||||
| Exit block | 4248 | 28.2 | 11.5–71.2 | <0.001 | |||
| (c) | |||||||
| N | Wait Time (Median; min) | Interquartile Range | p* | ||||
| 4LT | 10,636 | 25.3 | 12.3–52.9 | ||||
| 5LT | 13,608 | 28.1 | 13.2–58.2 | 0.001 | |||
| (d) | |||||||
| Year | N | Mean | Median | Interquartile Range | |||
| 2014 | T4 | 12,075 | 36.2 | 22.0 | 10.7–46.4 | ||
| T5 | - | - | - | - | |||
| 2015 | T4 | 10,636 | 40.0 | 25.3 | 12.3–52.9 | ||
| T5 | 1011 | 43.8 | 28.9 | 14.5–60.9 | |||
| 2016 | T4 | - | - | - | - | ||
| T5 | 12,597 | 43.7 | 28.0 | 13.1–58.0 | |||
| 2017 | T4 | - | - | - | |||
| T5 | 13,263 | 45.5 | 28.3 | 12.8–60.6 | |||
| 2018 | T4 | - | - | - | - | ||
| T5 | 14,576 | 52.7 | 33.5 | 14.5–72.9 | |||
| 2019 | T4 | - | - | - | - | ||
| T5 | 14,525 | 70.9 | 43.6 | 17.2–103.5 | |||
| 2020 | T4 | - | - | - | - | ||
| T5 | 11,716 | 58.5 | 32.7 | 13.8–80.1 | |||
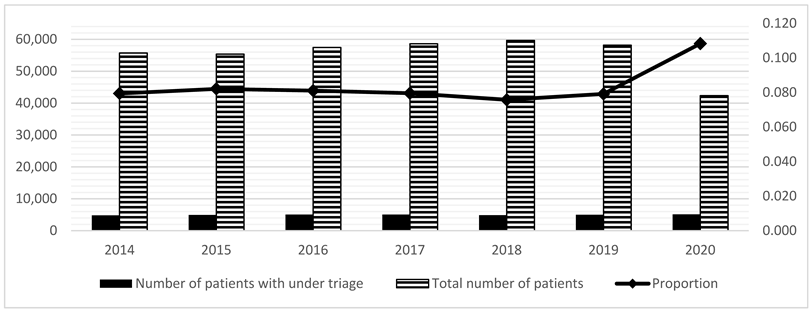
3.3. UT and OT
The risk of UT tended to decrease in the 5LT compared to the 4LT system period (Table 3; OR = 0.87, p < 0.001). Table 3 shows trends relative to care intensity areas. The three conditions most represented by this phenomenon (UT in medium-high-intensity) were chest pain (23.5%), dyspnea (22.6%), and neurological disorders (20.1%). The most frequent causes of these three symptoms were non-ST-elevation myocardial infarction (STEMI), acute heart failure, pneumonia, and stroke. The trend of the phenomenon (UT in medium-high-intensity) seems to have fluctuated over the years (2014, n = 135, 1.12%; 2015, n = 175, 1.50%; 2016, n = 248, 1.97%; 2017, n = 212, 1.60%; 2018, n = 181, 1.24%; 2019, n = 188, 1.29%; 2020, n = 210, 1.79%). UT has decreased since 2016, reaching a nadir in 2018 and gradually increasing again in 2019 and 2020 (Table 4).

Table 3.
Risk of UT and OT by period.

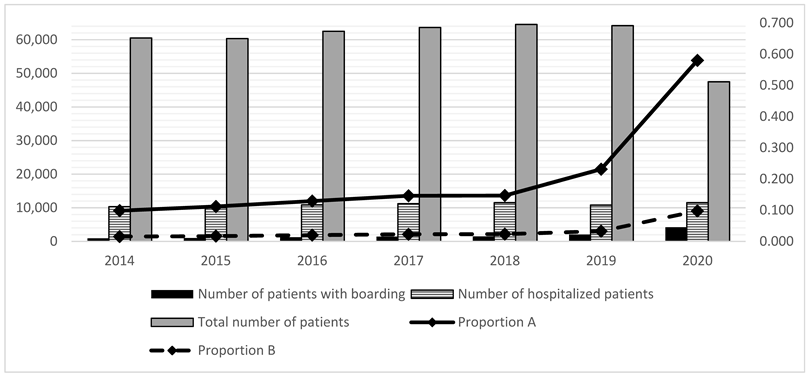
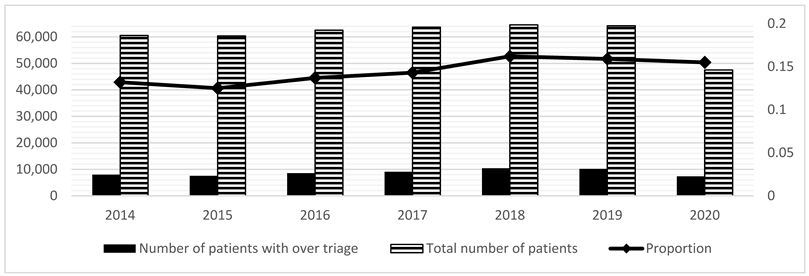
Table 4.
(a) # Proportion of boarding and exit block (calculated only on hospitalized patients) from 2014 to 2020; (b) Table + Figure. Evolution of boarding from 2014 to 2020; (c) Table + Figure. Evolution of Over Triage (OT) from 2014 to 2020; (d) Table + Figure. Evolution of Under Triage (UT) from 2014 to 2020.
3.4. Crowding
Boarding and exit blocks observed from 2014 to 2020 indicated that crowding had progressively increased (Table 4). The number of ED visits rose gradually until 2018, except for a slight deflection in 2015, and then decreased in 2019 and 2020 (Table 4). Boarding and exit blocks indicated longer wait times for low and medium-high-intensity care areas (Table 2; p < 0.001). We have chosen the crowding indices that are most reproducible with an automated data extraction [13,75,76,77,78,79]. Boarding substantially reduced the risk of OT and slightly decreased the risk of UT in both care intensity areas, as shown in Table 5a. Exit block substantially reduced the risk of OT and slightly reduced the risk of UT, as shown in Table 5b.

Table 5.
(a) Risk of UT and OT, by presence of boarding. (b) Risk of UT and OT, by presence of exit block.
3.5. LT of COVID Patients
Our ED encountered 3826 patients with COVID-19. Of these, 125 received a triage code 5, 2789 received a triage code 4, 169 received a triage code 3, 810 received a triage code 2, and 86 received a triage code 1. Of all of these, there were 159 positives for COVID-19 at a PCR test, and 78 positives died in the ED. The main wait times in this area were, respectively, 48 min for Code 5, 47 min for Code 4; 48 min for Code 3; 27 min for Code 2, and 10 min for Code 1.
