Abstract
Coffee is one of the most popular beverages worldwide. Coffee contains bioactive compounds that affect the human body such as caffeine, caffeic acid, chlorogenic acids, trigonelline, diterpenes, and melanoidins. Some of them have demonstrated potential anticarcinogenic effects in animal models and in human cell cultures, and may play a protective role against colorectal cancer. Colorectal cancer (CRC) is the third leading cause of cancer-related mortality in the USA and other countries. Dietary patterns, as well as the consumption of beverages, may reduce the risk of CRC incidence. In this review, we focus on published epidemiological studies concerning the association of coffee consumption and the risk of development of colorectal cancer, and provide a description of selected biologically active compounds in coffee that have been investigated as potential cancer-combating compounds: Caffeine, caffeic acid (CA), chlorogenic acids (CGAs), and kahweol in relation to colorectal cancer progression in in vitro settings. We review the impact of these substances on proliferation, viability, invasiveness, and metastasis, as well as on susceptibility to chemo- and radiotherapy of colorectal cancer cell lines cultured in vitro.
Keywords:
colorectal cancer; coffee; caffeine; caffeic acid; chlorogenic acid; kahweol; cancer progression 1. Introduction
Coffee is one of the most popular beverages in the world. Its consumption in Europe has been increasing, and currently it averages around 4.1 kg/person/year. The highest intake of coffee per capita has been observed in Finland (12 kg/year) [1]. Coffee contains many substances that affect the human body, which include polyphenols, among them caffeine, caffeic acid, trigonelline, chlorogenic acid, and diterpenes such as cafestol and kahweol [1]. Several research teams have demonstrated the anti-inflammatory and anticarcinogenic potential of these components [1]. Additionally, in many observational studies, coffee consumption has been associated with a reduced risk of several types of cancer [2], diabetes mellitus type 2, ischemic stroke, Alzheimer’s disease, and Parkinson’s disease [3]. Many research reports have linked the reduced risk of occurrence of the aforementioned diseases with polyphenols in the diet [4,5,6,7,8]. High coffee consumption is positively correlated with smoking, the number of cigarettes smoked per day, as well as with meat consumption [9].
Coffee has a great impact on the human body as a whole. Coffee-derived bioactive compounds, especially caffeine, chlorogenic acid, and caffeic acid, are present in serum and urine. Meta-analysis and cohort studies have revealed beneficial, rather than harmful, effects of coffee consumption on people’s health [10,11]. People consuming 3–4 cups per day demonstrated a reduced risk of all causes of cardiovascular mortality, as well as of the incidence of cardiovascular diseases, while high consumption of coffee was related to a lower risk of incidence of specific cancers and metabolic, digestive, liver, or neurological conditions. Some studies have reported that habitual consumption of coffee reduces the concentration of inflammation markers, such as interleukin-18, E-selectin, C-reactive protein, adipokines, or IFN-γ, and increases the concentration of adiponectin in serum, which generates anti-inflammatory effects and increases sensitivity to insulin [12,13,14,15], while others have revealed increased levels of C-reactive protein, interleukin-6, interleukin-10, TNF-α, E-selectin, and plasma fibrinogen [16,17]. On the other hand, systematic review by Paiva et al. showed the absence of changes in C-reactive protein concentration after coffee consumption and decreased concentration after caffeine intake [17]. Changes in the expression of genes, especially those involved in inflammation in human, animal, and in vitro models [18,19,20], were reported. According to one of the animal studies, bean roasting affected the anti-inflammatory and antioxidant properties of coffee [21]. Coffee has a variable impact on serum cholesterol level, as increased or unaffected concentrations have been reported [12,16,22,23]. A study by Andersen et al. showed that consumption of coffee was associated with reduced risk of death related to inflammatory and cardiovascular diseases in postmenopausal women [24]. According to recent meta-analysis, the consumption of caffeinated and decaffeinated coffee may significantly reduce the incidence rate of type 2 diabetes mellitus [25,26]: However, high consumption of coffee by patients with type 1 diabetes was related to the metabolic syndrome [27].
Chuang et al. identified DNA methylation (DNAm) sites in human genomes that relate to habitual coffee consumption [28]. DNAm has been proposed as a potential epigenetic mediator for caffeine’s influence on health. The authors found CpG sites located near 11 genes associated with habitual coffee consumption in peripheral blood mononuclear cells. Additionally, many differentially methylated CpGs were located in or near genes known to be associated with coffee-related diseases. Authors have hypothesized that this may be the possible mechanism of the beneficial effect of coffee.
Animal studies conducted by Nakayama and Oishi showed decreased counts of Escherichia coli in the distal small intestine and proximal colon in mice consuming coffee [29]. The authors also reported decreased counts of Enterococcus spp., Bacteroides spp., and Clostridium spp., but an increased count of Lactobacillus spp. in the proximal colon, when compared to mice drinking sterile water. The addition of coffee to agar inhibited the growth of E. coli and Enterococcus faecalis. In a study performed by Jaquet et el., it was shown that coffee increased the count of Bifidobacterium spp., which is known to be a beneficial health factor and is reknowned for its metabolic activity [30].
Coffee consumption has an impact on gut microbiota [31]. A study by Cuervo et al. showed that Clostridium, Lactococcus, and Lactobacillus spp. were more abundant in subjects diagnosed with rhinitis and allergic asthma, which resulted from phenolic acids from coffee.
The content of bioactive compounds in coffee depends on many conditions [32,33]. The concentration of caffeine in coffee varies, depending on the method of preparation and coffee type (72–130 mg in ~240 mL of brewed coffee and 58–76 mg in a single shot of espresso), bean roasting, and procedures applied by baristas (152–232 mg/serving) [34,35]. Additionally, the boiling water pouring number and coffee ground size influence the concentration of chlorogenic acid content (75–306 mg/serving) [33,35], while the concentration of kahweol depends on the potential usage of paper filter and the characteristics of such [14].
The above-mentioned data inspired the authors to investigate more thoroughly the specific compounds contained in coffee and to study their influence on colorectal cancer progression. This review paper focuses on the current state of knowledge about the impact of coffee consumption on colorectal cancer (CRC) development in epidemiological studies and on major bioactive compounds of coffee that have been investigated in in vitro studies concerning colorectal cancer: Caffeine, caffeic acid (CA), chlorogenic acids (CGAs), and kahweol (Figure 1), and their influence on CRC cell progression. We review the impact of these substances on proliferation, viability, invasiveness, and metastatic potential and properties, as well as the sensitivity of CRC cell lines to chemo- or radiotherapy.
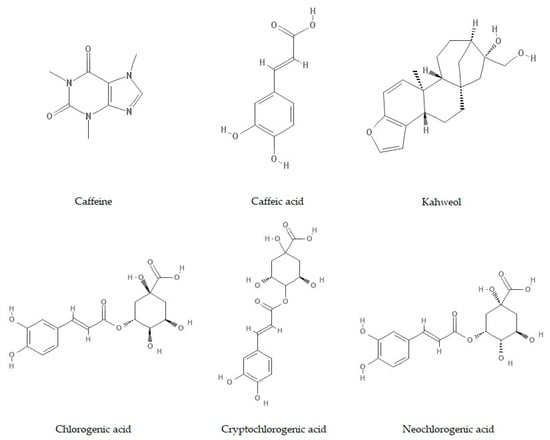
Figure 1.
Chemical structure of caffeine, caffeic acid (CA), kahweol, and chlorogenic acids (CGAs) (adapted from Pubchem).
Colorectal cancer is the third leading cause of cancer-related mortality in the United States (US). The estimated five-year survival rates range from approximately 90% for patients with stage I disease to less than 5% for patients with stage IV disease. The causes of CRC are complex and involve the interaction between genetic and environmental factors. The vast majority of CRC cases can be attributed to environmental causes, as they account for more than 70% of all incidences [36]. Some aspects of western dietary patterns may also influence the risk of CRC. Adiposity and higher levels of insulin in obese subjects are connected with an increased risk of CRC [37]. Diets rich in animal products and processed grains have been associated with higher C-peptide concentrations and elevated insulin levels in the serum of patients [38,39,40], whereas diets rich in whole grains, fiber, fruits, vegetables, as well as the consumption of coffee have typically been connected with lower concentrations of insulin or C-peptide [41,42,43,44]. Fung et al. demonstrated that specific dietary patterns were correlated with elevated C peptide concentrations and an increased incidence of colon cancer, especially in women who were overweight or whose lifestyle was sedentary [37].
Caffeine, caffeic acid, chlorogenic acids, and kahweol have shown potential anticarcinogenic effects in animal models and human cell cultures and may play a protective role against CRC [9]. Results of epidemiological studies have provided different results. Most of them have revealed no correlation between coffee consumption and CRC risk, some have shown decreased risk, and only a few have shown increased risk. A recent meta-analysis reported a reduced incidence of colon cancer in high versus no- or low-coffee-consuming subjects in case–control studies, but not in cohort studies for CRC [2]. The epidemiological assessment of the influence of coffee on colorectal cancer risk and progression has been limited to general coffee consumption and caffeine intake, while in vitro studies are more precise, focusing on single bioactive compounds present in coffee. The results of in vitro study data have suggested that all investigated bioactive compounds may prevent or reduce the growth of colorectal cancer cells. However, it is too early to recommend them for therapeutic application for the prevention of cancer, on the basis of the available evidence.
2. Coffee and Colorectal Cancer In Vivo
Chemoprotection against oxidative stress and DNA damage by means of coffee has been reported in in vitro research and in studies on rats and mice [45,46,47,48,49]. Soares et al. treated rats with pure caffeine, and both caffeinated and decaffeinated coffee, after exposure to carcinogens [49]. They found a decreased development of pre-neoplastic lesions in the colon only in rats treated with caffeinated coffee. Anti-metallothionein antibody staining revealed that decaffeinated coffee lacked a chemoprotective effect, which was induced by caffeinated coffee, and an analysis of COX-2 expression revealed that only caffeine and caffeinated coffee diminished carcinogen-related inflammatory reaction. On the other hand, caffeine and caffeinated and decaffeinated coffee reduced DNA damage in the colon, which was generated by carcinogens. According to those results, the authors claimed that coffee as a beverage had higher chemoprotective potential than caffeine alone. Kang et al. assessed the impact of caffeic acid, chlorogenic acid, and decaffeinated coffee on metastatic potential in tumor-bearing mice [50]. Mice were grafted with CT-26 colon cancer cells and then treated with different concentrations of compounds. After two weeks, the volume of lung tumors was measured. Decaffeinated coffee and CGA suppressed lung metastases in a dose-dependent manner, resulting in a decreased number and volume of tumor nodules. Additionally, CA decreased tumor nodule numbers and their weight. Both decaffeinated coffee and CGA inhibited COX-2, MMP-2, and MMP-9 expression, as well as ERK phosphorylation. Decaffeinated coffee and CA decreased MEK1 activity, while TOPK activity was inhibited by coffee, CA, and CGA, to a greater extent by CA than CGA. This resulted in the inhibition of metastases formation and enlargement.
Many epidemiological studies exploring the association between coffee consumption and colorectal cancer risk have been published. Their authors have provided much additional information about patients, such as information concerning sex, age, physical activity, dietary habits, smoking, alcohol consumption, education level, and others. On the other hand, coffee consumption is most commonly measured by the number of cups consumed per day. Some authors have distinguished caffeinated and decaffeinated coffee, but have provided no information about bean roasting level, brewing method, the addition of milk, sugar, or alcohol, or the amount of coffee used to brew one cup, nor have they distinguished coffee brewed from Coffea arabica and Coffea canephora (robusta) beans, which are very different in terms of the concentration of bioactive compounds, especially caffeine and kahweol [51]. Providing such information is very difficult, but without it the results of epidemiological studies cannot be compared and do not provide clear answers. This may serve as an explanation for the inconsistency between the observed inhibitory effect of bioactive compounds from coffee on colorectal cancer cells in the in vitro studies and inconclusive associations between coffee consumption and colorectal cancer risk in vivo.
Serum biomarkers related to habitual coffee consumption may help in understanding the association between coffee intake and colorectal cancer risk. A study by Guertin et al. showed that certain serum metabolites allow for distinguishing coffee drinkers from abstainers [52]. Additionally, higher concentrations of theophylline, caffeine, and paraxanthine were significantly inversely associated with colorectal cancer.
No significant association between total (not distinguishing between caffeinated and decaffeinated coffee), caffeinated, and decaffeinated coffee consumption and total colorectal cancer incidence risk was found in the prospective cohort study by Dik et al. [9]. Similar results were observed for caffeinated coffee (hazard ratio (HR) 1.18, p-trend 0.15). A prospective cohort study by Dominianni et al. also found no significant association between coffee consumption and the risk of colorectal cancer, also concerning the subsite distribution of cancers: Proximal, distal, or rectal cancer [53]. Bidel et al. investigated the potential association between coffee consumption and CRC incidence risk in a prospective cohort study conducted in Finland, the country with the highest consumption of coffee in the world [54]. The authors analyzed a wide range of consumption patterns, from 1 to 10 cups per day. No relationship between ingestion of coffee and incidence of colorectal, colon, and rectal cancer was found. Likewise, no association was found after adjusting patients for sex. According to the cohort study by Lukic et al., the association between coffee consumption and CRC risk was not significant (p-trend 0.10) [55]. The volume of one cup was estimated as 2.1 dL. Other population-based prospective cohort studies of Swedish patients have been performed by Terry et al., Mucci et al., Larsson et al., and Nilsson et al. [56,57,58,59]. No correlations between coffee consumption and colorectal, colon, proximal colon, distal colon, or rectal cancer were found. No associations of caffeinated coffee consumption and the incidence rate of colorectal, colon, and rectal cancer were found in a study by Michels et al. for groups pooled and adjusted for sex [60]. Nevertheless, the consumption of decaffeinated coffee was related to a marginally lower risk of colorectal and rectal cancer in pooled groups (p-trend 0.08, p-trend 0.06, respectively). No association was found also in Japanese patients with regard to colorectal, proximal, and distal colon cancer [61]. No association was observed by Peterson et al. in a prospective study for colon and rectal cancers, either [62].
