Abstract
Background/Objectives: The effect of glucagon-like peptide-1 receptor (GLP-1R) agonists on calcium homeostasis is poorly understood. This study aimed to investigate the association between GLP-1R agonist use and the risk of hypocalcemia and/or hypercalcemia, as well as other clinical outcomes. Methods: A retrospective cohort study used de-identified patient data from the TriNetX Global Collaborative Network, including 15,655 adult patients prescribed GLP-1R agonists and 15,655 propensity-matched controls. Outcomes included hypocalcemia, hypercalcemia, emergency visits, hospitalizations, cardiovascular events, and all-cause mortality. Results: GLP-1R agonist use was associated with a reduced risk of hypocalcemia (2.7% vs. 5.5%, RR 0.49, 95% CI: 0.44–0.55) but an increased risk of hypercalcemia (2.3% vs. 1.1%, RR 2.02, 95% CI: 1.69–2.42). The effect on hypocalcemia was most pronounced during the first six months of treatment. Among individual agents, tirzepatide showed the most pronounced effect, reducing hypocalcemia risk by 63% while increasing hypercalcemia risk by 85%. Semaglutide demonstrated similar effects, while dulaglutide and liraglutide showed modest effects. Furthermore, GLP-1R agonist use was associated with reduced risks of emergency visits (RR 0.57, 95% CI: 0.54–0.60), hospitalizations (RR 0.40, 95% CI: 0.36–0.44), cardiovascular events, and all-cause mortality (HR 0.27, 95% CI: 0.21–0.36). Conclusions: GLP-1R agonists exhibit a complex influence on calcium homeostasis, reducing hypocalcemia risk while increasing hypercalcemia risk. Beyond calcium regulation, these medications significantly reduce healthcare utilization, improve cardiovascular outcomes, and decrease mortality. Further research is needed to elucidate the mechanisms behind the differential effects of individual GLP-1R agonists, particularly tirzepatide, to optimize personalized treatment approaches and long-term safety.
1. Introduction
The incidence of type 2 diabetes and obesity has reached epidemic proportions, representing a significant public health challenge worldwide [1]. Among the evolving therapeutic options, glucagon-like peptide-1 receptor (GLP-1R) agonists have gained prominence due to their robust efficacy in improving glycemic control and conferring additional physiological benefits [2]. These drugs, including liraglutide, exenatide, and dulaglutide, mimic the effects of the incretin hormone GLP-1, resulting in multiple beneficial actions such as slowed gastric emptying, enhanced glucose-dependent insulin secretion, reduced appetite, decreased inappropriate glucagon secretion, and promotion of beta-cell proliferation [3].
Beyond their primary metabolic effects, GLP-1R agonists have been found to influence calcium handling and homeostasis in various tissues. Research has shown that these drugs modulate calcium dynamics in pancreatic β-cells [4], muscle cells, and cardiac myocytes [5]. Moreover, the impact of GLP-1R agonists on bone metabolism is an area of growing interest and concern [6]. Notably, some studies have reported improvements in bone mineral density and reductions in fracture risk among patients using GLP-1R agonists [7,8]. However, there remain significant concerns regarding their potential effects on bone turnover and mineralization, necessitating a thorough understanding of these implications [8,9]. These findings underscore the importance of evaluating the role of GLP-1R agonists in bone metabolism in tandem with their effects on calcium homeostasis for optimal patient care and treatment optimization [10].
Calcium homeostasis is critical for numerous physiological processes, including muscle contraction, neurotransmitter release, and intracellular signaling [11]. Maintaining proper calcium balance is essential for overall health, and disruptions in calcium homeostasis can profoundly affect cellular function and metabolism [12]. The multifaceted impact of GLP-1R agonists on calcium homeostasis in real-world settings involves several possible mechanisms. These drugs have been found to enhance insulin secretion, improve insulin sensitivity, and promote weight loss, all of which can indirectly affect calcium metabolism [13]. Additionally, improvements in cardiovascular outcomes associated with GLP-1R agonists may be mediated, in part, by their effects on calcium regulation [14]. However, the precise mechanisms by which GLP-1R agonists influence calcium homeostasis and the translation of these effects into clinical outcomes remain incompletely understood.
