Ipsilateral Recurrence of DCIS in Relation to Radiomics Features on Contrast Enhanced Breast MRI
Abstract
:1. Introduction
2. Materials and Methods
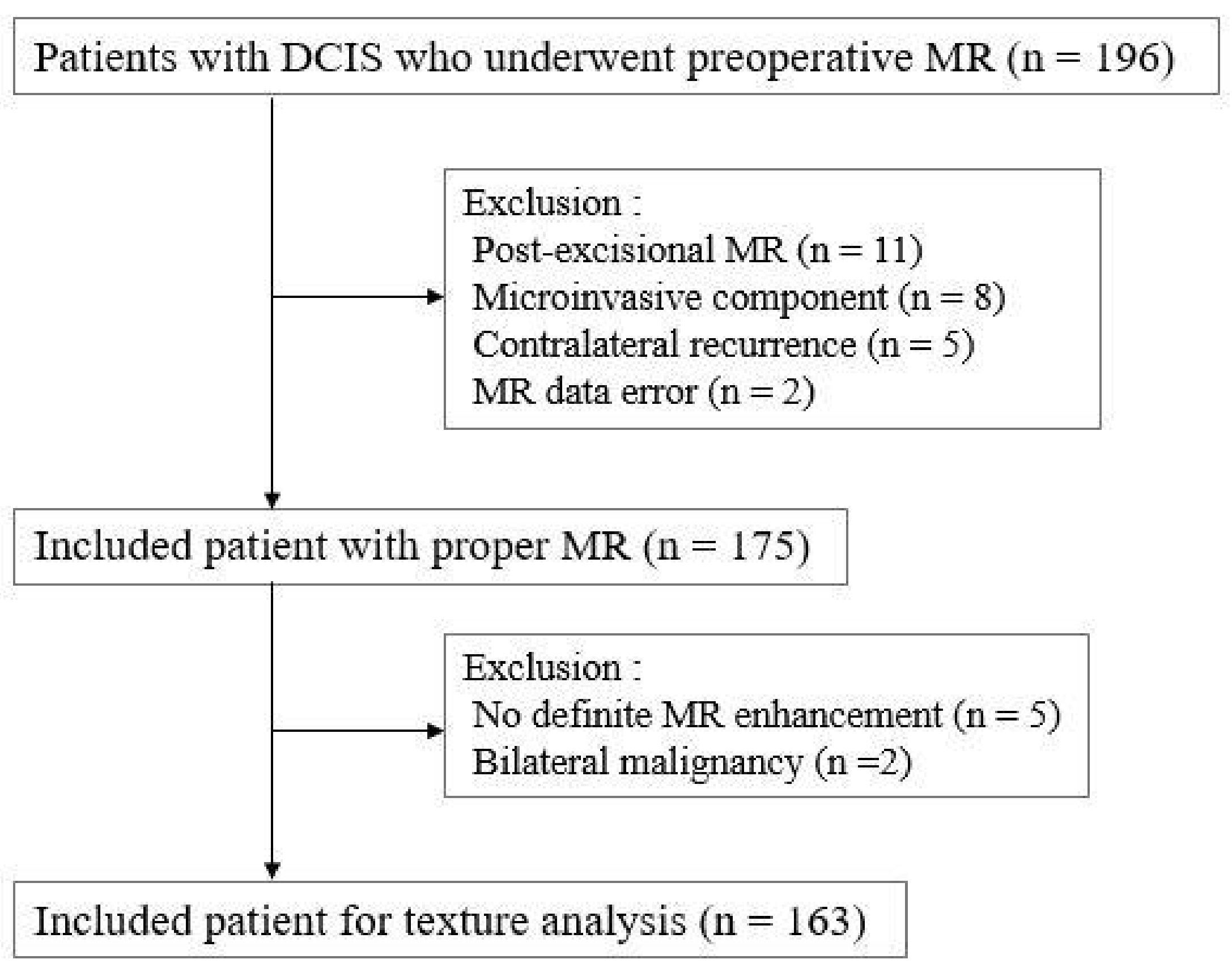
2.1. Study Population
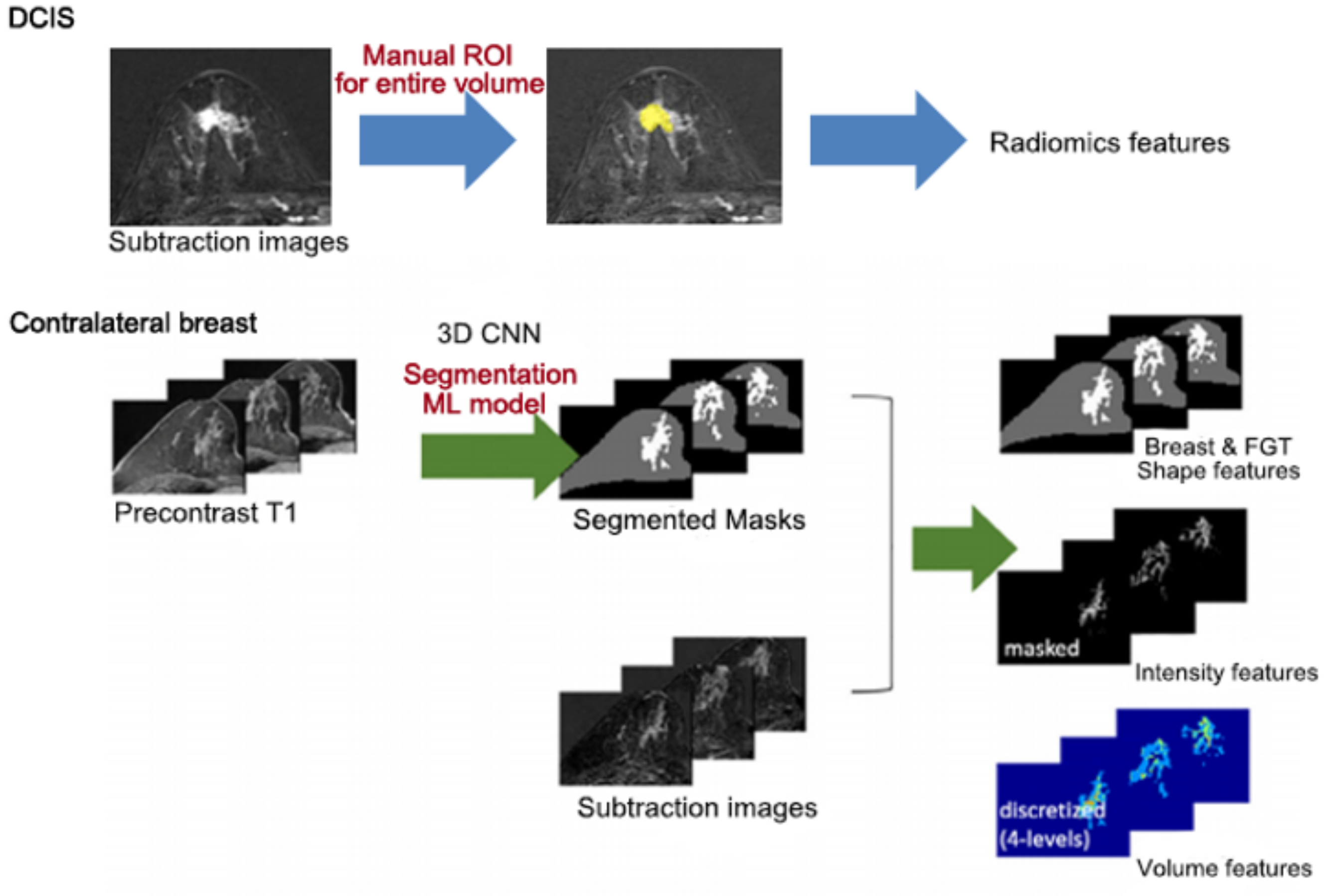
2.2. Radiomics Feature Extraction
2.3. Clinico-Pathological Analysis
2.4. MR Imaging Acquisition
2.5. Statistical Analysis
3. Results
3.1. Baseline Patients Characteristics
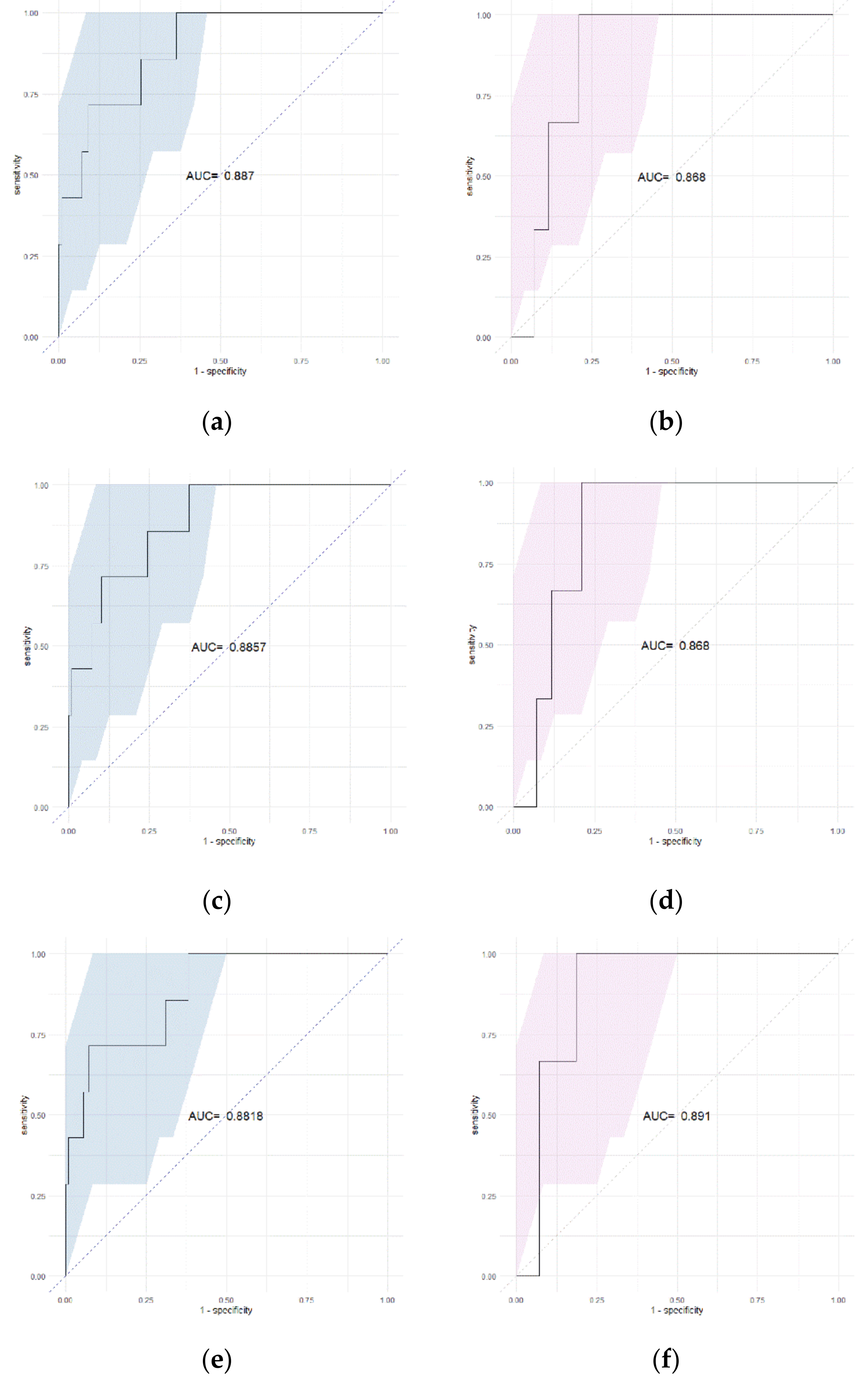
3.2. Feature Selection and Rad-Score Calculation
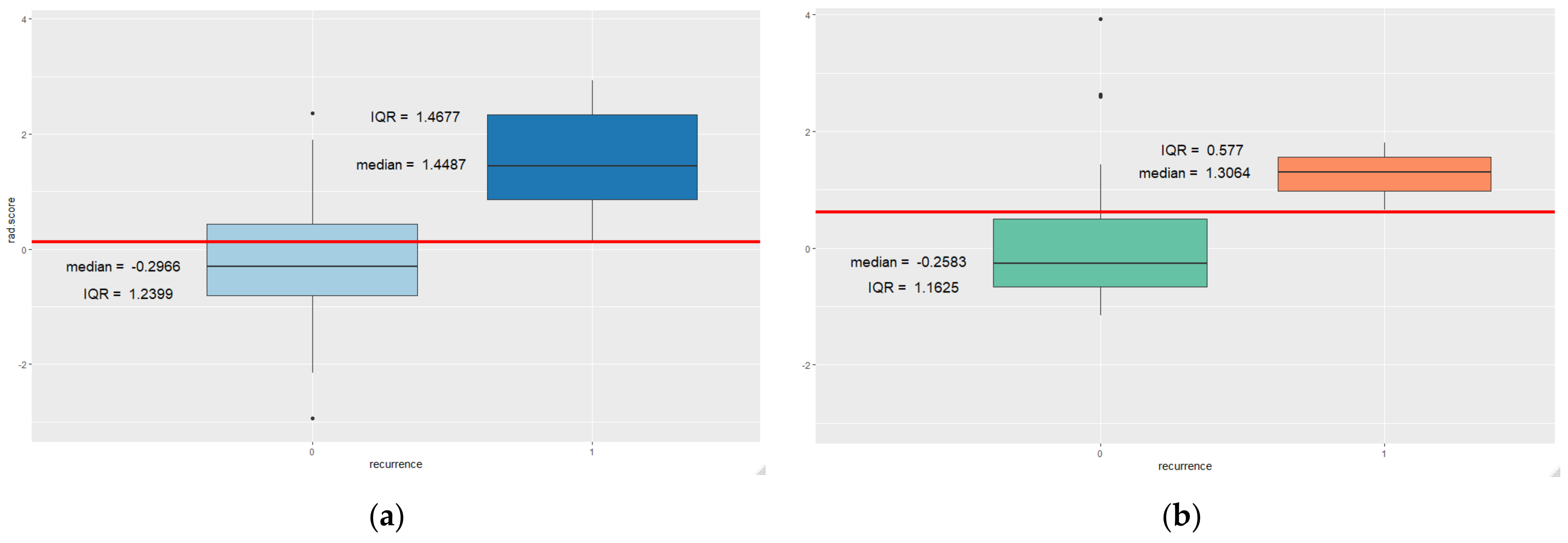
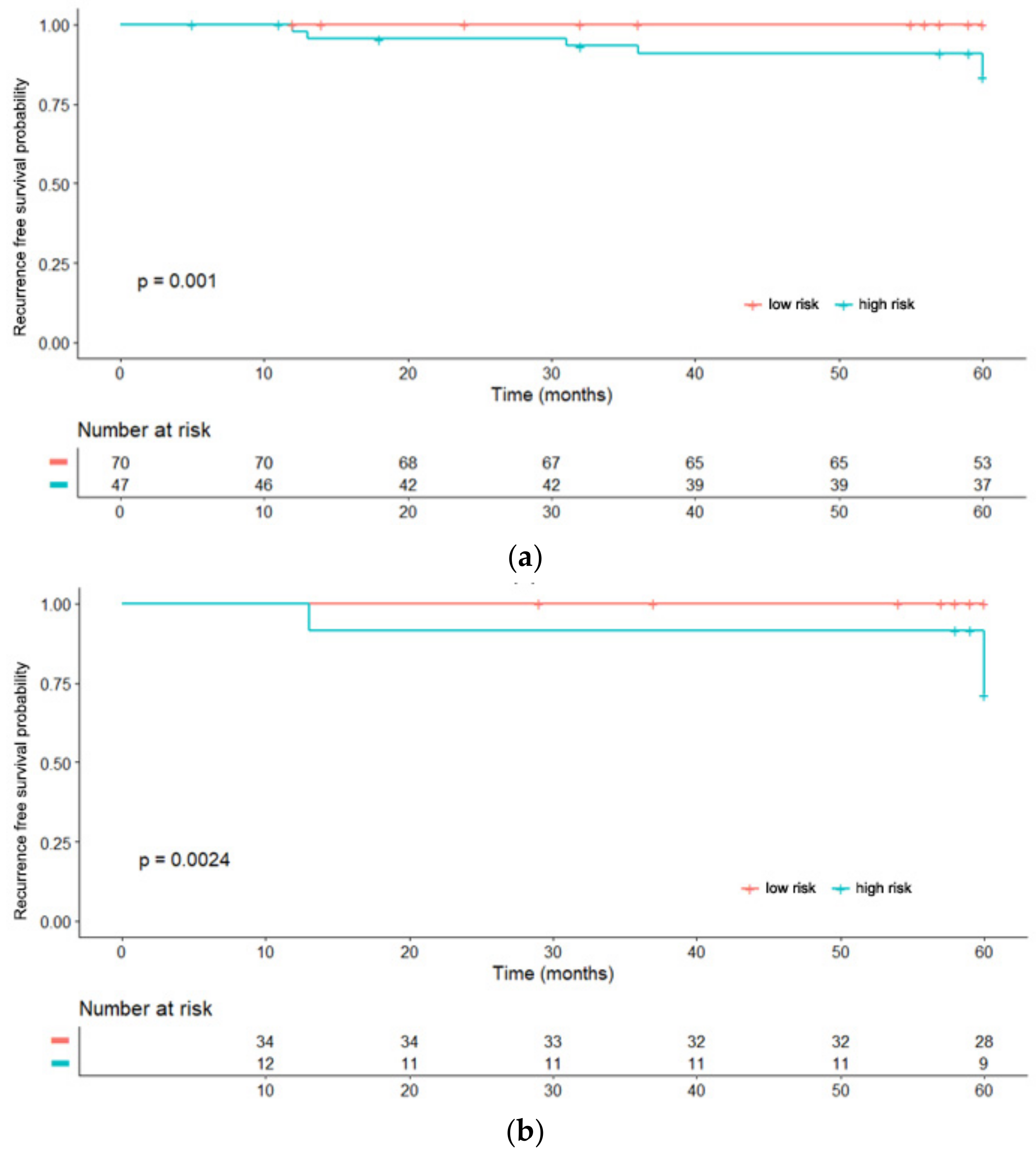
3.3. Rad-Score Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Allegra, C.J.; Aberle, D.R.; Ganschow, P.; Hahn, S.M.; Lee, C.N.; Millon-Underwood, S.; Pike, M.C.; Reed, S.; Saftlas, A.F.; Scarvalone, S.A.; et al. National Institutes of Health State-of-the-Science Conference Statement: Diagnosis and Management of Ductal Carcinoma In Situ 22–24 September 2009. JNCI J. Natl. Cancer Inst. 2010, 102, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2016. CA Cancer J. Clin. 2016, 66, 7–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Classification of Breast Tumours, 5th ed.; WHO Classification of Tumours: Geneva, Switzerland, 2019. [Google Scholar]
- Bijker, N.; Meijnen, P.; Peterse, J.L.; Bogaerts, J.; Van Hoorebeeck, I.; Julien, J.-P.; Gennaro, M.; Rouanet, P.; Avril, A.; Fentiman, I.S.; et al. Breast-Conserving Treatment with or Without Radiotherapy in Ductal Carcinoma-In-Situ: Ten-Year Results of European Organisation for Research and Treatment of Cancer Randomized Phase III Trial 10853—A Study by the EORTC Breast Cancer Cooperative Group and EORTC Radiotherapy Group. J. Clin. Oncol. 2006, 24, 3381–3387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holmberg, L.; Garmo, H.; Granstrand, B.; Ringberg, A.; Arnesson, L.