Abstract
With population growth and aging, the emergence of new diseases and immunodeficiency, the demand for emergency departments (EDs) increases, making overcrowding in these departments a global problem. Due to the disease severity and transmission rate of COVID-19, it is necessary to provide an accurate and automated triage system to classify and isolate the suspected cases. Different triage methods for COVID-19 patients have been proposed as disease symptoms vary by country. Still, several problems with triage systems remain unresolved, most notably overcrowding in EDs, lengthy waiting times and difficulty adjusting static triage systems when the nature and symptoms of a disease changes. In this paper, we conduct a comprehensive review of general ED triage systems as well as COVID-19 triage systems. We identified important parameters that we recommend considering when designing an e-Triage (electronic triage) system for EDs, namely waiting time, simplicity, reliability, validity, scalability, and adaptability. Moreover, the study proposes a scoring-based e-Triage system for COVID-19 along with several recommended solutions to enhance the overall outcome of e-Triage systems during the outbreak. The recommended solutions aim to reduce overcrowding and overheads in EDs by remotely assessing patients’ conditions and identifying their severity levels.
1. Introduction
On 30 January 2020, the World Health Organization (WHO) declared the spread of the COVID-19 pandemic to be a public health emergency of international concern. This epidemic has spread rapidly around the world, the virus is transmitted primarily through close contact between individuals, and often through respiratory droplets and droplets resulting from coughing, sneezing, or talking [1]. From this end, social distancing and reducing gatherings were recommended to reduce the chances of the virus being transmitted from an infected person to another healthy person [1,2,3]. The emergency departments (EDs) present great opportunities for the transmission of the virus, as it is possible that people with COVID-19 will be in contact with others due to the overcrowding and long waiting times [4]. Furthermore, preventive measures enacted by governments must be adhered to [5,6], as recent literature indicates that the COVID-19 virus spread is still expected to increase, and that the readiness of public health systems will face a global challenge [7].
Overcrowding in the ED has been linked with increased inpatient death, increased waiting times, and increased expenditures for admitted patients [8,9,10,11]. ED wait times and leave-without-treatment (times where patients arrive to the ED but leave prior to getting a medical assessment) are signs of overcrowding. Hospitals are continually trying to balance short ED wait times with the quality of emergency service. There are several triage approaches for arranging patients on the ED waiting lists as well as for determining waiting time. The triage method can depend on several factors [12] to determine the waiting time, such as how sick the admitted patient is, if other patients are sicker, how many nurses and doctors are on staff during the visit, and if there are critical patients who come in while you are waiting.
Due to the rise in COVID-19 cases [13], EDs will be overwhelmed with COVID-19 suspected or infected patients. Several protocols have been adopted to deal with this congestion and reduce the consequences of it, including the recruitment of special teams within the ED to manage the allocation of appropriate resources to suitable patients when there are a large number of COVID-19 cases. Adoption of the infrared thermal camera scanning at the first entry point to the hospital and the EDs for early detection of COVID-19 suspected cases by measuring the body temperature [14]. Also, to reduce overcrowding in outpatients clinics, medications prescribed for chronic cases are sent to them to reduce the need for hospital visits [8].
Telemedicine [15,16,17,18,19,20,21], Blockchain [22,23], machine learning algorithms [24], the adoption of sensor technologies [25,26] and Internet of Things devices in remote patient monitoring will play an important role in early detection of COVID-19 patients [27,28,29,30,31,32,33], in addition to that, it will reduce overcrowding of patients in EDs by monitoring patients’ vital signs remotely using sensors. Then, identify the severity level to determine if there is a need to visit the ED or not. However, there is no triage system for EDs that employ these techniques well to classify and prioritize patients remotely, which is an urgent need to deal with the risk of spreading COVID-19 and other infectious diseases.
There are three types of triage systems; namely emergency triage, disease triage, and outpatient triage [34]. The study in this paper focuses only on emergency triage. Most of the triage systems are designed with different characteristics to handle specific conditions, therefore, it was difficult to employ the current ED’s triage systems [35] to classify COVID-19 cases, which necessitated the need to quickly design a new system, which was not an electronic system. Moreover, the standard parameters that should be considered when designing an electronic triage system for EDs are not yet identified.
Providing an electronic triage (e-triage) system designed for COVID-19 considering its nature and characteristics will have great contributions to public healthcare facilities, governments, and society. The contributions include, for example, reducing the average waiting time at EDs, minimizing the overhead due to the outbreak, optimizing the usage of healthcare resources, and estimating patient severity level remotely.
In this paper, we study the popular international ED triage systems that were widespread, adopted based on the claim of a systematic review published in 2019 [35]. We also review other proposed ED triage systems found in the literature for classifying patients considering improving the ED’s triage process, including reducing waiting times, digitizing, and conducting the triage remotely, the literature will be reviewed in the range from 2016 to 2021 with snowballing to collect any relevant study. Exploring such studies could help define the capabilities of these systems to manage COVID-19 cases as well as investigate the possibility of adapting these systems to COVID-19 conditions. Moreover, we review the methods proposed and announced in the literature, since the beginning of the COVID-19 epidemic, to classify COVID-19 patients in EDs around the world. We study and classify the symptoms that are relied on to classify COVID-19 patients. We also provide a comprehensive taxonomy shows all the triage approaches reviewed in this paper.
Based on the literature review conducted in this paper, we introduce several evaluation parameters to be considered when designing or implementing ED triage system. Moreover, we present our recommendations for an e-triage system with considerations to the COVID-19 circumstances.
As we believe our study carries multiple strength of conducting a comprehensive search on multiple national and international triage systems and exploring advantages and disadvantages of each. As a summary, the main contributions in our study are as follows. First, as to our knowledge, this study explored most of the studies relevant to ED triage systems with a focus on COVID-19 outbreak where we presented main findings and observations about COVID-19 related symptoms, admission criteria, and patients’ classification rules during COVID-19 outbreak. Second, in this work, we provided discussions and summaries on different aspects of COVID-19 triaging systems, which would help other researchers to build on further evaluation studies on triage approaches at EDs during epidemics. Third, as a part of our evaluation section, we identified main parameters that should be considered when designing and building e-triage systems for controlling and managing outbreaks at EDs. Finally, we provided several recommended solutions to enhance e-triage systems used during outbreaks. For example, we recommended a scoring-based e-triage system to enhance the admission criteria during the COVID-19 pandemic considering the applied triage system adopted by the Ministry of Health (MOH) in Saudi Arabia. Moreover, we conducted an initial statistical evaluation for the recommended e-Triage scoring thresholds using a simple dataset obtained from our local COVID-19 patients who visited the ED during the pandemics which resulted in a proposed approach for e-triaging during pandemics.
The rest of this paper is organized as follows. First, Section 2 provides a review of the ED triage systems found in the literature. Then, Section 3 presents evaluation and discussion on different parameters of EDs triage systems. Then, Section 4 introduces our recommendations regarding the e-Triage system for COVID-19. Finally, Section 5 concludes the paper and presents future work directions.
2. Literature Review
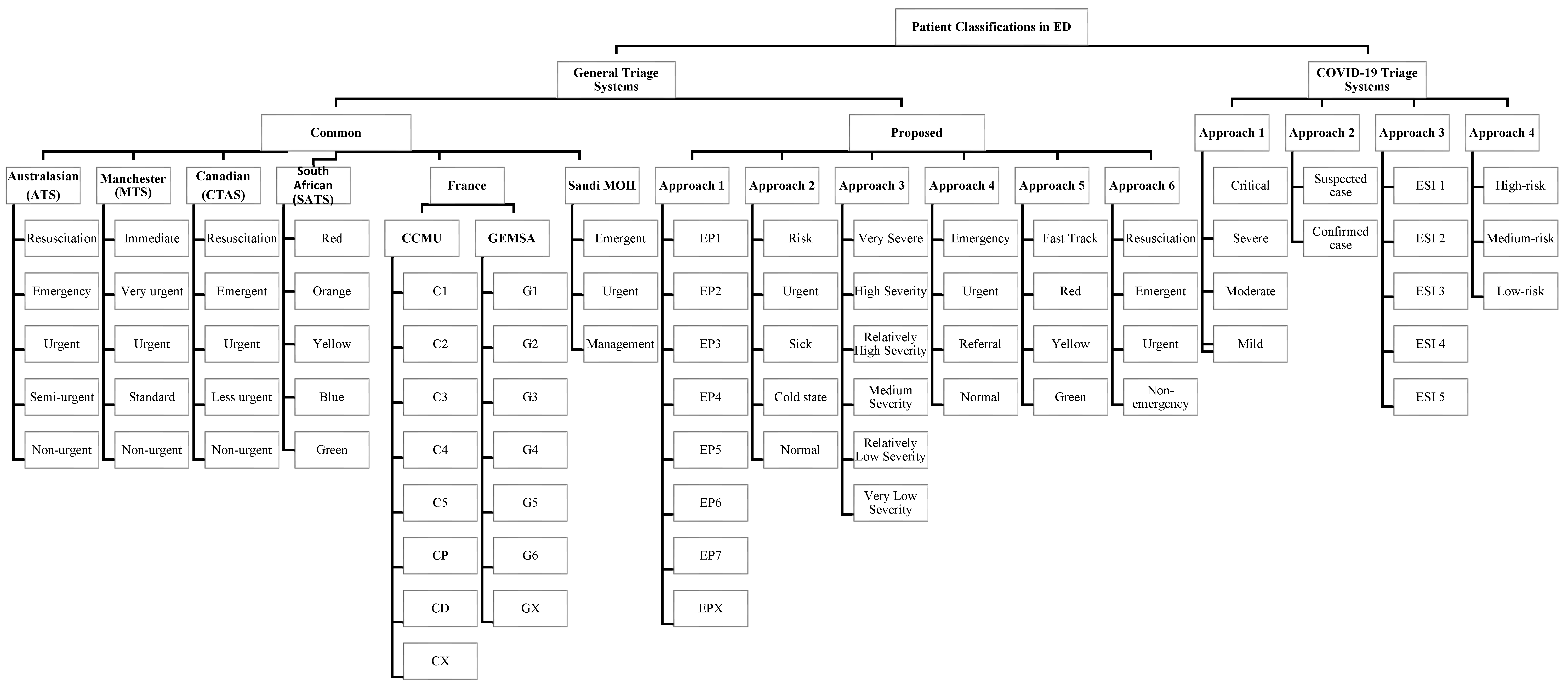
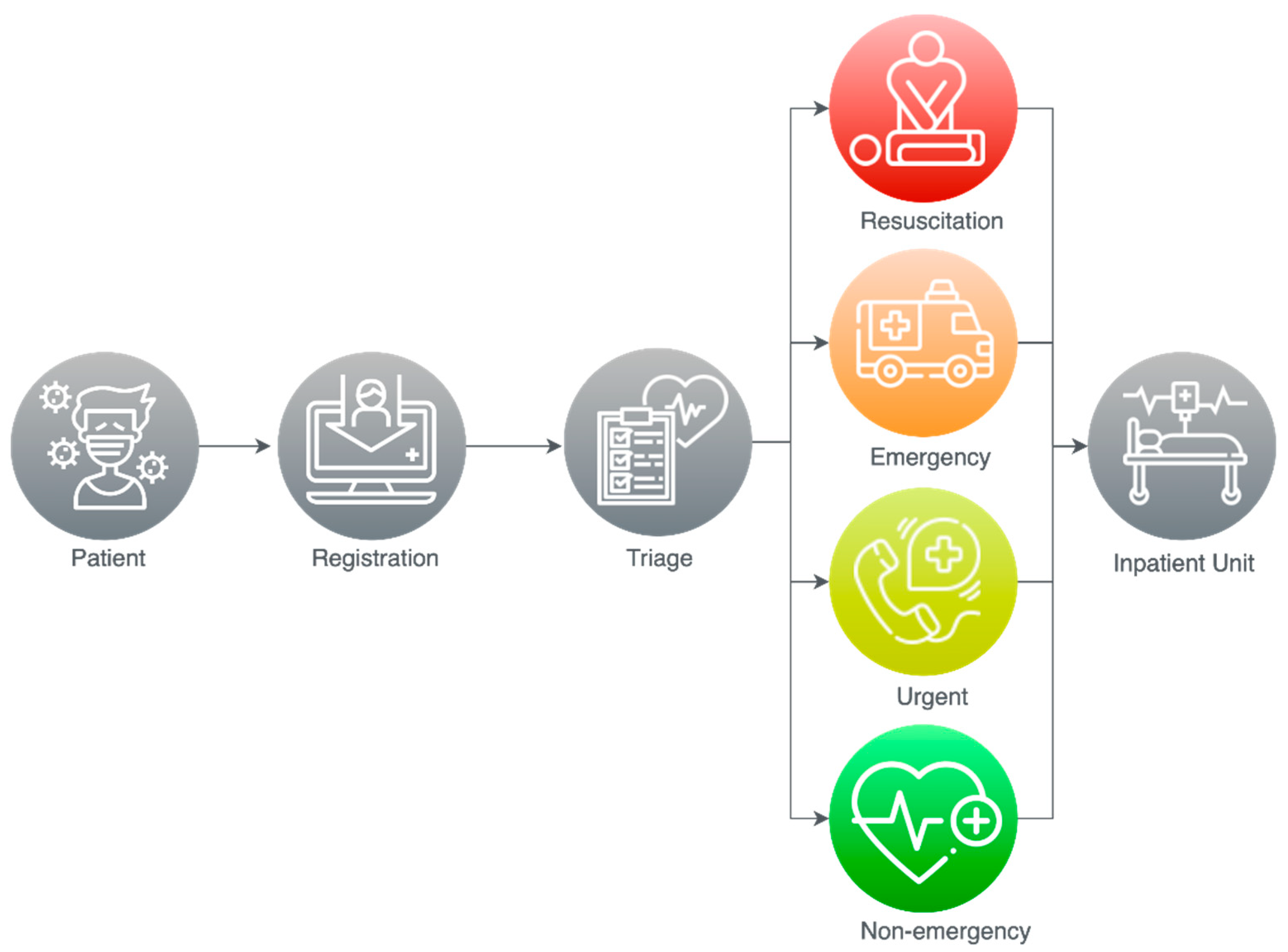
The literature provides a respectable number of triage approaches; however, this section will discuss and analyze the most important triage solutions used to enhance the EDs, where Figure 1 provides a classification of the approaches reviewed and shows their triage categories. Section 2.1 and Section 3 provide more details on the approaches and their classes. The rest of this section is divided into two subsections. First, Section 2.1 discusses the general EDs triage systems. Then, Section 2.2 focuses on the EDs triage systems that have addressed COVID-19.