Glucagon-like peptide-1 is well recognized for its insulinotropic effects, and evidence suggests it plays a role in bone homeostasis, potentially acting as a mediator within the entero-osseous axis. This hypothesis posits that gut-derived hormones, like GLP-1, may have systemic regulatory roles in bone turnover and mineralization [15]. Despite these intriguing connections, there is a notable paucity of large-scale studies specifically examining the association between GLP-1R agonist use and the risk of hypocalcemia or hypercalcemia [16]. Addressing this gap is fundamental, particularly as maintaining a constant plasma calcium level is crucial for many health processes, including maintaining proper bone mineral density and ensuring effective cellular function [17].
Given the expanding clinical application of GLP-1R agonists for both diabetes management and weight control, clarifying their safety profile concerning electrolyte homeostasis is increasingly important. As patients receive these treatments over extended periods, understanding any potential risks associated with calcium homeostasis becomes essential for optimizing therapeutic outcomes and preventing adverse events.
This study aims to explore, for the first time, whether treatment with GLP-1R agonists is associated with an elevated risk of blood calcium dysregulation and to discern the differential impacts of individual GLP-1R agonists on this parameter. By conducting a retrospective cohort analysis using real-world data from the “TriNetX electronic health record network”, we hope to provide insightful findings that could lead to more personalized and effective treatment strategies for patients with type 2 diabetes and related conditions. Our research intends not only to deepen the understanding of GLP-1R agonists’ role in calcium homeostasis but also to pave the way for future studies investigating their broader implications in metabolic and bone health.
2. Materials and Methods
2.1. Study Design and Data Source
We conducted a retrospective cohort study using de-identified patient data from the “TriNetX Global Collaborative Network”, a federated health research platform that provides access to electronic health records from over 150 million patients across more than 125 healthcare organizations worldwide. The TriNetX platform allows for real-time access to harmonized clinical data while ensuring patient privacy through de-identification and aggregation of results. Data were accessed on 6 July 2024.
2.2. Study Population
The study cohort included adult patients (age ≥ 18 years) with a prescription for a GLP-1R agonist (including liraglutide, semaglutide, dulaglutide, or tirzepatide). The index date was defined as the date of the first GLP-1R agonist prescription. Patients were excluded if they had a history of bariatric surgery, thyroid disorders, or hypocalcemia in the three months prior to the index date. A comparison cohort of patients not prescribed GLP-1R agonists was identified using propensity score matching based on age, sex, race, body mass index, comorbidities (including diabetes, hypertension, and chronic kidney disease), and use of medications that may affect calcium homeostasis. Inclusion and exclusion criteria are listed in Table 1 and Table 2.

Table 1.
Inclusion criteria for the study participants.

Table 2.
Exclusion criteria for the study participants.
The study cohort included adult patients (age ≥ 18 years) with a prescription for a GLP-1R agonist (including liraglutide, semaglutide, dulaglutide, or tirzepatide). The index date was defined as the date of the first GLP-1R agonist prescription. Patients were included if they had a diagnosis of obesity (BMI ≥ 30 kg/m2 or ICD-10 code for obesity).
Patients were excluded if they had a history of neoplasms, chronic kidney disease, osteoporosis, inflammatory bowel syndrome, parathyroidectomy, thyroidectomy, blood transfusion, vitamin D deficiency, corticosteroid use, pancreatitis, magnesium deregulation, bariatric surgery, or use of medications known to affect calcium levels (e.g., bisphosphonates, denosumab, cinacalcet, cisplatin, diuretics, proton pump inhibitors, certain antibiotics) in the three months prior to the index date. Patients with prior use of discontinued GLP-1R agonists (lixisenatide, albiglutide, exenatide) were also excluded (detailed inclusion and exclusion criteria are listed in Table 1 and Table 2).
A comparison cohort of patients not prescribed GLP-1R agonists was identified using propensity score matching based on age, sex, race, body mass index, smoking, alcohol use, and comorbidities (including diabetes and hypertension).
2.3. Exposure and Outcome Definitions
The primary exposure was defined as having at least one prescription for a GLP-1R agonist. The primary outcome was incident hypocalcemia, defined as either a serum calcium level ≤ 8.4 mg/dL, ionized calcium ≤ 1.10 mmol/L (or ≤4.60 mg/dL), or an ICD-10 diagnosis code for hypocalcemia (E83.51) occurring after the index date.
Secondary outcomes included serum parathyroid hormone (PTH) and vitamin D levels, emergency department visits, hospitalizations, osteoporosis, tetany/spasms/myalgia, seizures, arrhythmias, heart failure, depression/hallucinations/confusion, and all-cause mortality. These outcomes were identified using laboratory values, procedure codes, and ICD-10 diagnosis codes, as detailed in Supplementary Table S1.
