Abstract
Wearable activity trackers (wearables) embed numerous behaviour change techniques (BCTs) that have previously been shown to increase adult physical activity (PA). With few children and adolescents achieving PA guidelines, it is crucial to explore ways to increase their PA. This systematic review examined the acceptability, feasibility, and effectiveness of wearables and their potential mechanisms of action for increasing PA in 5 to 19-year-olds. A systematic search of six databases was conducted, including data from the start date of each database to December 2019 (PROSPERO registration: CRD42020164506). Thirty-three studies were included. Most studies (70%) included only adolescents (10 to 19 years). There was some—but largely mixed—evidence that wearables increase steps and moderate-to-vigorous-intensity PA and reduce sedentary behaviour. There were no apparent differences in effectiveness based on the number of BCTs used and between studies using a wearable alone or as part of a multi-component intervention. Qualitative findings suggested wearables increased motivation to be physically active via self-monitoring, goal setting, feedback, and competition. However, children and adolescents reported technical difficulties and a novelty effect when using wearables, which may impact wearables’ long-term use. More rigorous and long-term studies investigating the acceptability, feasibility, and effectiveness of wearables in 5 to 19-year-olds are warranted.
1. Introduction
Physical activity (PA) provides physical, psychological, social, and cognitive health benefits throughout a person’s lifespan [1,2,3]. Physical activity during childhood and adolescence is associated with current and future health outcomes such as reduced adiposity [4,5] and enhanced motor skill development [6]. There is evidence that increasing PA can reduce depressive symptoms [7], and higher levels of PA are related to a greater quality of life [8] in children and adolescents. Despite these benefits, physical inactivity is common amongst children and adolescents. An estimated 28% and 57% of adolescent girls and boys (12 to 17-years) in European countries meet the guidelines of 60 minutes of moderate-to-vigorous-intensity PA (MVPA) every day [9].
To date, PA interventions in ≤16 year-olds have produced negligible-to-small increases in total PA and MVPA [10]. Previous evidence suggests that PA interventions that embed numerous behavioural change techniques (BCTs) may be more effective than those that do not [11]. Behavioural change techniques are “observable, replicable, and irreducible component(s) of an intervention designed to alter or redirect causal processes that regulate behaviour” ([12] p. 82). A previous systematic review [11] reported that effective school-based PA interventions aimed at 15 to 19-year-olds had an average of 10.5 (range: 5–20) BCTs compared to ineffective interventions that had an average of 4 (range: 3–6) [11]. Behavioural change techniques unique to effective interventions included self-monitoring, feedback, goal setting, action planning, and social support [11].
Previous research has reported that wearable activity trackers (wearables) and their partnering applications (apps) embed an average of 19 (range: 15–24) BCTs, including self-monitoring, feedback, action planning, goal setting, prompts/cues, and social comparison [13]. Given the number and type of BCTs that wearables embed, wearables may offer an effective way of increasing child and adolescent PA. There is some evidence that wearables are a potentially effective way of increasing PA in adults [14,15,16,17,18,19,20,21]. A meta-analysis found that wearables can significantly increase an adult’s step count, MVPA, and energy expenditure [20]. It was found that multi-component interventions were more effective than those using a wearable alone, and authors have suggested that this may be due to wearables being combined with additional BCTs [20].
However, less is known about the effectiveness of wearables for increasing child and adolescent PA [22]. In 2016, a systematic review [22] identified three intervention studies [23,24,25] investigating the effectiveness of wearables in 5 to 19-year-olds. There was little evidence to suggest that wearables can increase PA in children and adolescents, with Ridgers et al. [22] concluding that further research using rigorous methods was needed. This review aims to update that presented by Ridgers et al. [22], exploring the most recent literature. Given the evidence that PA interventions are most effective the more BCTs they embed [11], this review will identify BCTs in wearable interventions and may provide insights into the potential mechanisms of action behind the level of effectiveness of interventions, which were not explored in the review by Ridgers et al. [22].
The acceptability and feasibility of wearables are also important to consider in order to allow researchers to understand the potential reasons for the level of effectiveness of interventions and how best to implement such interventions [26,27]. For example, similar devices, such as pedometers, have been found to increase PA in 5 to 18-year-olds [28]. However, pedometers require users to manually record their PA (e.g., steps) each day [29,30], which may reduce intervention compliance rates and limit effectiveness [31], whereas wearables provide incremental feedback via a monitoring screen, app, and/or online dashboard, enabling users to easily monitor their long-term PA. This suggests that wearables may be more acceptable and feasible than other similar devices (e.g., pedometers). The review by Ridgers et al. [22] identified two studies [32,33] exploring the feasibility of wearables in 5 to 19-year-olds. There was some evidence that wearables were viewed positively by children and adolescents and that wearables can encourage children and adolescents to be more physically active [22]. However, several barriers to wearable use were identified (e.g., access to technology, lack of comfort) [22]. Although these findings offer some insight into wearables’ acceptability and feasibility, they are based on a small number of studies, and common themes were not identified. This systematic review presents a thematic synthesis to identify key themes related to the acceptability and feasibility of using wearables in children and adolescents. This highlights the most common facilitators and barriers of using wearables and will allow researchers to focus on these factors when developing future wearable-based interventions.
In this review, acceptability refers to constructs outlined by the “Theoretical Framework of Acceptability” [34], including how children and adolescents feel about using a wearable (affective attitude), the amount of perceived effort required to use a wearable (burden), the perceived understanding of how to use a wearable and interpret PA outputs (intervention coherence), and the perceived impact wearables have on children and adolescents’ PA levels (perceived effectiveness). Feasibility refers to the considerations outlined by Abbott [35], such as the facilitators and barriers of using wearables.
This systematic review explores the acceptability, feasibility, effectiveness, and potential mechanisms of action underlying the effectiveness of wearables for increasing PA in children and adolescents (5 to 19 years).
Research Questions
This systematic review addresses the following research questions:
- How acceptable are wearables for increasing PA in 5 to 19-year-olds?
- How feasible are wearables for increasing PA in 5 to 19-year-olds?
- How effective are wearables for increasing PA in 5 to 19-year-olds?
- What are the mechanisms of action (BCTs) underlying the influence of wearables on PA in 5 to 19-year-olds?
2. Methods
This review is registered with the International Prospective Register for Systematic Reviews (PROSPERO; CRD42020164506) and follows the guidance of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; [36]).
2.1. Search Strategy
A search strategy was developed based on previous reviews [22,37] to identify potentially relevant studies from six databases: PubMed, Web of Science, Scopus, SPORTDiscus, PsycINFO, and ProQuest. Searches took place from the start date of each database to December 2019. Search strategies included the following search strings in four main areas: population (child*, adolescen*, youth, teen*, young person, young people, school child*, family, families, parent*, caregiver, mother, father, home-based, parent–child, parent–adolescent), intervention (intervention, trial, feasibility, pilot, acceptability, program), wearable activity tracker (electronic track*, electronic activ*, electronic activ* monitor*, electronic active* track*, electronic fitness track*, wearable device, wearable act* track*, consumer wearable, wearable, wearable tech*, fitness track*) and outcome (physical act*, energy expenditure, MVPA, steps). The full search strings for each database are presented in Supplementary Materials Table S1. Additional relevant studies were retrieved from the included studies’ bibliographies, which is a method used to identify additional studies in systematic reviews [38].
2.2. Inclusion Criteria
Inclusion criteria were developed using the “Population, Intervention, Comparison, Outcomes and Study” approach (PICOS; [36]). The following eligibility criteria were used: (a) published in English; (b) included participants aged 5 to 19-years; (c) examined the use of a wearable within an intervention, acceptability, or feasibility study; (d) measured PA (effectiveness) and/or experiences of using a wearable (acceptability/feasibility); and (e) were a full-text paper, using primary data, published in a peer-reviewed academic journal. All populations (e.g., clinical, overweight/obese), study designs, and settings were included. For acceptability/feasibility studies, experiences of using a wearable could be reported by children and adolescents (5 to 19-year-olds) or others (e.g., adults, such as parents) on behalf of the study population.
For the purpose of this review, wearables were defined as a commercially available wearable device, with the capability of tracking PA (e.g., accelerometry, steps) and at least one other feature (e.g., distance travelled, gamification/rewards) or multiple dimensions of PA (e.g., steps and PA intensities). The wearable needed to provide momentary tracking to gather incremental feedback via a monitoring display, online dashboard, or partnering application, beyond a traditional step-only display [22,39]. Wearables could be used in conjunction with a partnering application/online dashboard or alone, given that smartphone ownership is minimal in younger children [40].
2.3. Exclusion Criteria
Studies were excluded if (a) participants were <5 years and >19 years of age and (b) the wearable was not utilised as an intervention/feasibility tool (e.g., measurement tool).
