Abstract
Traditionally, atherosclerotic risk factors for cardiovascular disease and cancer are assessed using coronary artery calcium scoring. However, this neglects the impact of atherosclerotic disease more proximal to the cancer site. This study assesses whether aortoiliac atherosclerotic plaque is associated with prostate cancer. The dataset consisted of abdominopelvic CT of 93 patients with prostate cancer and 186 asymptomatic patients who underwent CT colonography as an age- and gender-matched control group. Agatston scores were measured in the abdominal aorta, common iliac, and internal iliac arteries. The scores were evaluated for associations with age, Framingham risk score, and prostate cancer-related biomarkers, including prostate-specific antigen, Gleason score, tumor location, prostatectomy, androgen deprivation therapy, mortality, and bone metastasis. The atherosclerotic plaque of prostate cancer patients did not differ from the control group (p = 0.22) and was not correlated with any of the prostate cancer-related biomarkers (p > 0.05). However, Agatston scores of abdominal plaques correlated well with age (p < 0.001) and Framingham risk scores (p = 0.002).
1. Introduction
Cancer survivors have a higher incidence of cardiovascular disease (CVD) compared to the general population [], and increased coronary artery calcification has been observed in cancer-diagnosed and cancer-treated patients []. Prostate cancer patients also have a high incidence of CVD [], and local atherosclerosis has been found in prostatectomy specimens of prostate cancer patients [].
Abdominal aortic calcification is known to be correlated with traditional CVD risk factors, including age, gender, smoking, hypertension, and Framingham risk score [,,]. However, the plaque burden in the abdominal aortic and iliac arteries of prostate cancer patients has yet to be reported. A technical challenge is that calcification scores are usually measured on non-contrast chest CT scans using the Agatson score (reflecting the total area of calcium deposits and density) [], but in daily practice, most abdominal CT scans are performed with intravenous contrast enhancement.
This case-control study involved comparing the plaque burden of a prostate cancer patient group with an age- and gender-matched control group of asymptomatic outpatients undergoing a screening CT colonography (CTC). The primary objective was to see if the abdominal Agatston scores had an association with a prostate cancer diagnosis, prostate cancer-related biomarkers, and the Framingham risk score (a score that estimates the 10-year risk of manifesting clinical CVD) []. A flow diagram of the study design can be found in Figure 1.
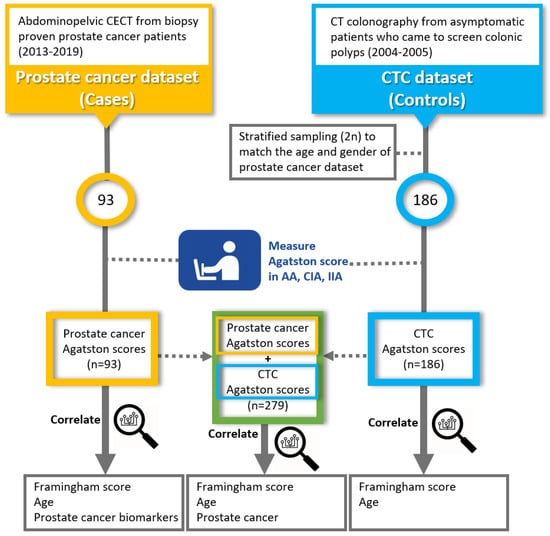
Figure 1.
Flow diagram of study outline. Abbreviations: CECT, contrast-enhanced CT; CTC, CT colonography; AA, abdominal aorta; CIA, common iliac artery; IIA, internal iliac artery.
2. Materials and Methods
This investigation was Health Insurance Portability and Accountability Act compliant and approved by the Institutional Review Boards at (BLINDED), and by the Office of Human Subjects Research Protection at (BLINDED). All research was performed in accordance with relevant guidelines/regulations and the Declaration of Helsinki. The requirement for signed informed consent was waived.
2.1. Datasets
Abdominopelvic contrast-enhanced CT (CECT) exams were retrospectively recruited from biopsy-proven metastatic adenocarcinoma prostate cancer patients (Gleason score 6 and higher) who participated in clinical trials involving neoadjuvant treatments at a single institution (BLINDED) from 2013 to 2019. The scans were taken at the beginning of the trial and performed with portal venous phase (PVP) contrast enhancement. Patients with missing clinical data or CT images were excluded. A total of 93 CECT scans were obtained. This dataset will be referred to as the Cases dataset.
