Cancer Prevention by Natural Products Introduced into the Diet—Selected Cyclitols
Abstract
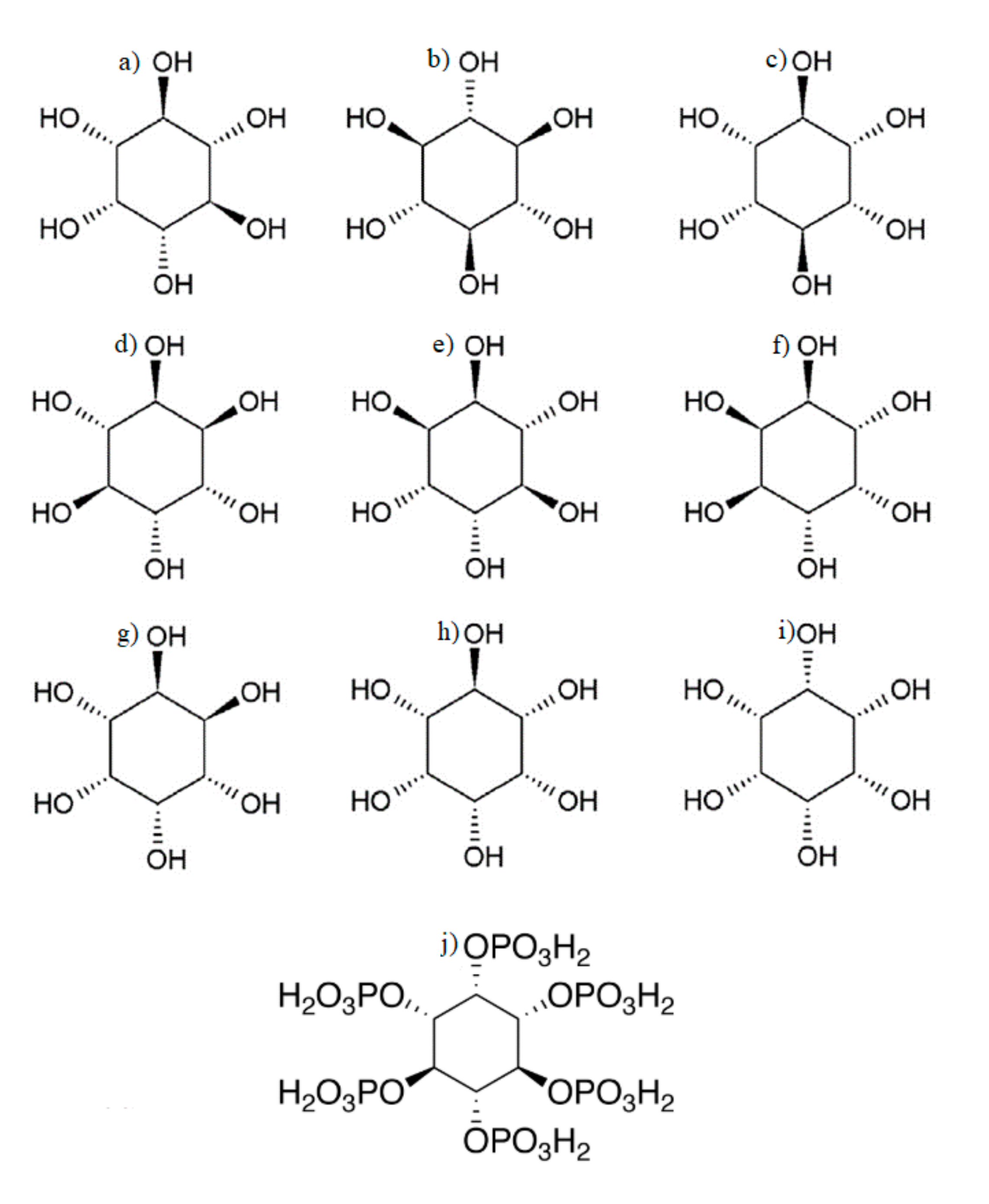
1. Cyclitols
2. Cancers
3. Lung Cancer and Cyclitols
4. Breast Cancer and Cyclitols
5. Colorectal Cancer and Cyclitols
6. Prostate Cancer and Cyclitols
7. Cyclitols and Other Cancers
8. Cyclitols and Other Disorders
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| IL-6 | interleukin-6 |
| STAT | signal transducer and activator of transcription gene family |
| BALF | bronchoalveolar lavage fluid |
| Akt | RAC-alpha serine/threonine–protein kinase |
| ERK | extracellular signal-regulated kinase |
| FEC-5 | fluorouracil, epidoxorubicin and cyclophosphamide |
| CMF | cyclophosphamide methotrexate fluorouracil |
| HLA-1 | human leukocyte antigen I |
| P-FAK | phosphorylated focal adhesion kinase |
| BMI body | mass index |
| HOMA-IR | homeostatic model assessment for insulin Resistance |
References
- Carlomagno, G.; Unfer, V. Inositol safety: Clinical evidence. Eur. Rev. Med. Pharmacol. 2011, 15, 931–936. [Google Scholar]
- Antonowski, T.; Osowski, A.; Lahuta, L.; Górecki, R.; Rynkiewicz, A.; Wojtkiewicz, J. Health-Promoting Properties of Selected Cyclitols for Metabolic Syndrome and Diabetes. Nutrients 2019, 11, 2314. [Google Scholar] [CrossRef] [PubMed]
- Bizzarri, M.; Fuso, A.; Dinicola, S.; Cucina, A.; Bevilacqua, A. Pharmacodynamics and pharmacokinetics of inositol(s) in health and disease. Expert Opin. On Drug Metab. Toxicol. 2016, 12, 1181–1196. [Google Scholar] [CrossRef] [PubMed]
- Facchinetti, F.; Bizzarri, M.; Benvenga, S.; D’Anna, R.; Lanzone, A.; Soulage, C.; Renzo, G.C.D.; Hod, M.; Cavalli, P.; Chiu, T.T.; et al. Results from the International Consensus Conference on Myo-inositol and d-chiro-inositol in Obstetrics and Gynecology: The link between metabolic syndrome and PCOS. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 195, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Holub, B.J. Metabolism and Function of myo-Inositol and Inositol Phospholipids. Annu. Rev. Nutr. 1986, 6, 563–597. [Google Scholar] [CrossRef]
- Schlemmer, U.; Frølich, W.; Prieto, R.M.; Grases, F. Phytate in foods and significance for humans: Food sources, intake, processing, bioavailability, protective role and analysis. Mol. Nutr. Food Res. 2009, 53, S330–S375. [Google Scholar] [CrossRef]
- Croze, M.L.; Soulage, C.O. Potential role and therapeutic interests of myo-inositol in metabolic diseases. Biochimie 2013, 95, 1811–1827. [Google Scholar] [CrossRef]
- Clements, R.S.; Darnell, B. Myo-inositol content of common foods: Development of a high-myo-inositol diet. Am. J. Clin. Nutr. 1980, 33, 1954–1967. [Google Scholar] [CrossRef]
- Nahapetian, A.; Young, V.R. Metabolism of 14C-Phytate in Rats: Effect of Low and High Dietary Calcium Intakes. J. Nutr. 1980, 110, 1458–1472. [Google Scholar] [CrossRef]
- Carlomagno, G.; Grazia, S.D.; Unfer, V.; Manna, F. Myo-inositol in a new pharmaceutical form: A step forward to a broader clinical use. Expert Opin. Drug Deliv. 2012, 9, 267–271. [Google Scholar] [CrossRef]
- Burton, L.E.; Ray, R.E.; Bradford, J.R.; Orr, J.P.; Nickerson, J.A.; Wells, W.W. myo-Inositol Metabolism in the Neonatal and Developing Rat Fed a myo-Inositol-free Diet. J. Nutr. 1976, 106, 1610–1616. [Google Scholar] [CrossRef] [PubMed]
- Lam, S. A Phase I Study of myo-Inositol for Lung Cancer Chemoprevention. Cancer Epidemiol. Biomark. Prev. 2006, 15, 1526–1531. [Google Scholar] [CrossRef] [PubMed]
- CFR—Code of Federal Regulations Title 21. Available online: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=184.1370 (accessed on 8 May 2020).
