Abstract
A relevant issue on the treatment of adrenocortical carcinoma (ACC) concerns the optimal duration of adjuvant mitotane treatment. We tried to address this question, assessing whether a correlation exists between the duration of adjuvant mitotane treatment and recurrence-free survival (RFS) of patients with ACC. We conducted a multicenter retrospective analysis on 154 ACC patients treated for ≥12 months with adjuvant mitotane after radical surgery and who were free of disease at the mitotane stop. During a median follow-up of 38 months, 19 patients (12.3%) experienced recurrence. We calculated the RFS after mitotane (RFSAM), from the landmark time-point of mitotane discontinuation, to overcome immortal time bias. We found a wide variability in the duration of adjuvant mitotane treatment among different centers and also among patients cared for at the same center, reflecting heterogeneous practice. We did not find any survival advantage in patients treated for longer than 24 months. Moreover, the relationship between treatment duration and the frequency of ACC recurrence was not linear after stratifying our patients in tertiles of length of adjuvant treatment. In conclusion, the present findings do not support the concept that extending adjuvant mitotane treatment over two years is beneficial for ACC patients with low to moderate risk of recurrence.
1. Introduction
Adrenocortical carcinoma (ACC) is a rare tumor characterized by an aggressive disease course that limits long-term survival [1,2,3]. Disease-specific outcomes are better for patients bearing early-stage tumors that can be resected completely; however, post-operative recurrence of ACC may be considered as part of the natural history of the disease [4,5,6,7,8]. We have recently reported a recurrence rate of 62.5% among 152 patients with stage I to III ACC who underwent complete macroscopic resection, with a five-year recurrence-free survival rate of 38.1% [9].
The remarkable propensity of ACC towards recurrence despite complete surgical removal makes a strong case for an adjuvant therapy. Until now, the most followed adjuvant approach relied on mitotane, an old adrenolytic drug specifically approved for treatment of advanced ACC [10,11]. Use of adjuvant mitotane increased in clinical practice following the observation that adjuvant mitotane treatment was associated with prolonged recurrence-free survival (RFS) compared to surveillance without active treatment after surgery, in a retrospective study of 177 ACC patients managed at different institutions using either adjuvant mitotane or no treatment. In this cohort study, we included 47 patients followed at Italian reference centers that systematically adopted adjuvant mitotane to all radically operated ACC, and a group of 55 Italian patients and 75 German patients followed in centers not giving any post-operative treatment [12]. In this study, we showed that adjuvant mitotane treatment was associated with a significant survival advantage. Despite the retrospective nature of the study, this finding informed clinical practice, although adjuvant mitotane is not universally accepted and some experts argue against the value of this approach [13,14]. Critics of adjuvant mitotane therapy evoke the drug-related toxicity, the complexity of caring for patients on treatment, and the long duration of a treatment course [15].
The overall level of evidence available on adjuvant mitotane can be graded as low, and all recommendations are based on retrospective, non-randomized studies, plagued by potential bias and confounding [10,16]. Despite this evidence gap, adjuvant mitotane is advised for patients with ACC at high risk of recurrence in the clinical guidelines endorsed by the European Society for Endocrinology (ESE)–European Network for the Study of Adrenal Tumours (ENSAT) and by the European Society for Medical Oncology (ESMO) [10,17]. The guidelines underline that scant information is currently available on many aspects dealing with practical management of mitotane therapy. Recommendations on how to conduct adjuvant mitotane treatment are mostly based on expert opinions stemming from personal experience and practice [18]. As a consequence, care of patients treated with mitotane is heterogeneous depending on local preferences.
One of the most relevant and uncertain issues concerns the optimal duration of adjuvant mitotane treatment. The ESE-ENSAT guidelines and ESMO guidelines suggest continued use of adjuvant mitotane for at least 2 years, but not longer than 5 years [10,17]. Since no study has ever specifically addressed this issue, this recommendation is based on the observation that most recurrences of ACC occur within two years after resection, while after 5 years, the rate of recurrence is too low to justify continuation of adjuvant therapy.
What is the optimal duration of adjuvant mitotane treatment, however, remains controversial, and practice varies even among referral centers. This issue has important consequences on both patient-centered outcomes, due to the unwanted effects of treatment and their impact on quality of life and health-care organizations, as surveillance of patients on mitotane is demanding and resource-consuming.