-G.; Sandelin, K.; Karlsson, P.; Anderson, H.; Emdin, S. Absolute Risk Reductions for Local Recurrence After Postoperative Radiotherapy After Sector Resection for Ductal Carcinoma In Situ of the Breast. J. Clin. Oncol. 2008, 26, 1247–1252. [Google Scholar] [CrossRef]
- Cuzick, J.; Sestak, I.; Pinder, S.E.; Ellis, I.; Forsyth, S.; Bundred, N.J.; Forbes, J.F.; Bishop, H.; Fentiman, I.S.; George, W.D. Effect of tamoxifen and radiotherapy in women with locally excised ductal carcinoma in situ: Long-term results from the UK/ANZ DCIS trial. Lancet Oncol. 2011, 12, 21–29. [Google Scholar] [CrossRef]
- Wapnir, I.L.; Dignam, J.J.; Fisher, B.; Mamounas, E.P.; Anderson, S.; Julian, T.B.; Land, S.R.; Margolese, R.G.; Swain, S.; Costantino, J.P.; et al. Long-Term Outcomes of Invasive Ipsilateral Breast Tumor Recurrences After Lumpectomy in NSABP B-17 and B-24 Randomized Clinical Trials for DCIS. JNCI J. Natl. Cancer Inst. 2011, 103, 478–488. [Google Scholar] [CrossRef]
- Donker, M.; Litière, S.; Werutsky, G.; Julien, J.-P.; Fentiman, I.S.; Agresti, R.; Rouanet, P.; De Lara, C.T.; Bartelink, H.; Duez, N.; et al. Breast-Conserving Treatment with or Without Radiotherapy in Ductal Carcinoma In Situ: 15-Year Recurrence Rates and Outcome After a Recurrence, From the EORTC 10853 Randomized Phase III Trial. J. Clin. Oncol. 2013, 31, 4054–4059. [Google Scholar] [CrossRef]
- Wärnberg, F.; Garmo, H.; Emdin, S.; Hedberg, V.; Adwall, L.; Sandelin, K.; Ringberg, A.; Karlsson, P.; Arnesson, L.-G.; Anderson, H.; et al. Effect of Radiotherapy After Breast-Conserving Surgery for Ductal Carcinoma in Situ: 20 Years Follow-Up in the Randomized SweDCIS Trial. J. Clin. Oncol. 2014, 32, 3613–3618. [Google Scholar] [CrossRef]