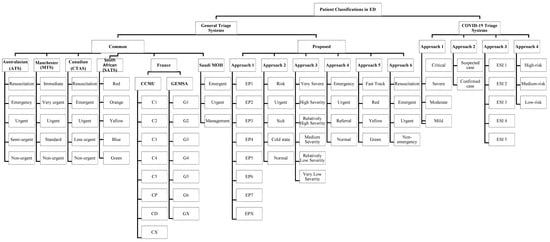
Figure 1.
Patient classification approaches in EDs.
2.1. ED General Triage Systems
Triage systems are applied in many countries worldwide. Table 1 shows the most common international systems used for classifying patients in EDs [35]. However, these systems are paper-based, applied on-site by the triage nurses, and the specified waiting time for some triage categories is not acceptable by patients and may worsen their condition. It is also challenging to adapt them to address different conditions such as the classification of patients with COVID-19. Therefore, several solutions have been suggested in the literature to address some of the issues in current ED triage systems.

Table 1.
Common international ED triage systems.
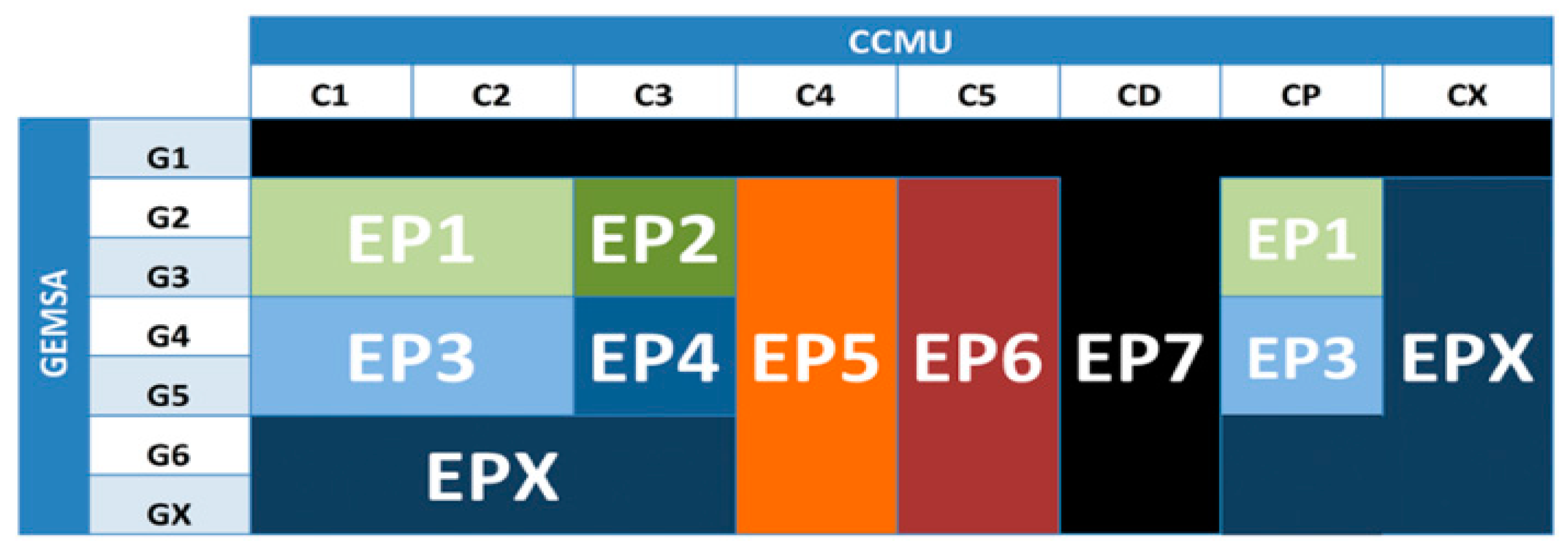
There are several solutions found in the literature that have attempted to address issues in current ED triage systems. For example, the authors in [8] tried to improve the French ED triage system. They proposed a new classification method for ED patients called EP which combines categories defined by the two classification methods used in the French triage system, namely CCMU and GEMSA. They also designed a time-series forecasting model to predict the daily number of ED visits. The EP classification method was based on statistical tests that were performed on patient data collected from the Troy Hospital ED during the period from 2010 to 2014 along with the experience of the staff using CCMU and GEMSA classifications. As shown in Figure 2, the EP classification method consists of eight categories created by grouping multiple categories defined by CCMU and GEMSA. The performance of their forecasting model was 91.08% for long-term predictions and 91.84% for short-term predictions. However, while the study aimed to predict the daily number of ED patients to help in managing the required resources, it did not address the treatment priority of patients or estimated waiting times.
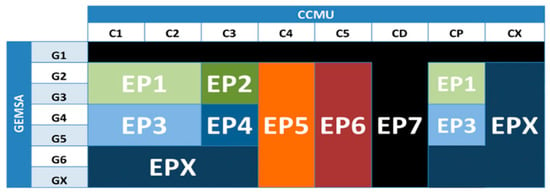
Figure 2.
EP classification of ED patients [8].
Furthermore, the authors in [44] introduced a framework named multi-sources healthcare architecture (MSHA) to enhance the scalability of advanced healthcare applications by adding tele-monitoring and remote triaging features. The framework adopts three sensors which monitor oxygen saturation (SpO2), electrocardiography (ECG) signals, and blood pressure. It also accepts text-based input from wireless body area network devices. It consists of three tiers, the first is for data collection, the second is for data pre-processing and patient prioritization processes to determine pathological conditions, while the third tier is for patient data management on a cloud database server. The patient triage level is determined based on medical guidelines and a multi-sources data fusion algorithm. Each patient will have a priority code (PC) ranging from 0 to 100 to describe the severity level of their health condition, where a higher PC indicates a more serious condition. The scheduling algorithm sorts patient requests into a queue based on the PC value. Requests with equal PC values are sorted in descending order based on each patient’s waiting time.
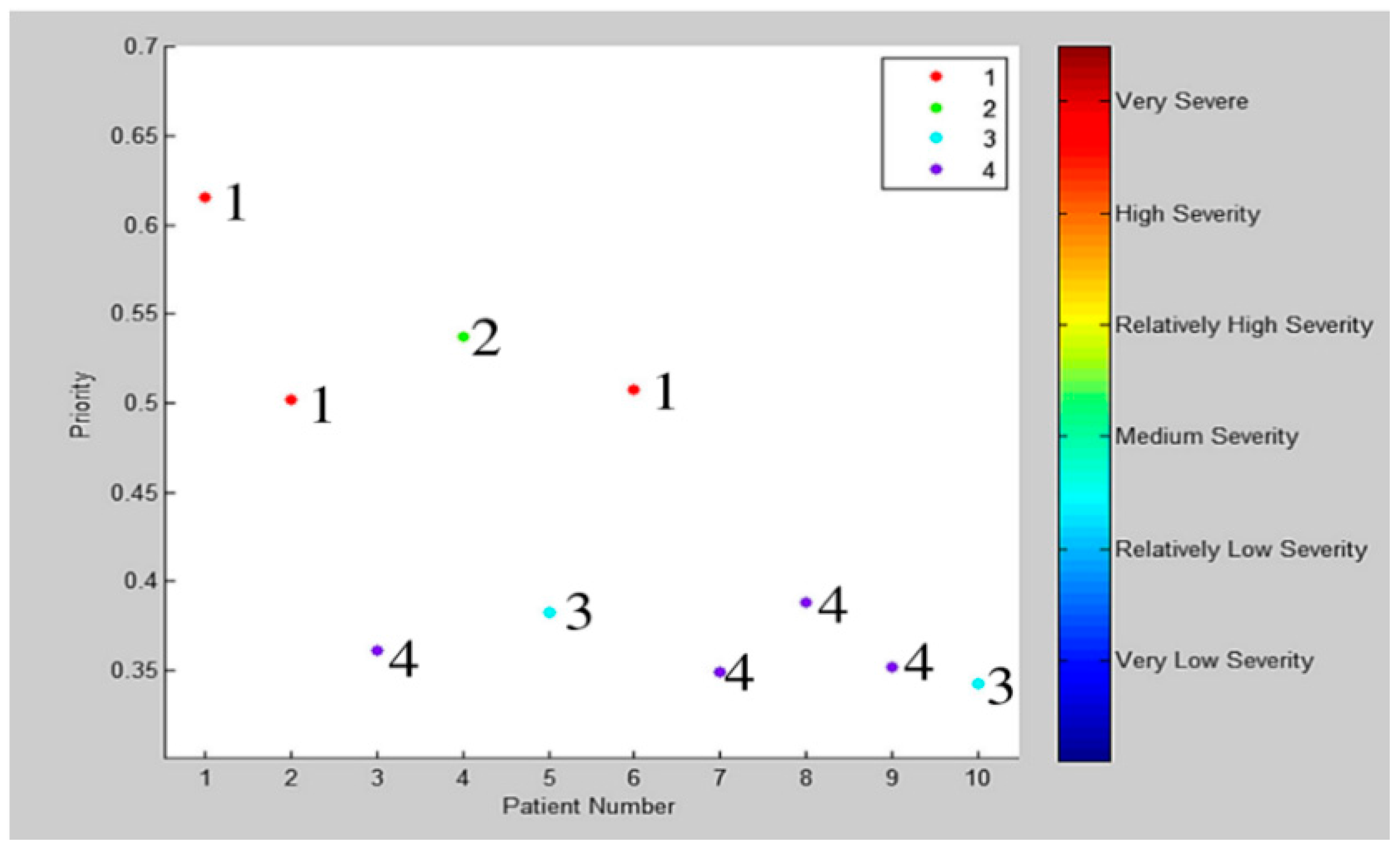
Alternatively, the authors in [45] improved the triage process by applying the group technology concept to develop a dynamic grouping and prioritization (DGP) algorithm. They have considered several measures of system performance, such as length of stay (LOS), time-to-bed (TTB), time in ED, throughput, percentage of late patients, and the risk of delaying patients. Patients are categorized into eight types based on their age, group, and priority. Patients will be prioritized in groups from 1 to 10 as shown in Figure 3.
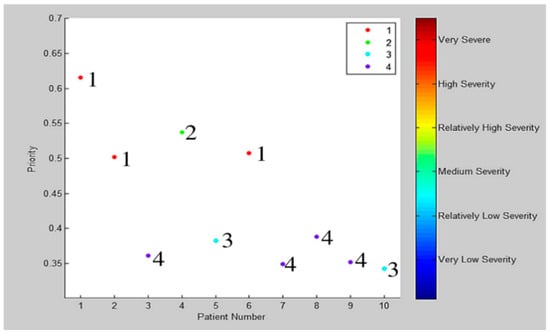
Figure 3.
Patients priority (the number next to each point represents the patient group) [45].
Moreover, the authors in [46] proposed a new system to prioritize and schedule patient visits based on the patient’s health and vital conditions. The system classifies patients into four categories and then prioritizes them according to the type of service required and its duration. The authors also tried to reduce the waiting time for both physicians and patients by using the genetic algorithm. When adding a patient to a queue, the algorithm permutates patients in that queue based on the priority of the patient who was added, which consequently reduces the average waiting time.
It is important to note that patients’ conditions may worsen during the waiting period, putting their lives at risk. As a solution, the authors in [47] proposed a real-time patient prioritization system that improves the Manchester triage system of emergency services. They suggested monitoring and evaluating the patient’s vital signs continuously through the patient’s hospital emergency smart band (HESB) and a smart priority recommendation and patient control system (SPRPC) to re-sort the patients when there is a risk alert. Moreover, the system can locate the patient inside the hospital through the passive communication between the smart patient’s wristband and the sensors placed on the buildings’ doors. However, the authors mentioned several challenges that could hinder the implementation of their proposal. First, the solution should be economically profitable, but it is a challenge to make the HESB cheap without losing the reliability or accuracy of its sensors. Also, it is best for the HESB to be reusable. Additionally, integrating the proposed system with existing hospital systems is a challenge, as hospital systems are mostly proprietary systems that are developed by external companies. It must also be ensured that wireless communications should not affect medical equipment.
There are several studies interested in improving the CTAS, such as the model proposed in [48] which aimed to estimate the waiting time and the required number of ED and IU resources by employing the queuing theory methods to achieve CTAS performance targets. It also investigated the effect of the fast track path on the average patient waiting time. It considered the priority of the different triage classes that require ED resources, and the effect of congestion on the time it takes patients to access the ED. However, there are several limitations of this model. The first being that the authors assumed that it is possible to accommodate any type of patient in the inpatient unit, while there are certain cases that require accommodation in specialized units. Additionally, the proposed model is based on steady-state and average arrival rates, while the arrival rate on the other hand is not fixed.