We tried to answer this question by organizing an international, multicentric, retrospective study aimed at assessing whether a correlation does exist between duration of adjuvant mitotane treatment and recurrence-free survival of patients with ACC.
2. Patients and Methods
2.1. Patients
We did an international, multicenter, retrospective analysis on 154 patients with ACC treated with adjuvant mitotane after radical surgery. Thirteen European centers and one center in Canada participated in the study.
To be included, patients had to meet the following inclusion criteria: age of 18 years or older at the time of diagnosis; histologically confirmed diagnosis of ACC (based on Weiss score [19]; ENSAT stage I-III [20]; R0 or Rx tumor resection, defined on the basis of a surgical report, pathology report, and post-operative imaging); treatment with adjuvant mitotane for at least 12 months following surgery; and clinical status being free of disease at the time of mitotane discontinuation. Exclusion criteria were: residual disease after resection, defined both microscopically or macroscopically (resection status, R1 or R2); patients concomitantly treated with other therapies (e.g., chemotherapy or radiotherapy); or patients experiencing ACC recurrence during adjuvant mitotane therapy. Follow-up for this study was closed in December 2017.
2.2. Methods
All data were obtained by reviewing patient history, medical records, and source documents. Data were processed by skilled and experienced personnel using specifically tailored data forms. We reported clinical and demographical characteristics, the date and type of surgery, stage at diagnosis, pathology reports (Weiss score and Ki-67 index), hormonal status, date of start and stop of mitotane treatment and reason for stops, date of recurrence and type of recurrence (single or multiple, local or distant), and the date of last follow-up or death. Date of diagnosis was defined as the date of surgery. Tumor stage was established according to the ENSAT classification (I, confined tumors ≤5 cm; II, confined tumors >5 cm; III, positive lymph nodes or infiltrating neighboring organs/veins without distant metastases; IV, distant metastases) [20]. Date of recurrence was defined as the date of radiological evidence of a new lesion. Patients underwent imaging follow-up (abdominal and thoracic computed tomography) every 3–4 months. Modalities of mitotane treatment, such as the initial high- or low-dose regimen, dose titration, and eventual dose changes due to toxicity were done according to local center preferences.
2.3. Statistical Analysis
The primary endpoint was to determine whether a correlation between duration of adjuvant mitotane treatment and patient survival did exist.
Frequencies and percentages were calculated for categorical data, and the median and interquartile range for continuous data. Differences in categorical variables were analyzed by means of the chi-squared test or Fisher test, as appropriate, while differences in continuous variables were analyzed by the Mann–Whitney U test. The survival curves were estimated with the Kaplan–Meyer product limit method. Recurrence-free survival (RFS) was calculated from the time of initial surgery to the first radiological evidence of recurrence. To adjust for the immortal bias due to the selection of patients who did not have recurrence on active treatment, we calculated the recurrence-free survival rate after adjuvant mitotane discontinuation (RFSAM) from the time of discontinuation of mitotane to ACC recurrence or end of follow-up. We calculated the overall survival rate after adjuvant mitotane discontinuation (OSAM) from the time of discontinuation of mitotane to the date of death. Patients who did not experience either of those events (recurrence or death) were censored at the date of the last follow-up visit for the specific survival analysis. Cox proportional hazards regression models were fitted to determine prognostic factors on survival. The following potential predictive factors for RFS and RFSAM were investigated: patient sex and age, tumor stage, hormone secretion, Weiss score, Ki67 index, mitoses, resection status, and duration of mitotane treatment. A genetic algorithm was employed to select the variables that resulted in the best-fitted model according to AIC score [21]. Firth correction was applied to reduce the bias due to the small number of events [22]. All reported P values are two-sided. P-values of less than 0.05 were considered as statistically significant. All statistical analyses were performed using R version 4.0.2.
3. Results
Baseline characteristics of patients are reported in Table 1.

Table 1.
Baseline characteristics of patients.
In our series, female sex was more prevalent, and ACC presented, in most cases, as a stage II hormone-secreting tumor. The present series was skewed toward low-grade tumors with a Ki67 index of less than 10%. Median duration of adjuvant mitotane therapy was 33 months (IQR, 24–59), and median follow-up after mitotane discontinuation was 38 months (IQR, 24–61).