The control group consisted of asymptomatic outpatients who had CT colonography (CTC) screening for detecting colonic polyps at a different institution from April 2004 to March 2005 []. To compare with the prostate cancer dataset, we selected 186 patients (2 times the size of the prostate cancer dataset) out of 829 patients by stratified random sampling. The age and sex were matched with the prostate cancer dataset. At the time of the scan, none of the 186 CTC outpatients had been diagnosed or treated for prostate cancer. During long-term (median 8.2 years) follow-up, 2 of the 186 outpatients developed prostate cancer, 2 and 5 years after the scan. This dataset will be referred to as the Controls dataset.
All CT scans were cropped to have the same field of view (FOV) from the diaphragm to the pelvic brim and resampled to 3 mm section thickness.
2.2. Agatston Score Measurement
Agatston scores were determined as described in the Supplementary Materials. All plaques were segmented using the segment editor module of 3D Slicer (version 4.10 RRID: SCR_005619) and measured with plug-in Python codes modified from the ‘Cardiac Agatston Scoring function’ codes []. Plaque scores were measured separately in: 1. the abdominal aorta (AA: 1cm above the celiac axis to the bifurcation point of the common iliac arteries), 2. the common iliac arteries (CIA: bifurcation point of common iliac arteries to the bifurcation of the external and internal iliac arteries), and 3. the internal iliac arteries (IIA: bifurcation of the external and internal iliac arteries to the visible end arteries of the internal iliac arteries inside the pelvic cavity). All measurements were done by a single radiologist with 12 years of experience. An example of plaque measurement can be found in Figure 2.
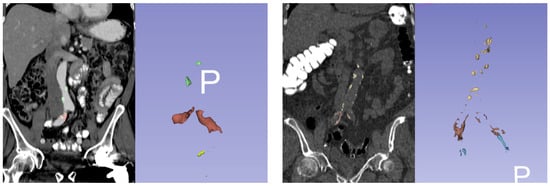
Figure 2.
Example of Agatston score measurement. (left) A 72-year-old male with prostate cancer. Agatston scores for abdominal aorta (AA), common iliac arteries (CIA), and internal iliac arteries (IIA) were 752, 3932, and 506. (right) A 74-year-old asymptomatic male from the control group. Agatston score for AA, CIA, and IIA were 2814, 3265, and 1555. Plaques in AA, CIA, and IIA are colored differently. 3D images are facing anterior to posterior (P).
2.3. Clinical Biomarkers
Framingham Risk Scores [] were calculated from CVD risk factors, including age, gender, systolic blood pressure (at the time or closest to the time of CT scan), hypertension (diagnosed or currently being treated), smoking habits (divided into current or past/non-smoker), prior CVD events, diabetes (diagnosed or currently being treated), total cholesterol, and HDL cholesterol (at the time or closet to the time of CT scan) in the Cases and Controls datasets. Prostate cancer-related biomarkers including prostate-specific antigen (PSA) at the time of diagnosis, pathology (Gleason score, anatomical location of the tumor within the prostate gland), prostatectomy at the time of CT scan, androgen deprivation therapy (ADT) usage at the time of the scan, and patient outcomes were obtained in the Cases dataset. The outcomes were mortality and bone metastasis reviewed for a mean period of 23 ± 16 months.
2.4. Statistical Analysis
The Agatston scores of Cases and Controls were compared with the Wilcoxon signed-rank test. The AA, CIA, and IIA scores were compared separately. To determine if plaque appearance in a certain vessel correlated with plaques in other vessels, we also calculated the Spearman’s rank correlation coefficient between the Agatston scores of the AA, CIA, and IIA. Since the vessels had a different range of scores depending on the vessel size, the scores were first stratified as percentiles (zero, 25th, 50th, and 75th) before the Spearman correlation.