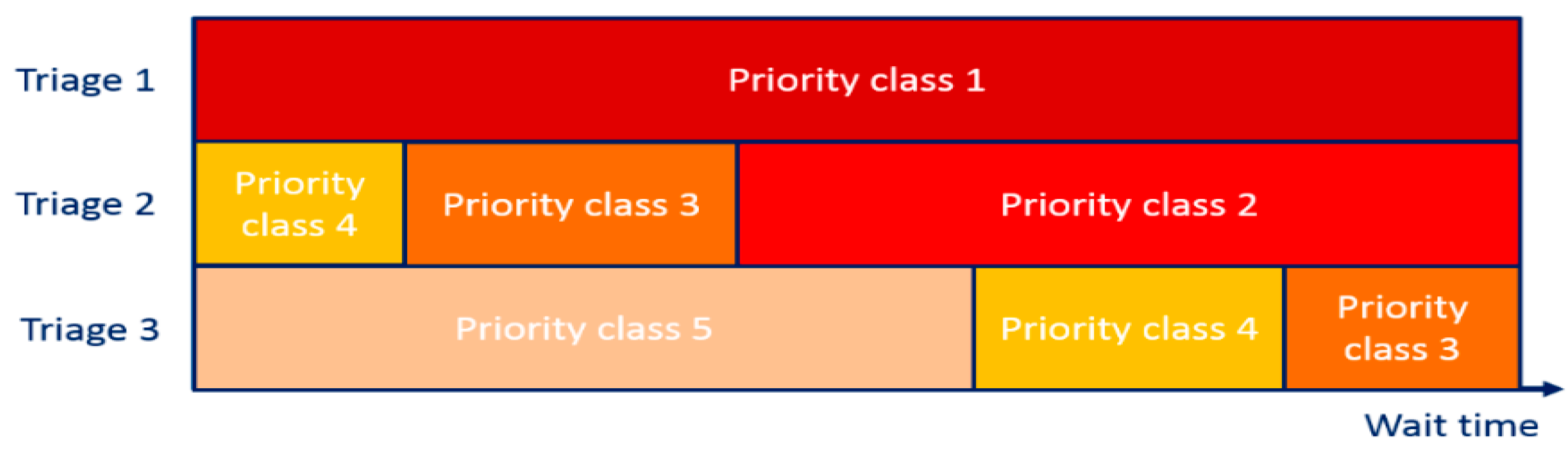
Furthermore, the authors in [49] analyzed the patient-routing behaviors of four ED decision-makers who were applying the CTAS. They estimated the cost of waiting for ED patients as recognized by the decision-makers, then derived policy implications, and made suggestions to enhance triage systems. They suggested considering risk factors and the level of congestion in ED when determining the patients’ waiting time. They also found that physicians are better suited to perform triage and prioritization tasks than the ED administrator/chief nurse, as this would improve certain metrics for operational performance such as waiting time. Furthermore, they suggested studying the possibility to enhance the CTAS by considering the delay-dependent priority rule, wherein Figure 4, they provided an example of the rule’s guidelines; the priority class is classified by the triage level and waiting time, and equal-priority patients are grouped into one priority class represented by the same color.
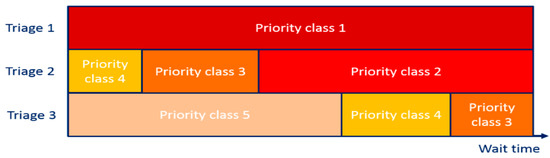
Figure 4.
Delay-based triage systems to prioritize patients [49].
In low- and middle-income countries, the ED faces many challenges, whether in the triage mechanism or the availability of medical equipment, and human resources. In addition, the lack of waiting rooms, which force patients to wait their turn outside the building under the sun for a period that may exceed 50 min. The study in [50] aimed to reduce the waiting time outside the triage room to be less than 30 min. The authors proposed several ideas to improve the triage and patient admission methodology, which include providing a triage training course for ED staff, eliminating redundant documentation, providing a uniform pre-printed triage form, reducing the turnover of triage’s nurses and ED health assistants, providing a color-coded wristband only for the critical condition patients, and rearrangement of the triage room.
The authors in [51] proposed a new priority queuing method to decrease delay time for high-priority patients in ED by estimating waiting times for multi-category patients. It depends on explicit expressions method to obtain the wait time when using the Markov queue, while the waiting time in the general queue is approximated using the isomorphism concept. When patients reach the ED, they will be treated according to the scheme in Figure 5. Patients are classified based on the severity of the disease and the patients with the highest priority are treated first, and the treatment of the patient is not interrupted until its completion even if a high-priority patient arrives.
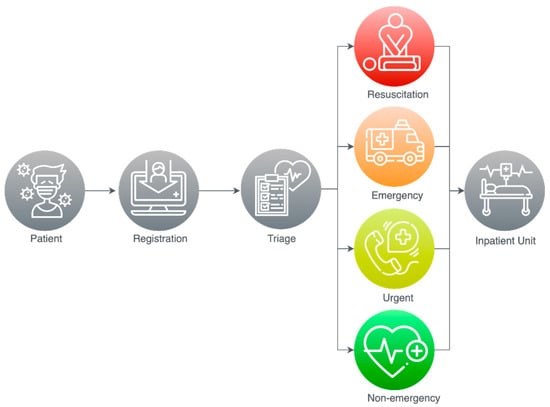
Figure 5.
The procedure followed in the ED.
A respectable number of important proposals have been reviewed in this section, where Table 2 summarizes our findings. However, these proposals have also failed to adapt to the COVID-19 situation as they were designed for general triaging.

Table 2.
Comparison of general proposed ED triage systems.
In the next section, we discuss studies that have addressed triage systems for classifying patients with COVID-19 in EDs.
2.2. ED Triage Systems for COVID-19
Hospitals and medical clinics are the most dangerous areas for transmission of infectious diseases such as COVID-19 as they are often crowded with patients. The infection spreads quickly in all hospital clinics, and is not limited to emergency departments. For example, when COVID-19 spread in China, it was discovered that 77.5% of the infected workers were working in general clinics [53]. Several studies are concerned with providing solutions to classify and triage patients to reduce their exposure to medical practitioners or other patients in hospital clinics. The authors in [54] and [55] discussed the need to provide preventive measures and develop appropriate plans to prevent and protect against the spread of COVID-19 in the dermatology departments. In [56], a structured remote triage system was implemented to counsel patients with neck and head cancer. The system calculates the patient’s risk rate to determine the appropriate way to provide counseling, whether remote over the phone or at the clinic.
The authors in [57] provided practical guidance to manage electromyography test requests during the COVID-19 pandemic. They proposed to classify patients’ electromyography referrals into three classes, (1) urgent, (2) non-urgent, and (3) possibly urgent. The authors in [58] provided guidelines for triaging heart disease patients during the COVID-19 pandemic.
As the spread of COVID-19 increased the demand for intensive care units (ICUs), a system of rapid resource assessment is required in hospitals. It is also important to classify patients with critical conditions such as ST-elevation myocardial infarction (STEMI) and assess their need for ICUs, as this will provide more resources to admit COVID-19 patients [59].
In this section, we focus on discussing the existing COVID-19 triage systems applied in EDs where we classify these systems into two groups according to where they are applied (1) Worldwide Triage systems and (2) Saudi Arabia triage system. Finally, we discuss the symptoms of COVID-19.
2.2.1. Worldwide Triage Systems
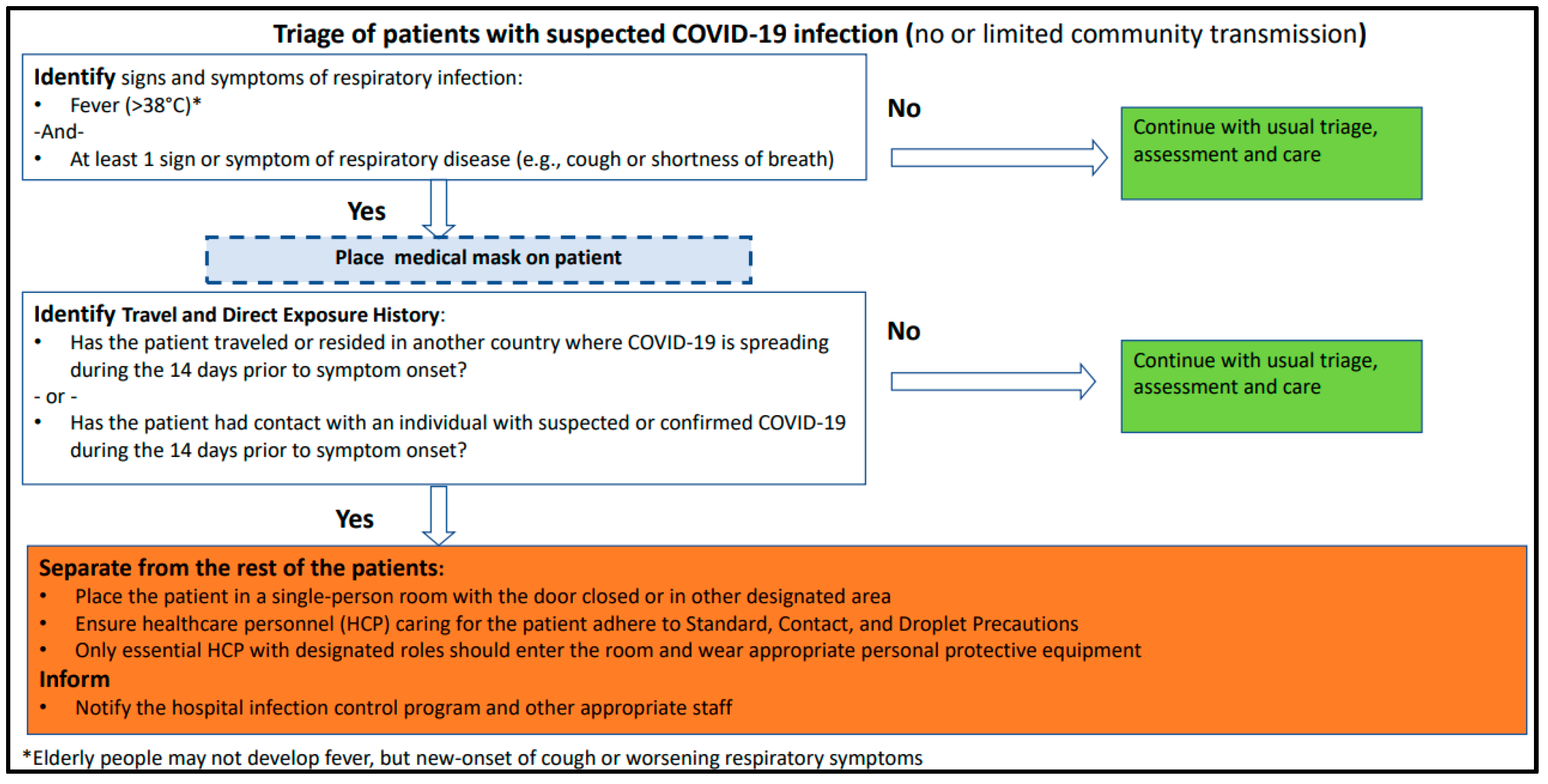
The Centers for Disease Control and Prevention (CDC) published a report [60] to help health workers protect themselves during patients triage process and gives guidelines for patients such as when they need to go to the healthcare facility, how they should inform healthcare providers if they suffer from any respiratory symptoms, wear face masks, clean their hands with water and soap, and preserve enough social distance over one meter. Several guidelines were proposed for protecting both patients and healthcare workers including communicating with patients ahead before they arrive to healthcare facility and set up of triage area for suspected cases. Moreover, they presented Triage Protocol for countries holding limited community transmission or even no community transmission as shown in Figure 6.
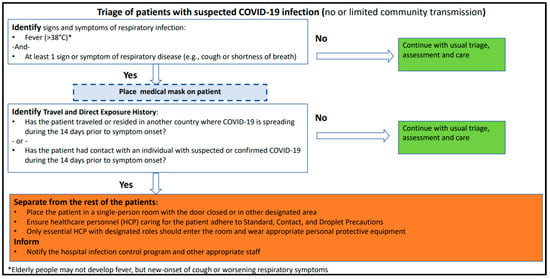
Figure 6.
Triage Protocol by CDC [60].
Authors in [61] provided guidelines for patients and healthcare personnel to support controlling the spread of COVID-19. The authors designed principles to enhance the ED’s triage system used by a triage nurse to classify the patients into five levels, as shown in Figure 1, depending on the “Emergency Severity Index” (ESI) triage method.
The authors in [62] analyzed and screened the case of 36 children suspected of having COVID-19 who had come to the fever clinic. They found that all children hospitalized at the isolation department had a fever, and about 71% of the patients presented cough, while having negative nucleic acid testing. They provided an improved evaluation questionnaire appropriate for early detection and controlling of children cases, where the children classified into three groups (High-risk, Medium-risk, Low-risk) relying on the epidemiological history score. This questionnaire is based on cumulative scores associated with specific symptoms to calculate the final score that is used as a guide to classify patients. However, the sample size was very small, and therefore further studies are required to determine the suitable triage method for children suspected of having COVID-19.
The authors in [52] proposed an algorithm as a framework for clinical triage to optimize patients’ triage, minimizes unnecessary clinician exposure, standardizes treatment, and maximizes adequate resource usage. The algorithm proposed five levels of patients’ acuity, each with a set of assumptions (pandemic conditions, in-person visits, vital sign assessment, clinical evaluation prior to disposition, and use by healthcare professionals). There were no measurements taken to validate the accuracy of the proposed algorithm; however, the authors hope that using this triage algorithm and guidelines would help frontline emergency staff dealing with COVID-19 patients.
2.2.2. Saudi Arabia’s Triage System
The Ministry of Health (MOH) issued a guidebook [63] titled “Hospital admission criteria for COVID-19 Pediatric patients Version 1.1” displaying great efforts in identifying strategies that contribute to effective prevention and optimal medical management of COVID-19 infections. Even though the clinical indicators of COVID-19 cases for children usually have low levels of severity compared to the clinical signs of adult patients, young children, especially infants, are at a higher risk of infection. However, the aim of the hospital admission criteria for COVID-19 pediatric patients is to determine the mechanism for admission and entry of COVID-19 infected children into health care facilities. This guide is for doctors who are treating and monitoring suspected or confirmed cases at all healthcare facilities. They recommend that any pediatric patient that meets the confirmed/suspected COVID-19 symptoms and high-risk standards be accepted [63].