We stratified our patients into three groups by treatment duration (expressed in tertiles); group 1 included patients treated for 13–25 months, group 2 for 26–48 months, and group 3 for 49–143 months, respectively. Group 3 had a higher Ki67 index, longer RFS compared to groups 1 and 2, and longer RFSAM compared to group 2 (Table 2).

Table 2.
Baseline characteristics of patients in different groups stratified by duration of therapy.
In most cases, mitotane was interrupted at the end of the scheduled period. Only in a few patients, treatment-related unwanted effects induced mitotane stop (Table 3), mainly during the second year of therapy.

Table 3.
Causes of mitotane discontinuation in different groups stratified by duration of therapy.
After excluding patients in which mitotane withdrawal was determined by adverse effects, we observed a wide variability in the duration of adjuvant mitotane, either among different centers or in the same center, as shown in Figure 1.

Figure 1.
Distribution of the duration of adjuvant mitotane for each center (only centers with at least five patients have been included in this analysis). 1 = Berlin; 2 = Munich; 3 = Wurzburg; 4 = Florence; 5 = Orbassano; 6 = Padua; 7 = IGR (Villejuif); 8 = Montreal. N = number of patients.
In our series, 19 patients experienced recurrence after mitotane discontinuation. Recurrence types were almost equally distributed between those which were local (10 cases, 53%) and distant (9 cases, 47%); the last ones mainly in the lung (6 cases). After mitotane discontinuation, death occurred in three patients, but in only one case the death was cancer-related.
To assess where any correlation did exist between adjuvant mitotane duration and RSF, we tried different approaches. We stratified our patients by the value of 24 months’ treatment duration. The comparison of the survival curves of patients treated up to 24 months vs. patients treated for a longer period, both for RFS (Figure 2) and RFSAM (Figure 3), did not show any significant difference.

Figure 2.
Kaplan–Meier estimates of recurrence-free survival (RFS) in patients treated <24 months versus patients treated >24 months.
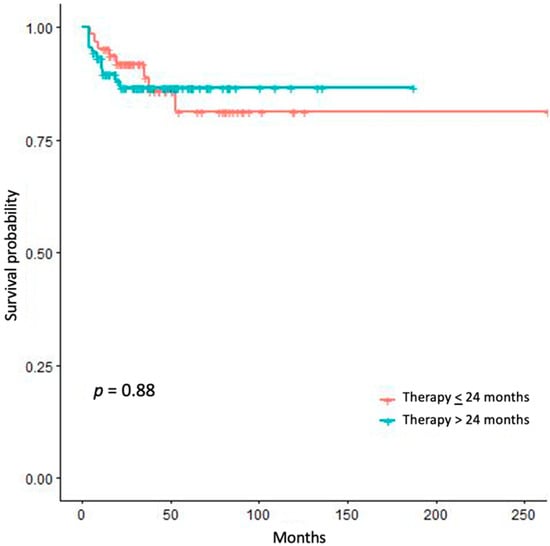
Figure 3.
Kaplan–Meier estimates of recurrence free survival after adjuvant mitotane discontinuation (RFSAM) in patients treated <24 months vs. patients treated >24 months.
We performed univariate analyses, both for RFS (Table 4) and RFSAM (Table 5), without identifying any significant prognostic factors.

Table 4.
Univariate analysis of predictive factors for recurrence-free survival (RFS).

Table 5.
Univariate analysis of predictive factors for recurrence free survival after adjuvant mitotane discontinuation (RFSAM).
At a multivariate level, the variables’ duration of adjuvant mitotane, which was modelled with a spline to account for non-linearity, sex, and Weiss were selected in the best-fitted model. Duration of adjuvant mitotane was the only statistically significant factor associated with RFS (HR 0.549, 95% CI 0.306–0.983; p = 0.044). The HR was calculated on a difference of 18 months in the duration of therapy, that is, 18 months’ increase of adjuvant mitotane therapy duration is associated with about 45% reduction in the hazard of RFS. No statistically significant factor resulted to be associated with RFSAM, or OSAM.