A population-based case–control study by Schmit et al. found a significant association between coffee consumption and decreased risk of colorectal cancer [63]. Coffee drinkers turned out to demonstrate a lower probability of developing colorectal, colon, and rectal cancer than nondrinkers (odds ratio (OR) 0.74, p < 0.001; OR 0.74, p < 0.001; OR 78, p < 0.04, respectively). Lower risk of CRC was significant also for decaffeinated coffee (OR 0.82, p < 0.001). Stratifying the group according to daily consumption of coffee and subsite-specific cancers allowed the authors to observe decreasing chances of developing colorectal, colon, and rectal cancer in a dose-dependent manner. The authors also distinguished different types of brewing procedures. Only boiled coffee was significantly associated with a lower risk of CRC (OR 0.82, p < 0.004), while the associations of espresso, instant, and filtered coffee were not significant. The authors explained the anticancer potential of unfiltered, boiled coffee with a high content of cafestol and kahweol, which may exert anticancerogenic activity and are removed from coffee during filtering. Similar associations between coffee consumption and a reduced risk of CRC was also found by Sinha et al. [64]. The risk of colorectal, colon, and proximal colon cancers significantly decreased in a dose-dependent manner for caffeinated and decaffeinated coffee alike. The highest decrease of CRC and colon cancer risk was observed in patients who drank more than 6 cups of decaffeinated coffee per day (HR 0.74, p-trend < 0.001; HR 0.73, p-trend 0.005, respectively), while the lowest risk of proximal colon was observed in patients who drank more than 6 cups of caffeine-containing coffee per day (HR 0.59, p < 0.001). The consumption of decaffeinated coffee was significantly associated with a reduced risk of rectal cancer (HR 0.71 for 4–5 cups/day, p-trend 0.003). There were no significant associations between consumption of all types of coffee and distal colon cancer as well as caffeinated coffee consumption and rectal cancer.
Coffee consumption was found to be significantly associated with a reduced risk of CRC in Japanese people [65]. The risk of colorectal, colon, and distal colon cancer decreased with more frequent consumption of coffee, up to 1–3 cups per day, but increased in people who drank more than 4 cups per day. There was no association noted for proximal colon cancer or rectal cancer. According to the results of another population-based prospective cohort study of Japanese men and women, the consumption of coffee was not associated with CRC risk for both men and women, but reduced the risk of invasive colon cancer in women ingesting less than 1, 1–2, and more than 3 cups of coffee per day (relative risk (RR) 0.79 vs. 0.74 vs. 0.44, respectively, p-trend 0.04) [66].
Coffee consumption was associated with decreased colorectal cancer mortality in women in a study conducted by Sugiyama et al. [67]. The ingestion of 1 cup per day reduced the risk of CRC more than merely occasional consumption (HR 0.26 vs. 0.74, p-trend 0.02). That relationship was not observed in men. In opposition to results obtained by Naganuma et al., a study by Nakagawa et al. found a significant inverse association between coffee consumption and the risk of CRC, with the highest reduction for the consumption of ≥3 cups per day (OR 0.78, p-trend 0.009) [68]. The authors assessed two case–control groups, and the results were calculated for both together. The authors also found a significant dose-dependent inverse risk of developing distal colon cancer (OR 0.80 for <1 cup/day, OR 0.78 for 1–2 cups/day, OR 0.77 for ≥3 cups per day, p-trend 0.048), while there was no association for proximal colon or rectal cancers. The odds ratio for CRC remained significant only for men after adjusting to sex (p-trend 0.033).
The most interesting results were obtained in a case–control study by Azzeh et al. [69]. The study, conducted on 137 patients diagnosed with colorectal cancer and 164 healthy controls, revealed that the consumption of coffee significantly reduced the risk of CRC, even by 92%. The risk reduction was not dose-dependent, and the lowest risk was observed for the consumption of 1–2 and more than 5 cups per day (OR 0.08; OR 0.11, p-trend 0.002). The patients from the control group consumed more coffee than patients with CRC (p < 0.001). There was no significant difference in the consumption of red meat and processed meat between the groups. Red and processed meat consumption was reported to increase the risk of colorectal cancer [70,71,72,73]. Also, the incidence rate of CRC in the Saudi population was high [74].
On the other hand, the study by Groessl et al. revealed the dose-dependent increased risk of colorectal cancer incidence in women [75]. When compared to the non-coffee-drinking control, the colorectal cancer hazard ratio was 1.14 for women drinking up to 4 cups of caffeinated coffee per day and 1.15 for those drinking more than 4 cups per day (p-trend 0.04): However, after multivariate adjustment, the association remained significant, but the confidence interval for patients drinking more than 4 cups per day was of borderline insignificance. Additionally, the authors distinguished between colon, rectum, and rectosigmoid cancers, and calculated HR for women drinking up to 4 and more than 4 cups of caffeinated coffee per day (HR 1.11, HR 1.17, p-trend 0.07; HR 1.30, HR 0.95, p-trend 0.53; HR 1.15, HR 1.39, p-trend 0.40, respectively). The authors constructed survival rate (Kaplan-Meier) curves, which showed lower survival free of colorectal cancer for patients with higher coffee intake.
A case-control study by Green et al. revealed that consumption of <1 cup/week and ≥1 cup/week of iced coffee significantly increased the risk of colorectal cancer, while consumption of <1 cup/month decreased it (adjusted odds ratio (AOR) 1.64, AOR 1.19, AOR 0.89, respectively, p-trend 0.035) [76]. The consumption of hot and decaffeinated coffee was not associated with CRC. As the authors admitted, the results of their study were inconsistent with other reports, which may have been caused by different methods of preparing coffee in Australia and in Europe, where most case–control studies have been performed. Green et al. observed that consumption of hot coffee was associated with elevated risk of distal colon cancer for the whole range of consumption patterns (AOR 1.55 for <1 cup/day, AOR 1.91 for 1 cup/day, AOR 1.78 for ≥2 cups/day, p-trend 0.085). Additionally, the consumption of <1 cup/week and ≥1 cup/week of iced coffee was associated with significantly greater risk of rectal cancer (AOR 2.06, AOR 1.52, respectively, p-trend 0.004). The authors pointed out that iced coffee in Australia is pre-made with milk and sugar and presumed that additional sugar increases the risk of rectal cancer.
Yamada et al. found a statistically significant association between the consumption of coffee and the incidence of colorectal cancer in Japanese male patients in a prospective cohort study [77]. Men who consumed 2–3 cups or more than 4 cups of coffee per day faced a significantly higher risk of colorectal cancer (HR 1.21, HR 1.57, respectively, p-trend 0.03). Interestingly, this association was not significant in women (p-trend 0.61). The authors additionally distinguished subsite-related cancers. The association remained significant in both groups of men for colon cancer but not for rectal cancer (HR 1.26, p-trend 0.03; HR 1.79, p-trend 0.53, respectively).
Hu et al. and Guercio et al. conducted a prospective study on patients diagnosed with CRC and colon cancer. Both studies revealed an inverse association between post-diagnostic coffee consumption and CRC-related as well as overall mortality. Guercio et al. analyzed patients with stage III colon cancer during chemotherapy [78]. Patients consuming 4 or more cups of total and caffeinated coffee per day had significantly lower hazard ratios for colon cancer recurrence or mortality risk (HR 0.58, p-trend 0.002; HR 0.48, p-trend 0.002, respectively) when compared to non-coffee-drinkers. Additionally, increasing caffeine intake was related to a significant reduction of cancer recurrence or mortality. The consumption of decaffeinated coffee had no impact on patients’ outcomes. Similar results have been obtained by Hu et al. [79]. Patients consuming 4 cups of coffee per day had a significantly lower risk of CRC-related as well as all-cause death ratios (HR 0.48, p-trend 0.003; HR 0.70, p-trend < 0.001, respectively). Contrary to the results from Guercio et al.’s study, the trend was significant both for caffeinated and decaffeinated coffee. The anticancer effect was dose-dependent. The assessment of correlation of coffee consumption and specific cancer-related death ratios by Gapstur et al. showed a dose-dependent inverse association of CRC-related deaths for caffeinated and decaffeinated coffee [80]. The results from those studies indicated the anticancer activity of coffee: However, according to prospective studies, coffee inhibited developed tumors rather than prevented cancer incidence and may have been an effective adjuvant during chemotherapy.
Table 1 presents the calculated risk coefficients for colorectal cancer for coffee consumption and the level of the model’s significance for reviewed studies. Please note that the groups in each study were adjusted for specific features. Some information was provided in this article for the sake of legibility of the table. Check the original manuscripts for more information.

Table 1.
The association between colorectal cancer risk and coffee consumption with risk coefficients for investigated coffee intake. Case–control and prospective cohort studies are distinguished with symbols.
The results of case–control and cohort studies have been compared and summarized in several meta-analyses. A meta-analysis of case control studies by Galeone et al. revealed a significant inverse association between coffee consumption and the risk of CRC (OR 0.83, p < 0.001), as well as subsite colon and rectal cancers: However, odds ratios were close to 1 (OR 0.93, p < 0.001; OR 0.98, p < 0.001, respectively) [81]. A more specific meta-analysis was conducted by Horisaki et al. The authors compared cohort and case–control studies conducted on a Japanese population and found that pooled CRC risk increased with coffee consumption in cohort studies and decreased in case–control studies: However, none of the associations were statistically significant [82]. Another meta-analysis of Japanese cohort studies was performed by Kashino et al. No association for CRC was found in men and women: However, colon cancer risk had a significant inverse association with the amount of coffee consumed by women [83]. Tian et al. prepared a meta-analysis of both case-control and cohort studies with dose-response analysis. The results of this study showed a significant nonlinear inverse association between coffee consumption and CRC risk in case–control studies, with reduced risk of CRC in patients consuming at least 4 cups of coffee (OR 0.89, p < 0.01) and an insignificant nonlinear inverse relationship in cohort studies [84]. Similar results were obtained in a study by Li et al. Combined results of case–control studies showed a significant inverse correlation of coffee consumption and colorectal and colon cancer risk in highest versus lowest or no coffee consumption (OR/RR 0.85, p < 0.001; OR/RR 0.79, p < 0.001, respectively), while an inverse correlation in cohort studies was marginal and insignificant [2]. A meta-analysis of prospective cohort studies performed by Je et al. showed no significant difference between patients with high and low consumption of coffee and the risk of colorectal, colon, and rectal cancer (RR 0.91, p = 0.73; RR 0.90, p = 0.43; RR 0.98, p = 0.70, respectively) [85]. The dose-response relation was also calculated in a meta-analysis of prospective cohort studies by Gan et al. The authors found a nonlinear inverse association that was significant for consumption of more than 5 cups of coffee per day [86]. The consumption of 4 cups per day reduced the risk of CRC by 7%, whereas the inverse association was stronger at higher levels of coffee intake. A meta-analysis performed within the Continuous Update Project, analyzing research on cancer prevention and survival, performed by Norat et al., found no significant associations between coffee consumption and the risk of colorectal, colon, and rectal cancer in pooled and stratified groups [87].
There has been no clear association between coffee consumption and the risk of colorectal and subsite-related cancers in case–control studies, while prospective cohort studies have been rather unambiguous in that respect and have shown no relationship. Interestingly, almost all inverse and only a few positive associations of CRC risk and coffee consumption have been statistically significant. Also, the results of meta-analyses have been in accordance with case–control and cohort studies. Additionally, a distinction between caffeinated and decaffeinated coffee has been revealed, with a significant inverse correlation for decaffeinated coffee. This may indicate that caffeine is not the most crucial bioactive compound of coffee in preventing colorectal cancer.
3. Caffeine
Caffeine (1,3,7-trimethylxanthine) is a purine alkaloid. Its content in roasted robusta beans is twice as high as in Arabica (2.5% vs. 1.2% dry weight) [51]. Stavric et al., Lelo et al., and Gillbert et al. have shown that caffeine content in a cup of coffee varies between 84 mg and 112 mg [88,89,90]. Caffeine content is strongly correlated with the method of coffee preparation. A cup of drip or percolated coffee contains 84 or 82 mg of caffeine, respectively. A single shot of espresso may contain 40–116 mg of caffeine [91]. The caffeine level in plasma in people drinking up to 6 cups of coffee varies and can reach 2–6 mg/L [89]. On the other hand, Elmenhorst et al. have shown that the consumption of 3 cups of coffee leads to caffeine levels in plasma equal to 8–10 mg/L [92]. The main problem of correlation between epidemiological and in vitro studies is the frequent occurrence of using high pharmacological rather than physiological doses of caffeine in the in vitro studies [93].
Caffeine is an antagonist of phosphodiesterases [94,95] and adenosine receptors A1, A2A, and A2B [96,97], which has the effect of stimulating the central nervous system by increasing the release of dopamine, noradrenaline, and glutamate [98,99]. Moreover, it may accelerate heart rate: It also increases systolic and diastolic blood pressure and dilates blood vessels [95,100,101,102,103,104]. It also may reduce myocardial blood flow by inhibiting adenosine receptors in blood vessels [104], and reduce cerebral blood flow as well [105]. An in vitro study by Mitani et al. showed that caffeine may suppress lipid accumulation in adipocytes by inhibiting the secretion of inflammatory cytokines [106].