- Barrio, A.V.; Van Zee, K.J. Controversies in the Treatment of Ductal Carcinoma in Situ. Annu. Rev. Med. 2017, 68, 197–211. [Google Scholar] [CrossRef] [Green Version]
- Castellano, G.; Bonilha, L.; Li, L.; Cendes, F. Texture analysis of medical images. Clin. Radiol. 2004, 59, 1061–1069. [Google Scholar] [CrossRef]
- Materka, A. Texture analysis methodologies for magnetic resonance imaging. Dialogues Clin. Neurosci. 2004, 6, 243–250. [Google Scholar]
- Gibbs, P.; Turnbull, L.W. Textural analysis of contrast-enhanced MR images of the breast. Magn. Reson. Med. 2003, 50, 92–98. [Google Scholar] [CrossRef]
- Grimm, L.J. Breast MRI radiogenomics: Current status and research implications. J. Magn. Reson. Imaging 2015, 43, 1269–1278. [Google Scholar] [CrossRef]
- Waugh, S.A.; Purdie, C.A.; Jordan, L.B.; Vinnicombe, S.; Lerski, R.A.; Martin, P.; Thompson, A.M. Magnetic resonance imaging texture analysis classification of primary breast cancer. Eur. Radiol. 2016, 26, 322–330. [Google Scholar] [CrossRef]
- Parikh, J.; Selmi, M.; Charles-Edwards, G.; Glendenning, J.; Ganeshan, B.; Verma, H.; Mansi, J.; Harries, M.; Tutt, A.; Goh, V. Changes in Primary Breast Cancer Heterogeneity May Augment Midtreatment MR Imaging Assessment of Response to Neoadjuvant Chemotherapy. Radiology 2014, 272, 100–112. [Google Scholar] [CrossRef]
- Henderson, S.; Purdie, C.; Michie, C.; Evans, A.; Lerski, R.; Johnston, M.; Vinnicombe, S.; Thompson, A.M. Interim heterogeneity changes measured using entropy texture features on T2-weighted MRI at 3.0 T are associated with pathological response to neoadjuvant chemotherapy in primary breast cancer. Eur. Radiol. 2017, 27, 4602–4611. [Google Scholar] [CrossRef] [Green Version]
- Li, J.; Song, Y.; Xu, S.; Wang, J.; Huang, H.; Ma, W.; Jiang, X.; Wu, Y.; Cai, H.; Li, L. Predicting underestimation of ductal carcinoma in situ: A comparison between radiomics and conventional approaches. Int. J. Comput. Assist. Radiol. Surg. 2018, 14, 709–721. [Google Scholar] [CrossRef]