4. Discussion
The present findings do not support the concept that a longer duration of mitotane therapy (more than 2 years) is associated with a survival advantage. Since the present series was enriched with low-risk tumors, these results may be not generalizable to high-risk ACC. Although RFS was prolonged in patients treated for more than 4 years, this finding may likely be the consequence of immortal time bias.
The inclusion criteria of the study may induce an immortal bias in patients scheduled to be treated for longer periods, since these patients could not have recurred in the months prior to mitotane discontinuation, as otherwise they would have been excluded from analysis. For this reason, we primarily focused on the outcome after the end of scheduled adjuvant treatment, of whatever duration it was. We calculated the recurrence-free survival rate after mitotane (RFSAM), from the landmark time-point of mitotane discontinuation, since landmark analysis is a method used to overcome immortal time bias [23].
The duration of mitotane therapy was a factor associated to RFS but not RFSAM, and this militates against an actual benefit of prolonging adjuvant mitotane treatment. Along these lines, the breakdown of RFS by 24 months of treatment duration, which is the recommended time-length of adjuvant mitotane according to the ESE-ENSAT and ESMO guidelines [10,17], did not disclose any survival advantage of patients treated for longer. Moreover, the relationship between treatment duration and the frequency of ACC recurrence was not linear after stratifying our patients in tertiles of length of adjuvant treatment.
An interesting finding is that a large variability in the duration of adjuvant mitotane treatment does appear between different centers, and also among patients cared for at the same center. This figure reflects uncertainty on management and heterogeneous practice. However, it appears that physicians were more eager to treat patients with unfavorable prognostic factors (higher Ki-67 index) for longer periods, although our series was selected toward low-risk tumors due to the specific inclusion criteria of the study (patients who did recur on treatment were excluded). That said, a sort of “geographical” pattern does appear, since at centers in Germany, adjuvant mitotane was generally discontinued after two years, whereas in Italian centers it was usually more prolonged. In these centers, however, there was a huge variability between patients, suggesting that a tailored approach, taking into account patient preferences and biological characteristics of ACC, was followed. The heterogeneity in practice between expert centers underlines the lack of evidence on this issue since, to the best of our knowledge, this is the first study that specifically addresses the issue of the duration of adjuvant mitotane therapy. As a matter of fact, duration of adjuvant mitotane was very heterogenous between studies on this topic [14,24,25,26,27,28].
The main issue with a retrospective analysis of treatment duration is that in many cases, the length of adjuvant treatment is set by the timing of ACC recurrence, and not by the planned treatment schedule. In this retrospective multicenter study carried out in referral centers for ACC that are part of ENSAT, we tried to overcome this problem by including only patients treated with adjuvant mitotane for at least 12 months, in which mitotane was suspended for reasons different from recurrence of disease. Consequently, all patients were free of disease at the end of adjuvant therapy.
Recognizing that a prospective randomized trial that includes patients with ACC treated with adjuvant mitotane for different, pre-specified time lengths is the best way to define what is the optimal duration of treatment, it can be plainly accepted that such a trial is not on the horizon for the near future. Up to now, only two randomized trials have been concluded on ACC [29,30], and this outlines how it is challenging to implement a randomized trial in a rare tumor such as ACC. Therefore, a well-designed retrospective study is almost all that can be done to answer this important clinical question.
5. Conclusions
In this study, we have addressed the challenging issue of identifying the optimal duration of adjuvant mitotane therapy in a retrospective analysis. We tried to overcome the bias and confounding inherent to a retrospective analysis of treatment duration by multiple approaches. With all the disclosed limits of our study, the present findings do not support the concept that extending adjuvant mitotane treatment over two years is beneficial for patients with ACC at low risk of recurrence. Conversely, patients with ACC at high risk of recurrence were under-represented in this study, thus precluding any definitive recommendations.
Answering the question of what is the optimal duration of adjuvant mitotane is an unmet clinical need, since current practice is heterogeneous and mainly dependent on personal preferences and expertise. To the best of our knowledge, no previous study has specifically addressed this point, and the recommendation of a standard duration of adjuvant mitotane treatment of two years is not based on specific evidence. Lacking randomized studies, which will be hardly feasible in the future, the present study does provide the only evidence available on this complex issue. Finding that no obvious advantage is associated to prolonged adjuvant mitotane treatment provides some guidance for the care of patients with ACC, and sparing low-risk patients from long exposure to a toxic treatment matters for clinical practice.