4. Discussion
4.1. Overall
This study analyzed the validity of a 5LT over a 4LT. To our best knowledge, this is the first published Italian study, the largest European study, and the first study conducted on an ED organized by care intensity area [80]. Although some real-life 5T studies have been performed, most of these have been performed on a single symptom or disease, often on a small number of patients. Some of these were wait time studies, and others were real-life 5LT validation studies [81,82,83,84,85].
Our work analyzes the function of triage by capturing the complexity of real life and studies the functionality and impact on waiting times over a long period for all causes of access. It is the first Italian study that compares the validity of 4LT and 5LT through the calculation of UT and OT on a large population sample.
Triage validity is the ability of the triage system to correlate with the patient’s acuity; since the real acuity of the patient is impossible to detect, surrogate indices are used such as the following: UT and OT, correlation with hospitalizations, mortality and hospitalization in resuscitation [86,87].
This is, to our knowledge, the first study that analyzes the mutual influences between triage and crowding by studying all the determinants of crowding, and in particular its main determinants: boarding and exit blocks.
Patients who present to the ED have become more numerous, frail, and sicker. This is underlined by the progressive rise in the patients’ ages, the decrease in spontaneous accesses, the higher number of accesses through the territorial emergency service or on a stretcher, and the number of higher triage and severity codes at discharge. This phenomenon has been reported in the literature for several years [44,45,46,47,49,50,51,52,53,54,55,56,64,65,73,74,75,88], which has increased since the onset of the COVID-19 pandemic and translated into higher hospitalization rates [76,77]. These factors increase exit block and boarding, which, together with the progressive reduction in available hospitalization beds, worsens crowding.
Collectively, these factors have changed the way ED physicians work, transforming their practice from “admit-to-care” to “care-to-admit” [13,76,77,78,79]. This change is reflected in a gradual extension of LOS and process times. Because of these changes, treatment and observation paths have been designed for pathologies that are also very complex or with complex management, such as, for example, severe trauma, heart failure and head trauma. [89,90,91,92,93,94,95]. Although increased crowding negatively affects patient outcomes and satisfaction, the consequences for triage—particularly on wait times and UT and OT frequency—have not yet been extensively investigated. Improvements in the correlation between the triage code and the severity code at discharge suggest that 5LT system triage codes more accurately reflect actual patient acuity compared to the 4LT system. These data, interpreted alongside data indicating a general reduction in UT, show how reducing the risk of UT directly benefits sicker patients, potentially improving their subsequent outcomes.
4.2. Waiting Time
In transitioning from a 4LT to a 5LT system, the triage codes for the medium-high care intensity remained unchanged: Code 1 for life-threatening conditions and Code 2 for very urgent conditions. In the 5LT system, patients with Codes 3, 4, or 5 were allocated to the low-intensity care area. Previously, in the 4LT system, there were only two levels of triage code (Code 3 and 4). Thus, an extra triage code was created for patients destined for the low-intensity area. Patients previously assigned triage code 2, who urgently needed to be seen by the doctor (high visit priority) but could be treated in a low-intensity care area, were assigned a Code 3 (e.g., pain due to renal colic).
The additional triage level, which characterized the implementation from the 4LT system to the 5LT system, enhanced our ability to identify patients in the low-intensity area who urgently needed to be seen by a doctor. Thus, it is expected that the benefits or the disadvantages of the 5LT introduction will be more evident in the low-intensity area.
The new Code 3 aimed to identify the most fragile or compromised patients to guarantee them the best possible path without inappropriate use of medium or high care intensity areas.
Codes 4 and 5 patients did not experience significantly increased wait times, underscoring one benefit of the 5LT system. However, though the wait times for Code 1 patients improved slightly, those for Code 2 patients lengthened. Because this could not be attributed to the transition to the 5LT system, the increased wait time for Code 2 was constant over the years before and after the shift to the 5LT system and corresponded with the increased presentation of Code 2 patients and hospital crowding. The increase that occurred in 2019 against a slight reduction in the number of Code 2 patients seems to be related to increased crowding that year during ED reorganization following a change in leadership. The 2020 drop seems related to the COVID-19 pandemic, characterized by a collapse of input factors and the exposure of throughput and output factors.
Exit block and boarding most frequently affect patients requiring admission or transfer to another health facility and are prevalent in higher care intensity ED areas. In addition to the examination and shock rooms, the medium-intensity care area also includes a holding area [9,10]. The medium-high-intensity care patient needs oxygen, non-invasive ventilation, telemetry, and continuous monitoring of vital parameters. These are, in turn, dependent on structural limits (i.e., the number of oxygen outlets, ventilators, and monitors). Increased patient assignments to this area and a simultaneous rise in the exit block result in resource saturation, with consequently higher times needed for patient processing.
Other changes in the internal departmental organization may also have contributed to increased LOS (i.e., doctor and nurse turn-over, different structure of shifts, etc.). However, they were analyzed by this study. As highlighted by Zoubir et al. [79], the association between boarding time and ED outcomes is still under investigation; Multicenter studies are needed to better clarify the various effects of boarding and exit block on adverse ED outcomes.
Additional attention should be paid to the performance of doctors and nurses working in triage. Placement of triage physicians allows for rapid disposition of low-acuity patients. Meanwhile, more-complex patients can be evaluated sooner, somewhat mitigating the effects of ED crowding. Placement of senior doctors, defined as a medical doctor who completed high specialty training in emergency medicine, with nurses in triage improves wait time, LOS, LWBS rates, and left without treatment complete rates. Furthermore, medical-nurse triage teams hold advantages for direct admission of medically complex or frail patients (e.g., elderly patients) who do not require time-dependent interventions but require hospitalization. Triage care teams can also reduce overcrowding [96,97,98].
4.3. UT and OT
The introduction of 5LT systems has reduced UT. Similar results have been shown in studies that analyzed the transition from 3- or 4LT to 5LT systems [22,80,99]. These results demonstrate that the 5LT systems are safer than 4LT systems: reducing UT similarly reduces unfavorable patient outcomes. Remarkably, this risk reduction is most evident in the low-intensity care area, which was also the most changed by introducing the 5LT system. The trend toward an increase in medium-high-intensity UT was already present during the 4LT period; however, the phenomenon clearly demonstrates an oscillatory trend. It, therefore, seems reasonable not to attribute this phenomenon to the 5LT system.