- Hou, R.; Grimm, L.J.; Mazurowski, M.A.; Marks, J.R.; King, L.M.; Maley, C.C.; Lynch, T.; van Oirsouw, M.; Rogers, K.; Stone, N.; et al. Prediction of Upstaging in Ductal Carcinoma in Situ Based on Mammographic Radiomic Features. Radiology 2022, 2022, 210407. [Google Scholar] [CrossRef]
- Lee, E.B.; Kim, S.H.; Park, G.E.; Lee, J.; Kang, B.J. Risk Stratification of Ductal Carcinoma In Situ and Texture Analysis of Contrast-Enhanced Breast Magnetic Resonance Imaging. J. Comput. Assist. Tomogr. 2021, 45, 843–848. [Google Scholar] [CrossRef]
- Nam, Y.; Park, G.E.; Kang, J.; Kim, S.H. Fully Automatic Assessment of Background Parenchymal Enhancement on Breast MRI Using Machine-Learning Models. J. Magn. Reson. Imaging 2021, 53, 818–826. [Google Scholar] [CrossRef]
- Morris, E.A.; Comstock, C.E.; Lee, C.H. ACR BI-RADS® Magnetic Resonance Imaging. In ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System; American College of Radiology: Reston, VA, USA, 2013. [Google Scholar]
- Silverstein, M.J.; Lagios, M.D.; Groshen, S.; Waisman, J.R.; Lewinsky, B.S.; Martino, S.; Gamagami, P.; Colburn, W.J. The Influence of Margin Width on Local Control of Ductal Carcinoma in Situ of the Breast. N. Engl. J. Med. 1999, 340, 1455–1461. [Google Scholar] [CrossRef]
- Hwang, E.S.; Hyslop, T.; Lynch, T.; Frank, E.; Pinto, D.; Basila, D.; Collyar, D.; Bennett, A.; Kaplan, C.; Rosenberg, S.; et al. The COMET (Comparison of Operative versus Monitoring and Endocrine Therapy) trial: A phase III randomised controlled clinical trial for low-risk ductal carcinoma in situ (DCIS). BMJ Open 2019, 9, e026797. [Google Scholar] [CrossRef] [Green Version]