2.4. Study Selection and Data Extraction
Study eligibility was independently assessed through title, abstract, and full text-screening by two reviewers (A.V.C. and D.D.B.) using a standardised, unblinded approach. Studies were screened independently, and any disagreements were resolved at the end of each stage by A.V.C. and D.D.B., with any persistent disagreements resolved by a third reviewer (S.C.). If insufficient information was provided, the author(s) of the identified studies were contacted by email to provide relevant information for eligibility assessment.
The first reviewer (A.V.C.) used a standardised form to extract data using an adapted version of the Cochrane data collection form for intervention reviews: RCTs and non-RCTs [41]. The following data were extracted: country of study, sample demographics (e.g., age, sex, ethnicity, weight status, socioeconomic status), study characteristics (e.g., design, description, no. of study arms, length, follow-up period(s), setting), measurement characteristics (e.g., measurement tool, reported outcome), device characteristics (e.g., device brand and model), and study results.
2.5. Behaviour Change Techniques (BCTs)
Two reviewers (A.V.C. and J.H.), used the Behaviour Change Technique Taxonomy v1 (BCTTv1), a 93-item coding framework [12], to independently code BCTs present in included studies that measured PA as an outcome of using a wearable (effectiveness studies). Behaviour change techniques present in the wearable, partnering app/online dashboard, and additional study/intervention components were coded. Control and comparator groups of effectiveness studies were also coded for BCTs. Each BCT was coded as present beyond all reasonable doubt (++), present in all probability (+), or absent (−), as recommended by Michie et al. ([12,42], https://www.bct-taxonomy.com/; accessed on 1 June 2020). Techniques were coded as present beyond all reasonable doubt (++) if the study authors provided detailed evidence that the BCT was applied to the target behaviour and population and explained how the BCT was used to promote PA. Techniques were coded as present in all probability (+) if there was mention of the BCT being used without detailed explanation of how the BCT was used, there was some evidence that the BCT was utilised without explicit mention of the BCT by the study authors, or if the wearable(s) had a BCT present, as stated in the study or by manufacturers, using official websites and device manuals, but it was unclear from the study whether they were utilised. The frequency and duration of BCT use/delivery was not coded.
2.6. Risk of Bias
The included studies that measured PA as an outcome of using a wearable (effectiveness studies) were assessed for Risk of Bias (RoB) by two reviewers (A.V.C. and D.D.B.) independently. The risk of bias criteria were utilised in a previous systematic review [22], which was adapted from the Methods Guide for Comparative Effectiveness Reviews [43]. The following eight criteria were used: (1) participants were randomly allocated, (2) minimal missing data, (3) data were analysed according to group allocation, (4) the study population was representative of the population of interest, (5) the timing of outcome assessments was similar in all groups, (6) the study reported the validity of the wearable, (7) the study reported the reliability of the wearable, and (8) the study was conducted independently of the wearable manufacturer. Each criterion was scored as yes (1) or no (0). If unclear, the criterion was scored as no (0). Table S2 provides further descriptions of each criterion. An overall score out of 8 was provided, and effectiveness studies were categorized as having a high (score 0–2), medium (score 3–5), and low (score 6–8) risk of bias (adapted from Lewis et al. [18]).
2.7. Data Synthesis
To synthesise the data, studies were split into “effectiveness studies” and “feasibility/acceptability studies”. Effectiveness studies were those that provided an outcome measure of PA. The term “effectiveness studies” was chosen as some studies that measured PA did not claim to be an intervention. Studies that reported the experiences of children/adolescents using the wearable, but did not measure PA, were considered feasibility/acceptability studies. A narrative review was conducted for effectiveness studies, given that the heterogeneity of study designs and outcomes did not permit a meta-analysis. A thematic synthesis was conducted for feasibility/acceptability studies in which the authors provided quotations from participants and/or the authors’ interpretations of participant experiences using a wearable (as used previously by Fletcher et al. [44]). The thematic synthesis followed the three stages outlined by Thomas and Harden, which are presented in Table 1 [45].

Table 1.
Stages of thematic synthesis [45].
Line-by-line coding was carried out by one reviewer (A.V.C.) using the NVivo software (QSR International, Melbourne, Australia), and the meaning and content of each code was agreed upon by a second reviewer (J.H.). One reviewer (A.V.C.) developed descriptive themes from the codes by grouping those that were similar together and further developed these into analytical themes by relating them to the reviews’ aims. These codes were discussed and refined with the help of J.H. This approach has been used previously [44] and was chosen as an inductive approach was taken.
3. Results
3.1. Search Results
Figure 1 outlines the PRISMA diagram. A total of 4759 studies were retrieved (4208 after removing duplicates). Thirty-three studies were eligible for inclusion. Eighteen were included in the narrative review (investigating effectiveness), nine were included in the thematic synthesis (investigating acceptability/feasibility), and six were included in both the narrative review and thematic synthesis (investigating acceptability/feasibility, and effectiveness). Table 2 presents descriptions of the included studies.
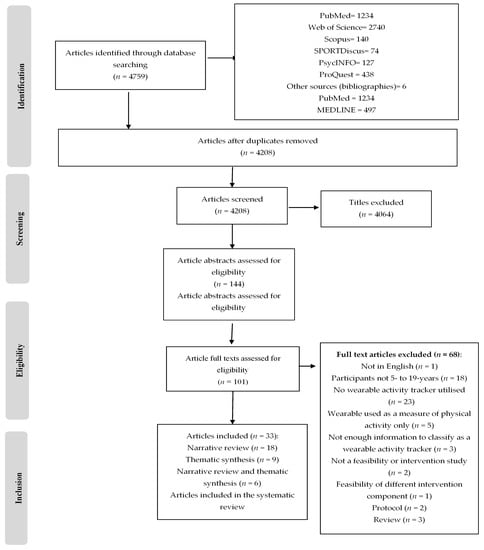
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram illustrating the review process.

Table 2.
Summary of included studies.
3.2. Countries
Most studies were conducted in the USA (n = 16; 48.5%). The remaining studies were conducted in England (n = 4; 12.1%), Australia (n = 3; 9.1%), Canada (n = 2; 6.1%), Germany, Finland, Poland, Netherlands, and New Caledonia (all n = 1; 3.0%). Three studies (9.1%) did not specify the country.
3.3. Population
Studies involved 1843 participants (range: 6–196). Most studies targeted only adolescents (10 to 19 years) (n = 23, 70%), with eight (24%) focusing on children and adolescents (5 to 19 years) and two (6%) on only younger children (5 to 9 years). Seventeen studies (51.5%) recruited participants from specific demographic groups (e.g., overweight/obesity, low PA, ADHD, cancer survivors, rural communities).
3.4. Study Design
Study periods ranged from 4 days [62] to 6 months [58,72]. Most studies were pilot or feasibility studies (n = 25; 75.8%), four (12.1%) were quasi-experimental, and four (12.1%) were RCTs. Of the 24 effectiveness studies, most had one study group (n = 18; 75%), with six (25%) comparing two study groups, of which one group did not use a wearable [69]. Sixteen effectiveness study groups used a wearable as part of a multi-component intervention (55.2%), and 13 (44.8%) used a wearable on its own. The most common additional component was technology-based (n = 5; 41.7%), with three studies using a social media platform [63,69,70].
3.5. Devices
Most studies used one wearable (n = 30; 90.9%). Twenty-one device models were used, with Fitbit devices being the most used brand (n = 17; 51.5%). Fifteen devices were wrist-worn (71.4%), five devices were attached to clothing (23.8%), and one device was worn on the upper arm (4.76%). One study [66] did not report the brand or model of the device.
3.6. Risk of Bias
Figure 2 and Table 3 provide a summary of the RoB results for the effectiveness studies. Six (25%), thirteen (54.2%), and five (20.8%) effectiveness studies were deemed to show a low, medium and high RoB. The most common high-risk practices were not reporting the validity (75%) and reliability (92%) of the wearable. The most common low-risk practice was a study being conducted independently of the wearable manufacturer (96%).
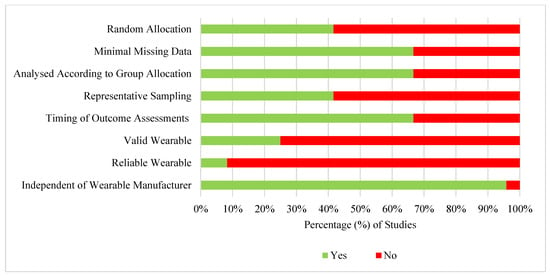
Figure 2.
Summary of the risk of bias results across all criteria for effectiveness studies (n = 24).

Table 3.
Risk of bias results for individual effectiveness studies.