- Cancer. Available online: https://www.who.int/health-topics/cancer#tab=tab_2 (accessed on 8 May 2020).
- Mcnamara, M.; Batur, P.; Walsh, J.M.E.; Johnson, K.M. HPV Update: Vaccination, Screening, and Associated Disease. J. Gen. Intern. Med. 2016, 31, 1360–1366. [Google Scholar] [CrossRef] [PubMed]
- Crawford, J.; Dale, D.C.; Lyman, G.H. Chemotherapy-induced neutropenia. Cancer 2004, 100, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Mones, J.V.; Soff, G. Management of Thrombocytopenia in Cancer Patients. In Thrombosis Hemostasis in Cancer; Springer: Berlin/Heidelberg, Germany, 2019; pp. 139–150. [Google Scholar]
- Cancer Today. Available online: https://gco.iarc.fr/today/data/factsheets/cancers/15-Lung-fact-sheet (accessed on 8 May 2020).
- Szabo, E.; Mao, J.T.; Lam, S.; Reid, M.E.; Keith, R.L. Chemoprevention of Lung Cancer. Chest 2013, 143, e40S–e60S. [Google Scholar] [CrossRef]
- Krzakowski, M.; Jassem, J.; Antczak, A.; Chorostowska-Wynimko, J.; Dziadziuszko, R.; Głogowski, M.; Grodzki, T.; Kowalski, D.; Olszewski, W.; Orłowski, T.; et al. Cancer of the lung, pleura and mediastinum. Oncol. Clin. Pract. 2019, 15, 20–50. [Google Scholar]
- National Lung Sceening Trial Research Team. Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef]
- Estensen, R.D.; Wattenberg, L.W. Studies of chemo-preventive effects of myo-inositol on benzo(a)pyrene-induced neoplasia of the lung and forestomach of female A/J mice. Carcinogenesis 1993, 14, 1975–1977. [Google Scholar] [CrossRef]
- Hecht, S.S.; Kenney, P.M.; Wang, M.; Upadhyaya, P. Dose–response study of myo-inositol as an inhibitor of lung tumorigenesis induced in A/J mice by benzo[a]pyrene and 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone. Cancer Lett. 2001, 167, 1–6. [Google Scholar] [CrossRef]
- Hecht, S.S. Inhibition of lung tumorigenesis in A/J mice by N-acetyl-S-(N-2-phenethylthiocarbamoyl)-L-cysteine and myo-inositol, individually and in combination. Carcinogenesis 2002, 23, 1455–1461. [Google Scholar] [CrossRef]
- Unver, N.; Delgado, O.; Zeleke, K.; Cumpian, A.; Tang, X.; Caetano, M.S.; Wang, H.; Katayama, H.; Yu, H.; Szabo, E.; et al. Reduced IL-6 levels and tumour-associated phospho-STAT3 are associated with reduced tumour development in a mouse model of lung cancer chemoprevention with myo-inositol. Int. J. Cancer 2017, 142, 1405–1417. [Google Scholar] [CrossRef] [PubMed]
- Iriki, T.; Ohnishi, K.; Fujiwara, Y.; Horlad, H.; Saito, Y.; Pan, C.; Ikeda, K.; Mori, T.; Suzuki, M.; Ichiyasu, H.; et al. The cell-cell interaction between tumour-associated macrophages and small cell lung cancer cells is involved in tumour progression via STAT3 activation. Lung Cancer 2017, 106, 22–32. [Google Scholar] [CrossRef]
- Han, W.; Gills, J.J.; Memmott, R.M.; Lam, S.; Dennis, P.A. The Chemo-preventive Agent Myoinositol Inhibits Akt and Extracellular Signal-Regulated Kinase in Bronchial Lesions from Heavy Smokers. Cancer Prev. Res. 2009, 2, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Lam, S.; Mandrekar, S.J.; Gesthalter, Y.; Ziegler, K.L.A.; Seisler, D.K.; Midthun, D.E.; Mao, J.T.; Aubry, M.C.; Mcwilliams, A.; Sin, D.D.; et al. A Randomized Phase IIb Trial of myo-Inositol in Smokers with Bronchial Dysplasia. Cancer Prev. Res. 2016, 9, 906–914. [Google Scholar] [CrossRef] [PubMed]