To correlate clinical biomarkers with the Agatston scores, Cases and Controls were first compared separately with age and Framingham risk scores using Spearman’s rank correlation. Then, age, Framingham risk scores, and prostate cancer diagnosis were assessed by univariate and multivariate analyses for predicting the plaque scores in the combined prostate cancer and CTC datasets. The log transformation of Agatston scores was used to make the Agatston score variable more suitable for fitting linear models. Only the factors that had a p-value lower than 0.05 were put into the multivariate analysis. Residual plots and variance inflation factor (VIF) scores were used to examine the appropriateness and multicollinearity of the regression models. The prostate cancer-related biomarkers were compared with Agatston scores using univariate/multivariate analysis, Spearman’s rank correlation, Mann–Whitney U test, and Kruskal–Wallis test, according to data types. All statistics were computed using R (version 3.6.3 RRID: SCR_001905).
3. Results
3.1. Patient Characteristics
The patient characteristics and CT parameters of each dataset are shown in Table 1 and Table 2. There was no significant difference in patient age between the Case and Control datasets (Figure S1).

Table 1.
Patient characteristics of the datasets.

Table 2.
Parameters and methods of CT scans.
3.2. Agatston Scores of the Cases and Controls Patients
Zero and non-zero Agatston scores were counted separately. In the Cases, the percentages of zero Agatston scores were 25.8% in the abdominal aorta (AA), 37.6% in the common iliac arteries (CIA), and 33.3% in the internal iliac arteries (IIA). In the Controls, the percent of zero Agatston scores were 16.3% in the AA, 26.3% in the CIA, and 31.9% in the IIA. The non-zero Agatston scores are shown in Figure 3.
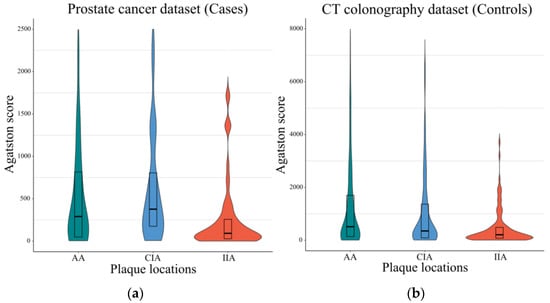
Figure 3.
Agatston scores of Cases and Controls patients in different arterial territories. (a) Agatston scores of Cases patients in different vessels. The median scores were 340 (IQR, 60-930) for the abdominal aorta (AA), 407 (IQR, 178-1064) for the common iliac arteries (CIA), and 92 (IQR, 28-257) for the internal iliac arteries (IIA). Cases scores are before calibration. Only non-zero plaques are included. The violin plots display the full distribution of the data, and the box plots represent the median, upper, and lower quartiles. (b) Agatston scores of Controls patients in different vessels. The median scores were 555 (IQR, 152-2212) for the AA, 349 (IQR, 89-1364) for the CIA, and 208 (IQR, 76-486) for the IIA. Abbreviations: IQR, interquartile range.
In the Cases dataset, there were high correlations between the Agatston scores of the AA, CIA, and IIA (Spearman’s Rho ≥ 0.5). The Controls dataset also showed similar high correlations between the Agatston scores of the AA, CIA, and IIA (Spearman’s Rho ≥ 0.7). Correlation heatmaps can be found in Figure 4.
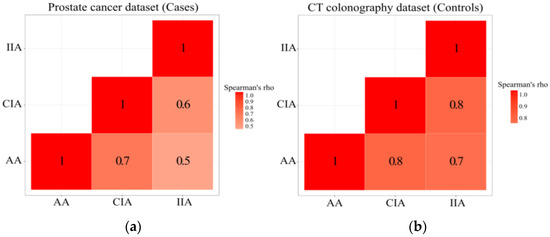
Figure 4.
Correlation of Agatston scores between different vessels. (a) Correlation of Agatston scores between the abdominal aorta (AA), common iliac arteries (CIA), and internal iliac arteries (IIA) in Cases dataset. (b) Correlation of Agatston scores between the AA, CIA, and IIA in the Controls dataset. The scores were first stratified into quartiles before Spearman’s correlation.
When comparing the calibrated Cases and Controls scores, there was no statistically significant difference between the two groups in the AA, CIA, IIA, and the sum of all plaques (Wilcoxon p = 0.062, 0.59, 0.47, and 0.22, respectively).