3.7. Behaviour Change Techniques (BCTs)
Figure 3 displays the number of BCTs present in the effectiveness studies. Behavioural change techniques were coded for 29 groups (groups using a wearable). Wearable studies investigating effectiveness had a mean of 7.8 (range: 2–12) BCTs. Sixty-four (68.8%) BCTs were not used in any effectiveness studies. Multi-component groups had on average 9.6 BCTs, compared to an average of 6.3 BCTs for those using a wearable alone. Eight BCTs were unique to multi-component groups. Four control groups (30.8%) had one BCT present [54,63,65]. One study had a comparator intervention group (no wearable), with eight BCTs present [69].
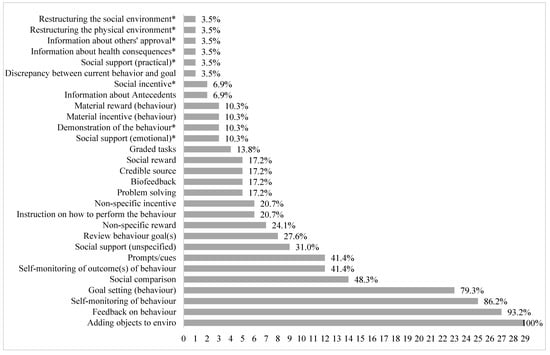
Figure 3.
Total number of wearable groups with BCTs present in studies investigating effectiveness (n = 29). * Present in multi-component study groups exclusively.
3.8. Outcomes
Of the 24 effectiveness studies, 14 (58.3%) used a wearable as an outcome measure, three (12.5%) used self-reporting, two (6.1%) used a research-grade monitoring-device (e.g., accelerometer), two (8.3%) used both a wearable and self-report, and three studies (12.5%) used a wearable and a research-grade monitoring-device. Most studies (n = 17; 70.8%) reported more than one PA outcome. Table S3 displays how the studies measured and defined PA outcomes.
3.9. Effectiveness of Wearables on Physical Activity Outcomes
Of the 24 studies examining the effectiveness of wearables for increasing PA in children and adolescents, a range of different outcome measures were used. The findings of these studies, according to the different outcomes, are summarised below. Findings are stratified by the number of BCTs included in the intervention (above or below the mean number of BCTs, which was eight in this review (see Section 3.7), and, where applicable, age group (children versus adolescents).
3.9.1. Step Count
Fifteen studies measured step count [23,25,47,48,50,51,53,58,59,64,66,67,70,72]. Most studies had a medium RoB (n = 10; 66.7%). Participants recorded an average of 8166 daily steps throughout the study periods [25,48,50,51,64,66,70,72].
Step count: ≥8 BCTs: Eight studies measuring step count incorporated ≥8 BCTs [23,25,51,58,59,64,66,70]. Two studies had child participants (5 to 9 years), with one finding that children took 630 more steps when using a wearable than in a typical recess period (not tested statistically) [23]. No change in step count was found in the second study [64]. Three studies had adolescent participants (10 to 19 years) [51,66,70]. One study found a significant increase in steps (+ 107 steps/day) [70] and one study found that the least active participants increased their daily steps by 15% [51] during intervention periods. There were no differences in step count between adolescents using a wearable on their own and adolescents using a wearable alongside their parent [66]. Three studies had both child and adolescent participants (5 to 19 years) [25,58,59]. One study found those participating in the intervention took significantly more steps (+ 2500 steps) than controls [59], whereas the two remaining studies found no significant change in step count [25] nor any differences in step count between the intervention and control group [58].
Step count: <8 BCTs: Five studies measuring step count incorporated <8 BCTs [47,50,53,67,72]. Four studies had only adolescent participants (10 to 19 years) [47,50,67,72], and the remaining studies had both child and adolescent participants (5 to 19 years) [53]. Two studies found no difference in step count from pre- to post-intervention [47] or between the intervention and control group [53]. One study found that step counts increased by 381 steps/day from intervention week 1 to week 4, but this was not tested statistically [50]. Adolescents participating in a multi-component intervention (wearable and acceptance-based behaviour counselling, with six BCTs), had a significantly higher step count throughout the intervention, which was not found in those receiving a wearable alone (with three BCTs) [67]. One study found a decrease in step count from pre- to post-intervention (−1361 steps/day, not tested statistically) [72].
Step count: ≥8 BCTs and <8 BCTs: Two studies measuring step count compared the results of adolescents participating in one of two intervention groups: one with ≥8 BCTs and one with <8 BCTs [48,50]. One study found higher step counts (not tested statistically) for adolescents receiving a multi-component intervention (wearable, step challenge, and video-based PA exercise sessions (with 11 BCTs)) than those receiving a wearable alone (with seven BCTs) [48], whereas the other study found no difference between adolescents receiving only a wearable (with four BCTs) and adolescents receiving a wearable alongside goal-setting and a behaviour change session (with 10 BCTs) [50].
3.9.2. Achievement of Step Goals
Four studies measured the achievement of daily step goals [46,51,53,72]. Most studies had a medium RoB (n = 3; 75%) and had adolescent participants [46,51,72] or both children and adolescent participants [53]. Three studies had <8 BCTs (5–7 [46,53,72]) and one study had 8 BCTs [51]. Daily step goals were personalised [46,53] at 10,000 [46,72], 11,000 [51] or 12,000 steps/day [46]. Participants achieved step goals on 35–54% of intervention days [46,51]. There were no differences in the achievement of step goals between the intervention and control groups [53]. One study reported that two participants (8.3%) achieved the step goal of 10,000 steps/day for at least half of the intervention days in months 1 and 2 [72].
3.9.3. Moderate-to-Vigorous Physical Activity (MVPA)
Fourteen studies reported MVPA [23,24,47,50,52,54,55,56,59,63,64,66,67,69]. Most studies measured MVPA in mins/day (n = 10, 71.4%), with the remaining reporting the number of days which included MVPA [47], the number of 30-minute bouts of MVPA per day [55], and the time spent in MVPA during recess [23] and school hours [59]. Six studies (42.9%) had a medium RoB, five studies (35.7%) had a low RoB, and three studies (21.4%) had a high RoB. Ten studies measured MVPA from pre- to post-intervention [24,47,50,52,55,56,59,63,67,69].
MVPA: ≥8 BCTs: Nine studies measuring MVPA incorporated ≥8 BCTs [23,24,54,56,59,63,64,66,69]. Two studies had child participants (5 to 9 years) [23,64]. Children achieved a mean of 83 ± 18 mins of daily MVPA whilst using the Garmin vivofit jr [64]. In six 8-year-olds, minutes spent in MVPA during recess increased from the control to intervention period by 21% (not tested statistically) [23]. Six studies had adolescent participants (10 to 19 years) [24,54,56,63,66,69], and one study had both child and adolescent participants [59]. Three studies found no differences in time spent in MVPA between the intervention and control group [24,63,69]. Two studies found participants in the intervention group spent significantly more time in MVP (+ 4.99–6.14 mins/day [54] and + 5 mins/day) [59] than the control group. One study found adolescents in the intervention group participated in an average of 15.26 mins/day of MVPA, which was significantly greater than those participating in the active control (9.12 mins/day) and passive control (10.27 mins/day) groups [54]. One study found no significant differences in time spent in MVPA throughout an intervention [66], whereas one study found time spent in MVPA decreased significantly by 9.5 mins/day [56].
MVPA: < 8 BCTs: Four studies measuring MVPA incorporated <8 BCTs [47,52,55,67]. All four studies had adolescent participants. In two studies, there was no change in the number of days spent participating in ≥60 mins of MVPA from pre- to post-intervention [47] or the number of bouts of MVPA throughout the intervention period [55]. One intervention found a significant average daily increase of 15 mins/day from pre- to post-intervention [52], and one study found that those receiving a wearable alone significantly increased their time spent in MVPA by 11.99 mins/day (with three BCTs), and those receiving multi-component intervention significantly increased their time spent in MVPA by 7.25 mins (with six BCTs) [67].
MVPA: ≥8 BCTs and <8 BCTs: One study measuring MVPA compared the results of adolescents participating in one of two intervention groups: one with ≥8 BCTs and one with <8 BCTs [50]. There were no significant differences in the minutes of MVPA between those receiving a wearable alone (with four BCTs) and those receiving a wearable alongside goal-setting and a behaviour change session (with 10 BCTs) [50].