- Shivapurkar, N.; Tang, Z.; Frost, A.; Alabaster, O. A rapid dual organ rat carcinogenesis bioassay for evaluating the chemoprevention of breast and colon cancer. Cancer Lett. 1996, 100, 169–179. [Google Scholar] [CrossRef]
- Vucenik, I.; Yang, G.-Y.; Shamsuddin, A.M. Inositol hexaphosphate and inositol inhibit DMBA-induced rat mammary cancer. Carcinogenesis 1995, 16, 1055–1058. [Google Scholar] [CrossRef]
- Vucenik, I.; Yang, G.Y.; Shamsuddin, A.M. Comparison of pure inositol hexaphosphate and high-bran diet in the prevention of DMBA-induced rat mammary carcinogenesis. Nutr. Cancer 1997, 28, 7–13. [Google Scholar] [CrossRef]
- Shamsuddin, A.M.; Vucenik, I.; Cole, K.E. IP6: A novel anti-cancer agent. Life Sci. 1997, 61, 343–354. [Google Scholar] [CrossRef]
- El-Sherbiny, Y.M.; Cox, M.C.; Ismail, Z.A.; Shamsuddin, A.M.; Vucenik, I. G0/G1 arrest and S phase inhibition of human cancer cell lines by inositol hexaphosphate (IP6). Anticancer Res. 2001, 21, 2393–2403. [Google Scholar]
- Tantivejkul, K.; Vucenik, I.; Shamsuddin, A.M. Inositol hexaphosphate (IP6) inhibits key events of cancer metastasis: I. In Vitro studies of adhesion, migration and invasion of MDA-MB 231 human breast cancer cells. Anticancer Res. 2003, 23, 3671–3679. [Google Scholar]
- Tantivejkul, K.; Vucenik, I.; Shamsuddin, A.M. Inositol hexaphosphate (IP6) inhibits key events of cancer metastasis: II. Effects on integrins and focal adhesions. Anticancer Res. 2003, 23, 3681–3689. [Google Scholar] [PubMed]
- Vucenik, I.; Ramakrishna, G.; Tantivejkul, K.; Anderson, L.M.; Ramljak, D. Inositol hexaphosphate (IP6) blocks proliferation of human breast cancer cells through a PKCδ-dependent increase in p27Kip1 and decrease in retinoblastoma protein (pRb) phosphorylation. Breast Cancer Res. Treat. 2005, 91, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Tantivejkul, K.; Vucenik, I.; Eiseman, J.; Shamsuddin, A.M. Inositol Hexaphosphate (IP6) Enhances the Anti-Proliferative Effects of Adriamycin and Tamoxifen in Breast Cancer. Breast Cancer Res. Treat. 2003, 79, 301–312. [Google Scholar] [CrossRef] [PubMed]
- Dinicola, S.; Fabrizi, G.; Masiello, M.G.; Proietti, S.; Palombo, A.; Minini, M.; Harrath, A.H.; Alwasel, S.H.; Ricci, G.; Catizone, A.; et al. Inositol induces mesenchymal-epithelial reversion in breast cancer cells through cytoskeleton rearrangement. Exp. Cell Res. 2016, 345, 37–50. [Google Scholar] [CrossRef]
- Bacic, I.; Druzijanic, N.; Karlo, R.; Skific, I.; Jagic, S. Efficacy of IP6 inositol in the treatment of breast cancer patients receiving chemotherapy: Prospective, randomized, pilot clinical study. J. Exp. Clin. Cancer Res. 2010, 29, 12. [Google Scholar] [CrossRef]
- Lyman, G.H.; Abella, E.; Pettengell, R. Risk factors for febrile neutropenia among patients with cancer receiving chemotherapy: A systematic review. Crit. Rev. Oncol. Hematol. 2014, 90, 190–199. [Google Scholar] [CrossRef]
- Proietti, S.; Pasta, V.; Cucina, A.; Aragona, C.; Palombi, E.; Vucenik, I.; Bizzarri, M. Inositol hexaphosphate (InsP6) as an effective topical treatment for patients receiving adjuvant chemotherapy after breast surgery. Eur. Rev. Med. Pharm. Sci. 2017, 21, 43–50. [Google Scholar]