2.4. Follow-Up and Time Periods
Patients were followed from the index date until the occurrence of hypocalcemia, death, loss to follow-up, or end of the study period (31 December 2023), whichever came first. We analyzed outcomes over three distinct periods: 0–6 months, 6–12 months, and 12–24 months after the index date to assess both short-term and longer-term risks. Additionally, we conducted an “anytime” analysis for all outcomes, including mortality, to capture events occurring at any point during the entire follow-up period after the index date.
2.5. Statistical Analysis
Baseline characteristics were compared between the GLP-1R agonist and control groups using standardized mean differences. The cumulative incidence of hypocalcemia was estimated using Kaplan–Meier methods, and hazard ratios (HRs) with 95% confidence intervals (CIs) were calculated using Cox proportional hazard models. Models were adjusted for potential confounders not accounted for in the propensity score matching. Subgroup analyses were performed to assess the risk of hypocalcemia across different GLP-1R agonists and patient characteristics. All analyses used the TriNetX network’s analytics features, which utilize R statistical software (version 4.3.0). p-values < 0.05 were considered statistically significant.
2.6. Ethical Considerations
This study used de-identified patient data and was determined to be exempt from full review by our institutional review board. This study followed the Declaration of Helsinki and good clinical practice guidelines.
3. Results
3.1. Characteristics of the Study Population
Our study analyzed data from 128,886,898 adult patients (≥18 years old) across 125 healthcare organizations. After applying inclusion and exclusion criteria, we identified 15,655 patients in the treated group (GLP-1R agonist users) and 217,365 patients in the control group. Table 3 presents the demographic and clinical characteristics of the study population before and after propensity score matching.

Table 3.
Characteristics of the study population.
Before matching, the treated group was slightly older than the control group (43.2 ± 13.0 vs. 42.6 ± 15.2 years, p < 0.001). Both groups had a higher proportion of females, with a slightly lower percentage in the treated group (55.2% vs. 56.5%, p = 0.002). White patients were more prevalent in the treated group (61.4% vs. 57.5%, p < 0.001) than controls. Regarding comorbidities, the treated group had significantly higher rates of diabetes (14.3% vs. 4.5%, p < 0.001) and hypertension (9.4% vs. 7.5%, p < 0.001), but lower rates of nicotine dependence (0.9% vs. 1.6%, p < 0.001) and alcohol use disorder (0.2% vs. 0.3%, p = 0.004). After propensity score matching, the characteristics between the treated and control groups were well balanced, ensuring that any differences observed in outcomes between the treated and control groups are more likely attributable to the effect of GLP-1R agonist treatment rather than underlying differences in patient characteristics.
3.2. Overall GLP-1R Agonist Use
Our analysis of all GLP-1R agonists combined revealed significant differences in outcomes between matched treated and control groups (Table 4). GLP-1R agonist use was associated with a reduced risk of hypocalcemia (2.7% vs. 5.5%, p < 0.001; RR 0.49, 95% CI: 0.44–0.55) and improved clinical outcomes, particularly in cardiovascular health. The incidence of congestive heart disease was lower in the treated group (1.1% vs. 2.8%, p < 0.001; RR 0.41, 95% CI: 0.34–0.49), as was the incidence of arrhythmia (1.6% vs. 2.8%, p < 0.001; RR 0.56, 95% CI: 0.48–0.66).

Table 4.
Comparison of outcomes between GLP-1R agonist users and controls.
Healthcare utilization was also favorably impacted, with GLP-1 agonist use associated with fewer emergency visits (12.7% vs. 21.9%, p < 0.001; RR 0.57, 95% CI: 0.54–0.60) and hospitalization visits (3.1% vs. 7.7%, p < 0.001; RR 0.40, 95% CI: 0.36–0.44). Notably, all-cause mortality was significantly lower in the GLP-1 agonist group (0.4% vs. 1.5%, p < 0.001; HR 0.27, 95% CI: 0.21–0.36).
However, the GLP-1 agonist group exhibited an increased risk of hypercalcemia (2.3% vs. 1.1%, RR 2.02, 95% CI: 1.69–2.42, p < 0.001) and a slight elevation in neuropsychiatric symptoms, with depression/hallucination/confusion being more common in the treated group (13.5% vs. 11.4%, p < 0.001; RR 1.18, 95% CI: 1.11–1.25).