Conversely, some symptoms (chest pain, dyspnea, and acute neurological disorders) have a major role in the studied period. UT can be attributed to the rapid evolution of these symptoms, with possible serious and unpredictable impairment of the patient’s clinical evolution. Examples may be ECG changes in the examination room that could lead to the activation of the STEMI pathway, sudden deterioration to coma, or shock resulting from these symptoms.
In our ED, UT tended to decline after the introduction of the 5LT system, reaching its nadir in 2018. Subsequent increases were observed in 2019 and 2020, with an increase in exit block and boarding phenomena. Notably, in these two years, the worsening of crowding outputs and throughput factors corresponded to a reduction in the number of ED visits.
While the 2020 trend could have resulted from the COVID-19 pandemic, the 2019 trend was likely influenced by the internal reorganization of our ED following a change of leadership, as already described in 2.5.
As described for some diseases, the reduction in UT is accompanied by an increase in OT [100,101]. Although we observed a slight increase in OT, it did not affect the medium-high care intensity area. Analysis of the OT trend over the years shows three periods of reductions in conjunction with reductions in the number of ED visits. This suggests that OT might be influenced by the number of ED visits. It is possible that, when visits increase, the tacit habit of “better to over- than to under-triage” can prevail, as previously assumed by some authors [102].
4.4. Crowding Indices
The data analyzed in this study underline the progressive increases in crowding. The rise in LOS, exit block, boarding, and processing times have resulted in a net increase in throughput and output factors, with a consequent lengthening of wait times. The increase is higher with exit blocks than boarding in low-intensity areas and for less-urgent triage codes. The presence of an exit block almost doubled the wait time. Furthermore, wait times were lengthened by approximately 25–30% for patients with high-priority codes who required medical examination (triage Codes 1 or 2).
These data demonstrate the influence of output factors on ED pathways. The exit block increases processing and LOS times, with a consequent slowdown of all ED processes and flows, including wait and handling times. The situation can be likened to a funnel into which patients continuously pour and whose outflow is limited by the diameter of the neck. On one side of the funnel is the “city”, on the other (the narrow one) the hospital with “beds”. The tighter the neck, the slower patient flow, starting at triage (Figure 4).
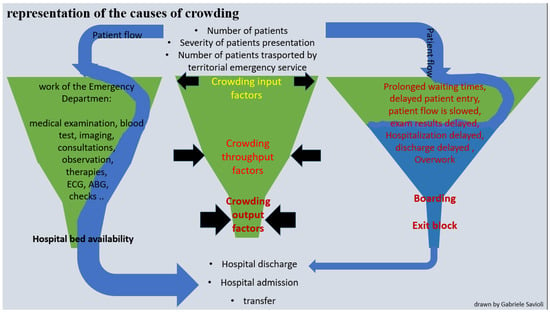
Figure 4.
Graphic representation of the causes of crowding. This figure represents crowding in EDs. The ED is represented by a funnel. The volume of patients who present to the ED is represented by the water which enters the funnel (blue arrow). The input factors (number of incoming patients, number of serious incoming codes, number of patients arriving by ambulance) are a large part of the funnel input. The throughput factors (blood tests, imaging, instrumental tests, consultations, checks, number of staff on medical and nursing shifts, tight shifts) comprise the body of the funnel. The output factors (exit block, boarding) are represented by the neck of the funnel. In a normal situation (left column), the flow of patients (blue arrow) enters the ED (the funnel) and leaves after normal processing (medical examination performed, any blood, any imaging, any consultations). The times, imaginatively represented by the time required for water to flow through the funnel, are normal in this situation. The central column represents crowding or increases in input factors, as in the case of hyper-influx or simultaneous arrival of medically complex or critically ill patients (situation represented by an enlarged funnel base), or due to internal factors, such as presentation of medically complex patients who require prolonged stabilization or numerous medical procedures (as represented by an enlarged funnel body) or for the worsening of the outgoing factors, as is necessary in the case of exit block (situation represented in this case by a restricted funnel neck). The resulting situation (right column) sees a global and marked slowdown in patient flow (blue arrow) and prolongation of time points (waiting, process, LOS). Normally, the outgoing flow is wider. In cases of crowding, it is markedly slowed, as represented by a thinner blue arrow at the exit.
With the low-intensity care and lower priority triage codes, both boarding and exit blocks substantially reduce the risk of OT and slightly reduce the risk of UT. Moreover, in both cases, triage is more accurate for patients with lower triage priorities. This may be due to increased attention from triage nurses in cases of crowding. However, the greater accuracy may also depend on the long wait times when patients are re-evaluated more easily and frequently.
In patients with life-threatening or urgent conditions (triage Codes 1 and 2), UT is reduced in boarding and, more significantly, in cases of exit block. In contrast, while OT in these patients is essentially unchanged with boarding, it increases in the event of an exit block. There is also an increased risk of OT when there are more ED visits. This phenomenon could be due to greater attention being paid by the triage nurses in cases of crowding, reflecting improved accuracy during boarding and exit block.
When facing overcrowding, attention tends to focus on reducing UT, which is even more reduced than in boarding alone (this time at the expense of increased OT).
Perhaps the worst accuracy, determined only by an increase in OT, might be because patients with Codes 1 and 2 also have longer wait times than usual; however, these wait times were not long enough to allow easier and more frequent re-evaluations. Therefore, it would seem that in the event of a large increase in crowding, overestimation is preferred to avoid UT. The response of “better to over- than to under-triage” could contribute to this effect. This phenomenon would be more valid during urgent visits and with patients requiring medium-high-intensity care.
Finally, it should be noted that the COVID-19 epidemic began in 2020. As shown in Table 4, crowding doubled in 2020, straining the system. This highlighted crowding effects on triage. Thus, 5LT confirmed the abovementioned advantages in the context of a pandemic.
4.5. The 5-Level Triage in COVID Patients
The present study includes the first year of the COVID outbreak. Our center has been involved since the dawn of the epidemic being one of the HUB centers for COVID in north Italy and having treated patient zero. During the COVID-19 pandemic, the ED underwent a profound reorganization to mitigate the risk of contagion and streamline access for patients based on need. During the first pandemic phase of 2020, an area was created in the Infectious Diseases building for positive COVID patients. Those who required hospitalization were referred to specialty inpatient wards for positive patients. When the pressure of the pandemic decreased, this need was maintained, and a similar area was created inside the general ED. Parallel to this, we began prohibiting visitors and companions (except for special circumstances) to reduce the risk of virus transmission. Entrance point screening with a SARS-CoV-2 nasal swab and rapid (within 6 h) results reporting was critically important for identifying positive patients.