- Koh, J.; Lee, E.; Han, K.; Kim, S.; Kim, D.-K.; Kwak, J.Y.; Yoon, J.H.; Moon, H.J. Three-dimensional radiomics of triple-negative breast cancer: Prediction of systemic recurrence. Sci. Rep. 2020, 10, 2976. [Google Scholar] [CrossRef] [Green Version]
- Park, H.; Lim, Y.; Ko, E.S.; Cho, H.-H.; Lee, J.E.; Han, B.-K.; Ko, E.Y.; Choi, J.S.; Park, K.W. Radiomics Signature on Magnetic Resonance Imaging: Association with Disease-Free Survival in Patients with Invasive Breast Cancer. Clin. Cancer Res. 2018, 24, 4705–4714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fox, M.J.; Gibbs, P.; Pickles, M.D. Minkowski functionals: An MRI texture analysis tool for determination of the aggressiveness of breast cancer. J. Magn. Reson. Imaging 2016, 43, 903–910. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.A.; Cho, N.; Ryu, E.B.; Seo, M.; Bae, M.S.; Chang, J.M.; Moon, W.K. Background parenchymal signal enhancement ratio at preoperative MR imaging: Association with subsequent local recurrence in patients with ductal carcinoma in situ after breast conservation surgery. Radiology 2014, 270, 699–707. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Johnston, B.S.; Kitsch, A.E.; Hippe, D.S.; Korde, L.A.; Javid, S.; Lee, J.M.; Peacock, S.; Lehman, C.D.; Partridge, S.C.; et al. Ductal Carcinoma in Situ: Quantitative Preoperative Breast MR Imaging Features Associated with Recurrence after Treatment. Radiology 2017, 285, 788–797. [Google Scholar] [CrossRef]
- Sung, J.S.; Corben, A.D.; Brooks, J.D.; Edelweiss, M.; Keating, D.M.; Lin, C.; Morris, E.A.; Patel, P.; Robson, M.; Woods, M.; et al. Histopathologic characteristics of background parenchymal enhancement (BPE) on breast MRI. Breast Cancer Res. Treat. 2018, 172, 487–496. [Google Scholar] [CrossRef]