3.9.4. Light, Moderate, and Vigorous-Intensity Physical Activity (LPA, MPA, VPA), Sedentary Time, and Metabolic Equivalents (METs)
Seven studies reported LPA, MPA, VPA, sedentary time, or total METs [24,48,51,55,58,63,69]. Most studies had a medium RoB (n = 5; 71.4%) and incorporated ≥8 BCTs (n = 5; 71.4%) [24,51,58,63,69]. One study found that adolescents participated in 64, 14 and 7 mins/day of LPA, MPA, and VPA, respectively [51]. Four (57.1%) studies reported at least one favourable effect, most commonly a reduction in sedentary behaviour [24,48,58,69]. Three studies found that time spent sedentary was significantly lower in the adolescents participating in the intervention group or a subsample (adolescent boys [24]) than the control group [24,58,69], whereas one found no difference [63]. Time spent sedentary was significantly lower for participants receiving Facebook-delivered lifestyle counselling and a wearable (with 11 BCTs) (but not those receiving Facebook-delivered lifestyle counselling alone, with eight BCTs) than the control group during weekdays [69] and for participants receiving a wearable, a step challenge, and video-based PA exercise sessions (with 11 BCTs) than those receiving a wearable alone (with seven BCTs) [48]. Of the three studies measuring pre- and post-intervention LPA, MPA, VPA, and/or METs, one reported a significant increase in MPA for adolescent girls receiving a wearable from baseline to 3 months post-intervention (but not at an 8 month follow-up) compared to the control group [24]. The remaining two studies [55,69] did not report any changes in pre- to post-intervention LPA, MPA, VPA, and/or METs.
3.9.5. Total Physical Activity
One medium-RoB study reported that self-reported PA did not significantly differ between 9 to 12-year-olds in the intervention and control groups (with nine BCTs) [58].
3.9.6. Active Minutes
Four medium-RoB studies reported active minutes [46,48,53,58]. Studies had adolescent participants [46,48] or both child and adolescent participants [53,58]. There were no differences in total active minutes [53], the achievement of active minute goals [53], and easy minutes [58] between intervention and control groups. Adolescents achieved their daily active goal on 55% of intervention days, achieving a mean of 101 active daily minutes by the last intervention week [46]. Adolescents given a wearable, step challenge, and video-based PA exercise sessions (with 11 BCTs) spent more daily minutes being fairly active and very active (not tested statistically) than those receiving a wearable alone (with seven BCTs) [48].
3.9.7. Calorie Expenditure
Two low-RoB studies reported the calories expended in adolescents [65,66]. Calories expended did not differ between intervention groups (wearable alone and wearable with parent, with 11 BCTs for both groups [66]) or the control group [65]. There was some evidence that adolescents who continued using the wearable burned more calories than those that did not [66].
3.10. Thematic Synthesis
Fifteen studies [32,33,49,50,57,58,60,61,62,63,65,67,68,71,72] were included in the thematic synthesis. Eleven [33,49,57,58,60,61,62,63,65,68,71] provided quotations from participants. Table 4 provides an overview of the themes identified, along with findings and supporting quotations. The inductive line-by-line coding resulted in 182 codes, which were developed into four analytical themes embedding 13 subthemes.

Table 4.
Themes, findings, and supporting quotations identified in the thematic synthesis.
4. Discussion
This systematic review investigated the acceptability, feasibility, effectiveness, and potential mechanisms of action underlying the effectiveness of wearables for increasing PA in children and adolescents (5 to 19 years). Thirty-three studies were identified, with 18 investigating effectiveness, nine investigating acceptability/feasibility, and six investigating both the acceptability/feasibility and effectiveness of wearables.
4.1. Effectiveness of Wearables on Physical Activity Outcomes
This review found that half of all effectiveness studies reported some evidence that wearables may increase PA outcomes (steps, MVPA) and reduce sedentary time. However, the evidence was mixed. There were no apparent differences in wearables’ effectiveness on steps or MVPA between interventions incorporating ≥8 BCTs, and <8 BCTs. There was mixed evidence that multi-component interventions that had more BCTs were more effective at increasing step counts and MVPA than using wearables on their own. However, it was found that multi-component interventions may be more effective at reducing sedentary behaviour than using wearables on their own. The heterogeneity of the study samples, design, and PA outcomes did not permit a meta-analysis to be conducted. Thus, it is difficult to determine what intervention approach may be effective and why the evidence was mixed. In contrast to this review’s findings, a meta-analysis exploring the effectiveness of wearables on adult PA and sedentary behaviour [20] found multi-component interventions had a greater effect on PA than those using wearables alone [20], and there was no evidence that wearables reduced sedentary time in adults [20]. Potential reasons for the differences between the findings of this review and previous reviews in adults may be due to the types of BCTs used and children/adolescents’ ability to understand and utilise the included BCTs, which is discussed in Section 4.2. However, there is a need for more controlled trials to establish whether multi-component interventions produce different PA outcomes in children and adolescents and adults than using wearables alone [20].
Despite this review’s aim of exploring wearable effects on child (5 to 9 years) and adolescent (10 to 19 years) PA, most studies included only adolescent participants (n = 23, 70%), with two studies (6%) including only child participants. Thus, caution should be taken when generalising results to all age groups (5 to 19-year-olds). A previous systematic review found that smartphone-based interventions were more effective at increasing child PA than adolescent PA [73]. It was suggested that younger participants would have required parental assistance to use the technology, which may have encouraged parental involvement and the monitoring of their child’s PA behaviours [73]. One study included in this review found no difference in daily steps, MVPA, or calorie expenditure between adolescents provided with a wearable alone and adolescents and their parent receiving a wearable [66]. Therefore, the potential addition of parental involvement in child-based wearable interventions may result in different PA outcomes to adolescent-based wearable interventions, in which parental involvement may have less of an influence. However, it is unclear whether there would be any differences in wearables’ effectiveness based on age groups as the included studies with child and adolescent participants did not stratify their results based on age groups.
Despite the mixed evidence regarding the effectiveness of wearables, the thematic synthesis revealed that some participants perceived an increase in their PA levels. This perceived increase in PA has been found in adult wearable users [39,74,75]. However, participants from three studies suggested that a wearable did not increase their PA, as they were already active. One study found adolescents in the adoption stage (participating in regular PA) of behaviour change increased their MVPA, whereas those in the preadoption stage (not participating in regular PA, with no/little intention to do so) did not [52]. This evidence suggests that wearables may be more effective for individuals who are already active. There is some evidence that PA interventions in general attract typically active individuals [76,77], thus reflecting a greater problem regarding PA promotion. In this review, four studies recruited inactive participants [24,49,67] or those with low motivation to be physically active [65]. There was some evidence that wearables increased inactive children/adolescents’ PA (MVPA [67], and MPA for girls [24]); thus, future research could benefit from engaging less active children/adolescents in wearable interventions.
4.2. Mechanisms of Action
On average, 7.8 BCTs were present in studies investigating the effectiveness of wearables. The most included BCTs (other than adding an object to the environment (wearable)) were feedback on behaviour, self-monitoring of behaviour, and goal setting. Previous evidence suggests that interventions incorporating feedback, self-monitoring, and goal setting are more effective at increasing PA than those without these components [11,78], prompting both short (≤6 months) and long-term (≥12 months) behaviour change [79]. The thematic synthesis found that children and adolescents perceived feedback, self-monitoring, and goal setting as an acceptable way of increasing their PA. However, with regards to effectiveness, there were no apparent associations between the type of BCTs and study effectiveness, given that most studies utilised these BCTs and mixed evidence was found. Discrepancies may be due to users’ ability to utilise the BCTs and the frequency and duration of the used BCTs. This is reflected in the thematic synthesis, whereby some participants suggested a lack of understanding of how to interpret PA data and use device features, such as setting goals [49]. Future interventions may benefit from supporting the use of BCTs and investigating the frequency and duration for which participants use BCTs.
Competition was identified as a potential mechanism of action underlying wearables’ impact on PA. Participants reported competition with friends and trying to beat their previous PA scores/goals. Previous research has found that adults also use competition as a way of increasing PA when using a wearable [39]. An interesting finding from the thematic synthesis was that competition, alongside goal setting, may discourage PA, creating feelings of pressure and guilt [57]. In one study, adolescents perceived that autonomy, relatedness, and competence decreased after using the Fitbit Charge [57]. Qualitative findings suggested that competition and predetermined goals may have contributed to these findings [57]. According to the self-determination theory, for a behaviour (e.g., PA) to occur, an individual must be motivated to perform the behaviour [57,80]. This motivation is supported by a person’s autonomy, relatedness, and competence [80]. Thus, the reduction in these three constructs [57] may suggest that wearables have a negative effect on motivation to be physically active. However, an online survey found that wearables resulted in minimal negative psychological consequences in current and previous adult wearable users [81]. More research is needed to explore the impact of wearables on child and adolescent mental health and well-being and to investigate how wearables may be best used to minimise the negative impact on an individual’s perceived autonomy, relatedness, and competence to be physically active.
A recent study found that wearables and their partnering apps had an average of 19 out of 93 BCTs (range: 15–24) [13]. This compares to the total of 7.8 found in the current review. Thus, the included studies did not utilise all BCTs that are already embedded in wearables. Indeed, 64 (68.8%) of the 93 BCTs were not used in any included effectiveness study, despite previous research confirming that some BCTs (e.g., action planning) are embedded in most wearables [13]. Some absent BCTs, such as action planning and self-talk, have previously been found to increase child and adolescent [11,82] and adults’ PA [83]. Future research may benefit from combining additional BCTs into wearable interventions, in addition to utilising the BCTs already embedded in wearables. A meta-analysis demonstrated the effectiveness of combining certain BCTs [84]. Interventions were less effective when providing feedback without instructions on how to perform the behaviour and most effective when combining BCTs that corresponded to providing information about health consequences, action planning, and prompts/cues [84].