Author Contributions
Conceptualization, V.B., S.P., M.F., and M.T.; methodology, P.P. and P.B.; software, not pertinent; validation, P.P. and P.B.; formal analysis, V.B., S.P., P.P., P.B., M.T.; investigation, V.B., S.P., B.A., L.C., R.L., F.C., F.B., M.Q., A.C., U.D., F.M., E.B., I.B., A.L., P.L., A.B., D.K., H.R.H.; resources, M.T.; data curation, V.B., S.P., A.C., B.A., L.C., R.L., F.C., F.B., M.Q., A.C., U.D., F.M., E.B., I.B., A.L., P.L., A.B., D.K., H.R.H.; writing—original draft preparation, V.B., S.P., M.T.; writing—review and editing, V.B., S.P. B.A., L.C., R.L., F.C., F.B., M.Q., A.C., P.P., P.B., U.D., F.M., E.B., I.B., A.L., P.L., A.B., D.K., H.R.H., M.F., M.T.; visualization, V.B., S.P., M.T.; supervision, M.F. and M.T.; project administration, M.T.; funding acquisition, M.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by “Associazione Italiana per la Ricerca sul Cancro” (AIRC), grant number IG2019-23069 to Massimo Terzolo.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. Ethical review and approval were waived for this study, due to the retrospective nature of the study and use of anonymized data.
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study and use of anonymized data.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
This project has been supported by the European Network for the Study of Adrenal Tumors (ENS@T). This work is generated within the European Reference Network for EndoERN (Adrenal).
Conflicts of Interest
Puglisi Soraya has received a grant for scientific writing from HRA Pharma; Massimo Terzolo has received research grants from HRA Pharma, and advisory board honoraria from HRA Pharma and Corcept Therapeutics; the others authors have stated explicitly that there are no conflicts of interest in connection with this article. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Else, T.; Kim, A.C.; Sabolch, A.; Raymond, V.M.; Kandathil, A.; Caoili, E.M.; Jolly, S.; Miller, B.S.; Giordano, T.J.; Hammer, G.D. Adrenocortical carcinoma. Endocr. Rev. 2014, 35, 282–326. [Google Scholar] [CrossRef]
- Tierney, J.F.; Chivukula, S.V.; Poirier, J.; Pappas, S.G.; Schadde, E.; Hertl, M.; Kebebew, E.; Keutgen, X. National Treatment Practice for Adrenocortical Carcinoma: Have They Changed and Have We Made Any Progress? J. Clin. Endocrinol. Metab. 2019, 104, 5948–5956. [Google Scholar] [CrossRef] [PubMed]
- Souteiro, P.; Donato, S.; Costa, C.; Pereira, C.A.; Simoes-Pereira, J.; Oliveira, J.; Belo, S.; Santos, A.P.; Cardoso, H.; Leite, V.; et al. Diagnosis, treatment, and survival analysis of adrenocortical carcinomas: A multicentric study. Hormones 2020, 19, 197–203. [Google Scholar] [CrossRef]
- Amini, N.; Margonis, G.A.; Kim, Y.; Tran, T.B.; Postlewait, L.M.; Maithel, S.K.; Wang, T.S.; Evans, D.B.; Hatzaras, I.; Shenoy, R.; et al. Curative Resection of Adrenocortical Carcinoma: Rates and Patterns of Postoperative Recurrence. Ann. Surg. Oncol. 2016, 23, 126–133. [Google Scholar] [CrossRef]
- Bedrose, S.; Daher, M.; Altameemi, L.; Habra, M.A. Adjuvant Therapy in Adrenocortical Carcinoma: Reflections and Future Directions. Cancers 2020, 12, 508. [Google Scholar] [CrossRef]