- Pasta, V.; Gullo, G.; Giuliani, A.; Harrath, A.H.; Alwasel, S.H.; Tartaglia, F.; Cucina, A.; Bizzarri, M. An association of boswellia, betaine and myo-inositol (Eumastós) in the treatment of mammographic breast density: A randomized, double-blind study. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 4419–4426. [Google Scholar]
- Boyd, N.F.; Martin, L.J.; Yaffe, M.J.; Minkin, S. Mammographic density and breast cancer risk: Current understanding and future prospects. Breast Cancer Res. 2011, 13, 223. [Google Scholar] [CrossRef]
- Pasta, V.; Dinicola, S.; Giuliani, A.; Harrath, A.H.; Alwasel, S.H.; Tartaglia, F.; Cucina, A.; Bizzarri, M. A Randomized Pilot Study of Inositol in Association with Betaine and Boswellia in the Management of Mastalgia and Benign Breast Lump in Premenopausal Women. Breast Cancer Basic Clin. Res. 2016, 10, S38408. [Google Scholar] [CrossRef]
- Santen, R.J.; Mansel, R. Benign Breast Disorders. N. Engl. J. Med. 2005, 353, 275–285. [Google Scholar] [CrossRef] [PubMed]
- Cerrato, F.; Labow, B. Diagnosis and Management of Fibroadenomas in the Adolescent Breast. Semin. Plast. Surg. 2013, 27, 023–025. [Google Scholar] [CrossRef] [PubMed]
- Drew, D.A.; Cao, Y.; Chan, A.T. Aspirin and colorectal cancer: The promise of precision chemoprevention. Nat. Rev. Cancer 2016, 16, 173–186. [Google Scholar] [CrossRef] [PubMed]
- Shamsuddin, A.M.; Elsayed, A.M.; Ullah, A. Suppression of large intestinal cancer in F344 rats by inositol hexaphosphate. Carcinogenesis 1988, 9, 577–580. [Google Scholar] [CrossRef] [PubMed]
- Pretlow, T.P.; Oriordan, M.A.; Somich, G.A.; Amini, S.B.; Pretlow, T.G. Aberrant crypts correlate with tumour incidence in F344 rats treated with azoxymethane and phytate. Carcinogenesis 1992, 13, 1509–1512. [Google Scholar] [CrossRef]
- Baten, A.; Ullah, A.; Tomazic, V.J.; Shamsuddin, A.M. Inositol-phosphate-induced enhancement of natural killer cell activity correlates with tumour suppression. Carcinogenesis 1989, 10, 1595–1598. [Google Scholar] [CrossRef]
- Zhang, Z. Inositol hexaphosphate-induced enhancement of natural killer cell activity correlates with suppression of colon carcinogenesis in rats. World J. Gastroenterol. 2005, 11, 5044. [Google Scholar] [CrossRef]
- Yang, G.Y.; Shamsuddin, A.M. IP6-induced growth inhibition and differentiation of HT-29 human colon cancer cells: Involvement of intracellular inositol phosphates. Anticancer Res. 1995, 15, 2479–2487. [Google Scholar]
- Liu, G.; Song, Y.; Cui, L.; Wen, Z.; Lu, X. Inositol hexaphosphate suppresses growth and induces apoptosis in HT-29 colorectal cancer cells in culture: PI3K/Akt pathway as a potential target. Int. J. Clin. Exp. Pathol. 2015, 8, 1402–1410. [Google Scholar]
- Kapral, M.; Wawszczyk, J.; Jesse, K.; Paul-Samojedny, M.; Kuśmierz, D.; Węglarz, L. Inositol Hexaphosphate Inhibits Proliferation and Induces Apoptosis of Colon Cancer Cells by Suppressing the AKT/mTOR Signaling Pathway. Molecules 2017, 22, 1657. [Google Scholar] [CrossRef]
- Schröterová, L.; Ježková, A.; Rudolf, E.; Caltová, K.; Králová, V.; Hanušová, V. Inositol hexaphosphate limits the migration and the invasiveness of colorectal carcinoma cells in vitro. Int. J. Oncol. 2018, 53, 1625–1632. [Google Scholar] [PubMed]