Caffeine is metabolized in the liver by CYP1A2, an isoform of cytochrome P450, and N-acetyltransferase 2 (NAT2) [9]. The activity of CYP1A2 and NAT2 varies widely between subjects and depends on genetic background (single nucleotide polymorphisms (SNPs)) and environmental factors such as ethnicity and diet [107,108,109]. Smoking has the strongest impact on CYP1A2 activity [110,111], however. The first products of metabolism are paraxanthine, theobromine, and theophylline [112], but the final major metabolites are 1-methylxanthine, 1-methylurate, and 5-acetylamino-6-formylamino-3-methyluracil [113]. Just a small amount of ingested caffeine (about 0.5–2%) is excreted unchanged with urine. The highest level of caffeine in plasma occurs 15 to 60 min after intake [113], and its half-life varies between 2 and 12 h [113,114]. The half-life of caffeine is also affected by such factors as cigarette smoking, sex, age, use of oral contraceptives, and pregnancy. For example, during pregnancy the half-life of caffeine increases [113,114,115], whereas smoking accelerates the metabolism of caffeine, leading to its shortened half-life [113]. Moreover, diet may also affect caffeine metabolism. The consumption of carrots, parsnips, dill, celery, and parsley slows down caffeine metabolism, in contrast to brassica vegetables such as broccoli, cauliflower, radish sprouts, and cabbage [113]. It must also be remembered that caffeine biotransformation depends on variations in CYP1A2 enzyme activity [116,117].
The Impact of Caffeine on Cancer Cell Progression In Vitro
Saito et al. demonstrated that caffeine increased cell growth inhibition and apoptosis rate in HCT116, SW480, and DLD-1 human CRC cell lines transfected by the PTEN suppressor gene [118]. Treatment with combinations of Ad-PTEN (adenovirus mediated PTEN gene transfer) and caffeine selectively induced the synergistic suppression of cell growth and apoptosis in colorectal cancer cells, but not in normal cells, through abrogation of G2/M arrest, downregulation of the Akt pathway, and modulation of the p44/42MAPK pathway. PTEN (phosphatase and tensin homolog deleted on chromosome ten) is a suppressor gene (locus 10q23.31). In many studies, PTEN has shown the ability to inhibit cell proliferation via apoptosis boost and increase cycle cell arrest at the G1 phase [115,116,117]. In the above-mentioned experiment, the authors observed a significant increase in cells in the sub-G0/G1 phase, particularly in HCT116 p53 (+/+) cells treated by a combination of caffeine and Ad-PTEN (13.05% of apoptotic cells in combined treatment, compared to 7.96% in cells transduced solely with Ad-PTEN) [118]. Merighi et al. have shown that caffeine significantly inhibited adenosine-induced HIF-1alpha protein accumulation in colorectal cancer cells cultured in hypoxic conditions [93]. Moreover, the pretreatment of cells with caffeine significantly reduced adenosine-induced VEGF promoter activity and VEGF and IL-8 expression. The mechanism of caffeine action seemed to involve the inhibition of the extracellular signal-regulated kinase 1/2 (ERK1/2), p38, and Akt, leading to a marked decrease in adenosine-induced HIF-1α accumulation, VEGF transcriptional activation, and VEGF and IL-8 protein accumulation. In this case, caffeine treatment resulted in a decrease in proliferation and migration potential in HT29 colorectal carcinoma cells. Choi et al. investigated the sensitivity of RKO colorectal carcinoma to radiotherapy in vitro [119]. They showed that caffeine at 3 mM concentration increased the sensitivity to radiation in RKO cells. They also demonstrated that caffeine reduced the activation of ATM kinase induced by radiation. As a result, it reduced the accumulation of cells in the G2 phase. Interestingly, Mhaidat et al. assessed the impact of 20 μM of caffeine administered to Colo205 colorectal cancer cells in vitro and their influence on paclitaxel-induced apoptosis [120]. Apparently, they found no difference in apoptosis when compared to the untreated control, together with induction of the MEK/ERK kinase survival pathway. The addition of caffeine to cells treated with paclitaxel (chemotherapeutic drug) changed the induced apoptosis from ~35% apoptotic cells after paclitaxel treatment to ~18% only, with paclitaxel and caffeine administration applied simultaneously. The administration of caffeine only increased the level of anti-apoptotic Mcl-1 and GRP78 proteins: However, the anti-apoptotic mechanism was inefficient when the authors pretreated the cells with chemical MEK inhibitor.
In vitro research may not fully reflect more complex relationships in organisms due to using high concentrations of compounds that cannot be physiologically achieved in human body. The intensity of in vitro research concerning caffeine in colorectal cancer has declined in recent years in favor of epidemiological studies.
4. Caffeic Acid
CA is one of the metabolites of chlorogenic acid (CGA) [121,122]. It is sometimes mistaken for caffeine, although its similarity ends in the name and occurrence. CA and CGA are nonflavonoid catecholic compounds [123] and have strong antioxidant properties [121,124]. CA occurs mostly in coffee beans, vegetables, and fruits [125,126], and 95% of caffeic acid is absorbed in the small intestine [127]. CA has been shown to possess anti-inflammatory, anticancerogenic, and enzyme-inhibiting properties (e.g., lipoxygenases, cyclooxygenases) [126]. The concentration of caffeic acid in coffee depends on the content of chlorogenic acids, and ranges from 96 to 1236 mg per average cup of coffee [128]. Monteiro et al. and Nardini et al. have reported mean concentrations of 1.6 μmol/L after 1.4 h after consumption and 20.9 ng/mL after 1 h, respectively [129,130].
Murphy et al. have analyzed pre-diagnostic concentrations of caffeic acid in serum [131]. There was no difference between patients diagnosed with CRC and healthy controls (median 430 vs. median 427 nmol/L, respectively, p = 0.93). The multivariable model demonstrated no relationship between CA concentration in serum and colon cancer risk. CA and CGA also have the ability to inhibit H2O2- and TNF-α-induced IL-8 production in human colorectal Caco-2 cell lines [132].
The Impact of CA on Cancer Cell Progression In Vitro
Murad et al. have determined the influence of different concentrations and exposure time on caffeic acid (CA) and 5-Caffeoylquinic acid on the viability and apoptosis of human colon carcinoma cells HT-29 [133]. A maximum uptake of CA was observed after 2 h of incubation. Inhibition of growth depended on different exposure times and concentration of CA: 24 h of exposition to 20, 40, and 80 μM caused 20–30% growth inhibition, 48 h of exposition on a 1.25–20 μM range caused ~25% growth inhibition, while 40 and 80 μM of CA caused ~40% inhibition. About 20–25% of inhibition was observed for 1.25–5 μM of CA and about 60% for 10–80 μM after 72 h of exposure. A whole range of concentrations caused 50–65% growth inhibition after 96 h incubation: However, the effect was not linear.
Interestingly, the highest inhibition during 96 h exposure was observed for 1.25 and 2.5 μM of CA, whereas for shorter times it was 20–80 μM. In addition, 48 h treatment with 5 μM of CA increased the number of cells in the G0/G1 phase, with no changes in G2/M, while 10 μM caused both an increase in the G0/G1 phase and a decrease in G2/M. Oleaga et al. found changes in the expression of STAT5B and ATF-2 in human carcinoma cells HT29 exposed to CA [134]. STAT5B overexpression and decreased levels of ATF-2 levels were confirmed in tested cells treated with CA, as compared to the control, untreated cells [135,136]. STAT5B plays a crucial role in colorectal cancer, taking part in cell growth, cell cycle progression, and apoptosis of CRC cells [137]. Inhibition of STAT5 induces G1 cell cycle arrest, but its overexpression may result in increased apoptosis [137,138]. Decreased levels of ATF-2 may have an anticancer action, as this protein is correlated with invasion, migration, proliferation, and DNA-damaging agents resistance in human breast cancer cells in vitro [134].
Sang Joon Lee et al. coupled CA with chitosan [139]. Chitosan itself, like caffeic acid, reveals antitumor activity [140]. Chito-CA conjugates dose-dependently reduced the viability of CT26 tumor cells and induced apoptosis and necrosis in cultures by means of an unknown mechanism. Furthermore, chito-CA conjugates also decreased the invasion of tested cells in in vitro conditions [139]. The inhibitory effect of CA on cancer cells and its mechanisms has been reported, but those observations were made in cells other than colorectal cancer ones (leukemia), as well as in normal human umbilical vein endothelial cells (HUVECs) [141].
5. Chlorogenic Acids
Chlorogenic acids are esters composed of quinic acid and one to four residues of certain trans-cinnamic acids. They belong to a group of plant polyphenols widely present in the human diet: Fruits, vegetables, coffee, tea, wine, and propolis [142,143]. Caffeoylquinic acid may theoretically have four isomers, but only three are present in plants and contain chlorogenic acid: 3-O-caffeoylquinic acid (3-CQA), neochlorogenic acid (5-O-caffeoylquinic acid, 5-CQA), or cryptochlorogenic acid (4-O-caffeoylquinic acid, 4-CQA). The most popular isomer, 5-CQA, is called chlorogenic acid (PubChem CID: 1794427CGA, CGA). It is an ester composed of caffeic acid and (−)-quinic acid [144]. The major source of chlorogenic acid in human diet is coffee, and its ingestion varies, depending on daily coffee consumption: Coffee drinkers ingest 0.5–1 g, while coffee abstainers ingest less than 100 mg of it per day [134]. Olthof et al. determined that about one-third of chlorogenic acid is absorbed intestinally [127], while the remaining two-thirds reach the colon and are most likely hydrolyzed to caffeic acid by colon cancer cells [145,146]. Epidemiological studies performed by Farah et al., Stalmach et al., and Renouf et al. have confirmed that caffeic acid isomers 3-CQA, 4-CQA, and 5-CQA are present in plasma and urine after consumption of coffee [147,148,149,150]. The concentration of chlorogenic acids in plasma and urine depends on ingested doses of coffee, but the results have been inconsistent. Some researchers have reported high amounts of intact 3-, 4-, and 5-CQA [129,147], while others have reported their absence [130,148]. Monteiro et al. showed the mean total CQA concentration to have been at 4.89 μmol/L for 4 h after consumption of coffee, while Farah et al. showed the mean concentration of total CQA to have been at 8.2 μmol/L for 3 h after consumption of capsulated decaffeinated green coffee extract [129,147]. CQA concentrations in serum after drinking green coffee bean extract were also measured by Matsui et al. The mean concentrations of 3-, 4-, and 5-CQA after 1 h from ingestion were 3.91, 6.81, and 7.39 ng/mL, respectively [151].
It is still disputed whether chlorogenic acid prevents or induces DNA damage. Some researchers have claimed it has a protective effect against free radical induced DNA oxidation in human colon HT29 and liver HepG2 cancer cell lines, human red blood cells, and human blood lymphocytes [152,153,154], while Xu et al. has confirmed antioxidant and DNA-protective action of 5-CQA and its isomers 3-CQA and 4-CQA [155]. On the other hand, a study by Burgos-Morón revealed that micromolar concentrations of chlorogenic acid generated DNA damage [156]. DNA damage was also observed by Li and Trush, Zheng et al., and Fan et al., but its damaging potential was quite low and increased in the presence of Cu(II) ions [157,158,159]. DNA damage, especially double-strand breaks and interstrand crosslinks, may be caused by many factors, such as the presence of reactive oxygen species and chemical compounds, or it may occur during physiological processes taking place in cells [160,161]. Both unrepaired and abnormally repaired double-strand breaks may cause rearrangements of chromosomes and loss of heterozygosity, which may result in cancer or cell death. Double-strand breaks may be repaired by nonhomologous end joining (NHEJ) and its variants or homologous recombination. Unregulated homologous recombination is one potential cancer promoter. Mutations of many homologous recombination genes have been reported in different cancers, including a mutation of the RAD54 gene in colon cancer, which leads to the conclusion that flawed DNA damage response and homologous recombination defects cause cancer and are common in cancer cells [160,162]. The inhibition of proteins involved in DNA repair is used in anticancer therapy [163].
The Impact of Chlorogenic Acid and Its Isomers on Cancer Cell Progression In Vitro
The number of research studies concerning CGA in colorectal cancer in vitro is still limited. Hou et al. assessed the influence of CGA on the viability of two human colorectal cancer cell lines, HCT116 and HT29, and CGA-induced ROS production in vitro [164]. They found that cell viability decreased in a dose-dependent manner for both tested cell lines. Cell viability was measured with MTT assay after 72 h exposure to CGA. There, 250 μmol/L of CGA caused the decrease of viability by ~36.0% and ~25.22% in HCT116 and HT29 cells, respectively. The highest assessed concentration, 1000 μmol/L, caused viability reduction by 50.1% and 55.2% for HCT116 and HT29 cells, respectively. The intracellular ROS level was measured using 5- (and 6-)chloromethyl-2′,7′-dichlorodihydroflurorescein diacetate (CM-H2DCFDA) and fluorescence microscopy. There, 250 μmol/L of CGA increased the ROS level by about 30% or 20%, while 1000 μmol/L increased the production of ROS by ~110% and ~90% in HCT116 and HT29 cells, respectively, when compared to the untreated control. The authors investigated cell cycle changes using PI and found that CGA induced cell arrest in phase S. Western blot analysis demonstrated the inactivation of phosphorylated ERK and increased levels of phosphorylated p53 in both lines treated with both concentrations of CGA. As the authors stated, S-phase arrest and inactivation of ERK may explain the lower viability of CGA-treated cells. Inhibition of the proliferation of the Caco-2 cell line was also found in a study performed by Wang et al. [165]. Wang et al. found an inhibition of proliferation in Caco-2 and HepG2 cells in vitro after administration of chlorogenic acid, with a median effective dose of (EC50) 2.8 ± 0.7 μg and 2.3 ± 1.1 μg, respectively. Sato et al. demonstrated that CGA and CA demonstrated antioxidant activity in human colon cancer cell line Caco-2 in a dose-dependent manner [121]. Antioxidant activity was measured using total antioxidant performance (TAP) and 2-methyl-6-p-methoxyphenylethynylimidazopyrazynone (MPEC) tests.