3.3. Individual GLP-1R Agonist Analyses
Separate propensity score matching was conducted for each GLP-1 receptor agonist, resulting in balanced treated and control groups: semaglutide (n = 7349 pairs), liraglutide (n = 1513 pairs), dulaglutide (n = 2695 pairs), and tirzepatide (n = 1379 pairs). This matching process, based on demographics and comorbidities, enabled a more precise evaluation of each drug’s unique effects. Subgroup analyses of these matched pairs showed varying degrees of impact on calcium levels (Table 5).

Table 5.
Comparison of hypocalcemia and hypercalcemia risks among individual GLP-1R agonists.
Tirzepatide demonstrated the most pronounced effect, reducing hypocalcemia risk by 63% (RR 0.37, 95% CI: 0.236–0.563) while increasing hypercalcemia risk by 85% (RR 1.85, 95% CI: 1.079–3.171). Semaglutide showed similar trends, with a 62% reduction in hypocalcemia (RR 0.38, 95% CI: 0.318–0.459) and a 51% increase in hypercalcemia (RR 1.51, 95% CI: 1.178–1.935). Dulaglutide and liraglutide exhibited modest effects. Dulaglutide reduced hypocalcemia risk by 34% (RR 0.66, 95% CI: 0.53–0.84, p = 0.001) and increased hypercalcemia risk by 76% (RR 1.76, 95% CI: 1.24–2.51, p = 0.001). Liraglutide showed a 40% reduction in hypocalcemia risk (RR 0.60, 95% CI: 0.43–0.82, p = 0.001), but the increase in hypercalcemia risk was not statistically significant (RR 1.47, 95% CI: 0.79–2.71, p = 0.21).
The time-dependent analysis demonstrated that the impact on hypocalcemia was most pronounced in the first six months of treatment for all drugs, with diminishing effects observed at 12 and 24 months (Figure 1A and Table S2). In contrast, the risk of hypercalcemia tended to persist or increase over time, particularly for semaglutide and dulaglutide (Figure 1B and Table S2).
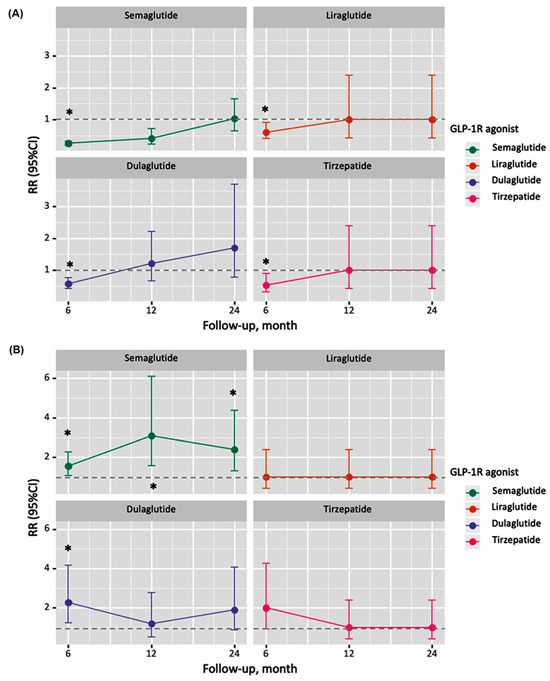
Figure 1.
Time-dependent analysis of hypocalcemia and hypercalcemia risks associated with GLP-1R agonist use. (A) Risk ratios for hypocalcemia at 0–6 months, 7–12 months, and 13–24 months after treatment initiation for each GLP-1R agonist. (B) Risk ratios for hypercalcemia at 0–6 months, 7–12 months, and 13–24 months after treatment initiation for each GLP-1R agonist. Error bars represent 95% confidence intervals. The dotted line (i.e., the control) indicates a risk ratio of 1 (no effect). Values below 1 indicate reduced risk, while above 1 indicate increased risk. Semaglutide (blue), liraglutide (red), dulaglutide (green), and tirzepatide (purple) are represented for each time interval. Asterisks (*) denote statistically significant differences (p < 0.05) compared to the control group.
A detailed time-series analysis of various outcomes for individual GLP-1R agonists compared to their propensity-matched controls is provided in Table 6. All drugs significantly reduced emergency visits and hospitalizations in the first six months, with semaglutide and tirzepatide maintaining this effect over time. For cardiovascular outcomes, such as congestive heart failure and arrhythmia, protective effects were shown for all drugs in the first six months, with semaglutide maintaining this effect at 24 months. Apart from tirzepatide, there is an increased risk of depression, hallucination, or confusion, especially at 12 and 24 months for most drugs.

Table 6.
Time-series analysis for outcomes for individual drugs of propensity-matched treated cohort and controls.