Patients arriving with the territorial emergency service or independently, and presenting fever, respiratory symptoms or COVID-like symptoms were referred to COVID triage. With this process, 3826 patients were then referred to the “COVID flow” in the year 2020 and were then subjected to COVID triage. All patients already identified positive at other centers and transferred only for treatment directly to dedicated COVID wards are therefore excluded from our database. Waiting times in the dedicated COVID area were in-line with general times.
Patients were treated and stabilized, and before being sent to the wards or being discharged, they had to wait for the result of a molecular PCR test. Those who were positive were referred to hospital wards dedicated to COVID patients. Patients with a negative test and with low clinical suspicion with an alternative diagnosis were referred to COVID-free wards. Patients with negative tests whose reports instead leaned toward a COVID infection were transferred to a gray area where they would repeat the tests.
Of these molecular tests performed in ED, only 159 were positive. The mortality of these patients remained high, while the management times were comparable to patients in the other areas.
4.6. Strengths and Limitations of the Study
The large size of our study cohort is certainly a strength of this study. However, this study was also limited by its retrospective design. We believe that simulated results are important; however, even well-designed studies will depart from “real-life” data obtained over a vast period. This study allowed us to analyze real-world processes in a “real” medically complex clinical cohort. Our conclusions are limited because of the study’s observational nature, including retrospective retrieval of information. Another limitation is that the study is monocentric one.
5. Conclusions
(i) The introduction of the 5LT has proved beneficial for the management of waiting times compared to the 4LT.
(ii) The introduction of a 5LT reduced UT, with a contextual increase in OT. These trends were directly proportional to the number of ED visits and increased crowding due to the worsening of output factors (such as access block) and the increase in input factors (such as the number of ED visits). Future research is needed to find models to reduce the increase in OT while trying not to lose the benefit of UT.
(iii) Crowding indices, such as boarding and access block, are related to increased wait times. The increase in boarding and access block over the years in fact corresponds to an increase in waiting times. Future research must be oriented toward finding and verifying response models that, by measuring the output factors in real time, can activate adequate triage responses aimed at limiting this worsening. This response must take into account that in the event of an increase in crowding, a reduction in the UT and a possible increase in the OT is expected.
(iv) The increase in crowding indices during the COVID pandemic underlines how this situation requires specific answers, on the design and feasibility of which future research will have to focus.
Triage remains an open challenge for the emergency physician even with 5LT introduction. Implementing AI triage algorithms in nursing routine could overcome age-specific issues. These data suggest that all Italian EDs should consider transitioning to the 5LT model.
Author Contributions
Conceptualization, G.S., M.A.B. and I.F.C.; methodology, M.A.B., G.S. and I.F.C.; software, A.V. (Angelica Varesi) and V.N.; validation, A.M., S.C., G.R. and C.E.; formal analysis, E.O.; investigation, M.A.B., G.S., A.D., Y.L. and I.F.C.; resources, C.Z.; data curation, A.S.; writing—original draft preparation, G.S., A.P. and F.P.; writing—review and editing, M.A.B., G.S., C.Z., G.B.P., I.F.C. and A.B.; visualization, E.O. and A.V. (Antonio Voza); supervision, C.Z. and G.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The studies involving human participants were reviewed and approved by the San Matteo Hospital IRCCS Ethics Committee on 17 august 2015 (Protocol number 20200114609). According to national legislation and institutional requirements, this study did not require informed consent for participation.
Informed Consent Statement
No potentially identifiable human images or data are presented in this study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study, in the collection, analyses, or interpretation of data, in the writing of the manuscript, or in the decision to publish the results.
References
- Iserson, K.V.; Moskop, J.C. Triage in medicine, part I: Concept, history, and types. Ann. Emerg. Med. 2007, 49, 275–281. [Google Scholar] [CrossRef]
- Hamamoto, J.; Yamase, H.; Yamase, Y. Impacts of the introduction of a triage system in Japan: A time series study. Int. Emerg. Nurs. 2014, 22, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Influence of Task Properties and Subjectivity on Consistency of Triage: A Simulation Study-Gerdtz-2007-Journal of Advanced Nursing-Wiley Online Library. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2648.2007.04192.x (accessed on 25 January 2023).
- Göransson, K.; Ehrenberg, A.; Marklund, B.; Ehnfors, M. Accuracy and concordance of nurses in emergency department triage. Scand. J. Caring Sci. 2005, 19, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Determinates of Throughput Times in the Emergency Department-La Vonne, A. Downey, Leslie S. Zun. 2007. Available online: https://journals.sagepub.com/doi/abs/10.1177/097206340700900103 (accessed on 25 January 2023).
- Farrohknia, N.; Castrén, M.; Ehrenberg, A.; Lind, L.; Oredsson, S.; Jonsson, H.; Asplund, K.; Göransson, K.E. Emergency Department Triage Scales and Their Components: A Systematic Review of the Scientific Evidence. Scand. J. Trauma Resusc. Emerg. Med. 2011, 19, 42. [Google Scholar] [CrossRef] [PubMed]
- Considine, J.; Shaban, R.Z.; Fitzgerald, G.J.; Thomas, S.; Graham, C.A. Triage and ATS: Collateral damage in the quest to improve ED performance. Australas. Emerg. Nurs. J. 2012, 15, 185–187. [Google Scholar] [CrossRef] [PubMed]
- Hodge, A.; Hugman, A.; Varndell, W.; Howes, K. A review of the quality assurance processes for the Australasian Triage Scale (ATS) and implications for future practice. Australas. Emerg. Nurs. J. 2013, 16, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Savioli, G.; Ceresa, I.F.; Maggioni, P.; Lava, M.; Ricevuti, G.; Manzoni, F.; Oddone, E.; Bressan, M.A. Impact of ED Organization with a Holding Area and a Dedicated Team on the Adherence to International Guidelines for Patients with Acute Pulmonary Embolism: Experience of an Emergency Department Organized in Areas of Intensity of Care. Medicines 2020, 7, 60. [Google Scholar] [CrossRef]
- Savioli, G.; Ceresa, I.F.; Manzoni, F.; Ricevuti, G.; Bressan, M.A.; Oddone, E. Role of a Brief Intensive Observation Area with a Dedicated Team of Doctors in the Management of Acute Heart Failure Patients: A Retrospective Observational Study. Medicina 2020, 56, 251. [Google Scholar] [CrossRef]
- (PDF) Reliability of Canadian Emergency Department Triage and Acuity Scale (CTAS) in Saudi Arabia. Available online: https://www.researchgate.net/publication/280867779_Reliability_of_Canadian_Emergency_Department_Triage_and_Acuity_Scale_CTAS_in_Saudi_Arabia (accessed on 25 January 2023).