4.3. Acceptability and Feasibility
The acceptability and feasibility of wearables are important for the engagement and effectiveness of an intervention [85]. This review found some evidence that wearables are acceptable and feasible for increasing PA in children and adolescents. The Technology Acceptance Model (TAM [86]) is a commonly used model for understanding users’ acceptance of technology [86,87,88]. The TAM suggests that perceived ease of use and perceived usefulness predict the intention to use technology and in turn actual technology use [49,88]. Perceived ease of use and usefulness of using wearables significantly predicted wearable use in adult users [89].
4.3.1. Perceived Ease of Use
Perceived ease of use is defined as the degree to which a person believes that using a system (wearable) would be free of effort [88]. There is some evidence that wearables were easy to use. One parent reported only using PA outputs that were easy for them to understand, such as steps and distance travelled, as they reflected everyday terminology compared to device-specific terminology (e.g., sqoins; [62]) [60]. Adults have suggested steps to be the most useful type of PA information provided by wearables [74,75]. However, some wearable features (e.g., partnering app challenges, goal setting [49,62]) were deemed difficult to use. The cost of using a wearable (e.g., mobile data allowance) was considered a barrier, regardless of an individual’s socio-economic status [52,68]. When access to technology was available, charging and syncing devices were considered burdensome, and some participants stopped carrying out these tasks. Researchers may have to support individuals to overcome these barriers, such as syncing and charging devices, or prompting participants via action planning techniques/reminders. However, this may reduce the feasibility of large-scale studies by increasing the burden on researchers.
4.3.2. Perceived Usefulness
Wearables were perceived as a useful (the degree to which users believe the wearable would enhance their performance; e.g., PA [88]) way to increase some, but not all, users’ PA (Section 4.1). The reported novelty effect may reflect a reduction in wearables’ perceived usefulness to increase PA in children and adolescents. This reported novelty effect corresponds to device adherence rates declining after 2–4 weeks of use [52,57,68]. It is unclear why this novelty period exists; however, some adults have reported stopping using a wearable due to boredom [90] or feeling that they learned everything they needed from the initial use of the wearable [74]. However, in one study included in this review, adolescents reported not having a safe space to be active [33]. This reflects general barriers to PA beyond wearable use and may contribute to the novelty effect. To encourage long-term device use, the wearable must support users’ pre-existing personal and social contexts [39]. Researchers should not only consider how to support wearables’ perceived usefulness but how to overcome individual barriers to PA.
4.4. Strengths and Limitations
A strength of this systematic review was the ability to update a previous review [22], given the progression in research. Despite this, the quality of these studies does not appear to have progressed, and due to the heterogeneity of study designs and the measuring and reporting of PA outcomes, a meta-analysis was unable to be carried out. Most studies were pilot/feasibility studies (n = 15), had short durations (with a mode of 4 weeks), lacked control groups (n = 12, 50%), and varied in terms of how PA was measured (21 different measurement tools). Physical activity outcomes were measured and defined differently (e.g., studies defined MVPA in nine different ways), and it was unclear how some studies defined outcomes (MVPA [64,66], MPA, VPA, easy minutes [58], and active minutes [46,53,58]). Nineteen (79.2%) studies used a wearable as a measure of PA, as well as the intervention/feasibility tool. Given the most common high-risk practices were the lack of reporting of the validity (75%) and reliability (92%) of wearables and that wearables overestimate step counts in children and adolescents [91,92], there is a need for more rigorous studies to evaluate the long-term effectiveness of wearables for children and adolescents’ PA.
Most studies (n = 23, 70%) had only adolescent participants (10 to 19 years); thus, the generalisability of the results to younger age groups (5 to 9 years) is limited. Future research would benefit from investigating wearable acceptability, feasibility, and effectiveness in 5 to 9-year-olds, and where applicable, stratify results based on age groups.
A strength of the current review was the mixed-method approach utilised. Mixed-method studies are widely used to develop PA interventions [93,94,95] and can help in understanding the mechanisms of action behind intervention effects [96]. In particular, integrating the quantitative and qualitative findings (the 1 + 1 = 3 approach [97]) rather than interpreting them separately is recognised as a way of enhancing the value of mixed-methods research [98]. Additionally, BCT coding had the potential to identify “active ingredients” that may create more effective future PA interventions [42]. The BCTTv1 offers an extensive list of well-defined and distinct BCTs [12], which can be mapped on to components of the Behaviour Change Wheel (e.g., Theoretical Domains Framework (TDF) and COM-B model), enabling a systematic way of developing future PA interventions and policies [42]. Unfortunately, the current review found no apparent differences between the number of BCTs utilised and the effectiveness of interventions. It may be that differences in BCT engagement (the frequency and duration of BCTs) rather than the presence (versus absence) of BCTs influenced the effectiveness of interventions. However, the included studies did not report the frequency and duration of BCTs, limiting the ability to code BCT engagement in the current review.
4.5. Conclusions
This review observed that approximately half of all effectiveness studies found some evidence that wearables can increase steps and MVPA and reduce sedentary behaviour; however, most evidence was mixed. There were no apparent differences in the effectiveness of interventions based on the number of BCTs used and between studies using a wearable alone or as part of a multi-component intervention. There was some evidence that wearables are acceptable for some children and adolescents, but technical difficulties, device designs, and the novelty effect of using these devices may impact their use. There were mixed perspectives on whether wearables increased PA. Most studies (70%) included only adolescent participants; therefore, caution should be taken when generalising results to younger children. More rigorous (e.g., RCTs and valid and reliable measures of PA) and long-term studies are required. Furthermore, future research would benefit from reporting the duration and frequency in which BCTs are used and investigating the acceptability, feasibility, and effectiveness of wearables in younger age groups (e.g., 5 to 9-year-olds). Further research should consider how to utilise wearable features that motivate individuals, encourage long-term use, limit negative feelings, and overcome barriers to using wearables, as well as barriers to general PA participation.
Supplementary Materials
The following are available online at: https://www.mdpi.com/article/10.3390/ijerph18126211/s1, Table S1: Search strings and results, Table S2: Risk of bias criteria, descriptions, and examples; Table S3: Physical activity measures, and classifications, used in effectiveness studies.
Authors Contributions
Screening of articles and risk of bias assessment: A.V.C. and D.D.B. Third reviewer for screening of articles: S.C. Behaviour change technique coding and thematic synthesis: A.V.C. and J.H. Review design, and protocol: A.V.C., D.D.B., S.C., S.A.C., J.H., N.D.R., S.E.B. All co-authors (D.D.B., S.C., S.A.C., J.H., N.D.R., S.E.B.) provided feedback and support throughout and approved the final manuscript to be published. All authors have read and agreed to the published version of the manuscript.
Funding
This review is funded as part of a PhD studentship by the Born in Bradford study. The Born in Bradford study receives core infrastructure funding from the Wellcome Trust (WT101597MA) and the National Institute for Health Research (NIHR), under its NIHR ARC Yorkshire and Humber (NIHR200166) and Clinical Research Network (CRN) research delivery support. For this work, funding from Sport England’s Local Delivery Pilot was awarded. S.A.C is supported by the NIHR Leicester Biomedical Research Centre—Lifestyle theme. The views expressed in this publication are those of the author(s) and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Competing Interests
N.D.R. declares involvement in a start-up technological company. All other authors report no competing interests.