- Shamsuddin, A.M.; Ullah, A. Inositol hexaphosphate inhibits large intestinal cancer in F344 rats 5 months after induction by azoxymethane. Carcinogenesis 1989, 10, 625–626. [Google Scholar] [CrossRef] [PubMed]
- Ullah, A.; Shamsuddin, A.M. Dose-dependent inhibition of large intestinal cancer by inositol hexaphosphate in F344 rats. Carcinogenesis 1990, 11, 2219–2222. [Google Scholar] [CrossRef]
- Challa, A. Interactive suppression of aberrant crypt foci induced by azoxymethane in rat colon by phytic acid and green tea. Carcinogenesis 1997, 18, 2023–2026. [Google Scholar] [CrossRef] [PubMed]
- Crawford, E. Epidemiology of prostate cancer. Urology 2003, 62, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Carter, H.B.; Piantadosi, S.; Isaacs, J.T. Clinical Evidence for and Implications of the Multistep Development of Prostate Cancer. J. Urol. 1990, 143, 742–746. [Google Scholar] [CrossRef]
- Stangelberger, A.; Waldert, M.; Djavan, B. Prostate cancer in elderly men. Rev. Urol. 2008, 10, 111–119. [Google Scholar]
- Shamsuddin, A.M.; Yang, G.-Y. Inositol hexaphosphate inhibits growth and induces differentiation of PC-3 human prostate cancer cells. Carcinogenesis 1995, 16, 1975–1979. [Google Scholar] [CrossRef]
- Lin, T.-H.; Tan, T.-W.; Tsai, T.-H.; Chen, C.-C.; Hsieh, T.-F.; Lee, S.-S.; Liu, H.-H.; Chen, W.-C.; Tang, C.-H. D-pinitol Inhibits Prostate Cancer Metastasis through Inhibition of αVβ3 Integrin by Modulating FAK, c-Src and NF-κB Pathways. Int. J. Mol. Sci. 2013, 14, 9790–9802. [Google Scholar] [CrossRef]
- Sharma, G.; Singh, R.P.; Agarwal, R. Growth inhibitory and apoptotic effects of inositol hexaphosphate in transgenic adenocarcinoma of mouse prostate (TRAMP-C1) cells. Int. J. Oncol. 2003, 23, 1413–1418. [Google Scholar] [CrossRef]
- Singh, R.P. In Vivo Suppression of Hormone-Refractory Prostate Cancer Growth by Inositol Hexaphosphate: Induction of Insulin-Like Growth Factor Binding Protein-3 and Inhibition of Vascular Endothelial Growth Factor. Clin. Cancer Res. 2004, 10, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Somasundar, P.; Riggs, D.R.; Jackson, B.J.; Cunningham, C.; Vona-Davis, L.; Mcfadden, D.W. Inositol Hexaphosphate (IP6): A Novel Treatment for Pancreatic Cancer. J. Surg. Res. 2005, 126, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Mcmillan, B.; Riggs, D.R.; Jackson, B.J.; Cunningham, C.; McFadden, D.W. Dietary Influence on Pancreatic Cancer Growth by Catechin and Inositol Hexaphosphate. J. Surg. Res. 2007, 141, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-J.; Lee, S.-A.; Choi, H. Dietary administration of inositol and/or inositol-6-phosphate prevents chemically-induced rat hepatocarcinogenesis. Asian Pac. J. Cancer Prev. 2005, 6, 41–47. [Google Scholar]
- Nishino, H. Phytochemicals in Hepatocellular Cancer Prevention. Nutr. Cancer 2009, 61, 789–791. [Google Scholar] [CrossRef]
- Ren, L.; Hong, E.S.; Mendoza, A.; Issaq, S.; Hoang, C.T.; Lizardo, M.; Leblanc, A.; Khanna, C. Metabolomics uncovers a link between inositol metabolism and osteosarcoma metastasis. Oncotarget 2017, 8, 38514. [Google Scholar] [CrossRef]