3.3. Association of Plaque and Cardiovascular Disease (CVD) Risk Factors
Age and Framingham scores were correlated with the Agatston scores of both Cases (p <0.001, Spearman’s Rho (ρ) 0.37 for age, p <0.001, ρ = 0.41 for Framingham risk score) and Controls (p <0.001, Spearman’s ρ = 0.67 for age, p <0.001, ρ = 0.49 for Framingham risk score). This was true for the AA, CIA, IIA, and the sum of all plaques (Table 3). When age, Framingham scores, and prostate cancer diagnosis were applied to the 2 groups in combination, only age and Framingham score had a significant association in the univariate analysis (p < 0.001 for age, <0.001 for Framingham score) and multivariate analysis (p < 0.001 for age, 0.002 for Framingham score). Prostate cancer diagnosis had no association in the univariate analysis (p = 0.95) (Table 4). The VIF for age and Framingham scores were 1.33 and 1.33, respectively, and the residual plot for the multivariate analysis model had a symmetrical distribution (Figure S2).

Table 3.
Correlation of abdominal aortic and iliac Agatston scores with CVD risk factors for Cases and Controls.

Table 4.
Correlation of abdominal aortic and iliac Agatston scores with CVD risk factors: combined dataset of Cases and Controls.
3.4. Association of Plaque and Prostate Cancer-Related Biomarkers
There was no significant association of the PSA, Gleason score, mortality, bone metastasis, prostatectomy, ADT use, and tumor location with the Cases’ Agatston scores (Table 5).

Table 5.
Association of prostate cancer-related biomarkers and abdominal aortic and iliac Agatston scores in Cases dataset.
4. Discussion
In this study, we found that the Agatston scores of the abdominal aortic and iliac plaques were not significantly different in the prostate cancer and control groups and also were not associated with prostate cancer-related biomarkers within prostate cancer patients. However, the abdominal aortic and iliac plaques had a good association with age and Framingham risk score, and this pattern was similar in both groups. We also examined the regional distribution of plaques and found that the abdominal aortic, common iliac, and internal iliac plaques were highly correlated with each other. This finding suggests that abdominal aortic plaque measurement alone may be sufficient in future investigations, increasing the efficiency of conducting such studies.
Prostate cancer and CVD have many shared etiologies, which adds complexity to explaining study results. Most published works that study CVD in prostate cancer patients focus on the coronary arteries, a more systemic marker. Abdominal arteries are more proximal to the site of prostate cancer and might theoretically have a closer association with the presence of cancer. In addition, many studies reporting a correlation between CVD and prostate cancer are not free from screening biases (higher screening rate of patients with underlying CVD) or confounding factors such as age, obesity, and cholesterolemia []. In a longitudinal coronary calcium score study, men with higher coronary calcium scores had an increased chance of developing cancer (55% prostate cancer) []. However, after adjusting for age, there was no significant difference between the cancer group and cancer-free group. Although other possible confounding factors exist (e.g., obesity and cholesterol), the prostate cancer group and control group in our study were age-matched and also showed no difference in the abdominal aortic and iliac calcifications. It is possible that the presence of stenoses, particularly in the smaller internal iliac arteries, may be associated with prostate cancer. This hypothesis could form the basis of future research.
ADT treatment of over 6 months is also reported to contribute to the increase of CVD []. The ADT treatment effect may have been weak in our prostate cancer group as the majority of patients had been treated for less than 3 months at the time of the CT scan.
The positive correlation between abdominal plaque and age or Framingham risk scores is not surprising [,,]. However, our study suggests CECT can also be used to measure abdominal plaque and can even be compared with non-contrast CT (NCT) measurements.