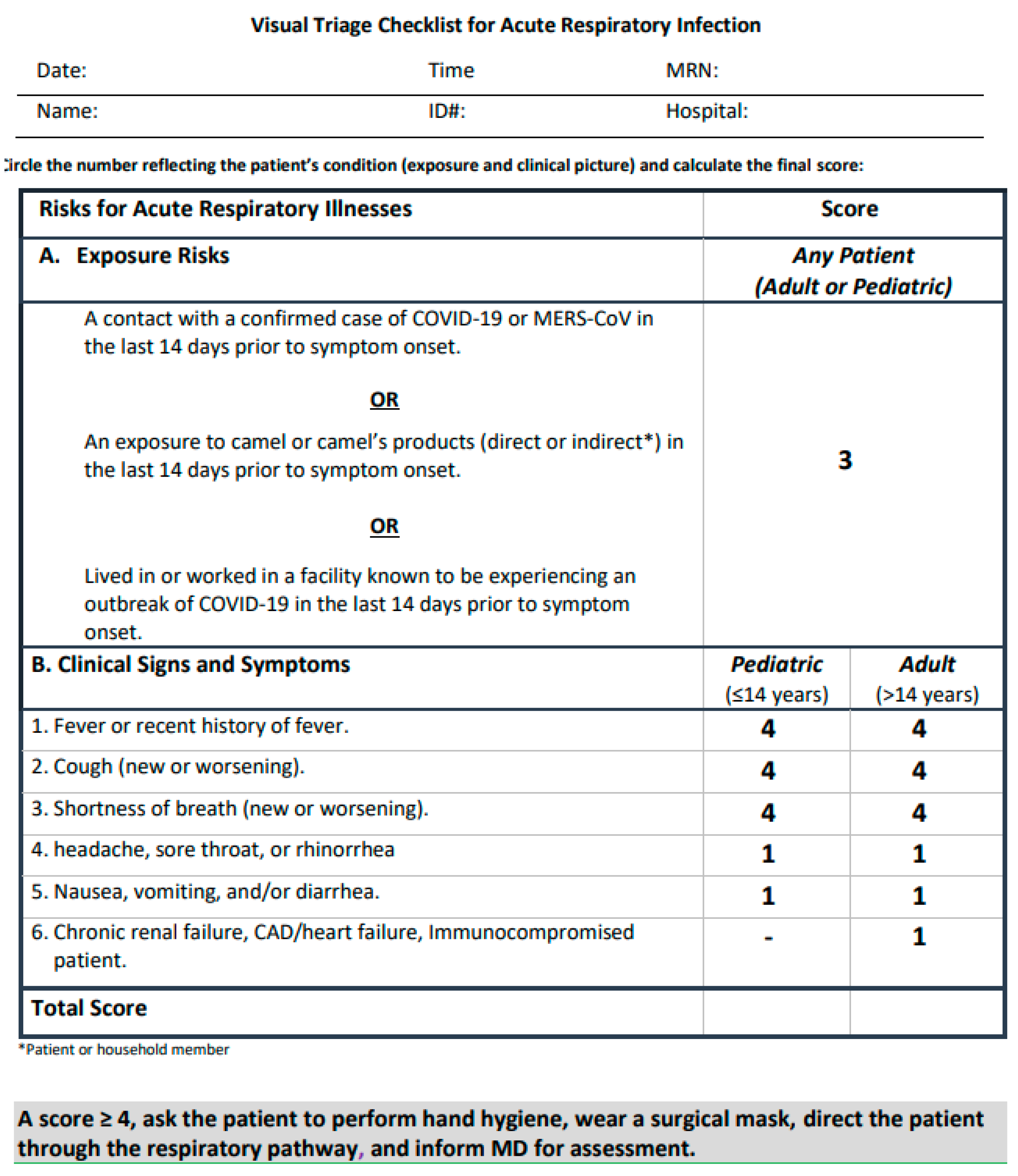
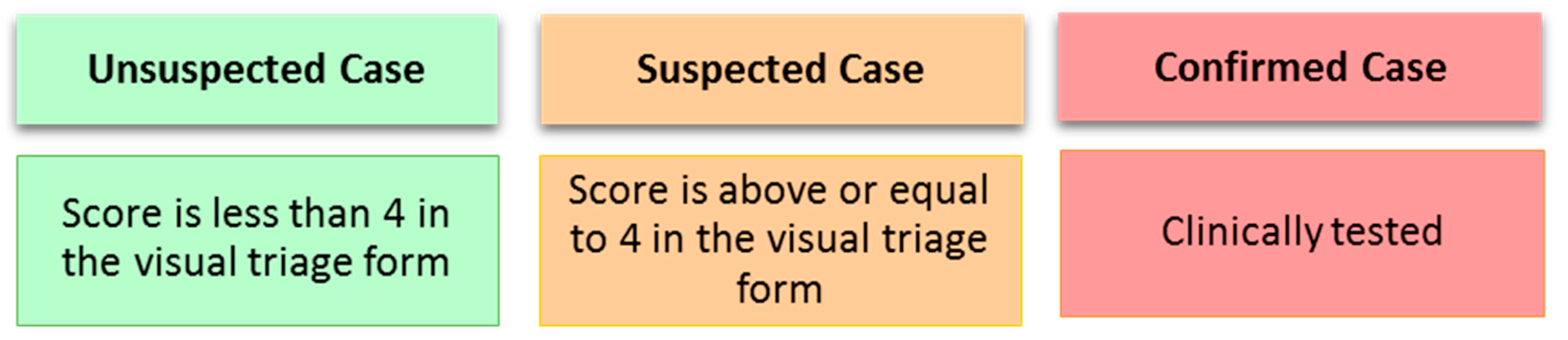
In [64], MOH has reported guidelines and instructions on Visual Triage Checklist for Acute Respiratory Infection (COVID-19/MERS-CoV) which shows a checklist following MOH and Weqaya guidelines. In this version of the report, they determined a scoring system for virtual triage system at EDs as shown in Figure 7 the general rule is when the total gain score is equal to or greater than 4, the patient must be directed through the respiratory pathway, and the medical staff is informed in order to perform an assessment.
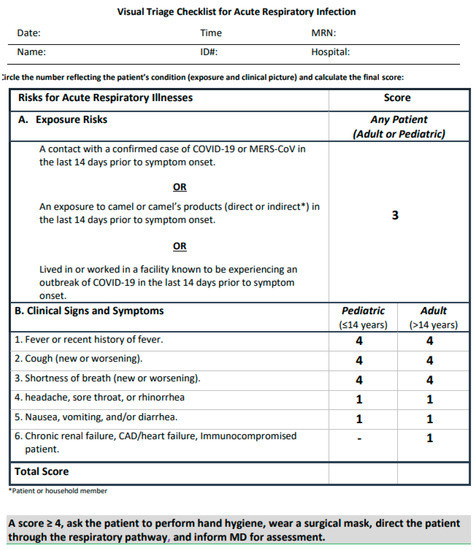
Figure 7.
Virtual Triage Checklist at MOH, version v1.3 [64].
In [65], the Saudi MOH published guidelines to optimize the usage of available medical resources and thus improving the response to the possible outbreak risks. The guidelines include restricted admission rules for the ICU unit to make it only available for patients that cannot be managed or treated with other resources. Generally, they considered three targeted queues or units which are the Critical Care Units, ED, and General wards. The rules for controlling COVID-19 ICU admissions are: (1) For patients requiring Invasive Mechanical Ventilation (IMV), the admission will be direct. (2) For patients requiring Non-Invasive Ventilation (NIV) for more than two hours or High Flow Nasal Cannula (HFNC), before admitting they should be assessed by a specialist. (3) Respiratory Distress patients will be admitted if resources are available based on the following: SpO2 > 92 or PaO2 > 65, high escalation of O2, with high difficulties in breathing (Tachypnea). (4) Other conditions related to several critical cases such as organ failure, hemodialysis, resuscitation, vasopressor, consciousness, heart issues, etc.
2.2.3. Symptoms of COVID-19 and Patient Classifications
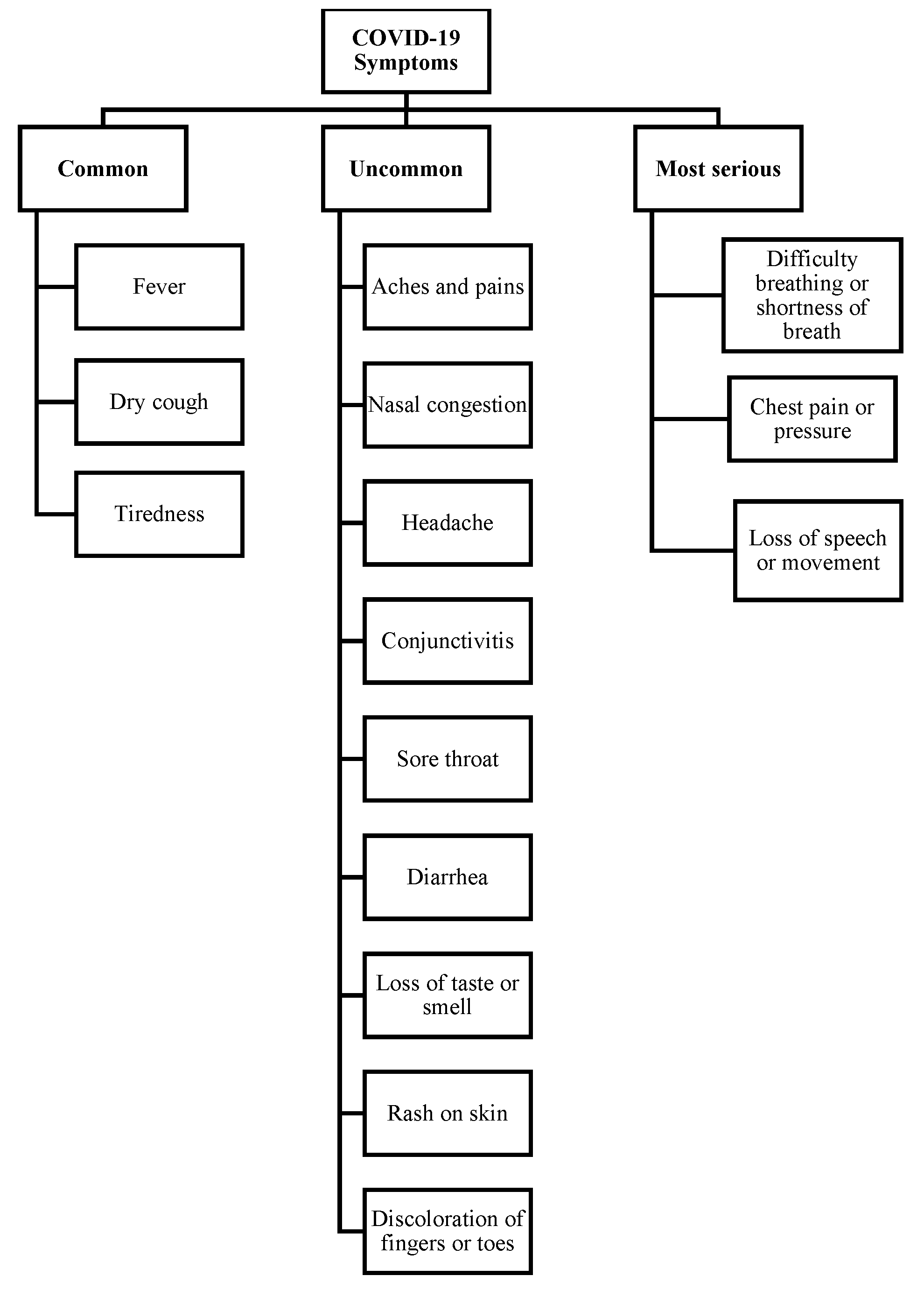
At the time of writing this paper, there are still high variations in reports on symptoms that could possibly identify COVID-19 cases. However, according to WHO [66], fever, dry cough, and tiredness are highly common symptoms in COVID-19 patients. Less common symptoms have been reported by the CDC [60] such as aches, headache, nasal congestion, conjunctivitis, diarrhea, sore throat, loss of smell or taste, skin rash, and discoloration of fingers or toes. Difficulty in breathing, chest pain, loss of speech, and difficulties in movement are the most critical symptoms that need urgent medical intervention and care [8].
A study [67] highlighted breathlessness and respiratory failure as respiratory symptoms of COVID-19. It also highlighted fever, muscle pain, headache, and confusion as constitutional symptoms. The Chinese Health Commission defined the surveillance of COVID-19 cases [68], which will be described later in this paper in Section 3.2.
The authors in [69] studied the changes in smelling and tasting in COVID-19 confirmed cases. The main problem with their study’s validity was a lack of enough samples to cover the factors that were studied, such as the geographical distribution of the samples and the disease’s subsequent course. However, their report covered the majority of the main symptoms that can be used to help select symptoms for COVID-19 diagnosis, as well as other studies. They primarily reported the prevalence of some of the COVID-19 symptoms listed in Table 3. In terms of symptom frequency, we listed the percentage found in this study as well as other frequencies discussed in other studies [70,71,72,73,74,75,76].

Table 3.
COVID-19 symptoms frequency.
The authors in [82] show that the average rate of skin disease symptoms for confirmed COVID-19 patients varied among the studies they reviewed, where the initial studies were conducted in Wuhan, China, on a group of 1099 confirmed COVID-19 cases reported a lower rate of cases presenting symptoms of skin diseases as it was only 0.2%. While the maculopapular rash observed in 47% of Spanish COVID-19 cases were over 50% of those said cases, they presented severe levels of pruritus for around nine days. As previously stated, the authors reviewed several studies related to skin disease symptoms of confirmed COVID-19 patients, and they believe that the difference in ratios between studies is due to the lack of interest in conducting skin tests on patients, especially those who are outside of the EDs. The study also indicated that skin related symptoms of COVID-19 could be helpful in initial diagnosis, triaging confirmed cases, and determining the severity level.