Interestingly, Xavier et al. found no change in viability or decrease of the level of phosphorylated Akt and ERK protein kinases in HCT15 and CO115 colorectal cancer cells after administration of different concentrations of CGA [166]. CGA concentrations were between 10 and 200 μmol/L, so they were lower than those in the study performed by Hou et al. [164], but partly similar as well. Viability was assessed with MTT assay, but the differences were not significant for any concentration. The level of phosphorylated Akt or ERK protein kinases was assessed with Western blot after administration of CGA (10 and 100 μmol/L), which caused no decrease of their levels in any cell line. Viability inhibition of HT-29 cells was observed by Murad et al. after 96 h of 5-CQA treatment, while shorter times of exposure (24, 48, 72 h) showed no significant differences throughout the range of concentrations (1.25–80 μM) [134]. Doses of 5 and 10 μM of 5-CQA increased the percentage of cells in the G0/G1 phase and decreased the number of cells in the G2/M phase after 48 and 96 h of exposure. The same concentrations increased the apoptosis to 1.6- and 1.8-fold after 48 h of exposure. Early apoptosis was observed in cells treated with a 5 μM dose, while late apoptotic cells were observed after treatment with a 10 μM dose.
Other studies performed in CGA-treated leukemia and hepatocellular cancer cell lines in vitro have also revealed similar results [156,167,168,169,170]. The authors stated that CGA may be a chemo-sensitizing agent during chemotherapy of selected cancers due to inactivation of ERK by overproduction of ROS.
6. Kahweol
Kahweol is a coffee-specific diterpene present in coffee beans and unfiltered coffee beverages [171,172]. Kahweol is a fat-soluble factor present in Arabica coffee beans oil, and its concentration in coffee ranges from 0.1 to 7 mg/mL [173,174]. According to a study by de Roos et al., about 70% of ingested kahweol is absorbed in humans [175]. It acts both as an adverse and chemoprotective factor [47,175]. Kahweol is known to increase the level of blood cholesterol in animal and human models [175]. On the other hand, it protects against carcinogens such as aflatoxin B1, 2-amino-l-methyl-6-phenylimidazo[4,5-b]-pyridine, and 2-amino-l-methyl-6-phenylimidazo[4,5-b]-pyridine [46,48,176].
The Impact of Kahweol on Cancer Cell Progression In Vitro
Choi et al. studied the impact of different concentrations (up to 200 μM) of kahweol, caffeine, CA, and CG on human colorectal cancer cells HT-29 [177]. Interestingly, the mere exposition to kahweol decreased the viability of cells and induced cell rounding, detachment, and lactate dehydrogenase (LDH) release in a dose-dependent manner when compared to the untreated control. The authors analyzed the level of apoptosis-related proteins using Western blot analysis. Treatment with kahweol increased the expression of pro-apoptotic-activated caspase-3 and cleaved poly ADP-ribose polymerase (PARP), simultaneously decreasing the expression of anti-apoptotic Bcl-2 and phosphorylated Akt in a dose-dependent manner. Additionally, the exposure to kahweol caused decreased expression of heat shock protein 70 (HSP 70), the protein known to promote epithelial-mesenchymal transition, to be overexpressed in tumors, and to promote their growth [178,179,180]. The authors found that HSP 70 played an important role in cytotoxicity caused by kahweol. HSP 70 expression caused a significant decrease in the expression of cleaved PARP and activated caspase-3 and turned out to increase the expression of Bcl-2 and phosphorylated Akt. The viability of cells pretreated with HSP 70 inhibitor triptolide and treated with kahweol was significantly lower than the viability of those treated with kahweol only. The impact of kahweol on human colorectal cancer cells HCT116 and SW480, and on human colon normal cells CCD-18C0, was also assessed by Park et al. [181]. The cells were treated with different concentrations of kahweol, up to 50 μM. Kahweol significantly inhibited cell growth in a time- and dose-dependent manner in both lines, but the inhibition was greater in HCT116 than in SW480 cells. Interestingly, the exposition to kahweol did not affect the proliferation of normal colon cells CCD-18Co, which may indicate cancer-specific antiproliferative activity. Using Western blot, the authors found out that kahweol treatment significantly attenuated the level of cyclin D1, which is a regulatory protein in G1-to-S phase transitions. Cyclin D1 is not expressed in normal colorectal tissue, but its overexpression has been confirmed in many cancers, including colorectal carcinoma [182,183]. The occurrence of cyclin D1 in colorectal tumors is correlated with high-grade cancer with metastases to lymph nodes and deeper invasion [184]. Patients with cyclin D1-positive expression colorectal cancer have a poorer prognosis and shorter survival [184,185]. Kahweol-induced inhibition of cyclin D1 expression is presumed to be a chemoprevention for colorectal cancer. Park et al. have observed that kahweol did not affect the levels of cyclin D1 mRNA and its promoter activity [181]. Unaffected levels of mRNA and decreased protein levels indicated proteasomal degradation of cyclin D1, which was confirmed in cells pretreated with proteasome inhibitor MG132. MG132 blocked kahweol-induced decreases of cyclin D1 protein levels. The authors stated that kahweol may decrease cyclin D1 protein stability, as it significantly reduced its half-life in HCT116 cells. Further analysis of cyclin D1 proteasomal degradation included pretreating HCT116 cells with inhibitors of ERK1/2, p38, JNK, IκK-α, and inhibitors of GSK3β kinases. Kahweol-mediated cyclin D1 degradation was decreased after inhibition of ERK1/2, JNK, or GSK3β. Additionally, kahweol induced phosphorylation of ERK1/2, JNK, and GSK3β. The activation of those kinases may induce threonine-286 phosphorylation of cyclin D1 and proteasomal degradation, which follows. Unfortunately, the authors did not provide any analysis of cell cycles, where the role of cyclin D1 is crucial. Park et al. conducted other research on human colorectal cancer cell lines HCT116, SW480, LoVo, and HT-29 treated with kahweol [186]. In that research, they analyzed the impact of kahweol on apoptosis. The administration of 50 μM of kahweol for 24 h significantly induced the cleaved PARP in all cell lines, which may indicate that kahweol may induce apoptosis. Using Western blot, the authors assessed the level of activating transcription factor 3 (ATF3), the protein known to act as a tumor suppressor in colorectal cancer. Its expression may lead to downregulation of the expression of MMP-2 [187] and cyclin D1, suppression of Ras-mediated tumorigenesis [188], and enhanced activation of the p53 protein [189]. The exposure to different concentrations of kahweol generated dose-dependent increases of ATF3 in HCT116 cells, while the administration of 50 μM significantly increased ATF3 levels in all cell lines, when compared to the untreated control. Using RT-PCR, the authors measured the level of mRNA of ATF3 and found that the kahweol-induced increase of ATF3 mRNA levels was similar to kahweol-induced ATF3 protein levels. The authors pretreated CHT116 cells with inhibitors of ERK1/2, p38, JNK, and GSK3β. It was only the inhibition of ERK1/2 and GSK3β kinases that lowered the kahweol-induced ATF3 expression, which points out their impact on ATF3 expression.
It is important to remember that none of the compounds investigated in in vitro studies have been involved in epidemiological research.
Table 2 and Figure 2 summarize the current state of knowledge about the impact of caffeine, CA, CGAs, and kahweol on colorectal cancer cells in vitro with corresponding mechanisms.

Table 2.
Potential mechanisms of caffeine, caffeic acid, chlorogenic acids, and kahweol on antitumor activity.
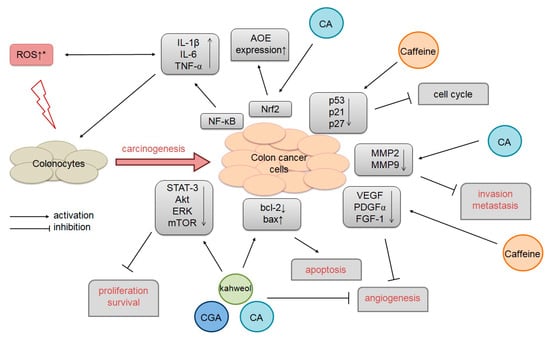
Figure 2.
The potential mechanism of caffeine and nonflavonoid catecholic compound influence on colorectal cancer. (*) ROS leads to spontaneous goblet cell dysfunction, impaired mucosal barrier function, and inflammation, and exacerbates the development of pathology (such as cancer). CA: Caffeic acid; CGA: Chlorogenic acid.
7. Conclusions
The content of bioactive compounds in coffee depends on many conditions, such as coffee species, the plantation where the coffee was grown, bean roasting time and procedure, grinding, and preparation method [32,33,34,35].
The impact of coffee on colorectal cancer has been investigated in many epidemiological studies. Statistically significant positive and inverse associations were found for colorectal and subsite-related cancers in various case–control research papers, but some results were significant in pooled groups, while others only after adjusting for sex. Significant inverse associations for decaffeinated coffee indicates that caffeine has a lower impact on CRC in vivo than it was reported in the in vitro studies. On the other hand, prospective cohort studies found no correlation.
The results of the presented in vitro studies revealed that selected compounds, namely caffeine, CA, CGAs, and kahweol, turned out to diminish the growth of human colorectal cancer cell lines, mainly by cell phase arrest and apoptosis boost. The in vitro setting of the studies must be kept in mind, as it may not have fully reflected the more complex relationships in the organism as a whole. The results may not have been identical to those observed in living subjects due to lack of physiological processes such as accumulation in tissues, the influence of individual human gut microbiota, or intolerance to certain foods. Additionally, concentrations of bioactive compounds or exposure times in the in vitro studies may have been inadequate for in vivo conditions. The results obtained from epidemiological studies of eating habits such as coffee consumption and colorectal cancer risk have not been consistent, possibly because of attenuation of associations due to measurement errors in dietary exposure determination.
Funding
The article processing charges has been covered from funds of Polish Ministry of Science and Higher Education.