4. Discussion
This large-scale retrospective cohort study provides compelling evidence for the complex effects of GLP-1R agonists on calcium homeostasis and clinical outcomes in a real-world setting. Our findings reveal a paradoxical impact on calcium levels, with these drugs significantly reducing the risk of hypocalcemia and increasing the risk of hypercalcemia. This “calcium conundrum” presents a fascinating aspect of GLP-1R agonist therapy that warrants further investigation.
The observed 51% reduction in hypocalcemia risk across all GLP-1R agonists is a novel finding with important clinical implications. This protective effect was consistent across individual agents, with tirzepatide showing the most pronounced reduction (63%). The mechanism underlying this protection against hypocalcemia is not fully understood but may be related to the known effects of GLP-1R agonists on bone metabolism and calcium homeostasis. GLP-1R agonists promote bone formation while inhibiting bone resorption [6]. However, the concurrent doubling of hypercalcemia risk (102% increase) highlights the complex interplay between these agents and calcium regulation. With an increased hypercalcemia risk, individuals are more prone to experiencing complications such as nephrolithiasis, distal renal tubular acidosis, cholelithiasis, and some mood disorders [18].
The basis for direct skeletal effects, and therefore indirect influence of calcium homeostasis, by GLP-1R agonists remains unclear. Pre-clinical studies have demonstrated that GLP-1 plays a role in regulating skeletal homeostasis, suggesting that GLP-1 may promote bone formation [7,19], though clinical studies have not supported these effects [20,21,22]. The role and related mechanisms of GLP-1R agonists in bone metabolism as they relate to calcium homeostasis need to be further elucidated and clarified [23,24].
Interestingly, our time-dependent analysis revealed that the effects on hypocalcemia were most pronounced in the first six months of treatment, with diminishing effects observed at 12 and 24 months. In contrast, the risk of hypercalcemia tended to persist or increase over time. This temporal pattern suggests a dynamic influence of GLP-1 receptor agonists on calcium metabolism that evolves throughout treatment. It raises crucial questions about the underlying mechanisms and emphasizes the need for careful monitoring of calcium levels in patients on these medications, especially in the early months of treatment and with newer agents like tirzepatide.
The differential effects observed among individual GLP-1R agonists are noteworthy. Tirzepatide and semaglutide demonstrated the most pronounced effects on hypocalcemia and hypercalcemia, while dulaglutide and liraglutide showed modest impacts. These differences may be attributed to the unique pharmacological properties of each agent, particularly tirzepatide’s dual action on gastric inhibitory polypeptide (GIP) and GLP-1 receptors [25]. GIP receptors have been found in osteoblasts and osteoclasts; they have been shown to protect osteoblasts from apoptosis and inhibit bone resorption [26]. Further research is needed to elucidate the specific mechanisms underlying the differential effects of individual GLP-1R agonists and their clinical significance [27].
The time-dependent analysis demonstrated that the impact on hypocalcemia was most pronounced in the first six months of treatment for all drugs, with diminishing effects observed at 12 and 24 months (Figure 1A). In contrast, the risk of hypercalcemia tended to persist or increase over time, particularly for semaglutide and dulaglutide (Figure 1B). Beyond calcium homeostasis, our study corroborates and extends previous findings on the cardiovascular benefits of GLP-1R agonists. We observed significant reductions in emergency visits, hospitalizations, cardiovascular events, and all-cause mortality. The 73% reduction in all-cause mortality is particularly striking and suggests that the benefits of these drugs may be even more pronounced in real-world settings than in controlled clinical trials. Further supporting the cardioprotective role of the GLP-1R agonists, evidence from other studies suggests that the agonists assist in promoting myocardial glucose uptake while reducing oxidative stress and decreasing apoptosis [28]. Additionally, the literature explains the role of GLP-1R agonists in increasing coronary blood flow through inducing vasodilation [29]. These vasodilatory effects also reduce systemic vascular resistance, thus lowering blood pressure [30]. Furthermore, the indirect effect of GLP-1R agonists in reducing cardiovascular morbidity via decreasing blood glucose levels, postprandial lipemia, inflammation, blood pressure, and body weight was reported by Ussher and Drucker in their interesting review [31].
The slight increase in reports of depression, hallucinations, or confusion in the GLP-1R agonist group is an unexpected finding that requires further investigation [32]. It is unclear whether this represents an adverse effect or is related to other factors, such as increased healthcare utilization or improved survival in this group [33].