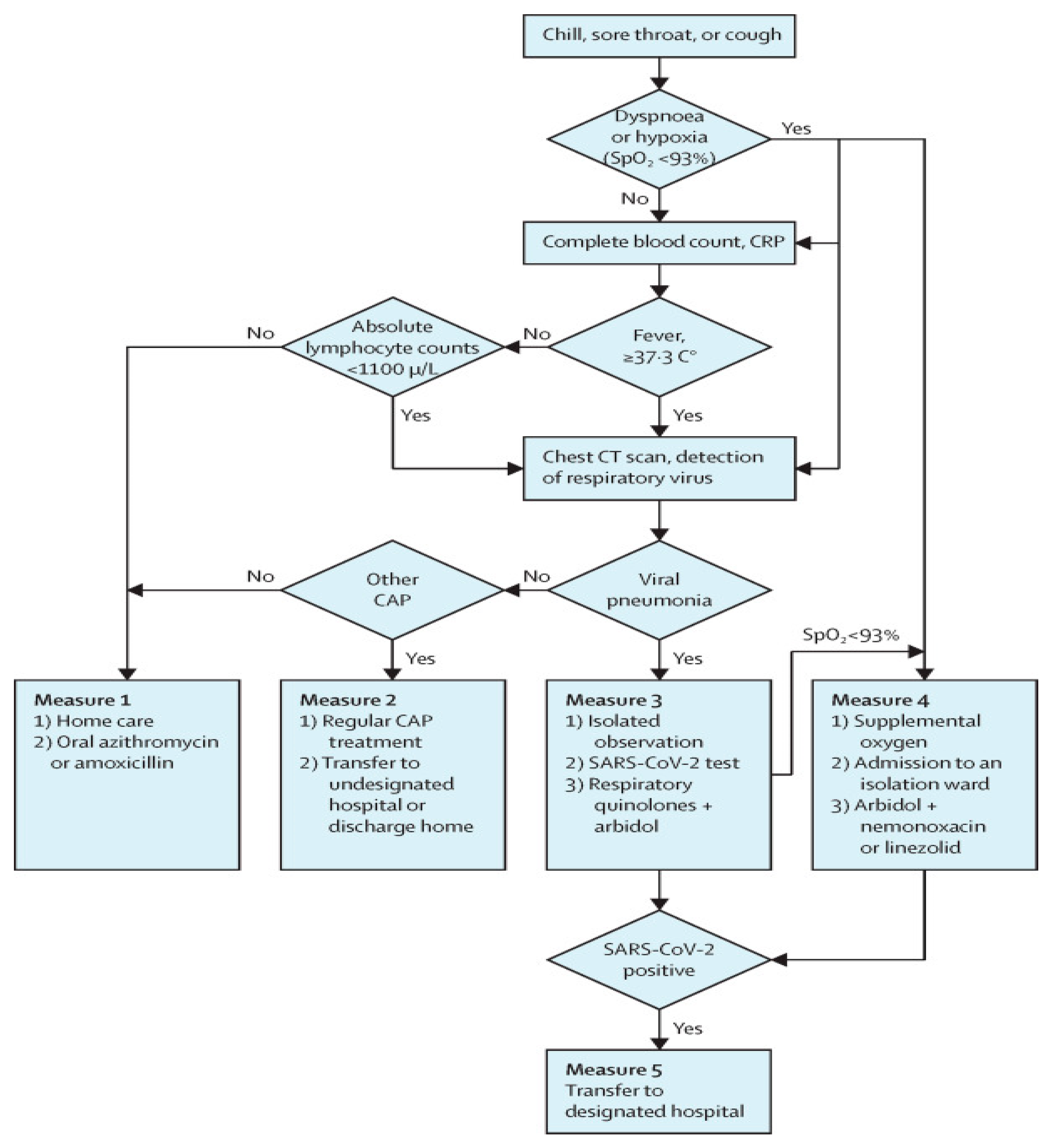
The authors in [83] developed a method for screening and classifying patients in adult fever clinics based on symptom measures, as shown in Figure 8. However, their methodology may not be applicable in other hospitals, because the proposed algorithm’s implementation is dependent on the ability to perform the medical tests that it employs.
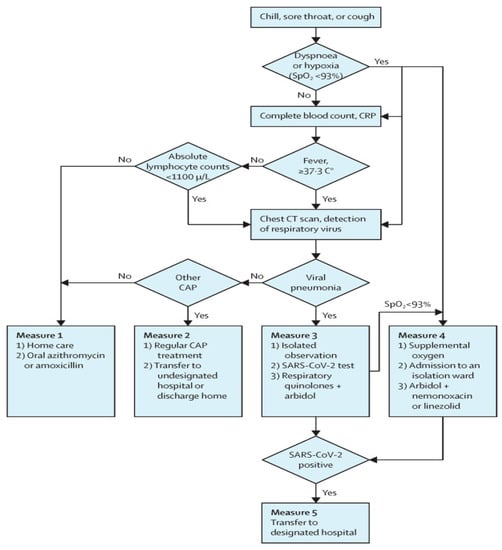
Figure 8.
A flowchart of COVID-19 treatment in in Wuhan fever clinics [83].
COVID-19 symptoms are similar to those of other virus-related upper respiratory diseases, which share symptoms such as fever, cough, tiredness, and breathing difficulties. To determine the level of risk and the appropriate treatment for each patient, said symptoms must be diagnosed [1].
Based on the studies discussed in this section, we classified COVID-19 symptoms in Figure 9. However, more research and studies are required to accurately identify COVID-19 symptoms and the level of risk each symptom poses to a patient.
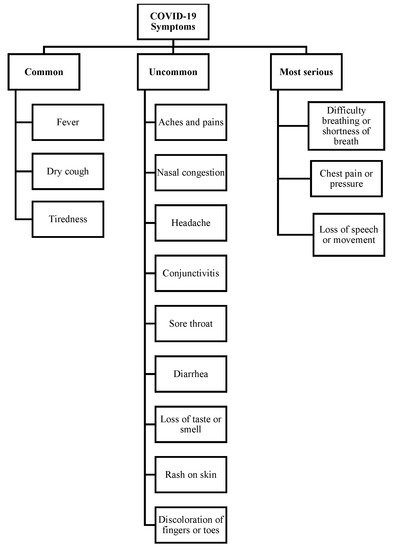
Figure 9.
COVID-19 Symptoms.
3. Evaluation and Discussion
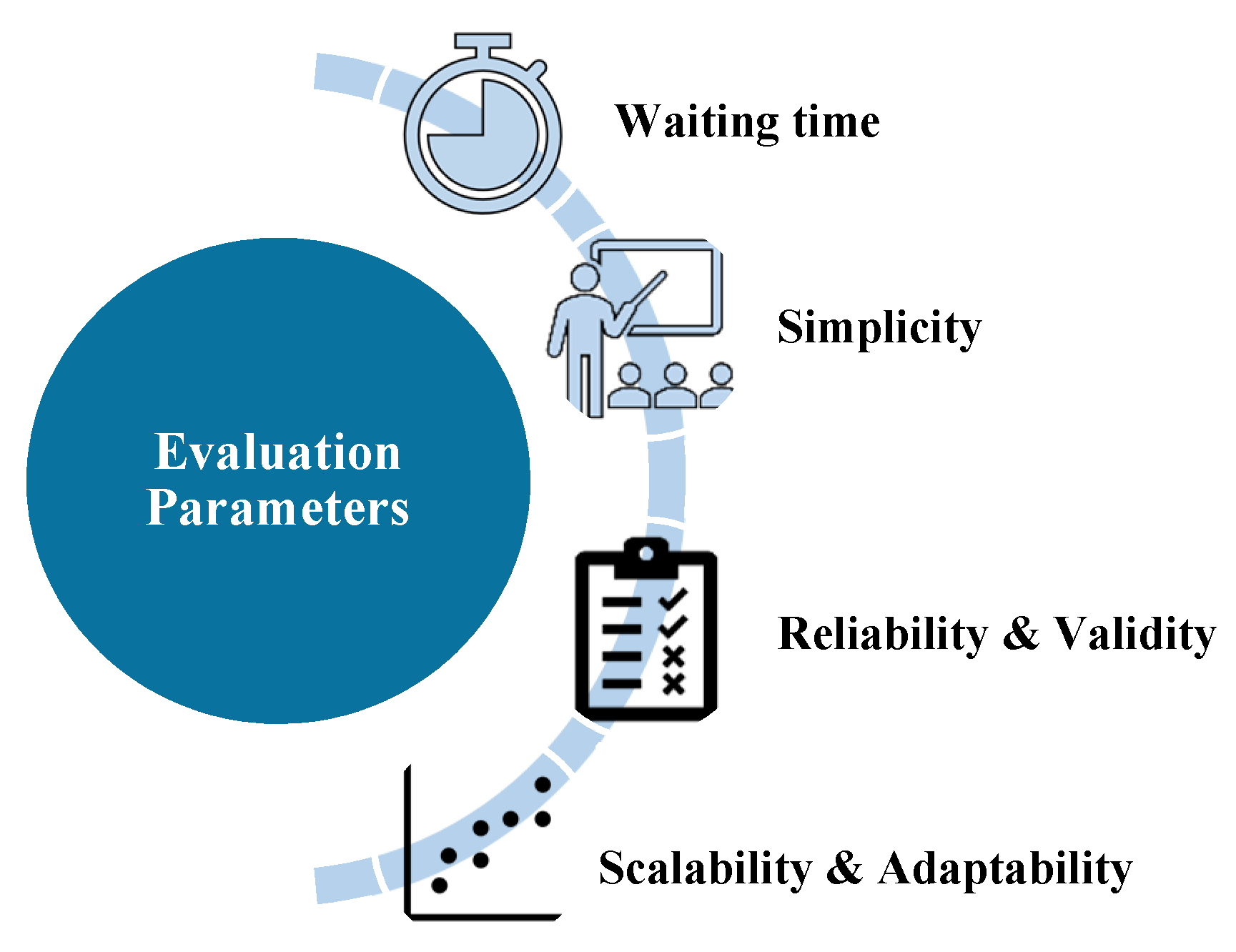
According to the findings of this paper’s research, there are numerous challenges that cannot be addressed by the current or proposed triaging systems. As a result, we identified several parameters, shown in Figure 10, that we recommend taking into account when designing an ED triage system. These parameters will be discussed in the subsections that follow.
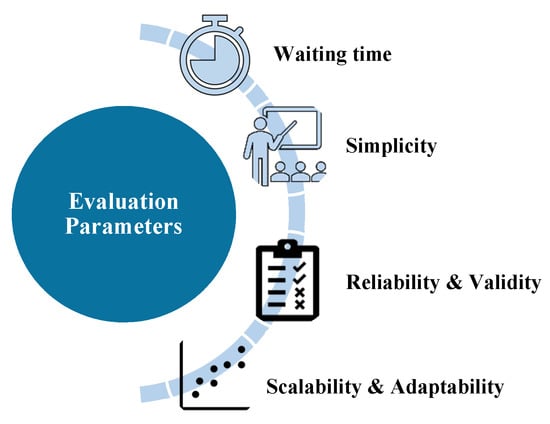
Figure 10.
Triage system evaluation parameters.
3.1. Waiting Time
As risk factors and ED congestion continue to rise, patient wait times are increasing [49]. The majority of studies have attempted to shorten the waiting time for patients with severe cases, while those at lower risk may deteriorate during the wait.
There are several factors [12] that affect the waiting time, including the triage nurse’s understanding of the system, the availability of medical staff and resources, the initial diagnosis of the patient’s condition, and the possibility of excluding non-emergency cases early before they reach the EDs.
3.2. Simplicity
To reduce the rate of errors, the triage system for EDs should be simple and easy to understand. In addition, the number of triage categories should be reasonable; as shown in Figure 1, the most common international systems have five levels, whereas the proposed COVID-19 systems have fewer levels. For example, the COVID-19 approaches reviewed in this paper use different criteria for classifying patients, as shown in Table 4, Table 5, Table 6 and Table 7, To set the best possible parameters into the triage system, these criteria should be reasonable in terms of number, as well as simple to understand and flexible. Furthermore, educating and training nurses on the triage system’s mechanism contributes to the system’s success [43].

Table 4.
Classification criteria of COVID-19 patients in approach 1.

Table 5.
Classification criteria of COVID-19 patients in approach 2.

Table 6.
Classification criteria of COVID-19 patients in approach 3.

Table 7.
Classification criteria of COVID-19 patients in approach 4.
3.3. Reliability and Validity
In EDs, the performance and accuracy of the triage system results vary depending on the spatial and temporal conditions. For example, the authors in [86] studied the results of ED waiting time after implementing the CTAS system in the ED of the “King Faisal Specialist Hospital and Research Center”. They found that physicians evaluated the wait time for category I patients which matched the time goals for CTAS, but this was not the case for the other four triage categories. As a result, we suggest that the triage system be reviewed on a regular basis under a variety of conditions in order to ensure its accuracy and prepare for future developments.
Most studies, such as [46,49,51], use wait times as a measure to evaluate this factor, while others, such as [45], use a variety of metrics, including Length of Stay (LOS), Time-to-Bed (TTB), throughput, percentage of late patients, time in ED, and the risk of delaying patients.
3.4. Scalability and Adaptability
The aging population and disasters such as the spread of COVID-19 [44] are expected to increase the number of patients in EDs. As a consequence, the triage method should be scalable and versatile enough to deal with several scenarios, including COVID-19 cases. To achieve this, we suggest considering the following:
- The majority of triage operations should be conducted by an automated system to minimize the rate of error and time spent by the triage nurse using conventional approaches. Table 2 shows that the majority of the suggested solutions automate the triage processes.
- Not all patients who come to the EDs are required to be admitted to these departments. Early classification of patients’ severity status will aid in reducing ED congestion, particularly in times where infectious diseases such as COVID-19 is spreading. Therefore, we recommend that the triage system be linked to a remote diagnostic system such as the systems proposed in [44,87], through which the patient’s condition is evaluated to determine the severity level upon which he will be admitted to the ED or transferred to other care departments.
- New diseases may emerge that require specific patient triaging criteria, which may change over time. For example, the COVID-19 pandemic, which is an infectious disease that necessitates rapid classification, the WHO has had to develop a specific system to classify suspected COVID-19 cases. From Table 3 as well as the discussion in Section 2.2.3, we can note that symptom variety and changeability play a big role in classifying patients. Therefore, we recommend that the system be flexible, scalable, and adjustable so it can easily and quickly adapt to changing conditions.