- Lo, W.M.; Kariya, C.M.; Hernandez, J.M. Operative Management of Recurrent and Metastatic Adrenocortical Carcinoma: A Systematic Review. Am. Surg. 2019, 85, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Glenn, J.A.; Else, T.; Hughes, D.T.; Cohen, M.S.; Jolly, S.; Giordano, T.J.; Worden, F.P.; Gauger, P.G.; Hammer, G.D.; Miller, B.S. Longitudinal patterns of recurrence in patients with adrenocortical carcinoma. Surgery 2019, 165, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Gaujoux, S.; Mihai, R.; Carnaille, B.; Dousset, B.; Fiori, C.; Porpiglia, F.; Hellman, P.; Iacobone, M.; Kraimps, J.L.; Donatini, G.; et al. European Society of Endocrine Surgeons (ESES) and European Network for the Study of Adrenal Tumours (ENSAT) recommendations for the surgical management of adrenocortical carcinoma. Br. J. Surg. 2017, 104, 358–376. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, A.; Basile, V.; Puglisi, S.; Perotti, P.; Pia, A.; Saba, L.; Berchialla, P.; Porpiglia, F.; Veltri, A.; Volante, M.; et al. Adjuvant mitotane therapy is beneficial in non-metastatic adrenocortical carcinoma at high risk of recurrence. Eur. J. Endocrinol. 2019, 180, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Fassnacht, M.; Dekkers, O.M.; Else, T.; Baudin, E.; Berruti, A.; de Krijger, R.; Haak, H.R.; Mihai, R.; Assie, G.; Terzolo, M. European Society of Endocrinology Clinical Practice Guidelines on the management of adrenocortical carcinoma in adults, in collaboration with the European Network for the Study of Adrenal Tumors. Eur. J. Endocrinol. 2018, 179, G1–G46. [Google Scholar] [CrossRef]
- Paragliola, R.M.; Corsello, A.; Locantore, P.; Papi, G.; Pontecorvi, A.; Corsello, S.M. Medical Approaches in Adrenocortical Carcinoma. Biomedicines 2020, 8, 551. [Google Scholar] [CrossRef]
- Terzolo, M.; Angeli, A.; Fassnacht, M.; Daffara, F.; Tauchmanova, L.; Conton, P.A.; Rossetto, R.; Buci, L.; Sperone, P.; Grossrubatscher, E.; et al. Adjuvant mitotane treatment for adrenocortical carcinoma. N. Engl. J. Med. 2007, 356, 2372–2380. [Google Scholar] [CrossRef]
- Huang, H.; Fojo, T. Adjuvant mitotane for adrenocortical cancer—A recurring controversy. J. Clin. Endocrinol. Metab. 2008, 93, 3730–3732. [Google Scholar] [CrossRef]
- Bertherat, J.; Coste, J.; Bertagna, X. Adjuvant mitotane in adrenocortical carcinoma. N. Engl. J. Med. 2007, 357, 1256–1257, author reply 1259. [Google Scholar] [CrossRef] [PubMed]
- Puglisi, S.; Calabrese, A.; Basile, V.; Pia, A.; Reimondo, G.; Perotti, P.; Terzolo, M. New perspectives for mitotane treatment of adrenocortical carcinoma. Best Pract. Res. Clin. Endocrinol. Metab. 2020, 101415. [Google Scholar] [CrossRef]
- Tang, Y.; Liu, Z.; Zou, Z.; Liang, J.; Lu, Y.; Zhu, Y. Benefits of Adjuvant Mitotane after Resection of Adrenocortical Carcinoma: A Systematic Review and Meta-Analysis. Biomed. Res. Int. 2018, 2018, 9362108. [Google Scholar] [CrossRef]
- Fassnacht, M.; Assie, G.; Baudin, E.; Eisenhofer, G.; de la Fouchardiere, C.; Haak, H.R.; de Krijger, R.; Porpiglia, F.; Terzolo, M.; Berruti, A.; et al. Adrenocortical carcinomas and malignant phaeochromocytomas: ESMO-EURACAN Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2020, 31, 1476–1490. [Google Scholar] [CrossRef] [PubMed]
- Puglisi, S.; Perotti, P.; Cosentini, D.; Roca, E.; Basile, V.; Berruti, A.; Terzolo, M. Decision-making for adrenocortical carcinoma: Surgical, systemic, and endocrine management options. Expert Rev. Anticancer Ther. 2018, 18, 1125–1133. [Google Scholar] [CrossRef]