- Mema, E.; Mango, V.L.; Guo, X.; Karcich, J.; Yeh, R.; Wynn, R.T.; Zhao, B.; Ha, R.S. Does breast MRI background parenchymal enhancement indicate metabolic activity? Qualitative and 3D quantitative computer imaging analysis. J. Magn. Reson. Imaging 2017, 47, 753–759. [Google Scholar] [CrossRef]
- Dontchos, B.N.; Rahbar, H.; Partridge, S.C.; Korde, L.A.; Lam, D.L.; Scheel, J.; Peacock, S.; Lehman, C.D. Are Qualitative Assessments of Background Parenchymal Enhancement, Amount of Fibroglandular Tissue on MR Images, and Mammographic Density Associated with Breast Cancer Risk? Radiology 2015, 276, 371–380. [Google Scholar] [CrossRef] [Green Version]
- Telegrafo, M.; Rella, L.; Ianora, A.A.S.; Angelelli, G.; Moschetta, M. Breast MRI background parenchymal enhancement (BPE) correlates with the risk of breast cancer. Magn. Reson. Imaging 2016, 34, 173–176. [Google Scholar] [CrossRef]
- Arasu, V.A.; Miglioretti, D.L.; Sprague, B.L.; Alsheik, N.H.; Buist, D.S.; Henderson, L.M.; Herschorn, S.D.; Lee, J.M.; Onega, T.; Rauscher, G.H.; et al. Population-Based Assessment of the Association Between Magnetic Resonance Imaging Background Parenchymal Enhancement and Future Primary Breast Cancer Risk. J. Clin. Oncol. 2019, 37, 954–963. [Google Scholar] [CrossRef]
- Thompson, C.M.; Mallawaarachchi, I.; Dwivedi, D.K.; Ayyappan, A.P.; Shokar, N.K.; Lakshmanaswamy, R.; Dwivedi, A.K. The Association of Background Parenchymal Enhancement at Breast MRI with Breast Cancer: A Systematic Review and Meta-Analysis. Radiology 2019, 292, 552–561. [Google Scholar] [CrossRef]
| Patients with No Recurrence (n = 153) | Patients with Ipsilateral Recurrence (n = 10) | p-Value | |
|---|---|---|---|
| Age | 52.9 ± 9.8 | 46.5 ± 7.5 | 0.05 |
| Last outpatient follow-up (months) | 82.2 ± 26.5 | 51.7 ± 36.1 | 0.009 |
| Surgery type | 0.109 | ||
| Total mastectomy | 100 | 9 | |
| BCS | 53 | 1 | |
| Radiation therapy | 0.343 | ||
| No | 100 | 8 | |
| Yes | 53 | 2 | |