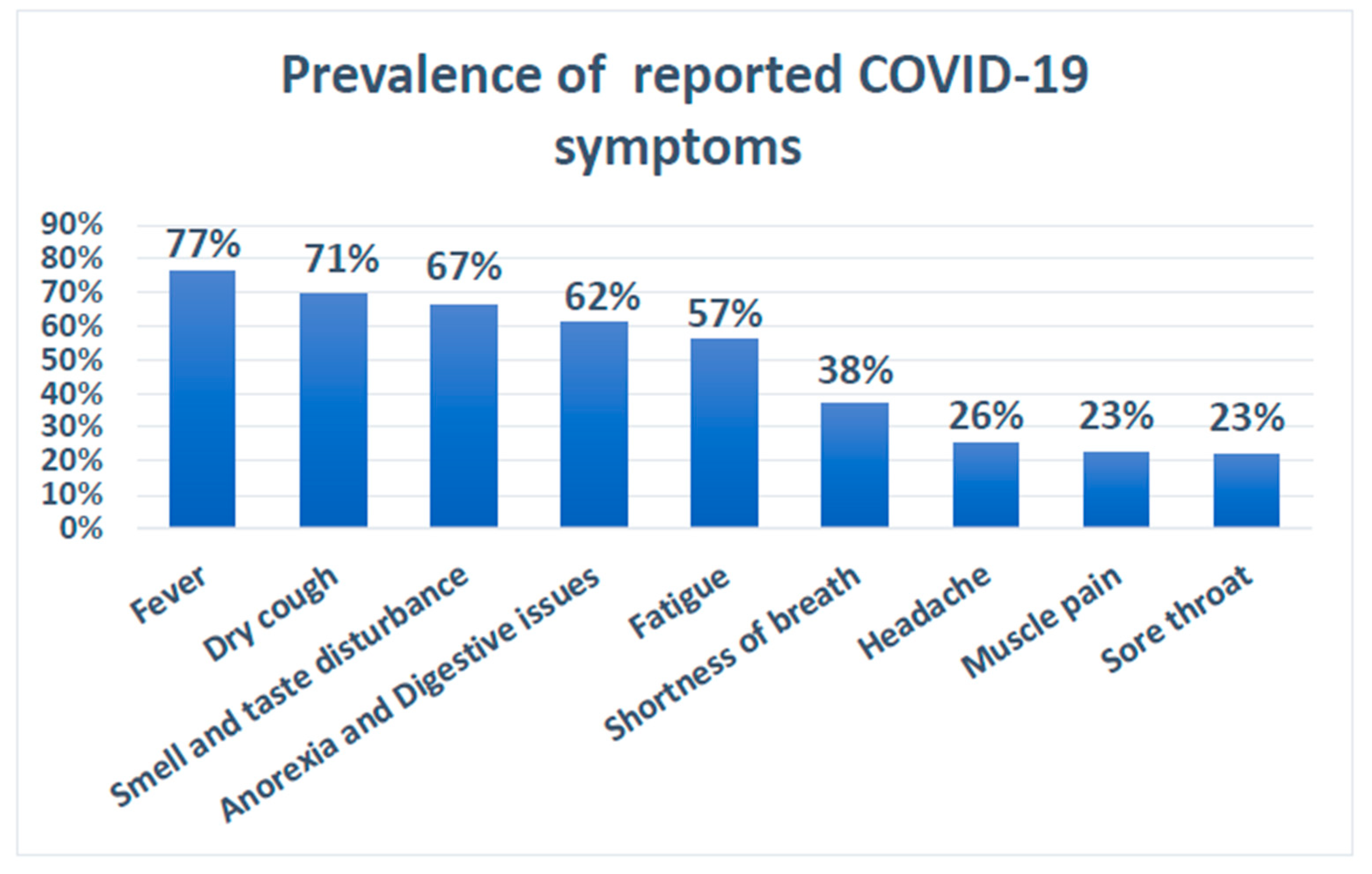
3.5. Observations
Several studies [69,76] examined datasets from hospitalized COVID-19 patients to determine the prevalence of some COVID-19 symptoms. As shown in Table 3 in Section 2, the prevalence varied across these studies. Furthermore, Figure 11 shows the average prevalence measured by using the median of the observed prevalence and considering the minimum and maximum reported values. Fever, dry cough, smell and taste dysfunction, digestive issues, and fatigue are the most common COVID-19 symptoms, with an estimated prevalence of over 50%. However, such findings do not represent or assert a medical fact on COVID-19 symptoms because it necessitates standard review and confirmation with sufficient data.
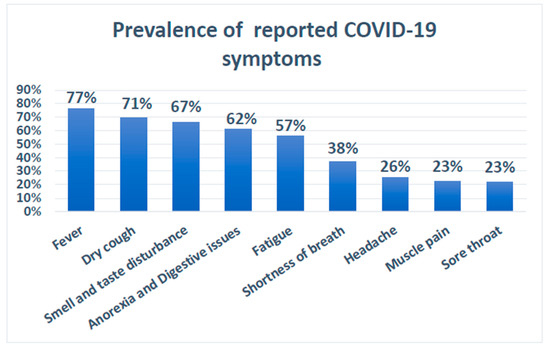
Figure 11.
Prevalence of reported COVID-19 symptoms.
The majority of the presented methods for general ED triaging primarily proposed improvements for prioritizing patients based on estimated waiting time [44], estimated duration of service [46], First Come First Serve (FCFS) [45,49,51], and risk level [47,50]. Waiting time and service duration are critical factors in reducing ED overhead, optimizing resources usage, and saving patients’ lives. However, in the case of a pandemic such as COVID-19, more criteria should be used in the triage systems to capture the outbreak’s considerations and characteristics. For example, among such parameters are the availability of special medical services and devices, effectiveness of the remote triaging through communication and mobile technologies, and the accuracy of patients’ classification based on vital signs and symptoms. The key problem with such general e-Triage systems is that they were developed to manage general ED cases and situations. As a result, further research is required to validate their usage during outbreaks.
Majority of the ED triaging studies proposed for COVID-19 rely on subjective measurements [54,55,56,57,58,61,63,65]. Just a few studies [59,62,64] use a scoring system to assess admission or severity level of patients. While scoring-based triage systems are deterministic, the accuracy of the involved rules must be validated using actual datasets obtained from EDs. Another discovered finding is that few of the reviewed studies were primarily planned for general emergency departments [61,64]. Table 8 summarizes the main findings from the proposed COVID-19 triage systems.

Table 8.
Proposed studies on COVID-19 triage systems.
Regarding the reported symptoms and classification criteria used with COVID-19 triaging systems, we discovered that the symptoms vary from source to source, owing to the fact that the disease itself is not well understood yet, of both old and new types that can manifest in the human body and cause a variety of clinical manifestations. According to Table 3 and Table 4, and Figure 11, the variety and changeability of symptoms have a significant role in classifying patients. As a result, there is a need for a triage method that is adaptable in terms of implementing various interventions as well as different thresholds for making decisions on patient classification at EDs. Moreover, the majority of the patients’ classification criteria are variable and subjective. The variations and subjectivity of the used parameters may be attributed to several factors, including the complexity of developing such triage systems based on available information about the pandemic, the level of risk in the countries and regions, the difficulty of implementing current scoring general triage systems, the volatility of pandemic situations, and rapid overhead on ED during the pandemic.
4. Recommended Solutions
Based on the literature review and gap analysis we made in the previous sections, we will provide a list of recommendations to address issues in the e-Triage system considering COVID-19 in the following subsections.
4.1. Electronic Triage System
Based on our findings, we recommend the use of an electronic system to reduce overcrowding and overhead in the EDs by remotely and electronically assessing patients’ condition to either accept or reject their admission to the ED. We suggest considering the following features when designing an e-Triage system.
- Since the COVID-19 pandemic case is not stable and many things arise while addressing the problem, there is a need for an adaptive system that allows resetting its parameters in a flexible and quick way.
- To reduce overcrowding in Eds, which results in the possible reduction of infection spreading, we recommend that the system provide a mechanism to receive patients’ requests remotely instead of personally coming to the ED.
- The system should have an expert model and decision support layer that guides the hospital in filtering requests and managing patient waiting time.
4.2. Electronic Medical Record
We recommend using technologies such as database management systems to maintain medical records and disease history. This will help in retrieving the required data when needed quickly and with high accuracy instead of asking the patient for such information.
4.3. Medical Sensors Devices
We recommend using medical sensors to recognize the patient’s symptoms remotely rather than asking the patient to answer several questions about symptoms they feel may not give accurate results. In addition, it will also reduce the treatment time as there is no need to check for specific symptoms by the triage nurse in the ED.
With that in mind, there is a need to find a flexible way to link sensors to symptoms of COVID-19; hence we suggest having an adjustable scoring system based on symptoms used in the diagnosis of COVID-19.
Therefore, to meet criterion 3 and 4 of the MOH approach [65] which are related to oxygen issues, we recommend a mobile application connected to health monitoring sensor devices to provide sensor readings of patients’ oxygen levels and other clinical signs.
4.4. Scoring System and Classification Criteria
We have studied a respectable number of triage systems that were found in the literature review, to highlight the admission criteria and the criteria that can be used to estimate the severity level of admitted COVID-19 patients.
4.4.1. Admission Criteria for COVID-19 Patients
To estimate COVID-19 cases of remote patients before their arrival at a health facility or before hospitalization, we recommend following approach 2 given in Table 5. Moreover, we recommend adding a third category that represents those with little to no symptoms that are major or common for COVID-19. Figure 12 shows the suggested categories along with the possible scoring approach adapted from MOH [38] presented in Figure 7.
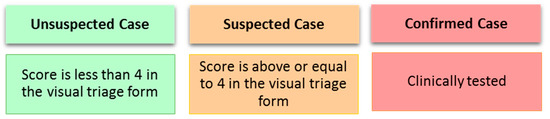
Figure 12.
Classification criteria of COVID-19 for remote patients.
Based on the above literature review and the locally implemented approach shown in Figure 7, we do suggest the following score-based criteria presented in Table 9 as a recommended admission approach that can be applied locally in Saudi Arabia. Moreover, regarding the admission criteria, we recommend establishing conditions that have some form of flexibility and adaptability to fit the nature and progression of the disease. Additionally, the capabilities of the country’s facilities should also be taken into consideration. For example, we do recommend the following adapted conditions for the locally adopted criteria in Saudi Arabia [65].

Table 9.
Recommended admission scored-based criteria for COVID-19.
- The first criterion is that if the patient requires invasive mechanical ventilation. To satisfy and determine this condition in our proposed system, it is required from the patient who is contacting the hospital through the mobile application to determine if they have a breathing problem. The ED needs to contact the patient and conduct a quick interview to ensure the existence of such condition. Considering the available resources, this condition is enough to accept a patient regardless of the other symptoms whether they are related or not to COVID-19.
- The second criterion is that if the patient requires NIV for more than two hours or HFNC. To ensure accuracy when determining such a condition, the ED can call and ask more questions to determine if the patient is in need for such treatments. Therefore, criterion 1 and 2 need the intervention of a specialist from the ED department to make a final decision on the case.
4.4.2. COVID-19 Severity Level-Based Criteria
Using approach 1 summarized in Table 4, approach 4 summarized in Table 7, and the suggested local approach presented in Table 9, we propose a set of criteria that combines the two approaches so that they correlate with the calculated scores based on measured symptoms. Accordingly, Table 10 reflects such updates where the points given for each level can be adjusted based on knowledge of the disease behavior and its symptoms. Given that the recommended scoring system in Table 10 is only for the inpatients considered to be COVID-19 patients. The idea is to have a COVID-19-based e-Triage system that can give a severity level based on only the taken clinical signs and symptoms. Thus, the other factors including exposure risks are excluded from the scoring system.

Table 10.
Proposed severity level-based classification criteria for COVID-19 patients.
Based on the visual triage checklist provided by MOH in [38], the main symptoms of COVID-19 are fever, cough, and shortness of breath, hence each of these symptoms was mapped to a score of 4, which is the highest possible score for a single symptom in the triaging checklist. The remaining symptoms are considered minor due to the minimum assigned score of 1. Therefore, in Table 10, we propose a severity level-based scoring system which categorizes a patient into one of four possible levels: mild, moderate, severe, or critical.
The mild level, as described in Table 4, represents the lowest severity level and thus would not involve any of the three main symptoms adopted in [38]. Therefore, we excluded the three main symptoms from the total scores and only considered the minor symptoms, resulting in a total score that ranges from 1 to 3.
The moderate level, as described in Table 4, is a level involving patients with moderate pneumonia. To ensure this level aligns with the scoring approach adopted in [38], we recommended considering only one of the main symptoms as an indicator for this level of severity. This results in a score that may range from 4 (having one of the main symptoms) to 7 (having one of the main symptoms and any of the minor ones).
As for the severe level, we recommended considering only two of the main symptoms as it does not involve respiratory failure as described in Table 4. Thus, the suggested possible scores for this level fall within a range of 8 to 11. Finally, the critical level, which is the highest severity level, involves all three main symptoms, hence resulting in a cumulative minimum score of 12 for this level.
Moreover, to further support our proposed scoring approach presented in Table 10, we used a dataset containing data collected from COVID-19 patients admitted to King Fahad University Hospital (KFUH). However, to validate the recommended scoring approach, there is a need to work on a sufficient number of samples collected from COVID-19 patients at EDs. The data should contain a variety of samples and symptoms related to the classification levels. It is worth noting that datasets can be used to design and validate the proposed ED scoring-based triage system, but the aid of medical professionals and experts is still quite necessary. Furthermore, although we analyze applying our proposed scoring system to the data collected from KFUH, the extent of our analysis is constrained by the percentage of patients in the data who present key symptoms of COVID-19. Therefore, this analysis may not necessarily constitute as a validation of the approach.
The dataset collected from KFUH consists of 243 records representing COVID-19 cases. After preprocessing and filtering out records with missing or invalid values, the remaining samples were 177 samples. Table 11 shows the description of the used dataset where we considered the features that could be mapped to our study. The processed dataset holds 43 samples classified with Target of 1, Group 1, representing the recovered cases at the time of collecting the data. The rest of the samples, 134 samples, are classified as Target of 2, Group 2, representing the most critical cases that are either deceased or active at the time of collecting the data.

Table 11.
KFUH dataset description.
Table 12 shows the general statistics of the two groups considering the features or symptoms that contribute to our study. Based on the statistical results presented in Table 12, it is obvious that the most significant factors/symptoms impacting the classification of the studied samples are fever, cough, and shortage of breath symptoms. Thus, we have considered them as the main factors used in this study to decide on the severity level of COVID-19 cases.

Table 12.
Statistical results of the two groups constituted the used dataset.