- Considine, J.; Lucas, E.; Payne, R.; Kropman, M.; Stergiou, H.E.; Chiu, H. Analysis of three advanced practice roles in emergency nursing. Australas. Emerg. Nurs. J. 2012, 15, 219–228. [Google Scholar] [CrossRef]
- Lauque, D.; Khalemsky, A.; Boudi, Z.; Östlundh, L.; Xu, C.; Alsabri, M.; Onyeji, C.; Cellini, J.; Intas, G.; Soni, K.D.; et al. Length-of-Stay in the Emergency Department and In-Hospital Mortality: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 12, 32. [Google Scholar] [CrossRef]
- Early Interventions in Severe Sepsis and Septic Shock: A Review of the Evidence One Decade Later-PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/22447123/ (accessed on 25 January 2023).
- FitzGerald, G.; Jelinek, G.A.; Scott, D.; Gerdtz, M.F. Emergency department triage revisited. Emerg. Med. J. 2010, 27, 86–92. [Google Scholar] [CrossRef]
- The Manchester Triage System Provides Good Reliability in an Australian Emergency Department-PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/19546267/ (accessed on 25 January 2023).
- Zanza, C.; Facelli, V.; Romenskaya, T.; Bottinelli, M.; Caputo, G.; Piccioni, A.; Franceschi, F.; Saviano, A.; Ojetti, V.; Savioli, G.; et al. Lactic Acidosis Related to Pharmacotherapy and Human Diseases. Pharmaceuticals 2022, 15, 1496. [Google Scholar] [CrossRef]
- Tanabe, P.; Gimbel, R.; Yarnold, P.R.; Adams, J.G. The Emergency Severity Index (version 3) 5-level triage system scores predict ED resource consumption. J. Emerg. Nurs. 2004, 30, 22–29. [Google Scholar] [CrossRef]
- Evaluation of the Emergency Severity Index (Version 3) Triage Algorithm in Pediatric Patients-PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/15741584/ (accessed on 25 January 2023).
- Refining Emergency Severity Index Triage Criteria-PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/15930399/ (accessed on 25 January 2023).
- Göransson, K.E.; Ehrenberg, A.; Ehnfors, M. Triage in emergency departments: National survey. J. Clin. Nurs. 2005, 14, 1067–1074. [Google Scholar] [CrossRef]
- Travers, D.A.; Waller, A.E.; Bowling, J.M.; Flowers, D.; Tintinalli, J. Five-level triage system more effective than three-level in tertiary emergency department. J. Emerg. Nurs. 2002, 28, 395–400. [Google Scholar] [CrossRef]
- Mackway-Jones, K.; Marsden, J.; Windle, J. Emergency Triage: Manchester Triage Group. 2013. Available online: https://www.semanticscholar.org/paper/Emergency-triage-%3A-Manchester-Triage-Group-Mackway-Jones-Marsden/89d40382342c87def9a533ca7a8b5fec993f802d (accessed on 25 January 2023).
- Beveridge, R. CAEP issues. The Canadian Triage and Acuity Scale: A new and critical element in health care reform. Canadian Association of Emergency Physicians. J. Emerg. Med. 1998, 16, 507–511. [Google Scholar] [PubMed]
- Wuerz, R.C.; Milne, L.W.; Eitel, D.R.; Travers, D.; Gilboy, N. Reliability and validity of a new five-level triage instrument. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2000, 7, 236–242. [Google Scholar] [CrossRef]
- Gilboy, N.; Tanabe, P.; Travers, D.A. The Emergency Severity Index Version 4: Changes to ESI level 1 and pediatric fever criteria. J. Emerg. Nurs. 2005, 31, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Martins, H.M.G.; Cuña, L.M.D.C.D.; Freitas, P. Is Manchester (MTS) more than a triage system? A study of its association with mortality and admission to a large Portuguese hospital. Emerg. Med. J. 2009, 26, 183–186. [Google Scholar] [CrossRef] [PubMed]
- van der Wulp, I.; van Baar, M.E.; Schrijvers, A.J.P. Reliability and validity of the Manchester Triage System in a general emergency department patient population in the Netherlands: Results of a simulation study. Emerg. Med. J. 2008, 25, 431–434. [Google Scholar] [CrossRef]
- Taboulet, P.; Moreira, V.; Haas, L.; Porcher, R.; Braganca, A.; Fontaine, J.P.; Poncet, M.C. Triage with the French Emergency Nurses Classification in Hospital scale: Reliability and validity. Eur. J. Emerg. Med. Off. J. Eur. Soc. Emerg. Med. 2009, 16, 61–67. [Google Scholar] [CrossRef]
- Gravel, J.; Manzano, S.; Arsenault, M. Validity of the Canadian Paediatric Triage and Acuity Scale in a tertiary care hospital. CJEM 2009, 11, 23–28. [Google Scholar] [CrossRef]
- Ma, W.; Gafni, A.; Goldman, R.D. Correlation of the Canadian Pediatric Emergency Triage and Acuity Scale to ED resource utilization. Am. J. Emerg. Med. 2008, 26, 893–897. [Google Scholar] [CrossRef]
- Roukema, J.; Steyerberg, E.W.; van Meurs, A.; Ruige, M.; van der Lei, J.; Moll, H.A. Validity of the Manchester Triage System in paediatric emergency care. Emerg. Med. J. 2006, 23, 906–910. [Google Scholar] [CrossRef]
- Eitel, D.R.; Travers, D.A.; Rosenau, A.M.; Gilboy, N.; Wuerz, R.C. The emergency severity index triage algorithm version 2 is reliable and valid. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2003, 10, 1070–1080. [Google Scholar] [CrossRef]
- Worster, A.; Fernandes, C.M.; Eva, K.; Upadhye, S. Predictive validity comparison of two five-level triage acuity scales. Eur. J. Emerg. Med. Off. J. Eur. Soc. Emerg. Med. 2007, 14, 188–192. [Google Scholar] [CrossRef]
- Doherty, S.R.; Hore, C.T.; Curran, S.W. Inpatient mortality as related to triage category in three New South Wales regional base hospitals. Emerg. Med. 2003, 15, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Which Triage Categories Die in Hospital after Being Admitted through Emergency Departments? A Study in One Teaching Hospital|Request PDF. Available online: https://www.researchgate.net/publication/229965635_Which_triage_categories_die_in_hospital_after_being_admitted_through_emergency_departments_A_study_in_one_teaching_hospital (accessed on 25 January 2023).