This study has several limitations. The Cases dataset was relatively small; therefore, small differences with the Controls could be missed. However, small differences are not likely to be clinically significant. Our findings warrant confirmation in a larger dataset. As mentioned above, there are other possible confounding factors besides age and gender between the Cases and Controls. Although the age was matched and the Framingham risk scores were not significantly different, known confounding risk factors such as obesity and cholesterol were not separately corrected, and this may have affected the plaque scores. Agatston score measurements can also be influenced by several other factors, including scanner type, tube current, voltage, kernel, and slice thickness [,,,,]. In this study, the tube voltages were all 120 kVp, and the slice thickness was identical for all datasets, but other factors were not matched, and these factors may have an effect on the Agatston scores. Although the CT colonography group was used as the non-cancer control group for this study, undiagnosed prostate cancer may be a possibility, as prostate cancer is suggested to be a slowly developing disease with a long preclinical phase []. In long-term follow-up, however, only 2 of the control patients were diagnosed with prostate cancer.
5. Conclusions
In conclusion, the atherosclerotic plaques of prostate cancer patients in arteries more proximal to the prostate were more correlated with CVD risk factors than with the diagnosis of prostate cancer or prostate cancer-related biomarkers. The presence of abdominal aortic and iliac plaques were highly correlated with each other, suggesting that future studies could avoid the need to measure both arteries. Abdominal arterial plaque scores on CT may serve as indicators for further investigations of CVD when coronary artery calcium scores are unavailable.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/tomography8020050/s1, Figure S1: Age distribution between prostate cancer patients and the CT colonography outpatients, Figure S2: Residual plot for multivariate analysis in Table 4, Figure S3: Intra-arterial lumen attenuation in portal venous phase CECT of all prostate cancer patients, Figure S4: Flow diagram of calculating conversion factors from multiphase CT scans, Figure S5: Data augmentation of Agatston score measurements using ‘Split islands to segments’ in 3D Slicer, Figure S6: The conversion factor of Agatston scores between non-contrast and portal venous phase CECT in multiphase CT.
Author Contributions
Conceptualization, S.L. and R.M.S.; methodology, S.L. and R.M.S.; software, D.C.E.; validation, S.L. and R.M.S. and P.J.P.; formal analysis, S.L.; investigation, S.L.; resources, J.L.G. and P.J.P. and W.L.D. and R.A.M. and P.A.P. and D.E.C.; data curation, S.L.; writing—original draft preparation, S.L.; writing—review and editing, S.L. and R.M.S.; visualization, S.L.; supervision, R.M.S.; project administration, S.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded in part by the Intramural Research Program of the National Institutes of Health, Clinical Center (1Z01 CL040004).
Institutional Review Board Statement
This investigation was Health Insurance Portability and Accountability Act compliant and approved by the Institutional Review Boards at the National Institutes of Health and University of Wisconsin, and by the Office of Human Subjects Research Protection at the NIH (Bethesda, MD, USA).
Informed Consent Statement
All research was performed in accordance with relevant guidelines/regulations and the Declaration of Helsinki. The requirement for signed informed consent was waived.
Conflicts of Interest
Author P.J.P receives royalties from Elsevier. He holds stock/stock options in Elucent, Cellectar, and SHINE. He is a consultant for Bracco. His institution has grants/grants pending with the National Institutes of Health. Author R.M.S. receives royalties from iCAD, ScanMed, Philips, Translation Holdings, and Ping An. His lab received research support from Ping An.