Considering the first group of samples, Group 1, it holds only 43 samples and thus we have excluded its statistics in this study. However, we relied on the second group, Group 2, which holds 134 samples representing only active or deceased cases. We believe that Group 2 is more suitable to decide about the most critical levels (Severe and Critical) due to the type of the samples in Group 2 (active and deceased cases) as well as its statistics showed that all the samples involve at least two of the three main factors.
Table 13 shows the statistics for Group 2 considering how many factors out of the three main factors being involved in the samples (two factors or three factors). Based on the statistical results presented in Table 13 and the recommendations presented in Table 9, we recommend that the severe level can involve two of the three main factors with a minimum accumulated score of eight points. On the other hand, the critical level can involve all the three main factors with a minimum accumulated score of 12 points.

Table 13.
Statistical results for Group 2.
Finally, regarding the mild and moderate levels, we recommend using only one of the three main factors as an essential criterion, in addition to the other non-main factors, to assign moderate level. Thus, the moderate level will have an accumulated score of [4 to 7]. On the other hand, the mild level, the lowest level, can be determined based only on the non-main factors with a range of [1 to 3] as shown above in Table 10.
5. Conclusions and Future Work
Due to the contingent nature of the COVID-19, long waiting times and interaction of the COVID-19 patients will increase the risk of the spread. Therefore, overcrowding in emergency departments need to be reduced to control the outbreak. Different triage systems have been proposed to classify patients into different levels based on the severity of their health condition. In this paper, number of these systems are reviewed, and the taxonomy of patient classification approaches is provided. The severity of a patient’s health condition can be determined by the pathological symptoms. Therefore, in this paper, a comprehensive survey was conducted to determine the symptoms of COVID-19 that were found in the literature review. It was noted that there are many challenges that cannot be addressed in the proposed triaging systems. However, several parameters were identified such as waiting time, simplicity, reliability, validity, scalability, and adaptability, and were recommended while designing an e-Triage system for EDs. Moreover, we recommend the use of an electronic system to reduce overcrowding and overheads in EDs by remotely and electronically assessing patients’ condition to either accept or reject their admission to the ED. Furthermore, we proposed a severity level classification approach of COVID-19 cases as a part of the recommended e-Triage system.
Having said that, our study carries some limitations, scoring systems, whether electronic or paper-based, solely based on the patient’s subjective answers and experience of the triaging personal especially that most of EDs depend on a nursing staff to do this task which may affect the accuracy of data entered. Similarly, many external factors might interfere with applicability of such approaches; limited resources availability especially in rural areas, numbers of patients, and ED design play a major factor in the success or failure of e-triaging systems. Thus, there is a need to conduct a validation on the recommended scoring-based triage systems using real patient’s data with enough samples considering the quality and statistics of the data. Moreover, there is always a need to update the findings on relevant symptoms for such outbreaks. Additionally, the symptoms themselves are highly variability from one another. As the disease itself is not well studied yet with old and current variants, which can manifest in the human body with different clinical manifestations. Finally, one of the limitations in this work is that the presented recommendations regarding enhancing admission criteria with scoring-based system were given mainly based on the triage system adopted in Saudi Arabia. Thus, more evaluation and analysis are required to generalize the recommended approach to be worldwide.
Author Contributions
Conceptualization, F.A., A.A. and S.A.; methodology, F.A.; software, N.A. and I.U.K.; validation, N.I., F.S. and A.A.; formal analysis, F.A., S.A. and N.I.; investigation, M.A.; resources, N.A. and I.U.K.; data curation, M.A.; writing—original draft preparation, F.A., S.A. and N.I.; writing—review and editing, H.A., Y.A. and D.A.; visualization, H.A., Y.A. and D.A.; supervision, F.A. and A.A.; project administration, N.I.; funding acquisition, A.A. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by King Abdulaziz City for Science and Technology (KACST) grant number 5-20-01-070-0017, which is a part of the COVID-19 Research Grant Program.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Imam Abdulrahman Bin Faisal University (IRB: 2020-09-189, 28 June 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data was obtained from King Fahd University Hospital and are available from the authors with the permission of King Fahd Hospital of University.
Acknowledgments
We acknowledge Amal Alsulaibikh from King Fahd University Hospital for providing comments and revision on the recommended solutions presented in this paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Chavez, S.; Long, B.; Koyfman, A.; Liang, S.Y. Coronavirus Disease (COVID-19): A primer for emergency physicians. Am. J. Emerg. Med. 2020. [Google Scholar] [CrossRef]
- White, D.B.; Lo, B. Mitigating Inequities and Saving Lives with ICU Triage during the COVID-19 Pandemic. Am. J. Respir. Crit. Care Med. 2021, 203, 287–295. [Google Scholar] [CrossRef]
- Adiga, A.; Dubhashi, D.; Lewis, B.; Marathe, M.; Venkatramanan, S.; Vullikanti, A. Mathematical Models for COVID-19 Pandemic: A Comparative Analysis. J. Indian Inst. Sci. 2020, 100, 793–807. [Google Scholar] [CrossRef]
- Morley, C.; Unwin, M.; Peterson, G.M.; Stankovich, J.; Kinsman, L. Emergency department crowding: A systematic review of causes, consequences and solutions. PLoS ONE 2018, 13, e0203316. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.-K.; Wang, C.-C.; Lin, M.-C.; Kung, C.-T.; Lan, K.-C.; Lee, C.-T. Effective strategies to prevent coronavirus disease-2019 (COVID-19) outbreak in hospital. J. Hosp. Infect. 2020, 105, 102–103. [Google Scholar] [CrossRef]
- Iacobucci, G. Covid-19: Emergency departments lack proper isolation facilities, senior medic warns. BMJ 2020, 368, m953. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Tang, K. Combating COVID-19: Health equity matters. Nat. Med. 2020, 26, 458. [Google Scholar] [CrossRef] [PubMed]
- Afilal, M.; Yalaoui, F.; Dugardin, F.; Amodeo, L.; Laplanche, D.; Blua, P. Forecasting the Emergency Department Patients Flow. J. Med. Syst. 2016, 40, 175. [Google Scholar] [CrossRef]
- Carmen, R.; Van Nieuwenhuyse, I.; Van Houdt, B. Inpatient boarding in emergency departments: Impact on patient delays and system capacity. Eur. J. Oper. Res. 2018, 271, 953–967. [Google Scholar] [CrossRef]
- Aboagye-Sarfo, P.; Mai, Q.; Sanfilippo, F.M.; Fatovich, D.M. Impact of population ageing on growing demand for emergency transportation to emergency departments in Western Australia, 2005–2020. Emerg. Med. Australas 2016, 28, 551–557. [Google Scholar] [CrossRef]
- Laudicella, M.; Martin, S.; Donni, P.L.; Smith, P.C. Do Reduced Hospital Mortality Rates Lead to Increased Utilization of Inpatient Emergency Care? A Population-Based Cohort Study. Health Serv. Res. 2017, 53, 2324–2345. [Google Scholar] [CrossRef] [PubMed]
- How Long Is Too Long to Wait in the Emergency Department? Southeastern Med Hospital—Cambridge Ohio. Available online: http://www.seormc.org/blog-archive/369-how-long-is-too-long-to-wait-in-the-emergency-department.html (accessed on 1 June 2020).
- Afilal, M.; Amodeo, L.; Yalaoui, F.; Dugardin, F. Forecasting Patient Flows into Emergency Services. In Hospital Logistics and e-Management; Wiley: Hoboken, NJ, USA, 2019; pp. 85–143. [Google Scholar]
- Jones, S.S.; Thomas, A.; Evans, R.S.; Welch, S.J.; Haug, P.J.; Snow, G.L. Forecasting Daily Patient Volumes in the Emergency Department. Acad. Emerg. Med. 2008, 15, 159–170. [Google Scholar] [CrossRef]
- Bashshur, R.; Doarn, C.R.; Frenk, J.M.; Kvedar, J.C.; Woolliscroft, J.O. Telemedicine and the COVID-19 Pandemic, Lessons for the Future. Telemed. e-Health 2020, 26, 571–573. [Google Scholar] [CrossRef] [PubMed]
- Gadzinski, A.J.; Gore, J.L.; Ellimoottil, C.; Odisho, A.Y.; Watts, K.L. Implementing Telemedicine in Response to the COVID-19 Pandemic. J. Urol. 2020, 204, 14–16. [Google Scholar] [CrossRef] [PubMed]
- Portnoy, J.; Waller, M.; Elliott, T. Telemedicine in the Era of COVID-19. J. Allergy Clin. Immunol. Pr. 2020, 8, 1489–1491. [Google Scholar] [CrossRef]
- Mihalj, M.; Carrel, T.; Gregoric, I.D.; Andereggen, L.; Zinn, P.O.; Doll, D.; Stueber, F.; Gabriel, R.A.; Urman, R.D.; Luedi, M.M. Telemedicine for preoperative assessment during a COVID-19 pandemic: Recommendations for clinical care. Best Pr. Res. Clin. Anaesthesiol. 2020, 34, 345–351. [Google Scholar] [CrossRef]
- Endler, M.; Lavelanet, A.; Cleeve, A.; Ganatra, B.; Gomperts, R.; Gemzell-Danielsson, K. Telemedicine for medical abortion: A systematic review. BJOG Int. J. Obstet. Gynaecol. 2019, 126, 1094–1102. [Google Scholar] [CrossRef]
- Lupton, D.; Maslen, S. Telemedicine and the senses: A review. Sociol. Health Illn. 2017, 39, 1557–1571. [Google Scholar] [CrossRef]
- Romanick-Schmiedl, S.; Raghu, G. Telemedicine—Maintaining quality during times of transition. Nat. Rev. Dis. Prim. 2020, 6, 1–2. [Google Scholar] [CrossRef]
- Ahir, S.; Telavane, D.; Thomas, R. The impact of Artificial Intelligence, Blockchain, Big Data and evolving technologies in Coronavirus Disease-2019 (COVID-19) curtailment. In Proceedings of the 2020 International Conference on Smart Electronics and Communication (ICOSEC), Trichy, Tamilnadu, 10–12 September 2020; Volume 2019, pp. 113–120. [Google Scholar]
- Celesti, A.; Ruggeri, A.; Fazio, M.; Galletta, A.; Villari, M.; Romano, A. Blockchain-Based Healthcare Workflow for Tele-Medical Laboratory in Federated Hospital IoT Clouds. Sensors 2020, 20, 2590. [Google Scholar] [CrossRef]
- La Gatta, V.; Moscato, V.; Postiglione, M.; Sperli, G. An Epidemiological Neural Network Exploiting Dynamic Graph Structured Data Applied to the COVID-19 Outbreak. IEEE Trans. Big Data 2021, 7, 45–55. [Google Scholar] [CrossRef]
- Khan, F.; Ghaffar, A.; Khan, N.; Cho, S.H. An Overview of Signal Processing Techniques for Remote Health Monitoring Using Impulse Radio UWB Transceiver. Sensors 2020, 20, 2479. [Google Scholar] [CrossRef] [PubMed]
- Moraes, M.; Mendes, T.; Arantes, R. Smart Wearables for Cardiac Autonomic Monitoring in Isolated, Confined and Extreme Environments: A Perspective from Field Research in Antarctica. Sensors 2021, 21, 1303. [Google Scholar] [CrossRef] [PubMed]
- Rath, M. Big Data and IoT-Allied Challenges Associated with Healthcare Applications in Smart and Automated Systems. Data Anal. Med. 2020, 1401–1414. [Google Scholar] [CrossRef]
- Rathore, M.M.; Ahmad, A.; Paul, A.; Wan, J.; Zhang, D. Real-time Medical Emergency Response System: Exploiting IoT and Big Data for Public Health. J. Med. Syst. 2016, 40, 283. [Google Scholar] [CrossRef]
- Saheb, T.; Izadi, L. Paradigm of IoT big data analytics in the healthcare industry: A review of scientific literature and mapping of research trends. Telemat. Inform. 2019, 41, 70–85. [Google Scholar] [CrossRef]
- Talal, M.; Zaidan, A.A.; Zaidan, B.B.; Albahri, A.S.; Alamoodi, A.H.; AlSalem, M.A.; Lim, C.K.; Tan, K.L.; Shir, W.L.; Mohammed, K.I. Smart Home-based IoT for Real-time and Secure Remote Health Monitoring of Triage and Priority System using Body Sensors: Multi-driven Systematic Review. J. Med. Syst. 2019, 43, 42. [Google Scholar] [CrossRef]
- Rathore, M.M.; Paul, A.; Hong, W.-H.; Seo, H.; Awan, I.; Saeed, S. Exploiting IoT and big data analytics: Defining Smart Digital City using real-time urban data. Sustain. Cities Soc. 2018, 40, 600–610. [Google Scholar] [CrossRef]
- Dash, S.P. The Impact of IoT in Healthcare: Global Technological Change & The Roadmap to a Networked Architecture in India. J. Indian Inst. Sci. 2020, 100, 773–785. [Google Scholar] [CrossRef]
- Mishra, K.N.; Chakraborty, C. A Novel Approach Towards Using Big Data and IoT for Improving the Efficiency of m-Health Systems. Recent Adv. Comput. Optim. 2019, 875, 123–139. [Google Scholar] [CrossRef]
- Bu, X.; Lu, L.; Zhang, Z.; Zhang, Q.; Zhu, Y. A General Outpatient Triage System Based on Dynamic Uncertain Causality Graph. IEEE Access 2020, 8, 93249–93263. [Google Scholar] [CrossRef]
- Hinson, J.S.; Martinez, D.A.; Cabral, S.; George, K.; Whalen, M.; Hansoti, B.; Levin, S. Triage Performance in Emergency Medicine: A Systematic Review. Ann. Emerg. Med. 2019, 74, 140–152. [Google Scholar] [CrossRef]
- Considine, J.; Levasseur, S.A.; Villanueva, E. The Australasian Triage Scale: Examining emergency department nurses’ performance using computer and paper scenarios. Ann. Emerg. Med. 2004, 44, 516–523. [Google Scholar] [CrossRef]
- Hodge, A.; Hugman, A.; Varndell, W.; Howes, K. A review of the quality assurance processes for the Australasian Triage Scale (ATS) and implications for future practice. Australas Emerg. Nurs. J. 2013, 16, 21–29. [Google Scholar] [CrossRef]
- Kiblboeck, D.; Steinrueck, K.; Nitsche, C.; Lang, W.; Kellermair, J.; Blessberger, H.; Steinwender, C.; Siostrzonek, P. Evaluation of the Manchester triage system for patients with acute coronary syndrome. Wien. Klin. Wochenschr. 2020, 132, 277–282. [Google Scholar] [CrossRef]
- Canadian Ministry of Health and Long-Term Care Prehospital Canadian Triage Acuity Scale: Prehospital CTAS Paramedic Guide. Ontario Hospital Association. 2016, Volume 2. Available online: http://www.ontariobasehospitalgroup.ca/Provincial-Standards/Downloads_GetFile.aspx?id=18042 (accessed on 1 June 2020).