References
- Kim, J.; Chun, S.; Heo, J.; Lee, S.; Han, A. Contribution of Leisure-Time Physical Activity on Psychological Benefits Among Elderly Immigrants. Appl. Res. Qual. Life 2016, 11, 461–470. [Google Scholar] [CrossRef]
- Poitras, V.J.; Gray, C.; Borghese, M.M.; Carson, V.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.; Pate, R.R.; Gorber, S.C.; Kho, M.; et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41, S197–S239. [Google Scholar] [CrossRef] [PubMed]
- Reiner, M.; Niermann, C.; Jekauc, D.; Woll, A. Long-term health benefits of physical activity—A systematic review of longitudinal studies. BMC Public Health 2013, 13, 813. [Google Scholar] [CrossRef] [PubMed]
- Mark, A.E.; Janssen, I. Influence of Movement Intensity and Physical Activity on Adiposity in Youth. J. Phys. Act. Health 2011, 8, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, B.G.C.; da Silva, I.C.M.; Ekelund, U.; Brage, S.; Ong, K.K.; Rolfe, E.D.L.; Lima, N.P.; da Silva, S.G.; de França, G.V.A.; Horta, B.L. Associations of physical activity and sedentary time with body composition in Brazilian young adults. Sci. Rep. 2019, 9, 5444. [Google Scholar] [CrossRef]
- Larouche, R.; Boyer, C.; Tremblay, M.S.; Longmuir, P. Physical fitness, motor skill, and physical activity relationships in grade 4 to 6 children. Appl. Physiol. Nutr. Metab. 2014, 39, 553–559. [Google Scholar] [CrossRef] [PubMed]
- Biddle, S.J.; Ciaccioni, S.; Thomas, G.; Vergeer, I. Physical activity and mental health in children and adolescents: An updated review of reviews and an analysis of causality. Psychol. Sport Exerc. 2019, 42, 146–155. [Google Scholar] [CrossRef]
- Wu, X.Y.; Han, L.H.; Zhang, J.H.; Luo, S.; Hu, J.W.; Sun, K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS ONE 2017, 12, e0187668. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Ortega, F.B.; Martínez-Gómez, D.; Labayen, I.; Moreno, L.A.; De Bourdeaudhuij, I.; Manios, Y.; Gonzalez-Gross, M.; Mauro, B.; Molnar, D.; et al. Objectively Measured Physical Activity and Sedentary Time in European Adolescents: The HELENA Study. Am. J. Epidemiol. 2011, 174, 173–184. [Google Scholar] [CrossRef]
- Metcalf, B.; Henley, W.; Wilkin, T. Effectiveness of intervention on physical activity of children: Systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54). BMJ 2012, 345, e5888. [Google Scholar] [CrossRef]
- Hynynen, S.T.; van Stralen, M.; Sniehotta, F.F.; Araújo-Soares, V.; Hardeman, W.; Chinapaw, M.; Vasankari, T.; Hankonen, N. A systematic review of school-based interventions targeting physical activity and sedentary behaviour among older adolescents. Int. Rev. Sport Exerc. Psychol. 2015, 9, 22–44. [Google Scholar] [CrossRef]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Düking, P.; Tafler, M.; Wallmann-Sperlich, B.; Sperlich, B.; Kleih, S. Behavior Change Techniques in Wrist-Worn Wearables to Promote Physical Activity: Content Analysis. JMIR mHealth uHealth 2020, 8, e20820. [Google Scholar] [CrossRef]
- Mercer, K.; Giangregorio, L.; Schneider, E.; Chilana, P.; Li, M.; Grindrod, K. Acceptance of commercially available weara-ble activity trackers among adults aged over 50 and with chronic illness: A mixed-methods evaluation. JMIR mHealth uHealth 2016, 4, e7. [Google Scholar] [CrossRef]
- Dean, D.A.L.; Griffith, D.M.; McKissic, S.A.; Cornish, E.K.; Johnson-Lawrence, V. Men on the Move–Nashville: Feasibility and Acceptability of a Technology-Enhanced Physical Activity Pilot Intervention for Overweight and Obese Middle and Older Age African American Men. Am. J. Men’s Health 2018, 12, 798–811. [Google Scholar] [CrossRef]
- Hardcastle, S.J.; Galliott, M.; Lynch, B.M.; Nguyen, N.H.; Cohen, P.A.; Mohan, G.R.; Johansen, N.J.; Saunders, C. Acceptability and utility of, and preference for wearable activity trackers amongst non-metropolitan cancer survivors. PLoS ONE 2018, 13, e0210039. [Google Scholar] [CrossRef]
- Hartman, S.J.; Nelson, S.H.; Weiner, L.S.; Lyons, E.; Dominick, G. Patterns of Fitbit Use and Activity Levels Throughout a Physical Activity Intervention: Exploratory Analysis from a Randomized Controlled Trial. JMIR mHealth uHealth 2018, 6, e29. [Google Scholar] [CrossRef]
- Lewis, Z.H.; Lyons, E.J.; Jarvis, J.M.; Baillargeon, J. Using an electronic activity monitor system as an intervention modality: A systematic review. BMC Public Health 2015, 15, 1–15. [Google Scholar] [CrossRef]
- Coughlin, S.S.; Stewart, J. Use of consumer wearable devices to promote physical activity: A review of health inter-vention studies. J. Environ. Health Sci. 2016, 2, 6. [Google Scholar] [CrossRef]
- Brickwood, K.-J.; Watson, G.; O’Brien, J.; Williams, A.D. Consumer-Based Wearable Activity Trackers Increase Physical Activity Participation: Systematic Review and Meta-Analysis. JMIR mHealth uHealth 2019, 7, e11819. [Google Scholar] [CrossRef]
- Cajita, M.I.; Kline, C.E.; Burke, L.E.; Bigini, E.G.; Imes, C.C. Feasible but Not Yet Efficacious: A Scoping Review of Wearable Activity Monitors in Interventions Targeting Physical Activity, Sedentary Behavior, and Sleep. Curr. Epidemiol. Rep. 2020, 7, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Ridgers, N.D.; A McNarry, M.; A Mackintosh, K. Feasibility and Effectiveness of Using Wearable Activity Trackers in Youth: A Systematic Review. JMIR mHealth uHealth 2016, 4, e129. [Google Scholar] [CrossRef] [PubMed]
- Hayes, L.B.; Van Camp, C.M. Increasing physical activity of children during school recess. J. Appl. Behav. Anal. 2015, 48, 690–695. [Google Scholar] [CrossRef] [PubMed]
- Slootmaker, S.M.; Chinapaw, M.J.; Seidell, J.; van Mechelen, W.; Schuit, J. Accelerometers and Internet for physical activity promotion in youth? Feasibility and effectiveness of a minimal intervention [ISRCTN93896459]. Prev. Med. 2010, 51, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Hooke, M.C.; Gilchrist, L.S.; Tanner, L.; Hart, N.; Withycombe, J.S. Use of a Fitness Tracker to Promote Physical Activity in Children With Acute Lymphoblastic Leukemia. Pediatr. Blood Cancer 2016, 63, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Yardley, L.; Ainsworth, B.; Arden-Close, E.; Muller, I. The person-based approach to enhancing the acceptability and feasibility of interventions. Pilot Feasibility Stud. 2015, 1, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Shaw, R.L.; Larkin, M.; Flowers, P. Expanding the evidence within evidence-based healthcare: Thinking about the context, acceptability and feasibility of interventions. Evid. Based Med. 2014, 19, 201–203. [Google Scholar] [CrossRef]
- Lubans, D.R.; Morgan, P.J.; Tudor-Locke, C. A systematic review of studies using pedometers to promote physical activity among youth. Prev. Med. 2009, 48, 307–315. [Google Scholar] [CrossRef]
- Ho, V.; Simmons, R.K.; Ridgway, C.L.; van Sluijs, E.; Bamber, D.J.; Goodyer, I.M.; Dunn, V.J.; Ekelund, U.; Corder, K. Is wearing a pedometer associated with higher physical activity among adolescents? Prev. Med. 2013, 56, 273–277. [Google Scholar] [CrossRef]
- Ridgers, N.D.; Lai, S.K. Use of Wearable Activity Trackers for Physical Activity Promotion; Oxford University Press (OUP): Oxford, UK, 2018. [Google Scholar]
- Kahan, D.; Nicaise, V. Walk as Directed! Adolescents’ Adherence to Pedometer Intervention Protocol. J. Phys. Act. Health 2012, 9, 962–969. [Google Scholar] [CrossRef]
- Schaefer, S.E.; Van Loan, M.; German, J.B. A Feasibility Study of Wearable Activity Monitors for Pre-Adolescent School-Age Children. Prev. Chronic Dis. 2014, 11, E85. [Google Scholar] [CrossRef]
- Schaefer, S.E.; Ching, C.C.; Breen, H.; German, J.B. Wearing, Thinking, and Moving: Testing the Feasibility of Fitness Tracking with Urban Youth. Am. J. Health Educ. 2016, 47, 8–16. [Google Scholar] [CrossRef]