- Khurana, S.; Baldeo, C.; Joseph, R.W. Inositol hexaphosphate plus inositol induced complete remission in stage IV melanoma. Melanoma Res. 2019, 29, 322–324. [Google Scholar] [CrossRef]
- Limani, P.; Linecker, M.; Kron, P.; Samaras, P.; Pestalozzi, B.; Stupp, R.; Jetter, A.; Dutkowski, P.; Müllhaupt, B.; Schlegel, A.; et al. Development of OXY111A, a novel hypoxia-modifier as a potential antitumor agent in patients with hepato-pancreato-biliary neoplasms—Protocol of a first Ib/IIa clinical trial. BMC Cancer 2016, 16, 812. [Google Scholar] [CrossRef]
- Unfer, V.; Carlomagno, G.; Dante, G.; Facchinetti, F. Effects of Myo-Inositol in Women with PCOS: A Systematic Review of Randomized Controlled Trials. Gynecol. Endocrinol. 2012, 28, 509–515. [Google Scholar] [CrossRef]
- Genazzani, A.D.; Lanzoni, C.; Ricchieri, F.; Jasonni, V.M. Myo-Inositol Administration Positively Affects Hyperinsulinemia and Hormonal Parameters in Overweight Patients with Polycystic Ovary Syndrome. Gynecol. Endocrinol. 2008, 24, 139–144. [Google Scholar] [CrossRef]
- Wojciechowska, A.; Osowski, A.; Jóźwik, M.; Górecki, R.; Rynkiewicz, A.; Wojtkiewicz, J. Inositols’ Importance in the Improvement of the Endocrine–Metabolic Profile in PCOS. Int. J. Mol. Sci. 2019, 20, 5787. [Google Scholar] [CrossRef] [PubMed]
- Gerli, S.; Papaleo, E.; Ferrari, A.; Di Renzo, G.C. Randomized, double-blind placebo-controlled trial: Effects of myo-inositol on ovarian function and metabolic factors in women with PCOS. Eur. Rev. Med. Pharmacol. Sci. 2007, 11, 347–354. [Google Scholar] [PubMed]
- Nordio, M.; Basciani, S. Treatment with Myo-Inositol and Selenium Ensures Euthyroidism in Patients with Autoimmune Thyroiditis. Int. J. Endocrinol. 2017, 2017, 1–6. [Google Scholar] [CrossRef] [PubMed]
| Study | Cyclitol | Human/Animal Species | Results |
|---|---|---|---|
| Enstensen et al. (1993) [22] | MI | A/J mouse |
|
| Hecht et al. (2001) [23] | MI | A/J mouse |
|
| Hecht et al. (2002) [24] | MI | A/J mouse |
|
| Lam et al. [12] (2006) | MI | Human |
|
| Han et al. [27] (2009) | MI | Human |
|
| Lam et al. [28] (2016) | MI | Human |
|
| Unver et al. (2018) [25] | MI | Mouse model (CcspCre/+; Kras LSL-G12D/+) |
|
| Study | Clinical status | Cyclitol | Results |
|---|---|---|---|
| Shivapurkar et al. (1995) [29] | MUN-induced rat mammary cancer | IP6 |
|
| Vucenik et al. (1995) [30] | DMBA-induced rat mammary cancer | IP6; Ins; IP6 + Ins |
|
| Shamsuddin et al. (1996) [32] | Human breast cancer cell lines MDA-MB-231 and MCF-7 | IP6 |
|
| El-Sherbiny et al. (2001) [33] | Human breast cancer cell lines MDA-MB-231 and MCF-7 | IP6 |
|
| Tantivejkul et al. (2003) [34] | Human breast cancer cell line: MDA-MB-231 | IP6 |
|
| Tantivejkul et al. (2003) [35] | Human breast cancer cell line: MDA-MB-231 | IP6 |
|
| Tantivejkul et al. (2003) [37] | MCF-7, MDA-MB 231 and adriamycin-resistant MCF-7 (MCF-7/Adr) human breast cell lines | IP6 |
|
| Vucenik et al. (2005) [36] | MCF-7 human breast cancer cell line | IP6 |
|
| Bačić et al. (2010) [39] | Ductal invasive breast cancer during FEC chemotherapy protocol | IP6 |
|
| Pasta et al. (2015) [42] | Mammographic breast density (premenopausal women) | MI |
|
| Pasta et al. (2016) [44] | Breast fibroadenomas | MI |
|