- Weiss, L.M.; Medeiros, L.J.; Vickery, A.L. Pathologic features of prognostic significance in adrenocortical carcinoma. Am. J. Surg. Pathol. 1989, 13, 202–206. [Google Scholar] [CrossRef] [PubMed]
- Fassnacht, M.; Johanssen, S.; Quinkler, M.; Bucsky, P.; Willenberg, H.S.; Beuschlein, F.; Terzolo, M.; Mueller, H.H.; Hahner, S.; Allolio, B.; et al. Limited prognostic value of the 2004 International Union Against Cancer staging classification for adrenocortical carcinoma: Proposal for a Revised TNM Classification. Cancer 2009, 115, 243–250. [Google Scholar] [CrossRef]
- Burnham, K.P.; Anderson, D.R. Model Selection and Multimodel Inference; Springer: New York, NY, USA, 2002. [Google Scholar]
- Heinze, G.; Schemper, M. A solution to the problem of monotone likelihood in Cox regression. Biometrics 2001, 57, 114–119. [Google Scholar] [CrossRef]
- Dekkers, O.M.; Groenwold, R.H.H. When observational studies can give wrong answers: The potential of immortal time bias. Eur. J. Endocrinol. 2021, 184, E1–E4. [Google Scholar] [CrossRef]
- Grubbs, E.G.; Callender, G.G.; Xing, Y.; Perrier, N.D.; Evans, D.B.; Phan, A.T.; Lee, J.E. Recurrence of adrenal cortical carcinoma following resection: Surgery alone can achieve results equal to surgery plus mitotane. Ann. Surg. Oncol. 2010, 17, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Else, T.; Williams, A.R.; Sabolch, A.; Jolly, S.; Miller, B.S.; Hammer, G.D. Adjuvant therapies and patient and tumor characteristics associated with survival of adult patients with adrenocortical carcinoma. J. Clin. Endocrinol. Metab. 2014, 99, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Beuschlein, F.; Weigel, J.; Saeger, W.; Kroiss, M.; Wild, V.; Daffara, F.; Libé, R.; Ardito, A.; Al Ghuzlan, A.; Quinkler, M.; et al. Major prognostic role of Ki67 in localized adrenocortical carcinoma after complete resection. J. Clin. Endocrinol. Metab. 2015, 100, 841–849. [Google Scholar] [CrossRef]
- Postlewait, L.M.; Ethun, C.G.; Tran, T.B.; Prescott, J.D.; Pawlik, T.M.; Wang, T.S.; Glenn, J.; Hatzaras, I.; Shenoy, R.; Phay, J.E.; et al. Outcomes of Adjuvant Mitotane after Resection of Adrenocortical Carcinoma: A 13-Institution Study by the US Adrenocortical Carcinoma Group. J. Am. Coll. Surg. 2016, 222, 480–490. [Google Scholar] [CrossRef] [PubMed]
- Berruti, A.; Grisanti, S.; Pulzer, A.; Claps, M.; Daffara, F.; Loli, P.; Mannelli, M.; Boscaro, M.; Arvat, E.; Tiberio, G.; et al. Long-Term Outcomes of Adjuvant Mitotane Therapy in Patients With Radically Resected Adrenocortical Carcinoma. J. Clin. Endocrinol. Metab. 2017, 102, 1358–1365. [Google Scholar] [CrossRef] [PubMed]
- Fassnacht, M.; Terzolo, M.; Allolio, B.; Baudin, E.; Haak, H.; Berruti, A.; Welin, S.; Schade-Brittinger, C.; Lacroix, A.; Jarzab, B.; et al. Combination chemotherapy in advanced adrenocortical carcinoma. N. Engl. J. Med. 2012, 366, 2189–2197. [Google Scholar] [CrossRef]
- Fassnacht, M.; Berruti, A.; Baudin, E.; Demeure, M.J.; Gilbert, J.; Haak, H.; Kroiss, M.; Quinn, D.I.; Hesseltine, E.; Ronchi, C.L.; et al. Linsitinib (OSI-906) versus placebo for patients with locally advanced or metastatic adrenocortical carcinoma: A double-blind, randomised, phase 3 study. Lancet Oncol. 2015, 16, 426–435. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).