- McHugh, M.; Tanabe, P.; McClelland, M.; Khare, R.K. More patients are triaged using the Emergency Severity Index than any other triage acuity system in the United States. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2012, 19, 106–109. [Google Scholar] [CrossRef] [PubMed]
- Savioli, G.; Bressan, M.; Ceresa, I. How Many Patients Are Triaged Using Five-Level Triage Scales Compared to Any Other Triage Acuity System in Italy? A SIMEU (Italian Scientific Society of Emergency Medicine) Faculty Triage Survey. In Proceedings of the EUSEM, Lisbon, Portugal, 27–31 October 2021. [Google Scholar]
- Bullard, M.J.; Musgrave, E.; Warren, D.; Unger, B.; Skeldon, T.; Grierson, R.; van der Linde, E.; Swain, J. Revisions to the Canadian Emergency Department Triage and Acuity Scale (CTAS) Guidelines 2016. CJEM 2017, 19, S18–S27. [Google Scholar] [CrossRef] [PubMed]
- Vermeulen, M.J.; Guttmann, A.; Stukel, T.A.; Kachra, A.; Sivilotti, M.L.A.; Rowe, B.H.; Dreyer, J.; Bell, R.; Schull, M. Are reductions in emergency department length of stay associated with improvements in quality of care? A difference-in-differences analysis. BMJ Qual. Saf. 2016, 25, 489–498. [Google Scholar] [CrossRef]
- Affleck, A.; Parks, P.; Drummond, A.; Rowe, B.H.; Ovens, H.J. Emergency department overcrowding and access block. CJEM 2013, 15, 359–384. [Google Scholar] [CrossRef] [PubMed]
- Bond, K.; Ospina, M.B.; Blitz, S.; Afilalo, M.; Campbell, S.G.; Bullard, M.; Innes, G.; Holroyd, B.; Curry, G.; Schull, M.; et al. Frequency, determinants and impact of overcrowding in emergency departments in Canada: A national survey. Healthc. Q. (Tor. Ont.) 2007, 10, 32–40. [Google Scholar] [CrossRef]
- Elrod, J.K.; Fortenberry, J.L. The hub-and-spoke organization design revisited: A lifeline for rural hospitals. BMC Health Serv. Res. 2017, 17 (Suppl. S4), 795. [Google Scholar] [CrossRef]
- Jones, P.; Wells, S.; Ameratunga, S. Towards a best measure of emergency department crowding: Lessons from current Australasian practice. Emerg. Med. Australas. 2018, 30, 214–221. [Google Scholar] [CrossRef]
- Hwang, U.; McCarthy, M.L.; Aronsky, D.; Asplin, B.; Crane, P.W.; Craven, C.K.; Epstein, S.K.; Fee, C.; Handel, D.A.; Pines, J.M.; et al. Measures of crowding in the emergency department: A systematic review. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2011, 18, 527–538. [Google Scholar] [CrossRef]
- Richards, J.R.; Navarro, M.L.; Derlet, R.W. Survey of directors of emergency departments in California on overcrowding. West. J. Med. 2000, 172, 385–388. [Google Scholar] [CrossRef]
- Derlet, R.; Richards, J.; Kravitz, R. Frequent overcrowding in U.S. emergency departments. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2001, 8, 151–155. [Google Scholar] [CrossRef]
- Hoot, N.R.; LeBlanc, L.J.; Jones, I.; Levin, S.R.; Zhou, C.; Gadd, C.S.; Aronsky, D. Forecasting Emergency Department Crowding: A Prospective, Real-time Evaluation. J. Am. Med. Inform. Assoc. 2009, 16, 338–345. [Google Scholar] [CrossRef]
- Han, J.H.; Zhou, C.; France, D.J.; Zhong, S.; Jones, I.; Storrow, A.B.; Aronsky, D. The effect of emergency department expansion on emergency department overcrowding. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2007, 14, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Miro, O.; Sanchez, M.; Espinosa, G.; Coll-Vinent, B.; Bragulat, E.; Milla, J.; Wardrope, J. Analysis of patient flow in the emergency department and the effect of an extensive reorganisation. Emerg. Med. J. 2003, 20, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Bullard, M.J.; Villa-Roel, C.; Bond, K.; Vester, M.; Holroyd, B.R.; Rowe, B.H. Tracking emergency department overcrowding in a tertiary care academic institution. Healthc. Q. (Tor. Ont.) 2009, 12, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Asaro, P.V.; Lewis, L.M.; Boxerman, S.B. Emergency department overcrowding: Analysis of the factors of renege rate. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2007, 14, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.S.; Evans, R.S.; Allen, T.L.; Thomas, A.; Haug, P.J.; Welch, S.J.; Snow, G.L. A multivariate time series approach to modeling and forecasting demand in the emergency department. J. Biomed. Inform. 2009, 42, 123–139. [Google Scholar] [CrossRef]
- Steele, R.; Kiss, A. EMDOC (Emergency Department Overcrowding) Internet-Based Safety Net Research. J. Emerg. Med. 2008, 35, 101–107. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, M.L.; Zeger, S.L.; Ding, R.; Levin, S.R.; Desmond, J.S.; Lee, J.; Aronsky, D. Crowding delays treatment and lengthens emergency department length of stay, even among high-acuity patients. Ann. Emerg. Med. 2009, 54, 492–503.e4. [Google Scholar] [CrossRef]
- Schneider, S.M.; Gallery, M.E.; Schafermeyer, R.; Zwemer, F.L. Emergency department crowding: A point in time. Ann. Emerg. Med. 2003, 42, 167–172. [Google Scholar] [CrossRef]
- Emergency Department Patient Flow: The Influence of Hospital Census Variables on Emergency Department Length of Stay-PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/19438415/ (accessed on 2 April 2023).
- Rathlev, N.K.; Chessare, J.; Olshaker, J.; Obendorfer, D.; Mehta, S.D.; Rothenhaus, T.; Crespo, S.; Magauran, B.; Davidson, K.; Shemin, R.; et al. Time series analysis of variables associated with daily mean emergency department length of stay. Ann. Emerg. Med. 2007, 49, 265–271. [Google Scholar] [CrossRef]
- Jones, S.S.; Thomas, A.; Evans, R.S.; Welch, S.J.; Haug, P.J.; Snow, G.L. Forecasting daily patient volumes in the emergency department. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2008, 15, 159–170. [Google Scholar] [CrossRef]
- Advanced Statistics: Developing a Formal Model of Emergency Department Census and Defining Operational Efficiency-PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/17726126/ (accessed on 2 April 2023).