- Bullard, M.J.; Musgrave, E.; Warren, D.; Unger, B.; Skeldon, T.; Grierson, R.; van der Linde, E.; Swain, J. Revisions to the Canadian Emergency Department Triage and Acuity Scale (CTAS) Guidelines. CJEM 2017, 19, S18–S27. [Google Scholar] [CrossRef] [PubMed]
- Paediatric Triage Working Group (PTWG) of the Western Cape Government the South African Triage Scale Training Manual. 2012. Available online: https://emssa.org.za/wp-content/uploads/2011/04/SATS-Manual-A5-LR-spreads.pdf (accessed on 27 March 2021).
- Qureshi, N. Triage systems: A review of the literature with reference to Saudi Arabia. East. Mediterr. Health J. 2010, 16, 690–698. [Google Scholar] [CrossRef] [PubMed]
- Al-Fayyadh, F.M.; Bin Saeed, A.; Alshomar, K.M.; Zekry, Z.W.; AlAmiri, N.N.; Abaalkhail, A.M.; Aldughaither, A.A.; Alaska, Y.A. Validating the implementation of the triage system in an emergency department in a University Hospital. J. Health Spéc. 2017, 5, 73. [Google Scholar] [CrossRef]
- Salman, O.H.; Rasid, M.F.A.; Saripan, M.I.; Subramaniam, S.K. Multi-Sources Data Fusion Framework for Remote Triage Prioritization in Telehealth. J. Med. Syst. 2014, 38, 1–23. [Google Scholar] [CrossRef]
- Ashour, O.M.; Kremer, G.E.O. Dynamic patient grouping and prioritization: A new approach to emergency department flow improvement. Health Care Manag. Sci. 2014, 19, 192–205. [Google Scholar] [CrossRef]
- Golgoun, A.S.; Sepidnam, G. The optimized algorithm for prioritizing and scheduling of patient appointment at a health center according to the highest rating in waiting Queue. Int. J. Sci. Technol. Res. 2018, 7, 240–245. [Google Scholar]
- Lima, B.; Faria, J.P. Towards Real-Time Patient Prioritization in Hospital Emergency Services. In Proceedings of the 2018 IEEE 20th International Conference on e-Health Networking, Applications and Services (Healthcom), Ostrava, Czech Republic, 17–20 September 2018; pp. 1–4. [Google Scholar]
- Lin, D.; Patrick, J.; LaBeau, F. Estimating the waiting time of multi-priority emergency patients with downstream blocking. Health Care Manag. Sci. 2014, 17, 88–99. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Park, E.; Nagarajan, M.; Grafstein, E. Patient Prioritization in Emergency Department Triage Systems: An Empirical Study of the Canadian Triage and Acuity Scale (CTAS). Manuf. Serv. Oper. Manag. 2019, 21, 723–741. [Google Scholar] [CrossRef]
- Kumar, A.; Lakshminarayanan, D.; Joshi, N.; Vaid, S.; Bhoi, S.; Deorari, A. Triaging the triage: Reducing waiting time to triage in the emergency department at a tertiary care hospital in New Delhi, India. Emerg. Med. J. 2019, 36, 558–563. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.; Zhao, X. Using a priority queuing approach to improve emergency department performance. J. Manag. Anal. 2019, 7, 28–43. [Google Scholar] [CrossRef]
- Wallace, D.W.; Burleson, S.L.; Heimann, M.A.; Crosby, J.C.; Swanson, J.; Gibson, C.B.; Greene, C. An adapted emergency department triage algorithm for the COVID-19 pandemic. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1374–1379. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Tao, J.; Song, Z.; Yang, L.; Huang, C.; Feng, A.; Man, X. Emergency management for preventing and controlling nosocomial infection of the 2019 novel coronavirus: Implications for the dermatology department. Br. J. Dermatol. 2020, 182, 1477–1478. [Google Scholar] [CrossRef] [PubMed]
- Corden, E.; Rogers, A.K.; Woo, W.A.; Simmonds, R.; Mitchell, C.D. A targeted response to the COVID-19 pandemic: Analysing effectiveness of remote consultations for triage and management of routine dermatology referrals. Clin. Exp. Dermatol. 2020, 45, 1047–1050. [Google Scholar] [CrossRef]
- Paleri, V.; Hardman, J.; Tikka, T.; Bradley, P.; Pracy, P.; Kerawala, C. Rapid implementation of an evidence-based remote triaging system for assessment of suspected referrals and patients with head and neck cancer on follow-up after treatment during the COVID -19 pandemic: Model for international collaboration. Head Neck 2020, 42, 1674–1680. [Google Scholar] [CrossRef]
- Kassardjian, C.D.; Desai, U.; Narayanaswami, P. The AANEM Quality and Patient Safety Committee of the AANEM Practical guidance for managing electromyography requests and testing during the COVID -19 pandemic. Muscle Nerve 2020, 62, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.B.; Welt, F.G.P.; Mahmud, E.; Phillips, A.; Kleiman, N.S.; Young, M.N.; Sherwood, M.; Batchelor, W.; Wang, D.D.; Davidson, L.; et al. Triage considerations for patients referred for structural heart disease intervention during the COVID -19 pandemic: An ACC/SCAI position statement. Catheter. Cardiovasc. Interv. 2020, 96, 659–663. [Google Scholar] [CrossRef] [PubMed]
- Lopez, J.J.; Ebinger, J.E.; Allen, S.; Yildiz, M.; Henry, T.D. Adapting STEMI care for the COVID -19 pandemic: The case for low-risk STEMI triage and early discharge. Catheter. Cardiovasc. Interv. 2020. [Google Scholar] [CrossRef] [PubMed]
- CDC Standard Operating Procedure (SOP) for Triage of Suspected COVID-19 Patients in non-US Healthcare Settings: Early Identi cation and Prevention of Transmission during Triage. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/sop-triage-prevent-transmission.html (accessed on 1 June 2020).
- Dadashzadeh, A.; Alamdari, N.G.; Ala, A.; Dehghannejad, J.; Jabbarzadeh, F.; Babaie, N. Triage guidelines for emergency department patients with COVID-19. J. Res. Clin. Med. 2020, 8, 12. [Google Scholar] [CrossRef]
- Zhang, N.; Deng, Y.; Li, W.; Liu, J.; Li, H.; Liu, E.; Zheng, X. Analysis and suggestions for the preview and triage screening of children with suspected COVID-19 outside the epidemic area of Hubei Province. Transl. Pediatr. 2020, 9, 126–132. [Google Scholar] [CrossRef]
- Saudi Ministry of Health (MOH). Hospital Admission Criteria for COVID-19 Pediatric Patients, Version 1.1. Available online: https://www.moh.gov.sa/Ministry/MediaCenter/Publications/Documents/Hospital-admission-criteria.pdf (accessed on 12 December 2020).
- Weqaya (SaudiCDC) Coronavirus Disease COVID-19 Guidelines, v1.3. Available online: https://www.moh.gov.sa/Ministry/MediaCenter/Publications/Documents/Coronavirus-Disease-2019-Guidelines-v1.2.pdf (accessed on 20 November 2020).
- Saudi Ministry of Health (MOH) ICU Triage, Admission, and Discharge Criteria during the COVID 19 Pandemic. Available online: https://www.moh.gov.sa/Ministry/MediaCenter/Publications/Documents/ICU-Criteria-during.pdf (accessed on 12 December 2020).
- Physiopedia-Contributors. Respiratory Management of COVID 19. Physiopedia. 2020. Available online: https://www.physio-pedia.com/Respiratory_Management_of_COVID_19 (accessed on 14 June 2020).
- Zu, Z.Y.; Di Jiang, M.; Xu, P.P.; Chen, W.; Ni, Q.Q.; Lu, G.M.; Zhang, L.J. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology 2020, 296, E15–E25. [Google Scholar] [CrossRef]
- General Office of National Health Committee. Office of State Administration of Traditional Chinese Medicine Notice on the Issuance of a New Coronavirus Infection Pneumonia Diagnosis and Treatmen Plan (Trial Fifth Version). Available online: http://bgs.satcm.gov.cn/zhengcewenjian/2020-02-06/12847.html (accessed on 27 June 2020).
- Spinato, G.; Fabbris, C.; Polesel, J.; Cazzador, D.; Borsetto, D.; Hopkins, C.; Boscolo-Rizzo, P. Alterations in Smell or Taste in Mildly Symptomatic Outpatients With SARS-CoV-2 Infection. JAMA 2020, 323, 2089–2090. [Google Scholar] [CrossRef]
- Feng, Y.; Ling, Y.; Bai, T.; Xie, Y.; Huang, J.; Li, J.; Xiong, W.; Yang, D.; Chen, R.; Lu, F.; et al. COVID-19 with Different Severities: A Multicenter Study of Clinical Features. Am. J. Respir. Crit. Care Med. 2020, 201, 1380–1388. [Google Scholar] [CrossRef]
- Zhao, X.; Zhang, B.; Li, P.; Ma, C.; Gu, J.; Hou, P.; Guo, Z.; Wu, H.; Bai, Y. Incidence, clinical characteristics and prognostic factor of patients with COVID-19: A systematic review and meta-analysis. medRxiv 2020. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Xu, X.-W.; Wu, X.-X.; Jiang, X.-G.; Xu, K.-J.; Ying, L.-J.; Ma, C.-L.; Li, S.-B.; Wang, H.-Y.; Zhang, S.; Gao, H.-N.; et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: Retrospective case series. BMJ 2020, 368, m606. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Mu, M.; Yang, P.; Sun, Y.; Wang, R.; Yan, J.; Li, P.; Hu, B.; Wang, J.; Hu, C.; et al. Clinical Characteristics of COVID-19 Patients With Digestive Symptoms in Hubei, China: A Descriptive, Cross-Sectional, Multicenter Study. Am. J. Gastroenterol. 2020, 115, 766–773. [Google Scholar] [CrossRef]
- World Health Organization. Clinical Management of Severe Acute Respiratory Infection (SARI) when COVID-19 Disease Is Suspected—Interim Guidance; World Health Organization, 2020. License: CC BY-NC-SA 3.0 IGO. Available online: https://apps.who.int/iris/handle/10665/331446 (accessed on 14 June 2020).
- Check if You or Your Child has Coronavirus Symptoms. Available online: https://www.nhs.uk/conditions/coronavirus-covid-19/symptoms/ (accessed on 14 June 2020).
- Yan, C.H.; Faraji, F.; Bs, D.P.P.; Boone, C.E.; DeConde, A.S. Association of chemosensory dysfunction and COVID-19 in patients presenting with influenza-like symptoms. Int. Forum Allergy Rhinol. 2020, 10, 806–813. [Google Scholar] [CrossRef]
- Tudrej, B.; Sebo, P.; Lourdaux, J.; Cuzin, C.; Floquet, M.; Haller, D.M.; Maisonneuve, H. Self-Reported Loss of Smell and Taste in SARS-CoV-2 Patients: Primary Care Data to Guide Future Early Detection Strategies. J. Gen. Intern. Med. 2020, 35, 2502–2504. [Google Scholar] [CrossRef]
- Giacomelli, A.; Pezzati, L.; Conti, F.; Bernacchia, D.; Siano, M.; Oreni, L.; Rusconi, S.; Gervasoni, C.; Ridolfo, A.L.; Rizzardini, G.; et al. Self-reported Olfactory and Taste Disorders in Patients With Severe Acute Respiratory Coronavirus 2 Infection: A Cross-sectional Study. Clin. Infect. Dis. 2020, 71, 889–890. [Google Scholar] [CrossRef]
- Yan, C.H.; Faraji, F.; Bs, D.P.P.; Ostrander, B.T.; DeConde, A.S. Self-reported olfactory loss associates with outpatient clinical course in COVID-19. Int. Forum Allergy Rhinol. 2020, 10, 821–831. [Google Scholar] [CrossRef]
- Wollina, U.; Karadağ, A.S.; Rowland-Payne, C.; Chiriac, A.; Lotti, T. Cutaneous signs in COVID-19 patients: A review. Dermatol. Ther. 2020, 33, e13549. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhou, L.; Yang, Y.; Peng, W.; Wang, W.; Chen, X. Therapeutic and triage strategies for 2019 novel coronavirus disease in fever clinics. Lancet Respir. Med. 2020, 8, e11–e12. [Google Scholar] [CrossRef]
- General Office of National Health Committee. Office of State Administration of Traditional Chinese Medicine Notice on the Issuance of a New Coronavirus Pneumonia Diagnosis and Treatment Plan (fo Trial Version 6). Available online: http://yzs.satcm.gov.cn/zhengcewenjian/2020-02-19/13221.html (accessed on 27 June 2020).
- World Health Organization. Home Care for Patients with Suspected Novel Coronavirus (nCoV) Infection Presenting with Mild Symptoms and Management of Contacts. 2020. License: CC BY-NC-SA 3.0 IGO. Available online: https://apps.who.int/iris/handle/10665/330671 (accessed on 14 June 2020).
- Elkum, N.B.; Barrett, C.; Al-Omran, H. Canadian Emergency DepartmentTriage and Acuity Scale: Implementation in a tertiary care center in Saudi Arabia. BMC Emerg. Med. 2011, 11, 3. [Google Scholar] [CrossRef] [PubMed]
- Almahdi, E.M.; Zaidan, A.A.; Zaidan, B.B.; AlSalem, M.A.; Albahri, O.S.; Albahri, A.S. Mobile-Based Patient Monitoring Systems: A Prioritisation Framework Using Multi-Criteria Decision-Making Techniques. J. Med. Syst. 2019, 43, 219. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).