| Endocrine therapy | 0.607 | ||
| No | 111 | 8 | |
| Yes | 42 | 2 | |
| DCIS size | 2.51 ± 1.89 | 2.35 ± 1.99 | 0.814 |
| DCIS nuclear grade | 0.075 | ||
| Non-high | 75 | 2 | |
| High | 78 | 8 | |
| Comedo necrosis | 0.128 | ||
| Negative | 50 | 1 | |
| Positive | 101 | 9 | |
| ER | 0.078 | ||
| Negative | 115 | 7 | |
| Positive | 38 | 3 | |
| PR | 0.765 | ||
| Positive | 100 | 7 | |
| Negative | 53 | 3 | |
| HER2 | 0.479 | ||
| Negative | 108 | 6 | |
| Positive | 45 | 4 | |
| Ki-67 (%) | 0.669 | ||
| <14% | 94 | 5 | |
| ≥14% | 56 | 4 | |
| IHC type | 0.562 | ||
| Luminal | 114 | 7 | |
| HER2-enriched | 26 | 3 | |
| Basal-like | 12 | 0 | |
| VNPG | |||
| Low risk | 38 | 1 | 0.287 |
| Non-low risk | 115 | 9 | |
| Comet classification | 0.031 | ||
| Low risk | 68 | 1 | |
| Non-low risk | 84 | 9 | |
| Resection margin (2 mm) | 0.078 | ||
| Negative | 136 | 7 | |
| Positive | 17 | 3 | |
| Fibroglandular tissue (FGT) | 0.743 | ||
| Almost entirely fat, Scattered | 54 | 3 | |
| Heterogenoues, Extreme | 99 | 7 | |
| Background parenchymal enhancement (BPE) | 0.028 | ||
| Minimal, Mild | 122 | 5 | |
| Mild, Marked | 31 | 5 |
| Training Cohort (n = 117) | Validation Cohort (n = 46) | p-Value | |
|---|---|---|---|
| Age | 53.5 ± 10.2 | 50.1 ± 8.13 | 0.12 |
| Surgery type | 0.41 | ||
| Total mastectomy | 42 | 12 | |
| BCS | 75 | 34 | |
| Radiation therapy | 0.41 | ||
| No | 44 | 11 | |
| Yes | 73 | 35 | |
| Endocrine therapy | 0.10 | ||
| No | 28 | 12 | |
| Yes | 78 | 41 | |
| Ipsilateral recurrence | 1 * | ||
| No recurrence | 110 | 43 | |
| Recurrence | 7 | 3 | |
| DCIS size (cm) | 2.52 ± 1.88 | 2.43 ± 1.94 | 0.62 |
| DCIS nuclear grade | 0.34 | ||
| Non-high | 58 | 19 | |
| High | 59 | 27 | |
| Comedo necrosis | 0.17 | ||
| Negative | 41 | 11 | |
| Positive | 76 | 35 | |
| ER | 0.80 | ||