Our study has several strengths, including its large sample size, real-world setting, and comprehensive assessment of multiple outcomes. However, it also has limitations inherent to retrospective studies using electronic health records. These include potential confounding by indication, lack of randomization, and possible incomplete capture of all relevant clinical information. Additionally, the relatively short follow-up period for newer agents like tirzepatide limits our ability to draw conclusions about their long-term effects.
5. Conclusions
This study provides robust evidence for the complex effects of GLP-1R agonists on calcium homeostasis and clinical outcomes in real-world patients. We found that these agents reduce hypocalcemia risk but increase hypercalcemia risk, with effects varying among individual drugs and over time. Significant improvements in cardiovascular outcomes and reduced all-cause mortality were also observed. These findings have important clinical implications, suggesting the need for close monitoring of calcium levels, especially during the first six months of treatment, and consideration of individual agent characteristics when selecting therapy. This study highlights the importance of using GLP-1R agonists not only for their effects on glycemic control and weight loss but also for their impact on calcium balance and cardiovascular health. Future research should focus on prospective studies to confirm these findings, explore underlying mechanisms, and assess long-term safety and efficacy, particularly for newer agents like tirzepatide. While GLP-1R agonists offer significant benefits in diabetes and obesity management, their complex effects on calcium homeostasis necessitate careful patient monitoring and individualized treatment approaches.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/jcm13164896/s1, Table S1: Outcome measures; Table S2: Overall serum levels and time points of the studied parameters in the study groups.
Author Contributions
Conceptualization, N.E., M.H.H. and E.A.T.; data curation, N.E., R.U., H.P., S.C., A.A., M.H.H. and M.S.F.; formal analysis, M.H.H. and E.A.T.; investigation, A.A.; methodology, R.U. and E.A.T.; resources, B.T.A., N.E., R.U., S.A.Z., M.S.F. and H.A.; software, M.H.H. and E.A.T.; validation, B.T.A., N.E., H.P., S.C., A.A., S.A.Z., M.S.F. and H.A.; writing—original draft, H.P., S.C. and E.A.T.; writing—review and editing, B.T.A., N.E., R.U., A.A., M.H.H., S.A.Z., M.S.F. and H.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the retrospective type of the study analysis on the database.
Informed Consent Statement
Patient consent was waived due to the retrospective type of the study analysis on the database.
Data Availability Statement
Restrictions apply to the availability of these data. Data were obtained from the TriNetX database and are available at https://trinetx.com/ with the permission of the TriNetX database authority.
Acknowledgments
We appreciate the TriNetX database and platform allowing us to access patients’ electronic health record data.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Chandrasekaran, P.; Weiskirchen, R. The Role of Obesity in Type 2 Diabetes Mellitus-An Overview. Int. J. Mol. Sci. 2024, 25, 1882. [Google Scholar] [CrossRef]
- Mariam, Z.; Niazi, S.K. Glucagon-like peptide agonists: A prospective review. Endocrinol. Diabetes Metab. 2024, 7, e462. [Google Scholar] [CrossRef] [PubMed]
- Son, J.W.; Lim, S. Glucagon-Like Peptide-1 Based Therapies: A New Horizon in Obesity Management. Endocrinol. Metab. 2024, 39, 206–221. [Google Scholar] [CrossRef]