Acknowledgments
None to declare.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Frost-Meyer, N.J.; Logomarsino, J.V. Impact of coffee components on inflammatory markers: A review. J. Funct. Foods 2012, 4, 819–830. [Google Scholar] [CrossRef]
- Li, G.; Ma, D.; Zhang, Y.; Zheng, W.; Wang, P. Coffee consumption and risk of colorectal cancer: A meta-analysis of observational studies. Public Health Nutr. 2013, 16, 346–357. [Google Scholar] [CrossRef] [PubMed]
- Bresciani, L.; Calani, L.; Bruni, R.; Brighenti, F.; Del Rio, D. Phenolic composition, caffeine content and antioxidant capacity of coffee silverskin. Food Res. Int. 2014, 61, 196–201. [Google Scholar] [CrossRef]
- Cheng, Y.-C.; Sheen, J.-M.; Hu, W.L.; Hung, Y.-C. Polyphenols and Oxidative Stress in Atherosclerosis-Related Ischemic Heart Disease and Stroke. Oxid. Med. Cell. Longev. 2017, 2017, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Guasch-Ferré, M.; Merino, J.; Sun, Q.; Fitó, M.; Salas-Salvadó, J. Dietary Polyphenols, Mediterranean Diet, Prediabetes, and Type 2 Diabetes: A Narrative Review of the Evidence. Oxid. Med. Cell. Longev. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Witkowska, A.M.; Waśkiewicz, A.; Zujko, M.E.; Szcześniewska, D.; Pająk, A.; Stepaniak, U.; Drygas, W. Dietary Polyphenol Intake, but Not the Dietary Total Antioxidant Capacity, Is Inversely Related to Cardiovascular Disease in Postmenopausal Polish Women: Results of WOBASZ and WOBASZ II Studies. Oxid. Med. Cell. Longev. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Freyssin, A.; Page, G.; Fauconneau, B.; Bilan, A.R. Natural polyphenols effects on protein aggregates in Alzheimer’s and Parkinson’s prion-like diseases. Neural. Regen. Res. 2018, 13, 955–961. [Google Scholar] [PubMed]
- Ravi, S.K.; Narasingappa, R.B.; Vincent, B. Neuro-Nutrients as Anti-Alzheimer’s Disease Agents: A Critical Review. Crit. Rev. Food Sci. Nutr. 2018. [Google Scholar] [CrossRef] [PubMed]
- Dik, V.K.; Bueno-de-Mesquita, H.B.; Van Oijen, M.G.H.; Siersema, P.D.; Uiterwaal, C.S.P.M.; Van Gils, C.H.; Van Duijnhoven, F.J.B.; Cauchi, S.; Yengo, L.; Froguel, P.; et al. Coffee and tea consumption, genotype-based CYP1A2 and NAT2 activity and colorectal cancer risk-Results from the EPIC cohort study. Int. J. Cancer 2014, 135, 401–412. [Google Scholar] [CrossRef] [PubMed]
- Poole, R.; Kennedy, O.J.; Roderick, P.; Fallowfield, J.A.; Hayes, P.C.; Parkes, J. Coffee consumption and health: Umbrella review of meta-analyses of multiple health outcomes. BMJ 2017, 360. [Google Scholar] [CrossRef] [PubMed]
- Gunter, M.J.; Murphy, N.; Cross, A.J.; Dossus, L.; Dartois, L.; Fagherazzi, G.; Kaaks, R.; Kühn, T.; Boeing, H.; Aleksandrova, K.; et al. Coffee Drinking and Mortality in 10 European Countries. Ann. Intern. Med. 2017, 167, 236–247. [Google Scholar] [CrossRef] [PubMed]
- Kempf, K.; Herder, C.; Erlund, I.; Kolb, H.; Martin, S.; Carstensen, M.; Koenig, W.; Sundvall, J.; Bidel, S.; Kuha, S.; et al. Effects of coffee consumption on subclinical inflammation and other risk factors for type 2 diabetes: A clinical trial. Am. J. Clin. Nutr. 2010, 91, 950–957. [Google Scholar] [CrossRef] [PubMed]
- Bøhn, S.K.; Blomhoff, R.; Paur, I. Coffee and cancer risk, epidemiological evidence, and molecular mechanisms. Mol. Nutr. Food Res. 2014, 58, 915–930. [Google Scholar] [CrossRef] [PubMed]
- Yovana, M.; Brígida, M.; Bragagnolo, N. Physical characteristics of the paper filter and low cafestol content filter coffee brews. Food Res. Int. 2018, 108, 280–285. [Google Scholar]
- Loftfield, E.; Freedman, N.D.; Graubard, B.I.; Guertin, K.A.; Black, A.; Huang, W.-Y.; Shebl, F.M.; Mayne, S.T.; Sinha, R. Association of Coffee Consumption With Overall and Cause-Specific Mortality in a Large US Prospective Cohort Study. Am. J. Epidemiol. 2015, 182, 1010–1022. [Google Scholar] [CrossRef] [PubMed]
- Zampelas, A.; Panagiotakos, D.B.; Pitsavos, C.; Chrysohoou, C.; Stefanadis, C. Associations between coffee consumption and inflammatory markers in healthy persons: The ATTICA study. Am. J. Clin. Nutr. 2004, 80, 862–867. [Google Scholar] [CrossRef] [PubMed]
- Paiva, C.; Beserra, B.; Reis, C.; Dorea, J.; Da Costa, T.; Amato, A. Consumption of coffee or caffeine and serum concentration of inflammatory markers: A systematic review. Crit. Rev. Food Sci. Nutr. 2017, 57, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Barnung, R.B.; Nøst, T.H.; Ulven, S.M.; Skeie, G.; Olsen, K.S. Coffee consumption and whole-blood gene expression in the Norwegian women and cancer post-genome cohort. Nutrients 2018, 10, 1047. [Google Scholar] [CrossRef] [PubMed]
- Paur, I.; Balstad, T.R.; Kolberg, M.; Pedersen, M.K.; Austenaa, L.M.; Jacobs, D.R.; Blomhoff, R. Extract of Oregano, Coffee, Thyme, Clove, and Walnuts Inhibits NF- B in Monocytes and in Transgenic Reporter Mice. Cancer Prev. Res. 2010, 3, 653–663. [Google Scholar] [CrossRef] [PubMed]
- Paur, I.; Balstad, T.R.; Blomhoff, R. Degree of roasting is the main determinant of the effects of coffee on NF-κB and EpRE. Free Radic. Biol. Med. 2010, 48, 1218–1227. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.; Jung, S.; Ko, K. Effects of Coffee Extracts with Different Roasting Degrees on Antioxidant and Anti-Inflammatory Systems in Mice. Nutrients 2018, 10, 363. [Google Scholar] [CrossRef] [PubMed]
- Corrêa, T.A.F.; Rogero, M.M.; Mioto, B.M.; Tarasoutchi, D.; Tuda, V.L.; César, L.A.M.; Torres, E.A.F.S. Paper-filtered coffee increases cholesterol and inflammation biomarkers independent of roasting degree: A clinical trial. Nutrition 2013, 29, 977–981. [Google Scholar] [CrossRef] [PubMed]
- Miranda, A.; Steluti, J.; Fisberg, R.; Marchioni, D. Association between Coffee Consumption and Its Polyphenols with Cardiovascular Risk Factors: A Population-Based Study. Nutrients 2017, 9, 276. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.F.; Jacobs, D.R.; Carlsen, M.H.; Blomhoff, R. Consumption of coffee is associated with reduced risk of death attributed to inflammatory and cardiovascular diseases in the Iowa Women’s Health Study. Am. J. Clin. Nutr. 2006, 83, 1039–1046. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Zhang, D.; Jiang, W. Coffee and caffeine intake and incidence of type 2 diabetes mellitus: A meta-analysis of prospective studies. Eur. J. Nutr. 2014, 53, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Ding, M.; Bhupathiraju, S.N.; Chen, M.; van Dam, R.M.; Hu, F.B. Caffeinated and Decaffeinated Coffee Consumption and Risk of Type 2 Diabetes: A Systematic Review and a Dose-Response Meta-analysis. Diabetes Care 2014, 37, 569–586. [Google Scholar] [CrossRef] [PubMed]
- Stutz, B.; Ahola, A.J.; Harjutsalo, V.; Forsblom, C.; Groop, P.; Group, S. Nutrition, Metabolism & Cardiovascular Diseases Association between habitual coffee consumption and metabolic syndrome in type 1 diabetes. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 470–476. [Google Scholar] [PubMed]
- Chuang, Y.H.; Quach, A.; Absher, D.; Assimes, T.; Horvath, S.; Ritz, B. Coffee consumption is associated with DNA methylation levels of human blood. Eur. J. Hum. Genet. 2017, 25, 608–616. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, T.; Oishi, K. Influence of coffee (Coffea arabica) and galacto-oligosaccharide consumption on intestinal microbiota and the host responses. FEMS Microbiol. Lett. 2013, 343, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Jaquet, M.; Rochat, I.; Moulin, J.; Cavin, C.; Bibiloni, R. International Journal of Food Microbiology Impact of coffee consumption on the gut microbiota: A human volunteer study. Int. J. Food Microbiol. 2009, 130, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Cuervo, A.; Hevia, A.; López, P.; Suárez, A.; Diaz, C.; Sánchez, B.; Margolles, A.; González, S. Phenolic compounds from red wine and coffee are associated with specific intestinal microorganisms in allergic subjects. Food Funct. 2016, 7, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Dong, W.; Tan, L.; Zhao, J.; Hu, R.; Lu, M. Characterization of Fatty Acid, Amino Acid and Volatile Compound Compositions and Bioactive Components of Seven Coffee (Coffea robusta) Cultivars Grown in Hainan Province, China. Molecules 2015, 20, 16687–16708. [Google Scholar] [CrossRef] [PubMed]
- Jeon, J.S.; Kim, H.T.; Jeong, I.H.; Hong, S.R.; Oh, M.S.; Park, K.H.; Shim, J.H.; Abd El-Aty, A.M. Determination of chlorogenic acids and caffeine in homemade brewed coffee prepared under various conditions. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2017, 1064, 115–123. [Google Scholar] [CrossRef] [PubMed]
- McCusker, R.R.; Goldberger, B.A.; Cone, E.J. Caffeine content of specialty coffees. J. Anal. Toxicol. 2003, 27, 520–522. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, I.A.; Mena, P.; Calani, L.; Cid, C.; Del Rio, D.; Lean, M.E.J.; Crozier, A. Variations in caffeine and chlorogenic acid contents of coffees: What are we drinking? Food Funct. 2014, 5, 1718–1726. [Google Scholar] [CrossRef] [PubMed]
- Guffey, C.R.; Fan, D.; Singh, U.P.; Murphy, E.A. Linking obesity to colorectal cancer. Curr. Opin. Clin. Nutr. Metab. Care 2013, 16, 595–600. [Google Scholar] [CrossRef] [PubMed]
- Fung, T.T.; Hu, F.B.; Schulze, M.; Pollak, M.; Wu, T.; Fuchs, C.S.; Giovannucci, E. A dietary pattern that is associated with C-peptide and risk of colorectal cancer in women. Cancer Causes Control 2012, 23, 959–965. [Google Scholar] [CrossRef] [PubMed]
- Fung, T.T.; Rimm, E.B.; Spiegelman, D.; Rifai, N.; Tofler, G.H.; Willett, W.C.; Hu, F.B. Association between dietary patterns and plasma biomarkers of obesity and cardiovascular disease risk. Am. J. Clin. Nutr. 2001, 73, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Giovannucci, E. Height, predictors of C-peptide and cancer risk in men. Int. J. Epidemiol. 2004, 33, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Kerver, J.M.; Yang, E.J.; Bianchi, L.; Song, W.O. Dietary patterns associated with risk factors for cardiovascular disease in healthy US adults. Am. J. Clin. Nutr. 2003, 78, 1103–1110. [Google Scholar] [CrossRef] [PubMed]
- Bobe, G.; Murphy, G.; Rogers, C.J.; Hance, K.W.; Albert, P.S.; Laiyemo, A.O.; Sansbury, L.B.; Lanza, E.; Schatzkin, A.; Cross, A.J. Serum Adiponectin, Leptin, C-Peptide, Homocysteine, and Colorectal Adenoma Recurrence in the Polyp Prevention Trial. Cancer Epidemiol. Biomark. Prev. 2010, 19, 1441–1452. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.K.; Koh-Banerjee, P.; Franz, M.; Sampson, L.; Grønbæk, M.; Rimm, E.B. Whole grains, bran, and germ in relation to homocysteine and markers of glycemic control, lipids, and inflammation. Am. J. Clin. Nutr. 2006, 83, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Loopstra-Masters, R.C.; Liese, A.D.; Haffner, S.M.; Wagenknecht, L.E.; Hanley, A.J. Associations between the intake of caffeinated and decaffeinated coffee and measures of insulin sensitivity and beta cell function. Diabetologia 2011, 54, 320–328. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Willett, W.C.; Hankinson, S.E.; Giovannucci, E. Caffeinated coffee, decaffeinated coffee, and caffeine in relation to plasma C-peptide levels, a marker of insulin secretion, in U.S. women. Diabetes Care 2005, 28, 1390–1396. [Google Scholar] [CrossRef] [PubMed]