| Negative | 29 | 12 | |
| Positive | 88 | 34 | |
| PR | 0.86 | ||
| Negative | 34 | 20 | |
| Positive | 72 | 33 | |
| HER2 | 0.23 | ||
| Negative | 85 | 29 | |
| Positive | 32 | 17 | |
| Ki-67 (%) | 14.8 ± 14.7 | 10.9 ± 8.21 | 0.41 |
| IHC_type | 0.69 | ||
| Luminal | 88 | 34 | |
| HER2-enriched | 19 | 10 | |
| Basal-like | 10 | 2 | |
| VNPG | 0.22 | ||
| Low risk | 31 | 8 | |
| Non-low risk | 86 | 38 | |
| COMET classification | 0.33 | ||
| Low risk | 53 | 17 | |
| Non-low risk | 64 | 29 | |
| Resection margin (2 mm) | 0.85 | ||
| Negative | 103 | 40 | |
| Positive | 14 | 6 | |
| Fibroglandular tissue (FGT) | 0.79 | ||
| Almost entirely fat, Scattered | 43 | 14 | |
| Heterogeneous, Extreme | 74 | 32 | |
| Background parenchymal enhancement (BPE) | 0.70 | ||
| Minimal, Mild | 93 | 34 | |
| Moderate, Marked | 24 | 12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, G.E.; Kim, S.H.; Lee, E.B.; Nam, Y.; Sung, W. Ipsilateral Recurrence of DCIS in Relation to Radiomics Features on Contrast Enhanced Breast MRI. Tomography 2022, 8, 596-606. https://doi.org/10.3390/tomography8020049
Park GE, Kim SH, Lee EB, Nam Y, Sung W. Ipsilateral Recurrence of DCIS in Relation to Radiomics Features on Contrast Enhanced Breast MRI. Tomography. 2022; 8(2):596-606. https://doi.org/10.3390/tomography8020049
Chicago/Turabian StylePark, Ga Eun, Sung Hun Kim, Eun Byul Lee, Yoonho Nam, and Wonmo Sung. 2022. "Ipsilateral Recurrence of DCIS in Relation to Radiomics Features on Contrast Enhanced Breast MRI" Tomography 8, no. 2: 596-606. https://doi.org/10.3390/tomography8020049
APA StylePark, G. E., Kim, S. H., Lee, E. B., Nam, Y., & Sung, W. (2022). Ipsilateral Recurrence of DCIS in Relation to Radiomics Features on Contrast Enhanced Breast MRI. Tomography, 8(2), 596-606. https://doi.org/10.3390/tomography8020049