- Sekhon, M.; Cartwright, M.; Francis, J.J. Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Serv. Res. 2017, 17, 1–13. [Google Scholar] [CrossRef]
- Abbott, J.H. The Distinction Between Randomized Clinical Trials (RCTs) and Preliminary Feasibility and Pilot Studies: What They Are and Are Not. J. Orthop. Sports Phys. Ther. 2014, 44, 555–558. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Brown, H.E.; Atkin, A.J.; Panter, J.; Wong, G.; Chinapaw, M.; van Sluijs, E. Family-based interventions to increase physical activity in children: A systematic review, meta-analysis and realist synthesis. Obes. Rev. 2016, 17, 345–360. [Google Scholar] [CrossRef]
- Horsley, T.; Dingwall, O.; Sampson, M. Checking reference lists to find additional studies for systematic reviews. Cochrane Database Syst. Rev. 2011, 2011, MR000026. [Google Scholar] [CrossRef]
- Shih, P.C.; Han, K.; Poole, E.S.; Rosson, M.B.; Carroll, J.M. Use and Adoption Challenges of Wearable Activity Trackers. In Proceedings of the iConference 2015, Newport Beach, CA, USA, 24–27 March 2015. [Google Scholar]
- Lauricella, A.R.; Cingel, D.P.; Blackwell, C.; Wartella, E.; Conway, A. The Mobile Generation: Youth and Adolescent Ownership and Use of New Media. Commun. Res. Rep. 2014, 31, 357–364. [Google Scholar] [CrossRef]
- Higgins, J.P.; Green, S. The Cochrane Collaboration. In Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Chichester, UK, 2011; Volume 4. [Google Scholar]
- Michie, S.; Atkins, L.; West, R. The Behaviour Change Wheel: A Guide to Designing Interventions; Silverback Publishing: London, UK, 2014. [Google Scholar]
- Viswanathan, M.; Patnode, C.D.; Berkman, N.D.; Bass, E.B.; Chang, S.; Hartling, L.; Murad, M.H.; Treadwell, J.R.; Kane, R.L. Assessing the risk of bias in sys-tematic reviews of health care interventions. In Methods Guide for Effectiveness and Comparative Effectiveness Reviews [Internet]: Agency for Healthcare Research and Quality (US); U.S. Department of Health & Human Services: Washington, DC, USA, 2017. [Google Scholar]
- Fletcher, B.R.; Hinton, L.; Hartmann-Boyce, J.; Roberts, N.W.; Bobrovitz, N.; McManus, R.J. Self-monitoring blood pressure in hypertension, patient and provider perspectives: A systematic review and thematic synthesis. Patient Educ. Couns. 2016, 99, 210–219. [Google Scholar] [CrossRef]
- Thomas, J.; Harden, A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med. Res. Methodol. 2008, 8, 45. [Google Scholar] [CrossRef]
- Bianchi-Hayes, J.; Schoenfeld, E.; Cataldo, R.; Hou, W.; Messina, C.; Pati, S. Combining Activity Trackers with Motivational Interviewing and Mutual Support to Increase Physical Activity in Parent-Adolescent Dyads: Longitudinal Observational Feasibility Study. JMIR Pediatr. Parent. 2018, 1, e3. [Google Scholar] [CrossRef] [PubMed]
- Bronikowski, M.; Bronikowska, M.; Glapa, A. Do they need goals or support? A report from a goal-setting intervention using physical activity monitors in youth. Int. J. Environ. Res. Public Health 2016, 13, 914. [Google Scholar] [CrossRef] [PubMed]
- Harris, H.B.; Chen, W. Technology-Enhanced Classroom Activity Breaks Impacting Children’s Physical Activity and Fitness. J. Clin. Med. 2018, 7, 165. [Google Scholar] [CrossRef] [PubMed]
- Drehlich, M.; Naraine, M.; Rowe, K.; Lai, S.K.; Salmon, J.; Brown, H.; Koorts, H.; Macfarlane, S.; Ridgers, N.D. Using the Technology Acceptance Model to Ex-plore Adolescents’ Perspectives on Combining Technologies for Physical Activity Promotion Within an Intervention: Usability Study. J. Med. Internet Res. 2020, 22, e15552. [Google Scholar] [CrossRef]
- Evans, E.W.; Abrantes, A.M.; Chen, E.; Jelalian, E. Using Novel Technology within a School-Based Setting to Increase Physical Activity: A Pilot Study in School-Age Children from a Low-Income, Urban Community. BioMed Res. Int. 2017, 2017, 1–7. [Google Scholar] [CrossRef]
- Galy, O.; Yacef, K.; Caillaud, C. Improving Pacific Adolescents’ Physical Activity Toward International Recommendations: Exploratory Study of a Digital Education App Coupled With Activity Trackers. JMIR mHealth uHealth 2019, 7, e14854. [Google Scholar] [CrossRef]
- Gaudet, J.; Gallant, F.; Bélanger, M.; Wang, J.; Coa, K. A Bit of Fit: Minimalist Intervention in Adolescents Based on a Physical Activity Tracker. JMIR mHealth uHealth 2017, 5, e92. [Google Scholar] [CrossRef]
- Götte, M.; Kesting, S.V.; Gerss, J.; Rosenbaum, D.; Boos, J. Feasibility and effects of a home-based intervention using activity trackers on achievement of individual goals, quality of life and motor performance in patients with paediatric cancer. BMJ Open Sport Exerc. Med. 2018, 4, e000322. [Google Scholar] [CrossRef]
- Guthrie, N.; Bradlyn, A.; Thompson, S.K.; Yen, S.; Haritatos, J.; Dillon, F.; Cole, S.W. Development of an Accelerometer-Linked Online Intervention System to Promote Physical Activity in Adolescents. PLoS ONE 2015, 10, e0128639. [Google Scholar] [CrossRef]
- Heale, L.D.; Dover, S.; Goh, Y.I.; Maksymiuk, V.A.; Wells, G.D.; Feldman, B.M. A wearable activity tracker intervention for promoting physical activity in adolescents with juvenile idiopathic arthritis: A pilot study. Pediatr. Rheumatol. 2018, 16, 1–8. [Google Scholar] [CrossRef]
- Kerner, C.; Burrows, A.; McGrane, B. Health wearables in adolescents: Implications for body satisfaction, motivation and physical activity. Int. J. Health Promot. Educ. 2019, 57, 191–202. [Google Scholar] [CrossRef]
- Kerner, C.; Goodyear, V. The Motivational Impact of Wearable Healthy Lifestyle Technologies: A Self-determination Perspective on Fitbits with Adolescents. Am. J. Health Educ. 2017, 48, 287–297. [Google Scholar] [CrossRef]
- Knox, E.; Glazebrook, C.; Randell, T.; Leighton, P.; Guo, B.; Greening, J.; Davies, E.B.; Amor, L.; Blake, H. SKIP (Supporting Kids with diabetes In Physical activity): Feasibility of a randomised controlled trial of a digital intervention for 9-12 year olds with type 1 diabetes mellitus. BMC Public Health 2019, 19, 1–14. [Google Scholar] [CrossRef]
- Larson, J.N.; Brusseau, T.A.; Wengreen, H.; Fairclough, S.J.; Newton, M.M.; Hannon, J.C. Fit “N” Cool Kids: The Effects of Character Modeling and Goal Setting on Children’s Physical Activity and Fruit and Vegetable Consumption. Clin. Med. Insights Pediatr. 2018, 12, 2–6. [Google Scholar] [CrossRef]
- Mackintosh, K.A.; E Chappel, S.; Salmon, J.; Timperio, A.; Ball, K.; Brown, H.; Macfarlane, S.; Ridgers, N.D. Parental Perspectives of a Wearable Activity Tracker for Children Younger Than 13 Years: Acceptability and Usability Study. JMIR mHealth uHealth 2019, 7, e13858. [Google Scholar] [CrossRef]
- Marttinen, R.; Daum, D.; Fredrick, R.N.; Santiago, J.; Silverman, S. Students’ Perceptions of Technology Integration During the F.I.T. Unit. Res. Q. Exerc. Sport 2019, 90, 206–216. [Google Scholar] [CrossRef]
- Masteller, B.; Sirard, J.; Freedson, P.; Routen, A.; Fuemmeler, B. The Physical Activity Tracker Testing in Youth (P.A.T.T.Y) Study: Content Analysis and Children’s Perceptions. JMIR mHealth uHealth 2017, 5, e55. [Google Scholar] [CrossRef]
- Mendoza, J.A.; Baker, K.S.; Moreno, M.A.; Whitlock, K.; Abbey-Lambertz, M.; Waite, A.; Colburn, T.; Chow, E.J. A Fitbit and Facebook mHealth intervention for promoting physical activity among adolescent and young adult childhood cancer survivors: A pilot study. Pediatr. Blood Cancer 2017, 64, e26660. [Google Scholar] [CrossRef]
- Müller, J.; Hoch, A.-M.; Zoller, V.; Oberhoffer, R. Feasibility of Physical Activity Assessment with Wearable Devices in Children Aged 4–10 Years—A Pilot Study. Front. Pediatr. 2018, 6, 5. [Google Scholar] [CrossRef]
- Nation-Grainger, S. ‘It’s just PE’ till ‘It felt like a computer game’: Using technology to improve motivation in physical education. Res. Pap. Educ. 2017, 23, 1–18. [Google Scholar] [CrossRef]