- Würzner, H.-P.; Lindström, E.; Vuataz, L.; Luginbühl, H. A 2-year feeding study of instant. Coffees in rats. II. Incidence and types of neoplasms. Food Cosmet. Toxicol. 1977, 15, 289–296. [Google Scholar] [CrossRef]
- Stalder, R.; Bexter, A.; Würzner, H.P.; Luginbühl, H. A carcinogenicity study of instant coffee in Swiss mice. Food Chem. Toxicol. 1990, 28, 829–837. [Google Scholar] [CrossRef]
- Cavin, C.; Holzhaeuser, D.; Scharf, G.; Constable, A.; Huber, W.W.; Schilter, B. Cafestol and kahweol, two coffee specific diterpenes with anticarcinogenic activity. Food Chem. Toxicol. 2002, 40, 1155–1163. [Google Scholar] [CrossRef]
- Lee, K.J.; Jeong, H.G. Protective effects of kahweol and cafestol against hydrogen peroxide-induced oxidative stress and DNA damage. Toxicol. Lett. 2007, 173, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Soares, P.V.; Kannen, V.; Jordão Junior, A.A.; Garcia, S.B. Coffee, but Neither Decaffeinated Coffee nor Caffeine, Elicits Chemoprotection Against a Direct Carcinogen in the Colon of Wistar Rats. Nutr. Cancer 2018, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kang, N.J.; Lee, K.W.; Kim, B.H.; Bode, A.M.; Lee, H.-J.; Heo, Y.-S.; Boardman, L.; Limburg, P.; Lee, H.J.; Dong, Z. Coffee phenolic phytochemicals suppress colon cancer metastasis by targeting MEK and TOPK. Carcinogenesis 2011, 32, 921–928. [Google Scholar] [CrossRef] [PubMed]
- Ky, C.-L.; Louarn, J.; Dussert, S.; Guyot, B.; Hamon, S.; Noirot, M. Caffeine, trigonelline, chlorogenic acids and sucrose diversity in wild Coffea arabica L. and C. canephora P. accessions. Food Chem. 2001, 75, 223–230. [Google Scholar] [CrossRef]
- Guertin, K.A.; Loftfield, E.; Boca, S.M.; Sampson, J.N.; Moore, S.C.; Xiao, Q.; Huang, W.-Y.; Xiong, X.; Freedman, N.D.; Cross, A.J.; et al. Serum biomarkers of habitual coffee consumption may provide insight into the mechanism underlying the association between coffee consumption and colorectal cancer. Am. J. Clin. Nutr. 2015, 101, 1000–1011. [Google Scholar] [CrossRef] [PubMed]
- Dominianni, C.; Huang, W.; Berndt, S.; Hayes, R.B.; Ahn, J. Prospective study of the relationship between coffee and tea with colorectal cancer risk: The PLCO Cancer Screening Trial. Br. J. Cancer 2013, 109, 1352–1359. [Google Scholar] [CrossRef] [PubMed]
- Bidel, S.; Hu, G.; Jousilahti, P.; Antikainen, R.; Pukkala, E.; Hakulinen, T.; Tuomilehto, J. Coffee consumption and risk of colorectal cancer. Eur. J. Clin. Nutr. 2010, 64, 917–923. [Google Scholar] [CrossRef] [PubMed]
- Lukic, M.; Licaj, I.; Lund, E.; Skeie, G. Coffee consumption and the risk of cancer in the Norwegian Women and Cancer (NOWAC) Study. Eur. J. Epidemiol. 2016, 31, 905–916. [Google Scholar] [CrossRef] [PubMed]
- Terry, P. Coffee consumption and risk of colorectal cancer in a population based prospective cohort of Swedish women. Gut 2001, 49, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Mucci, L.A.; Adami, H.; Wolk, A. Prospective study of dietary acrylamide and risk of colorectal cancer among women. Int. J. Cancer 2006, 118, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Bergkvist, L.; Giovannucci, E.; Wolk, A. Coffee Consumption and Incidence of Colorectal Cancer in Two Prospective Cohort Studies of Swedish Women and Men. Am. J. Epidemiol. 2006, 163, 638–644. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, L.M.; Johansson, I.; Lenner, P.; Lindahl, B.; Van Guelpen, B. Consumption of filtered and boiled coffee and the risk of incident cancer: A prospective cohort study. Cancer Causes Control 2010, 21, 1533–1544. [Google Scholar] [CrossRef] [PubMed]
- Michels, K.B.; Willett, W.C.; Fuchs, C.S.; Giovannucci, E. Coffee, Tea, and Caffeine Consumption and Incidence of Colon and Rectal Cancer. JNCI J. Natl. Cancer Inst. 2005, 97, 282–292. [Google Scholar] [CrossRef] [PubMed]
- Naganuma, T.; Kuriyama, S.; Akhter, M.; Kakizaki, M.; Nakaya, N.; Matsuda-Ohmori, K.; Shimazu, T.; Fukao, A.; Tsuji, I. Coffee consumption and the risk of colorectal cancer: A prospective cohort study in Japan. Int. J. Cancer 2007, 120, 1542–1547. [Google Scholar] [CrossRef] [PubMed]
- Peterson, S.; Yuan, J.-M.; Koh, W.-P.; Sun, C.-L.; Wang, R.; Turesky, R.J.; Yu, M.C. Coffee Intake and Risk of Colorectal Cancer Among Chinese in Singapore: The Singapore Chinese Health Study. Nutr. Cancer 2009, 62, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Schmit, S.L.; Rennert, H.S.; Rennert, G.; Gruber, S.B. Coffee Consumption and the Risk of Colorectal Cancer. Cancer Epidemiol. Biomark. Prev. 2016, 25, 634–639. [Google Scholar] [CrossRef] [PubMed]
- Sinha, R.; Cross, A.J.; Daniel, C.R.; Graubard, B.I.; Wu, J.W.; Hollenbeck, A.R.; Gunter, M.J.; Park, Y.; Freedman, N.D. Caffeinated and decaffeinated coffee and tea intakes and risk of colorectal cancer in a large prospective study. Am. J. Clin. Nutr. 2012, 96, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z. Dietary polyphenols and colorectal cancer risk: The Fukuoka colorectal cancer study. World J. Gastroenterol. 2013, 19, 2683–2690. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Inoue, M.; Otani, T.; Iwasaki, M.; Sasazuki, S.; Tsugane, S. Coffee consumption and risk of colorectal cancer in a population-based prospective cohort of Japanese men and women. Int. J. Cancer 2007, 121, 1312–1318. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, K.; Kuriyama, S.; Akhter, M.; Kakizaki, M.; Nakaya, N.; Ohmori-Matsuda, K.; Shimazu, T.; Nagai, M.; Sugawara, Y.; Hozawa, A.; et al. Coffee Consumption and Mortality Due to All Causes, Cardiovascular Disease, and Cancer in Japanese Women. J. Nutr. 2010, 140, 1007–1013. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa-Senda, H.; Ito, H.; Hosono, S.; Oze, I.; Tanaka, H.; Matsuo, K. Coffee consumption and the risk of colorectal cancer by anatomical subsite in Japan: Results from the HERPACC studies. Int. J. Cancer 2017, 141, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Azzeh, F.S.; Alshammari, E.M.; Alazzeh, A.Y.; Jazar, A.S.; Dabbour, I.R.; El-Taani, H.A.; Obeidat, A.A.; Kattan, F.A.; Tashtoush, S.H. Healthy dietary patterns decrease the risk of colorectal cancer in the Mecca Region, Saudi Arabia: A case-control study. BMC Public Health 2017, 17. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Chan, D.S.M.; Vieira, A.R.; Navarro Rosenblatt, D.A.; Vieira, R.; Greenwood, D.C.; Kampman, E.; Norat, T. Red and processed meat intake and risk of colorectal adenomas: A systematic review and meta-analysis of epidemiological studies. Cancer Causes Control 2013, 24, 611–627. [Google Scholar] [CrossRef] [PubMed]
- Pham, N.M.; Mizoue, T.; Tanaka, K.; Tsuji, I.; Tamakoshi, A.; Matsuo, K.; Wakai, K.; Nagata, C.; Inoue, M.; Tsugane, S.; et al. Meat Consumption and Colorectal Cancer Risk: An Evaluation Based on a Systematic Review of Epidemiologic Evidence Among the Japanese Population. Jpn. J. Clin. Oncol. 2014, 44, 641–650. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, A.M.; Song, M.; Zhang, X.; Pan, A.; Wang, M.; Fuchs, C.S.; Le, N.; Chan, A.T.; Willett, W.C.; Ogino, S.; et al. Processed and Unprocessed Red Meat and Risk of Colorectal Cancer: Analysis by Tumor Location and Modification by Time. PLoS ONE 2015, 10. [Google Scholar] [CrossRef] [PubMed]
- Ananthakrishnan, A.N.; Du, M.; Berndt, S.I.; Brenner, H.; Caan, B.J.; Casey, G.; Chang-Claude, J.; Duggan, D.; Fuchs, C.S.; Gallinger, S.; et al. Red Meat Intake, NAT2, and Risk of Colorectal Cancer: A Pooled Analysis of 11 Studies. Cancer Epidemiol. Biomark. Prev. 2015, 24, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Mosli, M.H.; Al-Ahwal, M.S. Colorectal Cancer in the Kingdom of Saudi Arabia: Need for Screening. Asian Pac. J. Cancer Prev. 2012, 13, 3809–3813. [Google Scholar] [CrossRef]
- Groessl, E.J.; Allison, M.A.; Larson, J.C.; Ho, S.B.; Snetslaar, L.G.; Lane, D.S.; Tharp, K.M.; Stefanick, M.L. Coffee Consumption and the Incidence of Colorectal Cancer in Women. J. Cancer Epidemiol. 2016, 2016, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Green, C.J.; de Dauwe, P.; Boyle, T.; Tabatabaei, S.M.; Fritschi, L.; Heyworth, J.S. Tea, Coffee, and Milk Consumption and Colorectal Cancer Risk. J. Epidemiol. 2014, 24, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Yamada, H.; Kawado, M.; Aoyama, N.; Hashimoto, S.; Suzuki, K.; Wakai, K.; Suzuki, S.; Watanabe, Y.; Tamakoshi, A. Coffee Consumption and Risk of Colorectal Cancer: The Japan Collaborative Cohort Study. J. Epidemiol. 2014, 24, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Guercio, B.J.; Sato, K.; Niedzwiecki, D.; Ye, X.; Saltz, L.B.; Mayer, R.J.; Mowat, R.B.; Whittom, R.; Hantel, A.; Benson, A.; et al. Coffee Intake, Recurrence, and Mortality in Stage III Colon Cancer: Results From CALGB 89803 (Alliance). J. Clin. Oncol. 2015, 33, 3598–3607. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Ding, M.; Yuan, C.; Wu, K.; Smith-Warner, S.A.; Hu, F.B.; Chan, A.T.; Meyerhardt, J.A.; Ogino, S.; Fuchs, C.S.; et al. Association Between Coffee Intake After Diagnosis of Colorectal Cancer and Reduced Mortality. Gastroenterology 2018, 154, 916–926. [Google Scholar] [CrossRef] [PubMed]
- Gapstur, S.M.; Anderson, R.L.; Campbell, P.T.; Jacobs, E.J.; Hartman, T.J.; Hildebrand, J.S.; Wang, Y.; McCullough, M.L. Associations of Coffee Drinking and Cancer Mortality in the Cancer Prevention Study-II. Cancer Epidemiol. Biomark. Prev. 2017, 26, 1477–1486. [Google Scholar] [CrossRef] [PubMed]
- Galeone, C.; Turati, F.; La Vecchia, C.; Tavani, A. Coffee consumption and risk of colorectal cancer: A meta-analysis of case–control studies. Cancer Causes Control 2010, 21, 1949–1959. [Google Scholar] [CrossRef] [PubMed]
- Horisaki, K.; Takahashi, K.; Ito, H.; Matsui, S. A Dose-Response Meta-analysis of Coffee Consumption and Colorectal Cancer Risk in the Japanese Population: Application of a Cubic-Spline Model. J. Epidemiol. 2018, 28, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Kashino, I.; Akter, S.; Mizoue, T.; Sawada, N.; Kotemori, A.; Matsuo, K.; Oze, I.; Ito, H.; Naito, M.; Nakayama, T.; et al. Coffee drinking and colorectal cancer and its subsites: A pooled analysis of 8 cohort studies in Japan. Int. J. Cancer 2018, 143, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Tian, C.; Wang, W.; Hong, Z.; Zhang, X. Coffee consumption and risk of colorectal cancer: A dose–response analysis of observational studies. Cancer Causes Control 2013, 24, 1265–1268. [Google Scholar] [CrossRef] [PubMed]
- Je, Y.; Liu, W.; Giovannucci, E. Coffee consumption and risk of colorectal cancer: A systematic review and meta-analysis of prospective cohort studies. Int. J. Cancer 2009, 124, 1662–1668. [Google Scholar] [CrossRef] [PubMed]
- Gan, Y.; Wu, J.; Zhang, S.; Li, L.; Cao, S.; Mkandawire, N.; Ji, K.; Herath, C.; Gao, C.; Xu, H.; et al. Association of coffee consumption with risk of colorectal cancer: A meta-analysis of prospective cohort studies. Oncotarget 2017, 8, 18699–18711. [Google Scholar] [CrossRef] [PubMed]
- Norat, T.; Vingeliene, S.; Thompson, R.; Stevens, C. World Cancer Research Fund International Systematic Literature Review—The Associations between Food, Nutrition and Physical Activity and the Risk of Colorectal Cancer. Imp. Coll. London 2017. Available online: https://www.wcrf.org/sites/default/files/colorectal-cancer-slr.pdf (accessed on 11 December 2018).