- Paradiz Leitgeb, E.; Kercmar, J.; Krizancic Bombek, L.; Pohorec, V.; Skelin Klemen, M.; Slak Rupnik, M.; Gosak, M.; Dolensek, J.; Stozer, A. Exendin-4 affects calcium signalling predominantly during activation and activity of beta cell networks in acute mouse pancreas tissue slices. Front. Endocrinol. 2023, 14, 1315520. [Google Scholar] [CrossRef]
- Huang, J.H.; Chen, Y.C.; Lee, T.I.; Kao, Y.H.; Chazo, T.F.; Chen, S.A.; Chen, Y.J. Glucagon-like peptide-1 regulates calcium homeostasis and electrophysiological activities of HL-1 cardiomyocytes. Peptides 2016, 78, 91–98. [Google Scholar] [CrossRef]
- Zhao, C.; Liang, J.; Yang, Y.; Yu, M.; Qu, X. The Impact of Glucagon-Like Peptide-1 on Bone Metabolism and Its Possible Mechanisms. Front. Endocrinol. 2017, 8, 98. [Google Scholar] [CrossRef]
- Ma, X.; Meng, J.; Jia, M.; Bi, L.; Zhou, Y.; Wang, Y.; Hu, J.; He, G.; Luo, X. Exendin-4, a glucagon-like peptide-1 receptor agonist, prevents osteopenia by promoting bone formation and suppressing bone resorption in aged ovariectomized rats. J. Bone Miner. Res. 2013, 28, 1641–1652. [Google Scholar] [CrossRef]
- Sun, H.X.; Lu, N.; Luo, X.; Zhao, L.; Liu, J.M. Liraglutide, the glucagon-like peptide-1 receptor agonist, has anabolic bone effects in diabetic Goto-Kakizaki rats. J. Diabetes 2015, 7, 584–588. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Lee, S.K.; Jo, K.J.; Song, D.Y.; Lim, D.M.; Park, K.Y.; Bonewald, L.F.; Kim, B.J. Exendin-4 increases bone mineral density in type 2 diabetic OLETF rats potentially through the down-regulation of SOST/sclerostin in osteocytes. Life Sci. 2013, 92, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Daniilopoulou, I.; Vlachou, E.; Lambrou, G.I.; Ntikoudi, A.; Dokoutsidou, E.; Fasoi, G.; Govina, O.; Kavga, A.; Tsartsalis, A.N. The Impact of GLP1 Agonists on Bone Metabolism: A Systematic Review. Medicina 2022, 58, 224. [Google Scholar] [CrossRef]
- Lin, G.; Rennie, M.; Adeeko, A.; Scarlata, S. The role of calcium in neuronal membrane tension and synaptic plasticity. Biochem. Soc. Trans. 2024, 52, 937–945. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.; Pizzo, P.; Filadi, R. Calcium, mitochondria and cell metabolism: A functional triangle in bioenergetics. Biochim. Et Biophys. Acta. Mol. Cell Res. 2019, 1866, 1068–1078. [Google Scholar] [CrossRef]
- Ghodsi, M.; Larijani, B.; Keshtkar, A.A.; Nasli-Esfahani, E.; Alatab, S.; Mohajeri-Tehrani, M.R. Mechanisms involved in altered bone metabolism in diabetes: A narrative review. J. Diabetes Metab. Disord. 2016, 15, 52. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.S.; Lin, F.J.; Chen, Y.C.; Lin, Y.K.; Higa, S.; Chen, S.A.; Chen, Y.J. Glucagon-like Peptide-1 Receptor Activation Reduces Pulmonary Vein Arrhythmogenesis and Regulates Calcium Homeostasis. Int. J. Mol. Sci. 2023, 24, 13100. [Google Scholar] [CrossRef] [PubMed]
- Helsted, M.M.; Gasbjerg, L.S.; Lanng, A.R.; Bergmann, N.C.; Stensen, S.; Hartmann, B.; Christensen, M.B.; Holst, J.J.; Vilsboll, T.; Rosenkilde, M.M.; et al. The role of endogenous GIP and GLP-1 in postprandial bone homeostasis. Bone 2020, 140, 115553. [Google Scholar] [CrossRef] [PubMed]
- Trujillo, J.M.; Nuffer, W.; Smith, B.A. GLP-1 receptor agonists: An updated review of head-to-head clinical studies. Ther. Adv. Endocrinol. Metab. 2021, 12, 2042018821997320. [Google Scholar] [CrossRef]
- Hamroun, A.; Pekar, J.-D.; Lionet, A.; Ghulam, A.; Maboudou, P.; Mercier, A.; Brousseau, T.; Grzych, G.; Glowacki, F. Ionized calcium: Analytical challenges and clinical relevance. J. Lab. Precis. Med. 2020, 5. [Google Scholar] [CrossRef]
- Sukhija, T.; Midha, V.; Mittal, N.; Kalra, E.; Chouhan, K.; Singh, D.; Dishant, F.; Attri, P.; Goyal, M.K.; Arora, S. Clinical Profile and Outcomes of Patients With Hypercalcemia in an Indian Tertiary Care Center. Cureus 2023, 15, e46062. [Google Scholar] [CrossRef]