- Phan, T.-L.T.; Barnini, N.; Xie, S.; Martinez, A.; Falini, L.; Abatemarco, A.; Waldron, M.; Benton, J.M.; Frankenberry, S.; Coleman, C.; et al. Feasibility of Using a Commercial Fitness Tracker as an Adjunct to Family-Based Weight Management Treatment: Pilot Randomized Trial. JMIR mHealth uHealth 2018, 6, e10523. [Google Scholar] [CrossRef] [PubMed]
- Remmert, J.E.; Woodworth, A.; Chau, L.; Schumacher, L.M.; Butryn, M.L.; Schneider, M. Pilot Trial of an Acceptance-Based Behavioral Intervention to Promote Physical Activity Among Adolescents. J. Sch. Nurs. 2019, 35, 449–461. [Google Scholar] [CrossRef] [PubMed]
- Ridgers, N.D.; Timperio, A.; Brown, H.; Ball, K.; Macfarlane, S.; Lai, S.K.; Richards, K.; A Mackintosh, K.; A McNarry, M.; Foster, M.; et al. Wearable Activity Tracker Use Among Australian Adolescents: Usability and Acceptability Study. JMIR mHealth uHealth 2018, 6, e86. [Google Scholar] [CrossRef] [PubMed]
- Ruotsalainen, H.; Kyngäs, H.; Tammelin, T.; Heikkinen, H.; Kääriäinen, M. Effectiveness of Facebook-Delivered Lifestyle Counselling and Physical Activity Self-Monitoring on Physical Activity and Body Mass Index in Overweight and Obese Adolescents: A Randomized Controlled Trial. Nurs. Res. Pr. 2015, 2015, 1–14. [Google Scholar] [CrossRef]
- Schoenfelder, E.; Moreno, M.; Wilner, M.; Whitlock, K.B.; Mendoza, J.A. Piloting a mobile health intervention to increase physical activity for adolescents with ADHD. Prev. Med. Rep. 2017, 6, 210–213. [Google Scholar] [CrossRef]
- Sharaievska, I.; A Battista, R.; Zwetsloot, J.; Brakenridge, C.; Lyons, E. Use of Physical Activity Monitoring Devices by Families in Rural Communities: Qualitative Approach. JMIR Pediatr. Parent. 2019, 2, e10658. [Google Scholar] [CrossRef]
- Yoost, J.; Gerlach, J.; Sinning, K.; Cyphert, H. The Use of Fitbit Technology among Rural Obese Adolescents. J. Obes. Nutr. Disord. 2018, 10. [Google Scholar]
- He, Z.; Wu, H.; Yu, F.; Fu, J.; Sun, S.; Huang, T.; Wang, R.; Chen, D.; Zhao, G.; Quan, M. Effects of Smartphone-Based Interventions on Physical Activity in Children and Adolescents: Systematic Review and Meta-analysis. JMIR mHealth uHealth 2021, 9, e22601. [Google Scholar] [CrossRef]
- Maher, C.; Ryan, J.; Ambrosi, C.; Edney, S. Users’ experiences of wearable activity trackers: A cross-sectional study. BMC Public Health 2017, 17, 1–8. [Google Scholar] [CrossRef]
- Kinney, D.A.; Nabors, L.A.; Merianos, A.L.; Vidourek, R.A. College Students’ Use and Perceptions of Wearable Fitness Trackers. Am. J. Heal. Educ. 2019, 50, 298–307. [Google Scholar] [CrossRef]
- Vandelanotte, C.; Duncan, M.J.; Kolt, G.S.; Caperchione, C.M.; Savage, T.N.; Van Itallie, A.; Oldmeadow, C.; Alley, S.J.; Tague, R.; Maeder, A.J.; et al. More real-world trials are needed to establish if web-based physical activity interventions are effective. Br. J. Sports Med. 2018, 53, 1553–1554. [Google Scholar] [CrossRef]
- Vandelanotte, C.; Stanton, R.; Rebar, A.L.; Van Itallie, A.K.; Caperchione, C.M.; Duncan, M.J.; Savage, T.N.; Rosenkranz, R.R.; Kolt, G.S. Physical activity screening to recruit inactive randomized controlled trial participants: How much is too much? Trials 2015, 16, 1–3. [Google Scholar] [CrossRef]
- Eckerstorfer, L.V.; Tanzer, N.K.; Vogrincic-Haselbacher, C.; Kedia, G.; Brohmer, H.; Dinslaken, I.; Corcoran, K. Key Elements of mHealth Interventions to Successfully Increase Physical Activity: Meta-Regression. JMIR mHealth uHealth 2018, 6, e10076. [Google Scholar] [CrossRef]
- Samdal, G.B.; Eide, G.E.; Barth, T.; Williams, G.; Meland, E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1–14. [Google Scholar] [CrossRef]
- Ryan, R.M.; Patrick, H. Self-determination theory and physical. Hell. J. Psychol. 2009, 6, 107–124. [Google Scholar]
- Ryan, J.; Edney, S.; Maher, C. Anxious or empowered? A cross-sectional study exploring how wearable activity trackers make their owners feel. BMC Psychol. 2019, 7, 1–8. [Google Scholar] [CrossRef]
- Golley, R.K.; Hendrie, G.A.; Slater, A.; Corsini, N. Interventions that involve parents to improve children’s weight-related nutrition intake and activity patterns—What nutrition and activity targets and behaviour change techniques are associated with intervention effectiveness? Obes. Rev. 2011, 12, 114–130. [Google Scholar] [CrossRef]
- Williams, S.L.; French, D.P. What are the most effective intervention techniques for changing physical activity self-efficacy and physical activity behaviour--and are they the same? Health Educ. Res. 2011, 26, 308–322. [Google Scholar] [CrossRef]
- Dusseldorp, E.; Van Genugten, L.; van Buuren, S.; Verheijden, M.W.; Van Empelen, P. Combinations of techniques that effectively change health behavior: Evidence from Meta-CART analysis. Health Psychol. 2014, 33, 1530–1540. [Google Scholar] [CrossRef]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C.; et al. How We Design Feasibility Studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef]
- Davis, F.D. A Technology Acceptance Model for Empirically Testing New End-User Information Systems: Theory and Results. Ph.D. Thesis, Massachusetts Institute of Technology, Cambridge, MA, USA, 1985. [Google Scholar]
- Lee, Y.; Kozar, K.A.; Larsen, K.R. The technology acceptance model: Past, present, and future. Commun. Assoc. Inf. Syst. 2003, 12, 50. [Google Scholar] [CrossRef]
- Marangunić, N.; Granić, A. Technology acceptance model: A literature review from 1986 to 2013. Univers. Access Inf. Soc. 2015, 14, 81–95. [Google Scholar] [CrossRef]
- Lunney, A.; Cunningham, N.R.; Eastin, M.S. Wearable fitness technology: A structural investigation into acceptance and perceived fitness outcomes. Comput. Hum. Behav. 2016, 65, 114–120. [Google Scholar] [CrossRef]
- Friel, C.P.; Garber, C.E. Who Uses Wearable Activity Trackers and Why? A Comparison of Former and Current Users in the United States. Am. J. Health Promot. 2020, 34, 762–769. [Google Scholar] [CrossRef]
- Schneider, M.; Chau, L. Validation of the Fitbit Zip for monitoring physical activity among free-living adolescents. BMC Res. Notes 2016, 9, 448. [Google Scholar] [CrossRef]
- Hamari, L.; Kullberg, T.; Ruohonen, J.; Heinonen, O.J.; Díaz-Rodríguez, N.; Lilius, J.; Pakarinen, A.; Myllymäki, A.; Leppänen, V.; Salanterä, S. Physical activity among children: Objective measurements using Fitbit One® and ActiGraph. BMC Res. Notes 2017, 10, 1–6. [Google Scholar] [CrossRef]
- Willenberg, L.J.; Ashbolt, R.; Holland, D.; Gibbs, L.; MacDougall, C.; Garrard, J.; Green, J.B.; Waters, E. Increasing school playground physical activity: A mixed methods study combining environmental measures and children’s perspectives. J. Sci. Med. Sport 2010, 13, 210–216. [Google Scholar] [CrossRef]
- Kolehmainen, N.; Ramsay, C.; McKee, L.; Missiuna, C.; Owen, C.; Francis, J. Participation in Physical Play and Leisure in Children With Motor Impairments: Mixed-Methods Study to Generate Evidence for Developing an Intervention. Phys. Ther. 2015, 95, 1374–1386. [Google Scholar] [CrossRef]
- Khan, M.; Bell, R. Bell Effects of a School Based Intervention on Children’s Physical Activity and Healthy Eating: A Mixed-Methods Study. Int. J. Environ. Res. Public Health 2019, 16, 4320. [Google Scholar] [CrossRef]
- Withall, J.; Jago, R.; Fox, K.R. Why some do but most don’t. Barriers and enablers to engaging low-income groups in physical activity programmes: A mixed methods study. BMC Public Health 2011, 11, 507. [Google Scholar] [CrossRef]
- Fetters, M.D.; Freshwater, D. The 1 + 1 = 3 Integration Challenge; SAGE Publications Sage: Los Angeles, CA, USA, 2015. [Google Scholar]
- Fetters, M.D.; Curry, L.A.; Creswell, J.W. Achieving Integration in Mixed Methods Designs-Principles and Practices. Health Serv. Res. 2013, 48, 2134–2156. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).