References
- Sturgeon, K.M.; Deng, L.; Bluethmann, S.M.; Zhou, S.; Trifiletti, D.M.; Jiang, C.; Kelly, S.P.; Zaorsky, N.G. A population-based study of cardiovascular disease mortality risk in US cancer patients. Eur. Heart J. 2019, 40, 3889–3897. [Google Scholar] [CrossRef] [PubMed]
- Whitlock, M.C.; Yeboah, J.; Burke, G.L.; Chen, H.; Klepin, H.D.; Hundley, W.G. Cancer and Its Association With the Development of Coronary Artery Calcification: An Assessment From the Multi-Ethnic Study of Atherosclerosis. J. Am. Heart Assoc. 2015, 4, e002533. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.A., 2nd; Gerber, L.; Banez, L.L.; Moreira, D.M.; Rittmaster, R.S.; Andriole, G.L.; Freedland, S.J. Prostate cancer risk in men with baseline history of coronary artery disease: Results from the REDUCE Study. Cancer Epidemiol. Biomark. Prev. 2012, 21, 576–581. [Google Scholar] [CrossRef] [PubMed]
- Hager, M.; Mikuz, G.; Bartsch, G.; Kolbitsch, C.; Moser, P.L. The association between local atherosclerosis and prostate cancer. BJU Int. 2007, 99, 46–48. [Google Scholar] [CrossRef] [PubMed]
- Davila, J.A.; Johnson, C.D.; Behrenbeck, T.R.; Hoskin, T.L.; Harmsen, W.S. Assessment of cardiovascular risk status at CT colonography. Radiology 2006, 240, 110–115. [Google Scholar] [CrossRef]
- O’Connor, S.D.; Graffy, P.M.; Zea, R.; Pickhardt, P.J. Does Nonenhanced CT-based Quantification of Abdominal Aortic Calcification Outperform the Framingham Risk Score in Predicting Cardiovascular Events in Asymptomatic Adults? Radiology 2019, 290, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Chuang, M.L.; Massaro, J.M.; Levitzky, Y.S.; Fox, C.S.; Manders, E.S.; Hoffmann, U.; O’Donnell, C.J. Prevalence and distribution of abdominal aortic calcium by gender and age group in a community-based cohort (from the Framingham Heart Study). Am. J. Cardiol. 2012, 110, 891–896. [Google Scholar] [CrossRef]
- Agatston, A.S.; Janowitz, W.R.; Hildner, F.J.; Zusmer, N.R.; Viamonte, M., Jr.; Detrano, R. Quantification of coronary artery calcium using ultrafast computed tomography. J. Am. Coll. Cardiol. 1990, 15, 827–832. [Google Scholar] [CrossRef]
- D’Agostino, R.B.S.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef] [PubMed]
- lassoan. Cardiac Agatston Scoring Function for 3D Slicer. Available online: https://gist.github.com/lassoan/d85be45b7284a3b4e580688fccdb1d02/revisions (accessed on 30 December 2021).
- O’Farrell, S.; Garmo, H.; Holmberg, L.; Adolfsson, J.; Stattin, P.; Van Hemelrijck, M. Risk and timing of cardiovascular disease after androgen-deprivation therapy in men with prostate cancer. J. Clin. Oncol. 2015, 33, 1243–1251. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, B.; Kantert, C.; Meyer, T.; Hadamitzky, M.; Martinoff, S.; Schömig, A.; Hausleiter, J. Cardiovascular risk assessment based on the quantification of coronary calcium in contrast-enhanced coronary computed tomography angiography. Eur. Heart J. Cardiovasc. Imaging 2012, 13, 468–475. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Groen, J.M.; Greuter, M.J.; Schmidt, B.; Suess, C.; Vliegenthart, R.; Oudkerk, M. The influence of heart rate, slice thickness, and calcification density on calcium scores using 64-slice multidetector computed tomography: A systematic phantom study. Investig. Radiol. 2007, 42, 848–855. [Google Scholar] [CrossRef] [PubMed]
- Komen, N.; Klitsie, P.; Hermans, J.J.; Niessen, W.J.; Kleinrensink, G.J.; Jeekel, J.; Lange, J.F. Calcium scoring in unenhanced and enhanced CT data of the aorta-iliacal arteries: Impact of image acquisition, reconstruction, and analysis parameter settings. Acta Radiol. 2011, 52, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Mühlenbruch, G.; Thomas, C.; Wildberger, J.E.; Koos, R.; Das, M.; Hohl, C.; Katoh, M.; Günther, R.W.; Mahnken, A.H. Effect of varying slice thickness on coronary calcium scoring with multislice computed tomography in vitro and in vivo. Investig. Radiol. 2005, 40, 695–699. [Google Scholar] [CrossRef]
- McCollough, C.H.; Ulzheimer, S.; Halliburton, S.S.; Shanneik, K.; White, R.D.; Kalender, W.A. Coronary artery calcium: A multi-institutional, multimanufacturer international standard for quantification at cardiac CT. Radiology 2007, 243, 527–538. [Google Scholar] [CrossRef]
- Bell, K.J.; Del Mar, C.; Wright, G.; Dickinson, J.; Glasziou, P. Prevalence of incidental prostate cancer: A systematic review of autopsy studies. Int. J. Cancer 2015, 137, 1749–1757. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).