- Nuche-Berenguer, B.; Lozano, D.; Gutierrez-Rojas, I.; Moreno, P.; Marinoso, M.L.; Esbrit, P.; Villanueva-Penacarrillo, M.L. GLP-1 and exendin-4 can reverse hyperlipidic-related osteopenia. J. Endocrinol. 2011, 209, 203–210. [Google Scholar] [CrossRef]
- Li, R.; Xu, W.; Luo, S.; Xu, H.; Tong, G.; Zeng, L.; Zhu, D.; Weng, J. Effect of exenatide, insulin and pioglitazone on bone metabolism in patients with newly diagnosed type 2 diabetes. Acta Diabetol. 2015, 52, 1083–1091. [Google Scholar] [CrossRef]
- Gilbert, M.P.; Marre, M.; Holst, J.J.; Garber, A.; Baeres, F.M.; Thomsen, H.; Pratley, R.E. Comparison of the Long-Term Effects of Liraglutide and Glimepiride Monotherapy on Bone Mineral Density in Patients with Type 2 Diabetes. Endocr. Pract. 2016, 22, 406–411. [Google Scholar] [CrossRef] [PubMed]
- Hansen, M.S.S.; Tencerova, M.; Frolich, J.; Kassem, M.; Frost, M. Effects of gastric inhibitory polypeptide, glucagon-like peptide-1 and glucagon-like peptide-1 receptor agonists on Bone Cell Metabolism. Basic Clin. Pharmacol. Toxicol. 2018, 122, 25–37. [Google Scholar] [CrossRef]
- Mabilleau, G.; Pereira, M.; Chenu, C. Novel skeletal effects of glucagon-like peptide-1 (GLP-1) receptor agonists. J. Endocrinol. 2018, 236, R29–R42. [Google Scholar] [CrossRef]
- Xie, B.; Chen, S.; Xu, Y.; Han, W.; Hu, R.; Chen, M.; Zhang, Y.; Ding, S. The Impact of Glucagon-Like Peptide 1 Receptor Agonists on Bone Metabolism and Its Possible Mechanisms in Osteoporosis Treatment. Front. Pharmacol. 2021, 12, 697442. [Google Scholar] [CrossRef] [PubMed]
- Wang, L. Designing a Dual GLP-1R/GIPR Agonist from Tirzepatide: Comparing Residues Between Tirzepatide, GLP-1, and GIP. Drug Des. Dev. Ther. 2022, 16, 1547–1559. [Google Scholar] [CrossRef]
- Hansen, M.S.; Soe, K.; Christensen, L.L.; Fernandez-Guerra, P.; Hansen, N.W.; Wyatt, R.A.; Martin, C.; Hardy, R.S.; Andersen, T.L.; Olesen, J.B.; et al. GIP reduces osteoclast activity and improves osteoblast survival in primary human bone cells. Eur. J. Endocrinol. 2023, 188, 144–157. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, C.R.; Andersen, A.; Knop, F.K.; Vilsboll, T. How glucagon-like peptide 1 receptor agonists work. Endocr. Connect. 2021, 10, R200–R212. [Google Scholar] [CrossRef] [PubMed]
- Ban, K.; Noyan-Ashraf, M.H.; Hoefer, J.; Bolz, S.S.; Drucker, D.J.; Husain, M. Cardioprotective and vasodilatory actions of glucagon-like peptide 1 receptor are mediated through both glucagon-like peptide 1 receptor-dependent and -independent pathways. Circulation 2008, 117, 2340–2350. [Google Scholar] [CrossRef] [PubMed]
- Puglisi, S.; Rossini, A.; Poli, R.; Dughera, F.; Pia, A.; Terzolo, M.; Reimondo, G. Effects of SGLT2 Inhibitors and GLP-1 Receptor Agonists on Renin-Angiotensin-Aldosterone System. Front. Endocrinol. 2021, 12, 738848. [Google Scholar] [CrossRef] [PubMed]
- Ferhatbegovic, L.; Mrsic, D.; Macic-Dzankovic, A. The benefits of GLP1 receptors in cardiovascular diseases. Front. Clin. Diabetes Healthc. 2023, 4, 1293926. [Google Scholar] [CrossRef]
- Ussher, J.R.; Drucker, D.J. Glucagon-like peptide 1 receptor agonists: Cardiovascular benefits and mechanisms of action. Nat. Rev. Cardiol. 2023, 20, 463–474. [Google Scholar] [CrossRef] [PubMed]
- Arillotta, D.; Floresta, G.; Guirguis, A.; Corkery, J.M.; Catalani, V.; Martinotti, G.; Sensi, S.L.; Schifano, F. GLP-1 Receptor Agonists and Related Mental Health Issues; Insights from a Range of Social Media Platforms Using a Mixed-Methods Approach. Brain Sci. 2023, 13, 1503. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Cai, P.; Zou, W.; Fu, Z. Psychiatric adverse events associated with GLP-1 receptor agonists: A real-world pharmacovigilance study based on the FDA Adverse Event Reporting System database. Front. Endocrinol. 2024, 15, 1330936. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).