- McCarthy, M.L.; Aronsky, D.; Jones, I.D.; Miner, J.R.; Band, R.A.; Baren, J.M.; Desmond, J.S.; Baumlin, K.M.; Ding, R.; Shesser, R. The emergency department occupancy rate: A simple measure of emergency department crowding? Ann. Emerg. Med. 2008, 51, 15–24. [Google Scholar] [CrossRef]
- Hoot, N.R.; Zhou, C.; Jones, I.; Aronsky, D. Measuring and forecasting emergency department crowding in real time. Ann. Emerg. Med. 2007, 49, 747–755. [Google Scholar] [CrossRef]
- Schweigler, L.M.; Desmond, J.S.; McCarthy, M.L.; Bukowski, K.J.; Ionides, E.L.; Younger, J.G. Forecasting models of emergency department crowding. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2009, 16, 301–308. [Google Scholar] [CrossRef]
- Litvak, E.; McManus, M.; Cooper, A. Root Cause Analysis of Emergency Department Crowding and Ambulance Diversion in Massachusetts. Boston Univ. Program. Manag. Var. Health Care Deliv. 2002, 4, 4–5. [Google Scholar]
- Ospina, M.B.; Bond, K.; Schull, M.; Innes, G.; Blitz, S.; Rowe, B.H. Key indicators of overcrowding in Canadian emergency departments: A Delphi study. CJEM 2007, 9, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Solberg, L.I.; Asplin, B.R.; Weinick, R.M.; Magid, D.J. Emergency department crowding: Consensus development of potential measures. Ann. Emerg. Med. 2003, 42, 824–834. [Google Scholar] [CrossRef]
- Schull, M.J.; Kiss, A.; Szalai, J.P. The effect of low-complexity patients on emergency department waiting times. Ann. Emerg. Med. 2007, 49, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Oredsson, S.; Jonsson, H.; Rognes, J.; Lind, L.; Göransson, K.E.; Ehrenberg, A.; Asplund, K.; Castrén, M.; Farrohknia, N. A systematic review of triage-related interventions to improve patient flow in emergency departments. Scand. J. Trauma Resusc. Emerg. Med. 2011, 19, 43. [Google Scholar] [CrossRef]
- Total Access Block Time: A Comprehensive and Intuitive Way to Measure the Total Effect of Access Block on the Emergency Department-PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/18251728/ (accessed on 26 January 2023).
- Al-Qahtani, S.; Alsultan, A.; Haddad, S.; Alsaawi, A.; Alshehri, M.; Alsolamy, S.; Felebaman, A.; Tamim, H.M.; Aljerian, N.; Al-Dawood, A.; et al. The association of duration of boarding in the emergency room and the outcome of patients admitted to the intensive care unit. BMC Emerg. Med. 2017, 17, 34. [Google Scholar] [CrossRef]
- Cha, W.C.; Cho, J.S.; Shin, S.D.; Lee, E.J.; Ro, Y.S. The impact of prolonged boarding of successfully resuscitated out-of-hospital cardiac arrest patients on survival-to-discharge rates. Resuscitation 2015, 90, 25–29. [Google Scholar] [CrossRef]
- Chalfin, D.B.; Trzeciak, S.; Likourezos, A.; Baumann, B.M.; Dellinger, R.P.; DELAY-ED Study Group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit. Care Med. 2007, 35, 1477–1483. [Google Scholar] [CrossRef]
- Saviano, A.; Ojetti, V.; Zanza, C.; Franceschi, F.; Longhitano, Y.; Martuscelli, E.; Maiese, A.; Volonnino, G.; Bertozzi, G.; Ferrara, M.; et al. Liver Trauma: Management in the Emergency Setting and Medico-Legal Implications. Diagnostics 2022, 12, 1456. [Google Scholar] [CrossRef]
- Development of a Site Sampling form for Evaluation of ED Overcrowding-PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/12165740/ (accessed on 26 January 2023).
- Savioli, G.; Ceresa, I.F.; Gri, N.; Bavestrello Piccini, G.; Longhitano, Y.; Zanza, C.; Piccioni, A.; Esposito, C.; Ricevuti, G.; Bressan, M.A. Emergency Department Overcrowding: Understanding the Factors to Find Corresponding Solutions. J. Pers. Med. 2022, 12, 279. [Google Scholar] [CrossRef] [PubMed]
- Savioli, G.; Ceresa, I.F.; Novelli, V.; Ricevuti, G.; Bressan, M.A.; Oddone, E. How the coronavirus disease 2019 pandemic changed the patterns of healthcare utilization by geriatric patients and the crowding: A call to action for effective solutions to the access block. Intern. Emerg. Med. 2022, 17, 503. [Google Scholar] [CrossRef] [PubMed]
- Savioli, G.; Ceresa, I.; Guarnone, R.; Muzzi, A.; Novelli, V.; Ricevuti, G.; Iotti, G.; Bressan, M.; Oddone, E. Impact of Coronavirus Disease 2019 Pandemic on Crowding: A Call to Action for Effective Solutions to “Access Block”. West J Emerg Med. 2021, 22, 860–870. [Google Scholar] [CrossRef]
- Savioli, G.; Ceresa, I.F.; Novara, E.; Persiano, T.; Grulli, F.; Ricevuti, G.; Bressan, M.A.; Oddone, E. Brief intensive observation areas in the management of acute heart failure in elderly patients leading to high stabilisation rate and less admissions. J. Gerontol. Geriatr. 2021, 69, 87–97. [Google Scholar] [CrossRef]
- Boudi, Z.; Lauque, D.; Alsabri, M.; Östlundh, L.; Oneyji, C.; Khalemsky, A.; Lojo Rial, C.; Liu, S.; Camargo, C.A., Jr.; Aburawi, E.; et al. Association between boarding in the emergency department and in-hospital mortality: A systematic review. PLoS ONE 2020, 15, e0231253. [Google Scholar] [CrossRef]
- Kuriyama, A.; Urushidani, S.; Nakayama, T. Five-level emergency triage systems: Variation in assessment of validity. Emerg. Med. J. 2017, 34, 703–710. [Google Scholar] [CrossRef]
- Ausserhofer, D.; Zaboli, A.; Pfeifer, N.; Siller, M.; Turcato, G. Performance of the Manchester Triage System in patients with dyspnoea: A retrospective observational study. Int. Emerg. Nurs. 2020, 53, 100931. [Google Scholar] [CrossRef]