- Stavric, B.; Klassen, R.; Watkinson, B.; Karpinski, K.; Stapley, R.; Fried, P. Variability in caffeine consumption from coffee and tea: Possible significance for epidemiological studies. Food Chem. Toxicol. 1988, 26, 111–118. [Google Scholar] [CrossRef]
- Lelo, A.; Miners, J.O.; Robson, R.; Birkett, D.J. Assessment of caffeine exposure: Caffeine content of beverages, caffeine intake, and plasma concentrations of methylxanthines. Clin. Pharmacol. Ther. 1986, 39, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, R.M.; Marshman, J.A.; Schwieder, M.; Berg, R. Caffeine content of beverages as consumed. Can. Med. Assoc. J. 1976, 114, 205–208. [Google Scholar] [PubMed]
- Mandel, H.G. Update on caffeine consumption, disposition and action. Food Chem. Toxicol. 2002, 40, 1231–1234. [Google Scholar] [CrossRef]
- Elmenhorst, D.; Meyer, P.T.; Matusch, A.; Winz, O.H.; Bauer, A. Caffeine Occupancy of Human Cerebral A1 Adenosine Receptors: In Vivo Quantification with 18F-CPFPX and PET. J. Nucl. Med. 2012, 53, 1723–1729. [Google Scholar] [CrossRef] [PubMed]
- Merighi, S.; Benini, A.; Mirandola, P.; Gessi, S.; Varani, K.; Simioni, C.; Leung, E.; Maclennan, S.; Baraldi, P.G.; Borea, P.A. Caffeine Inhibits Adenosine-Induced Accumulation of Hypoxia-Inducible Factor-1, Vascular Endothelial Growth Factor, and Interleukin-8 Expression in Hypoxic Human Colon Cancer Cells. Mol. Pharmacol. 2007, 72, 395–406. [Google Scholar] [CrossRef] [PubMed]
- Boswell-Smith, V.; Spina, D.; Page, C.P. Phosphodiesterase inhibitors. Br. J. Pharmacol. 2009, 147, S252–S257. [Google Scholar] [CrossRef] [PubMed]
- Umemura, T.; Ueda, K.; Nishioka, K.; Hidaka, T.; Takemoto, H.; Nakamura, S.; Jitsuiki, D.; Soga, J.; Goto, C.; Chayama, K.; et al. Effects of Acute Administration of Caffeine on Vascular Function. Am. J. Cardiol. 2006, 98, 1538–1541. [Google Scholar] [CrossRef] [PubMed]
- Holtzman, S.G.; Mante, S.; Minneman, K.P. Role of adenosine in caffeine tolerance. J. Pharmacol. Exp. Ther. 1991, 256, 62–68. [Google Scholar] [PubMed]
- Ribeiro, J.A.; Sebastio, A.M. Caffeine and adenosine. J. Alzheimer’s Dis. 2010, 20. [Google Scholar] [CrossRef] [PubMed]
- Ferré, S.; Fredholm, B.B.; Morelli, M.; Popoli, P.; Fuxe, K. Adenosine-dopamine receptor-receptor interactions as an integrative mechanism in the basal ganglia. Trends Neurosci. 1997, 20, 482–487. [Google Scholar] [CrossRef]
- Smits, P.; Boekema, P.; De Abreu, R.; Thien, T.; van ’t Laar, A. Evidence for an antagonism between caffeine and adenosine in the human cardiovascular system. J. Cardiovasc. Pharmacol. 1987, 10, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Higdon, J. V.; Frei, B. Coffee and Health: A Review of Recent Human Research. Crit. Rev. Food Sci. Nutr. 2006, 46, 101–123. [Google Scholar] [CrossRef] [PubMed]
- Babu, K.M.; Church, R.J.; Lewander, W. Energy Drinks: The New Eye-Opener For Adolescents. Clin. Pediatr. Emerg. Med. 2008, 9, 35–42. [Google Scholar] [CrossRef]
- Glade, M.J. Caffeine—Not just a stimulant. Nutrition 2010, 26, 932–938. [Google Scholar] [CrossRef] [PubMed]
- Satel, S. Is Caffeine Addictive?—A Review of the Literature. Am. J. Drug Alcohol Abuse 2006, 32, 493–502. [Google Scholar] [CrossRef] [PubMed]
- Namdar, M.; Schepis, T.; Koepfli, P.; Gaemperli, O.; Siegrist, P.T.; Grathwohl, R.; Valenta, I.; Delaloye, R.; Klainguti, M.; Wyss, C.A.; et al. Caffeine impairs myocardial blood flow response to physical exercise in patients with coronary artery disease as well as in age-matched controls. PLoS ONE 2009, 4, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Cameron, O.G.; Modell, J.G.; Hariharan, M. Caffeine and human cerebral blood flow: A positron emission tomography study. Life Sci. 1990, 47, 1141–1146. [Google Scholar] [CrossRef]
- Mitani, T.; Nagano, T.; Harada, K.; Yamashita, Y.; Ashida, H. Caffeine-Stimulated Intestinal Epithelial Cells Suppress Lipid Accumulation in Adipocytes. J. Nutr. Sci. Vitaminol. (Tokyo) 2017, 63, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Perera, V.; Gross, A.S.; McLachlan, A.J. Diurnal variation in CYP1A2 enzyme activity in South Asians and Europeans. J. Pharm. Pharmacol. 2013, 65, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Gunes, A.; Dahl, M.-L. Variation in CYP1A2 activity and its clinical implications: Influence of environmental factors and genetic polymorphisms. Pharmacogenomics 2008, 9, 625–637. [Google Scholar] [CrossRef] [PubMed]
- Hein, D.W.; Doll, M.A.; Fretland, A.J.; Leff, M.A.; Webb, S.J.; Xiao, G.H.; Devanaboyina, U.S.; Nangju, N.A.; Feng, Y. Molecular genetics and epidemiology of the NAT1 and NAT2 acetylation polymorphisms. Cancer Epidemiol. Biomark. Prev. 2000, 9, 29–42. [Google Scholar] [PubMed]
- Dobrinas, M.; Cornuz, J.; Oneda, B.; Kohler Serra, M.; Puhl, M.; Eap, C.B. Impact of smoking, smoking cessation, and genetic polymorphisms on CYP1A2 activity and inducibility. Clin. Pharmacol. Ther. 2011, 90, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Dobrinas, M.; Cornuz, J.; Pedrido, L.; Eap, C.B. Influence of cytochrome P450 oxidoreductase genetic polymorphisms on CYP1A2 activity and inducibility by smoking. Pharmacogenet. Genomics 2012, 22, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Wierzejska, R. Kofeina—Powszechny składnik diety i jej wpływ na zdrowie. Rocz. Państw. Zakładu. Hig. 2012, 63, 141–147. [Google Scholar]
- Grosso, L.M.; Bracken, M.B. Caffeine Metabolism, Genetics, and Perinatal Outcomes: A Review of Exposure Assessment Considerations during Pregnancy. Ann. Epidemiol. 2005, 15, 460–466. [Google Scholar] [CrossRef] [PubMed]
- Nawrot, P.; Jordan, S.; Eastwood, J.; Rotstein, J.; Hugenholtz, A.; Feeley, M. Effects of caffeine on human health. Food Addit. Contam. 2003, 20, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Klebanoff, M.A.; Levine, R.J.; Dersimonian, R.; Clemens, J.D.; Wilkins, D.G. Serum caffeine and paraxanthine as markers for reported caffeine intake in pregnancy. Ann. Epidemiol. 1998, 8, 107–111. [Google Scholar] [CrossRef]
- Nakajima, M.; Yokoi, T.; Mizutani, M.; Kinoshita, M.; Funayama, M.; Kamataki, T. Genetic polymorphism in the 5’-flanking region of human CYP1A2 gene: Effect on the CYP1A2 inducibility in humans. J. Biochem. 1999, 125, 803–808. [Google Scholar] [CrossRef] [PubMed]
- Han, X.M.; Ou-Yang, D.S.; Lu, P.X.; Jiang, C.H.; Shu, Y.; Chen, X.P.; Tan, Z.R.; Zhou, H.H. Plasma caffeine metabolite ratio (17X/137X) in vivo associated with G-2964A and C734A polymorphisms of human CYP1A2. Pharmacogenetics 2001, 11, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Saito, Y.; Gopalan, B.; Mhashilkar, A.M.; Roth, J.A.; Chada, S.; Zumstein, L.; Ramesh, R. Adenovirus-mediated PTEN treatment combined with caffeine produces a synergistic therapeutic effect in colorectal cancer cells. Cancer Gene Ther. 2003, 10, 803–813. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.K.; Ji, I.M.; Lee, S.R.; Kook, Y.H.; Griffin, R.J.; Lim, B.U.; Kim, J.-S.; Lee, D.S.; Song, C.W.; Park, H.J. Radiosensitization of tumor cells by modulation of ATM kinase. Int. J. Radiat. Biol. 2006, 82, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Mhaidat, N.M.; Alzoubi, K.H.; Al-Azzam, S.I.; Alsaad, A.A. Caffeine inhibits paclitaxel-induced apoptosis in colorectal cancer cells through the upregulation of Mcl-1 levels. Mol. Med. Rep. 2014, 9, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Itagaki, S.; Kurokawa, T.; Ogura, J.; Kobayashi, M.; Hirano, T.; Sugawara, M.; Iseki, K. In vitro and in vivo antioxidant properties of chlorogenic acid and caffeic acid. Int. J. Pharm. 2011, 403, 136–138. [Google Scholar] [CrossRef] [PubMed]
- Gonthier, M.; Verny, M.; Besson, C.; Rémésy, C.; Scalbert, A. Chlorogenic Acid Bioavailability Largely Depends on Its Metabolism by the Gut Microflora in Rats. J. Nutr. 2003, 133, 1853–1859. [Google Scholar] [CrossRef] [PubMed]
- Moridani, M.Y.; Scobie, H.; Jamshidzadeh, A.; Salehi, P.; O’Brien, P.J. Caffeic acid, chlorogenic acid, and dihydrocaffeic acid metabolism: Glutathione conjugate formation. Drug Metab. Dispos. 2001, 29, 1432–1439. [Google Scholar] [PubMed]
- Marinova, E.M.; Toneva, A.; Yanishlieva, N. Comparison of the antioxidative properties of caffeic and chlorogenic acids. Food Chem. 2009, 114, 1498–1502. [Google Scholar] [CrossRef]
- Jaganathan, S.K. Growth Inhibition by Caffeic Acid, One of the Phenolic Constituents of Honey, in HCT 15 Colon Cancer Cells. Sci. World J. 2012, 2012, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Chung, T.-W.; Moon, S.-K.; Chang, Y.-C.; Ko, J.-H.; Lee, Y.-C.; Cho, G.; Kim, S.-H.; Kim, J.-G.; Kim, C.-H. Novel and therapeutic effect of caffeic acid and caffeic acid phenyl ester on hepatocarcinoma cells: Complete regression of hepatoma growth and metastasis by dual mechanism. FASEB J. 2004, 18, 1670–1681. [Google Scholar] [CrossRef] [PubMed]
- Olthof, M.R.; Hollman, P.C.H.; Katan, M.B. Chlorogenic Acid and Caffeic Acid Are Absorbed in Humans. J. Nutr. 2001, 131, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Williamson, G.; Dionisi, F.; Renouf, M. Flavanols from green tea and phenolic acids from coffee: Critical quantitative evaluation of the pharmacokinetic data in humans after consumption of single doses of beverages. Mol. Nutr. Food Res. 2011, 55, 864–873. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, M.; Farah, A.; Perrone, D.; Trugo, L.C.; Donangelo, C. Chlorogenic Acid Compounds from Coffee Are Differentially Absorbed and Metabolized in Humans. J. Nutr. 2007, 137, 2196–2201. [Google Scholar] [CrossRef] [PubMed]
- Nardini, M.; Cirillo, E.; Natella, F.; Scaccini, C. Absorption of Phenolic Acids in Humans after Coffee Consumption. J. Agric. Food Chem. 2002, 50, 5735–5741. [Google Scholar] [CrossRef] [PubMed]
- Murphy, N.; Achaintre, D.; Zamora-Ros, R.; Jenab, M.; Boutron-Ruault, M.-C.; Carbonnel, F.; Savoye, I.; Kaaks, R.; Kühn, T.; Boeing, H.; et al. A prospective evaluation of plasma polyphenol levels and colon cancer risk. Int. J. Cancer 2018, 143, 1620–1631. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.S.; Satsu, H.; Bae, M.-J.; Zhao, Z.; Ogiwara, H.; Totsuka, M.; Shimizu, M. Anti-inflammatory effect of chlorogenic acid on the IL-8 production in Caco-2 cells and the dextran sulphate sodium-induced colitis symptoms in C57BL/6 mice. Food Chem. 2015, 168, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Murad, L.D.; Soares, N.D.C.P.; Brand, C.; Monteiro, M.C.; Teodoro, A.J. Effects of caffeic and 5-caffeoylquinic acids on cell viability and cellular uptake in human colon adenocarcinoma cells. Nutr. Cancer 2015, 67, 532–542. [Google Scholar] [CrossRef] [PubMed]
- Oleaga, C.; Ciudad, C.J.; Noé, V.; Izquierdo-Pulido, M. Coffee polyphenols change the expression of STAT5B and ATF-2 modifying cyclin D1 levels in cancer cells. Oxid. Med. Cell. Longev. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Lim, E.J.; Joung, Y.H.; Jung, S.M.; Park, S.H.; Park, J.H.; Kim, S.Y.; Hwang, T.S.; Hong, D.Y.; Chung, S.C.; Ye, S.-K.; et al. Yang Hemin inhibits cyclin D1 and IGF-1 expression via STAT5b under hypoxia in ERα-negative MDA-MB 231 breast cancer cells. Int. J. Oncol. 2010, 36, 1243–1251. [Google Scholar] [CrossRef]
- Lewis, J.S.; Thomas, T.J.; Pestell, R.G.; Albanese, C.; Gallo, M.A.; Thomas, T. Differential effects of 16alpha-hydroxyestrone and 2-methoxyestradiol on cyclin D1 involving the transcription factor ATF-2 in MCF-7 breast cancer cells. J. Mol. Endocrinol. 2005, 34, 91–105. [Google Scholar] [CrossRef] [PubMed]
- Du, W.; Wang, Y.-C.; Hong, J.; Su, W.-Y.; Lin, Y.-W.; Lu, R.; Xiong, H.; Fang, J.-Y. STAT5 isoforms regulate colorectal cancer cell apoptosis via reduction of mitochondrial membrane potential and generation of reactive oxygen species. J. Cell. Physiol. 2012, 227, 2421–2429. [Google Scholar] [CrossRef] [PubMed]
- Xiong, H.; Su, W.-Y.; Liang, Q.-C.; Zhang, Z.-G.; Chen, H.-M.; Du, W.; Chen, Y.-X.; Fang, J.-Y. Inhibition of STAT5 induces G1 cell cycle arrest and reduces tumor cell invasion in human colorectal cancer cells. Lab. Investig. 2009, 89, 717–725. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Kang, M.-S.; Oh, J.-S.; Na, H.S.; Lim, Y.J.; Jeong, Y.-I.; Lee, H.C. Caffeic acid-conjugated chitosan derivatives and their anti-tumor activity. Arch. Pharm. Res. 2013, 36, 1437–1446. [Google Scholar] [CrossRef] [PubMed]
- Jarmila, V.; Vavríková, E. Chitosan derivatives with antimicrobial, antitumour and antioxidant activities—A review. Curr. Pharm. Des. 2011, 17, 3596–3607. [Google Scholar] [PubMed]