| Dinicola et al. (2016) [38] | Human breast cancer cell lines MDA-MB-231 and ZR-75 | Inositol |
|
| Proietti et al. (2017) [41] | Ductal breast cancer stages II‒III postoperative (lumpectomy); during polychemotherapy CMF | IP6 |
|
| Study | Clinical Status | Human/Animal Species | Cyclitol | Results |
|---|---|---|---|---|
| Shamsuddin et al. (1988) [48] | AOM-induced colon cancer | Rat | IP6 |
|
| Shamsuddin et al. (1989) [56] | AOM-induced colon cancer | Rat | IP6 |
|
| Baten et al. (1989) [50] | DMH-induced colon cancer | Mouse | IP6 |
|
| Ullah et al. (1990) [57] | AOM-induced colon cancer | Rat | IP6 |
|
| Pretlow et al. (1992) [49] | AOM-induced colon cancer | Rat | IP6 |
|
| Yang et al. (1995) [52] | HT-29 human colon carcinoma cells | IP6 |
| |
| Shivapurkar et al. (1995) [29] | AOM-induced colon cancer | Rat | IP6 |
|
| Challa et al. (1997) [58] | AOM-induced colon cancer | Rat | IP6 |
|
| El-Sherbiny et al. (2001) [33] | HT-29 human colon carcinoma cells | IP6 |
| |
| Zhang et al. (2005) [51] | DMH-induced colon cancer | Rat | IP6 |
|
| Liu et al. (2015) [53] | HT-29 human colon carcinoma cells | IP6 |
| |
| Kapral et al. (2017) [54] | Colon cancer Caco-2 cells | IP6 |
| |
| Schröterová et al. (2018) [55] | Colon cancer SW620 cells | IP6 |
| |
| Type of Cancer | Study | Clinical Status | Cyclitol | Results |
|---|---|---|---|---|
| Prostate | Shamsuddin et al. (1995) [62] | PC-3 human prostate cells | IP6 |
|
| Prostate | Sharma et al. (2003) [64] | Mouse prostate (TRAMP-C1) cells | IP6 |
|
| Prostate | Singh et al. (2004) [65] | DU145 cells injected into nude mice | IP6 |
|
| Prostate | Lin et al. (2013) [63] | PC-3 and DU145 cells | d-pinitol |
|
| Pancreas | Somasundar et al. (2004) [66] | MIAPACA and PANC1 pancreatic cancer cell lines | IP6 |
|
| Pancreas | McMillan et al. (2007) [67] | PANC1 and MIAPACA | IP6 |
|
| Liver | Lee et al. (2005) [68] | Rat treated with DEN | IP6 and Ins |
|
| Liver | Nishino (2009) [69] | Patients with chronic viral hepatitis and cirrhosis | MI |
|
| Osteosarcoma | Ren et al. (2017) [70] | In vitro (K7M2 and MG63.3 cells) and in vivo trials (mice with injected K7M2 cells) | IP6 |
|
| Melanoma | Khurana et al. (2018) [71] | Case report | IP6 + Ins |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wiśniewski, K.; Jozwik, M.; Wojtkiewicz, J. Cancer Prevention by Natural Products Introduced into the Diet—Selected Cyclitols. Int. J. Mol. Sci. 2020, 21, 8988. https://doi.org/10.3390/ijms21238988
Wiśniewski K, Jozwik M, Wojtkiewicz J. Cancer Prevention by Natural Products Introduced into the Diet—Selected Cyclitols. International Journal of Molecular Sciences. 2020; 21(23):8988. https://doi.org/10.3390/ijms21238988
Chicago/Turabian StyleWiśniewski, Karol, Marcin Jozwik, and Joanna Wojtkiewicz. 2020. "Cancer Prevention by Natural Products Introduced into the Diet—Selected Cyclitols" International Journal of Molecular Sciences 21, no. 23: 8988. https://doi.org/10.3390/ijms21238988
APA StyleWiśniewski, K., Jozwik, M., & Wojtkiewicz, J. (2020). Cancer Prevention by Natural Products Introduced into the Diet—Selected Cyclitols. International Journal of Molecular Sciences, 21(23), 8988. https://doi.org/10.3390/ijms21238988