- Brutschin, V.; Kogej, M.; Schacher, S.; Berger, M.; Gräff, I. The presentational flow chart “unwell adult” of the Manchester Triage System-Curse or blessing? PLoS ONE 2021, 16, e0252730. [Google Scholar] [CrossRef]
- Zanza, C.; Romenskaya, T.; Zuliani, M.; Piccolella, F.; Bottinelli, M.; Caputo, G.; Rocca, E.; Maconi, A.; Savioli, G.; Longhitano, Y. Acute Traumatic Pain in the Emergency Department. Diseases 2023, 11, 45. [Google Scholar] [CrossRef] [PubMed]
- Travers, D.A.; Waller, A.E.; Katznelson, J.; Agans, R. Reliability and validity of the emergency severity index for pediatric triage. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2009, 16, 843–849. [Google Scholar] [CrossRef]
- González, J.; Soltero, R. Emergency Severity Index (ESI) triage algorithm: Trends after implementation in the emergency department. Boletín Asoc. Médica Puerto Rico 2009, 101, 7–10. [Google Scholar]
- Parenti, N.; Reggiani, M.L.B.; Iannone, P.; Percudani, D.; Dowding, D. A systematic review on the validity and reliability of an emergency department triage scale, the Manchester Triage System. Int. J. Nurs. Stud. 2014, 51, 1062–1069. [Google Scholar] [CrossRef]
- Zachariasse, J.M.; Seiger, N.; Rood, P.P.M.; Alves, C.F.; Freitas, P.; Smit, F.J.; Roukema, G.R.; Moll, H.A. Validity of the Manchester Triage System in emergency care: A prospective observational study. PLoS ONE 2017, 12, e0170811. [Google Scholar] [CrossRef] [PubMed]
- Hoot, N.R.; LeBlanc, L.J.; Jones, I.; Levin, S.R.; Zhou, C.; Gadd, C.S.; Aronsky, D. Forecasting Emergency Department Crowding: A Discrete Event Simulation. Ann. Emerg. Med. 2008, 52, 116–125. [Google Scholar] [CrossRef]
- Savioli, G.; Ceresa, I.F.; Macedonio, S.; Gerosa, S.; Belliato, M.; Luzzi, S.; Lucifero, A.G.; Manzoni, F.; Ricevuti, G.; Bressan, M.A. Major Trauma in Elderly Patients: Worse Mortality and Outcomes in an Italian Trauma Center. J. Emerg. Trauma Shock 2021, 14, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Savioli, G.; Ceresa, I.F.; Giordano, M.; Ferrari, I.; Varesi, A.; Floris, V.; Esposito, C.; Croesi, B.; Ricevuti, G.; Calvi, M.; et al. The Reliability of Anamnestic Data in the Management of Clostridium Tetani Infection in Elderly. Front. Med. 2021, 8, 684594. [Google Scholar] [CrossRef]
- Savioli, G.; Ceresa, I.F.; Luzzi, S.; Giotta Lucifero, A.; Pioli Di Marco, M.S.; Manzoni, F.; Preda, L.; Ricevuti, G.; Bressan, M.A. Mild Head Trauma: Is Antiplatelet Therapy a Risk Factor for Hemorrhagic Complications? Medicina 2021, 57, 357. [Google Scholar] [CrossRef]
- Savioli, G.; Ceresa, I.F.; Macedonio, S.; Gerosa, S.; Belliato, M.; Iotti, G.A.; Luzzi, S.; Del Maestro, M.; Mezzini, G.; Giotta Lucifero, A.; et al. Trauma Coagulopathy and Its Outcomes. Medicina 2020, 56, 205. [Google Scholar] [CrossRef]
- Messina, A.; Longhitano, Y.; Zanza, C.; Calabrò, L.; Villa, F.; Cammarota, G.; Sanfilippo, F.; Cecconi, M.; Robba, C. Cardiac dysfunction in patients affected by subarachnoid haemorrhage affects in-hospital mortality: A systematic review and metanalysis. Eur. J. Anaesthesiol. 2023. Epub ahead of print. [Google Scholar] [CrossRef]
- Savioli, G.; Ceresa, I.F.; Luzzi, S.; Gragnaniello, C.; Giotta Lucifero, A.; Del Maestro, M.; Marasco, S.; Manzoni, F.; Ciceri, L.; Gelfi, E.; et al. Rates of Intracranial Hemorrhage in Mild Head Trauma Patients Presenting to Emergency Department and Their Management: A Comparison of Direct Oral Anticoagulant Drugs with Vitamin K Antagonists. Medicina 2020, 56, 308. [Google Scholar] [CrossRef]
- Savioli, G.; Ceresa, I.F.; Ciceri, L.; Sciutti, F.; Belliato, M.; Iotti, G.A.; Luzzi, S.; Del Maestro, M.; Mezzini, G.; Lafe, E.; et al. Mild head trauma in elderly patients: Experience of an emergency department. Heliyon 2020, 6, e04226. [Google Scholar] [CrossRef]
- Emergency Medicine Physicians’ Ability to Predict Hospital Admission at the Time of Triage-PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/29960659/ (accessed on 26 January 2023).
- Herzog, S.M.; Jenny, M.A.; Nickel, C.H.; Nieves Ortega, R.; Bingisser, R. Emergency department patients with weakness or fatigue: Can physicians predict their outcomes at the front door? A prospective observational study. PLoS ONE 2020, 15, e0239902. [Google Scholar] [CrossRef]
- Zwank, M.D.; Koops, J.J.; Adams, N.R. Provider-in-triage prediction of hospital admission after brief patient interaction. Am. J. Emerg. Med. 2021, 40, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.C.; Ng, C.J.; Wu, C.T.; Chen, L.C.; Chen, J.C.; Hsu, K.H. Effectiveness of a five-level Paediatric Triage System: An analysis of resource utilisation in the emergency department in Taiwan. Emerg. Med. J. 2013, 30, 735–739. [Google Scholar] [CrossRef]
- Lerner, E.B.; Shah, M.N.; Swor, R.A.; Cushman, J.T.; Guse, C.E.; Brasel, K.; Blatt, A.; Jurkovich, G.J. Comparison of the 1999 and 2006 trauma triage guidelines: Where do patients go? Prehospital Emerg. Care 2011, 15, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Lerner, E.B.; Cushman, J.T.; Drendel, A.L.; Badawy, M.; Shah, M.N.; Guse, C.E.; Cooper, A. Effect of the 2011 Revisions to the Field Triage Guidelines on Under- and Over-Triage Rates for Pediatric Trauma Patients. Prehospital Emerg. Care 2017, 21, 456–460. [Google Scholar] [CrossRef]
- Ellebrecht, N. Why Is Treatment Urgency Often Overestimated? An Experimental Study on the Phenomenon of Over-triage. Disaster Med. Public Health Prep. 2020, 14, 563–567. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).