- Zambonin, L.; Caliceti, C.; Vieceli Dalla Sega, F.; Fiorentini, D.; Hrelia, S.; Landi, L.; Prata, C. Dietary phenolic acids act as effective antioxidants in membrane models and in cultured cells, exhibiting proapoptotic effects in leukaemia cells. Oxid. Med. Cell. Longev. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Upadhyay, R.; Mohan Rao, L.J. An Outlook on Chlorogenic Acids-Occurrence, Chemistry, Technology, and Biological Activities. Crit. Rev. Food Sci. Nutr. 2013, 53, 968–984. [Google Scholar] [CrossRef] [PubMed]
- Bonamigo, T.; Campos, J.F.; Alfredo, T.M.; Balestieri, J.B.P.; Cardoso, C.A.L.; Paredes-Gamero, E.J.; De Picoli Souza, K.; Dos Santos, E.L. Antioxidant, Cytotoxic, and Toxic Activities of Propolis from Two Native Bees in Brazil: Scaptotrigona depilis and Melipona quadrifasciata anthidioides. Oxid. Med. Cell. Longev. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Oboh, G.; Agunloye, O.M.; Adefegha, S.A.; Akinyemi, A.J.; Ademiluyi, A.O. Caffeic and chlorogenic acids inhibit key enzymes linked to type 2 diabetes (in vitro): A comparative study. J. Basic Clin. Physiol. Pharmacol. 2015, 26, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Olthof, M.R.; Hollman, P.C.H.; Buijsman, M.N.C.P.; Van Amelsvoort, J.M.M.; Katan, M.B. Human Nutrition and Metabolism Chlorogenic Acid, Quercetin-3-Rutinoside and Black Tea Phenols Are Extensively Metabolized in Humans 1. J. Nutr. 2003, 133, 1806–1814. [Google Scholar] [CrossRef] [PubMed]
- Da Encarnação, J.A.; Farrell, T.L.; Ryder, A.; Kraut, N.U.; Williamson, G. In vitro enzymic hydrolysis of chlorogenic acids in coffee. Mol. Nutr. Food Res. 2015, 59, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Farah, A.; Monteiro, M.; Donangelo, C.M.; Lafay, S. Chlorogenic Acids from Green Coffee Extract are Highly Bioavailable in Humans. J. Nutr. 2008, 138, 2309–2315. [Google Scholar] [CrossRef] [PubMed]
- Stalmach, A.; Mullen, W.; Barron, D.; Uchida, K.; Yokota, T.; Cavin, C.; Steiling, H.; Williamson, G.; Crozier, A. Metabolite Profiling of Hydroxycinnamate Derivatives in Plasma and Urine after the Ingestion of Coffee by Humans: Identification of Biomarkers of Coffee Consumption. Drug Metab. Dispos. 2009, 37, 1749–1758. [Google Scholar] [CrossRef] [PubMed]
- Stalmach, A.; Williamson, G.; Crozier, A. Impact of dose on the bioavailability of coffee chlorogenic acids in humans. Food Funct. 2014, 5, 1727–1737. [Google Scholar] [CrossRef] [PubMed]
- Renouf, M.; Marmet, C.; Giuffrida, F.; Lepage, M.; Barron, D.; Beaumont, M.; Williamson, G.; Dionisi, F. Dose-response plasma appearance of coffee chlorogenic and phenolic acids in adults. Mol. Nutr. Food Res. 2014, 58, 301–309. [Google Scholar] [CrossRef] [PubMed]
- Matsui, Y.; Nakamura, S.; Kondou, N.; Takasu, Y.; Ochiai, R.; Masukawa, Y. Liquid chromatography-electrospray ionization-tandem mass spectrometry for simultaneous analysis of chlorogenic acids and their metabolites in human plasma. J. Chromatogr. B 2007, 858, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Glei, M.; Kirmse, A.; Habermann, N.; Persin, C.; Pool-Zobel, B.L. Bread Enriched With Green Coffee Extract Has Chemoprotective and Antigenotoxic Activities in Human Cells. Nutr. Cancer 2006, 56, 182–192. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.Z.; Liu, Z.Q. Chemical kinetic behavior of chlorogenic acid in protecting erythrocyte and DNA against radical-induced oxidation. J. Agric. Food Chem. 2008, 56, 11025–11029. [Google Scholar] [CrossRef] [PubMed]
- Cinkilic, N.; Cetintas, S.K.; Zorlu, T.; Vatan, O.; Yilmaz, D.; Cavas, T.; Tunc, S.; Ozkan, L.; Bilaloglu, R. Radioprotection by two phenolic compounds: Chlorogenic and quinic acid, on X-ray induced DNA damage in human blood lymphocytes in vitro. Food Chem. Toxicol. 2013, 53, 359–363. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.G.; Hu, Q.P.; Liu, Y. Antioxidant and DNA-protective activities of chlorogenic acid isomers. J. Agric. Food Chem. 2012, 60, 11625–11630. [Google Scholar] [CrossRef] [PubMed]
- Burgos-Morón, E.; Calderón-Montaño, J.M.; Orta, M.L.; Pastor, N.; Pérez-Guerrero, C.; Austin, C.; Mateos, S.; López-Lázaro, M. The coffee constituent chlorogenic acid induces cellular DNA damage and formation of topoisomerase I- and II-DNA complexes in cells. J. Agric. Food Chem. 2012, 60, 7384–7391. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Trush, M.A. Reactive oxygen-dependent DNA damage resulting from the oxidation of phenolic compounds by a copper-redox cycle mechanism. Cancer Res. 1994, 54, 1895s–1898s. [Google Scholar] [PubMed]
- Zheng, L.F.; Dai, F.; Zhou, B.; Yang, L.; Liu, Z.L. Prooxidant activity of hydroxycinnamic acids on DNA damage in the presence of Cu (II) ions: Mechanism and structure-activity relationship. Food Chem. Toxicol. 2008, 46, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Fan, G.J.; Jin, X.L.; Qian, Y.P.; Wang, Q.; Yang, R.T.; Dai, F.; Tang, J.J.; Shang, Y.J.; Cheng, L.X.; Yang, J.; et al. Hydroxycinnamic acids as DNA-cleaving agents in the presence of CuIIions: Mechanism, structure-activity relationship, and biological implications. Chem. A Eur. J. 2009, 15, 12889–12899. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, S.; Nandi, S. Choices have consequences: The nexus between DNA repair pathways and genomic instability in cancer. Clin. Transl. Med. 2016, 5. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, S.; Nandi, S. DNA damage response and cancer therapeutics through the lens of the Fanconi Anemia DNA repair pathway. Cell Commun. Signal. 2017, 15, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hiramoto, T.; Nakanishi, T.; Sumiyoshi, T.; Fukuda, T.; Matsuura, S.; Tauchi, H.; Komatsu, K.; Shibasaki, Y.; Inui, H.; Watatani, M.; et al. Mutations of a novel human RAD54 homologue, RAD54B, in primary cancer. Oncogene 1999, 18, 3422–3426. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, S.; Nandi, S. Synthetic lethality in DNA repair network: A novel avenue in targeted cancer therapy and combination therapeutics. IUBMB Life 2017, 69, 929–937. [Google Scholar] [CrossRef] [PubMed]
- Hou, N.; Liu, N.; Han, J.; Yan, Y.; Li, J. Chlorogenic acid induces reactive oxygen species generation and inhibits the viability of human colon cancer cells. Anticancer. Drugs 2017, 28, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Chen, Q.; He, M.; Mir, P.; Su, J.; Yang, Q. Inhibitory effect of antioxidant extracts from various potatoes on the proliferation of human colon and liver cancer cells. Nutr. Cancer 2011, 63, 1044–1052. [Google Scholar] [CrossRef] [PubMed]
- Xavier, C.P.R.; Lima, C.F.; Fernandes-Ferreira, M.; Pereira-Wilson, C. Hypericum androsaemum water extract inhibits proliferation in human colorectal cancer cells through effects on MAP kinases and PI3K/Akt pathway. Food Funct. 2012, 3, 844–852. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.-S.; Liu, C.-W.; Ma, Y.-S.; Weng, S.-W.; Tang, N.-Y.; Wu, S.-H.; Ji, B.-C.; Ma, C.-Y.; Ko, Y.-C.; Funayama, S.; et al. Chlorogenic Acid Induces Apoptotic Cell Death in U937 Leukemia Cells through Caspase- and Mitochondria-dependent Pathways. In Vivo (Brooklyn) 2012, 26, 971–978. [Google Scholar]
- Liu, Y.-J.; Zhou, C.-Y.; Qiu, C.-H.; Lu, X.-M.; Wang, Y.-T. Chlorogenic acid induced apoptosis and inhibition of proliferation in human acute promyelocytic leukemia HL-60 cells. Mol. Med. Rep. 2013, 8, 1106–1110. [Google Scholar] [CrossRef] [PubMed]
- Rakshit, S.; Mandal, L.; Pal, B.C.; Bagchi, J.; Biswas, N.; Chaudhuri, J.; Chowdhury, A.A.; Manna, A.; Chaudhuri, U.; Konar, A.; et al. Involvement of ROS in chlorogenic acid-induced apoptosis of Bcr-Abl+ CML cells. Biochem. Pharmacol. 2010, 80, 1662–1675. [Google Scholar] [CrossRef] [PubMed]
- Bandyopadhyay, G. Chlorogenic acid inhibits Bcr-Abl tyrosine kinase and triggers p38 mitogen-activated protein kinase-dependent apoptosis in chronic myelogenous leukemic cells. Blood 2004, 104, 2514–2522. [Google Scholar] [CrossRef] [PubMed]
- Urgert, R.; van der Weg, G.; Kosmeijer-Schuil, T.G.; van de Bovenkamp, P.; Hovenier, R.; Katan, M.B. Levels of the Cholesterol-Elevating Diterpenes Cafestol and Kahweol in Various Coffee Brews. J. Agric. Food Chem. 1995, 43, 2167–2172. [Google Scholar] [CrossRef]
- Gross, G.; Jaccaud, E.; Huggett, A.C. Analysis of the content of the diterpenes cafestol and kahweol in coffee brews. Food Chem. Toxicol. 1997, 35, 547–554. [Google Scholar] [CrossRef]
- Arab, L. Epidemiologic Evidence on Coffee and Cancer. Nutr. Cancer 2010, 62, 271–283. [Google Scholar] [CrossRef] [PubMed]
- Ranheim, T.; Halvorsen, B. Coffee consumption and human health—Beneficial or detrimental? - Mechanisms for effects of coffee consumption on different risk factors for cardiovascular disease and type 2 diabetes mellitus. Mol. Nutr. Food Res. 2005, 49, 274–284. [Google Scholar] [CrossRef] [PubMed]
- De Roos, B.; Sawyer, J.K.; Katan, M.B.; Rudel, L.L. Validity of animal models for the cholesterol-raising effects of coffee diterpenes in human subjects. Proc. Nutr. Soc. 1999, 58, 551–557. [Google Scholar] [CrossRef] [PubMed]
- Huber, W.W.; McDaniel, L.P.; Kaderlik, K.R.; Teitel, C.H.; Lang, N.P.; Kadlubar, F.F. Chemoprotection against the formation of colon DNA adducts from the food-borne carcinogen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) in the rat. Mutat. Res. 1997, 376, 115–122. [Google Scholar] [CrossRef]
- Choi, D.W.; Lim, M.S.; Lee, J.W.; Chun, W.; Lee, S.H.; Nam, Y.H.; Park, J.M.; Choi, D.H.; Kang, C.D.; Lee, S.J.; et al. The Cytotoxicity of Kahweol in HT-29 Human Colorectal Cancer Cells Is Mediated by Apoptosis and Suppression of Heat Shock Protein 70 Expression. Biomol. Ther. (Seoul) 2015, 23, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Grivicich, I.; Regner, A.; Zanoni, C.; Correa, L.P.; Jotz, G.P.; Henriques, J.A.P.; Schwartsmann, G.; da Rocha, A.B. Hsp70 response to 5-fluorouracil treatment in human colon cancer cell lines. Int. J. Colorectal Dis. 2007, 22, 1201–1208. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Li, Y.; Liu, D.; Sun, H.; Su, D.; Yang, F.; Liu, J. Extracellular HSP70/HSP70-PCs Promote Epithelial-Mesenchymal Transition of Hepatocarcinoma Cells. PLoS ONE 2013, 8. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.A.; Kim, Y.; Kwon, B.; Han, D.C. The Natural Compound Cantharidin Induces Cancer Cell Death through Inhibition of Heat Shock Protein 70 (HSP70) and Bcl-2-associated Athanogene Domain 3 (BAG3) Expression by Blocking Heat Shock Factor 1 (HSF1) Binding to Promoters. J. Biol. Chem. 2013, 288, 28713–28726. [Google Scholar] [CrossRef] [PubMed]
- Park, G.H.; Song, H.M.; Jeong, J.B. The coffee diterpene kahweol suppresses the cell proliferation by inducing cyclin D1 proteasomal degradation via ERK1/2, JNK and GKS3 b -dependent threonine-286 phosphorylation in human colorectal cancer cells. Food Chem. Toxicol. 2016, 95, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Holland, T.A.; Elder, J.; McCloud, J.M.; Hall, C.; Deakin, M.; Fryer, A.A.; Elder, J.B.; Hoban, P.R. Subcellular localisation of cyclin D1 protein in colorectal tumours is associated with p21(WAF1/CIP1) expression and correlates with patient survival. Int. J. Cancer 2001, 95, 302–306. [Google Scholar] [CrossRef]
- Bahnassy, A.A.; Zekri, A.N.; El-Houssini, S.; El-Shehaby, A.M.; Mahmoud, M.R.; Abdallah, S.; El-Serafi, M. Cyclin A and cyclin D1 as significant prognostic markers in colorectal cancer patients. BMC Gastroenterol. 2004, 4, 22. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Yin, L.-L.; Su, K.-L.; Zhang, G.-F.; Wang, J. Concomitant depletion of PTEN and p27 and overexpression of cyclin D1 may predict a worse prognosis for patients with post-operative stage II and III colorectal cancer. Oncol. Lett. 2014, 8, 1543–1550. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wei, J.; Xu, C.; Zhao, Z.; You, T. Prognostic Significance of Cyclin D1 Expression in Colorectal Cancer: A Meta-Analysis of Observational Studies. PLoS ONE 2014, 9. [Google Scholar] [CrossRef] [PubMed]
- Park, G.H.; Song, H.M.; Jeong, J.B. Kahweol from Coffee Induces Apoptosis by Upregulating Activating Transcription Factor 3 in Human Colorectal Cancer Cells. Biomol. Ther. (Seoul) 2017, 25, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.H.; Wang, D.L. Nitric oxide inhibits matrix metalloproteinase-2 expression via the induction of activating transcription factor 3 in endothelial cells. Mol. Pharmacol. 2004, 65, 1130–1140. [Google Scholar] [CrossRef] [PubMed]
- Lu, D.; Wolfgang, C.D.; Hai, T. Activating Transcription Factor 3, a Stress-inducible Gene, Suppresses Ras-stimulated Tumorigenesis. J. Biol. Chem. 2006, 281, 10473–10481. [Google Scholar] [CrossRef] [PubMed]
- Yan, C.; Lu, D.; Hai, T.; Boyd, D.D. Activating transcription factor 3, a stress sensor, activates p53 by blocking its ubiquitination. EMBO J. 2005, 24, 2425–2435. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).