- Article
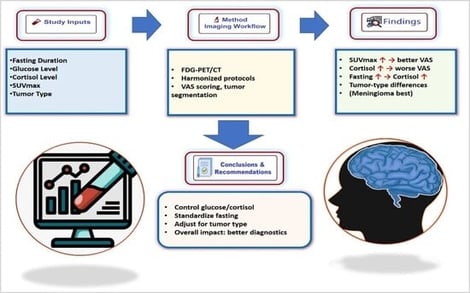
Objectives: This retrospective, multi-center study analyzed pre-existing anonymized clinical data from electronic health records and imaging archives. The analysis utilized real-world clinical data from 200 patients across four tertiary care centers, without additional patient recruitment or interventions. This study aims to investigate the impact of metabolic and physiological factors—specifically blood glucose levels, cortisol concentrations, fasting duration, and tumor histology—on the quality and diagnostic reliability of 18F-FDG PET/CT imaging in patients with primary brain tumors and inflammatory lesions. Methods: A total of 200 patients with primary brain tumors (including astrocytoma, glioblastoma, meningioma, and oligodendroglioma) were evaluated across four institutions using standardized protocols. The study examined the effects of prolonged fasting (>12 h), hyperglycemia (>150 mg/dL), and strict fasting (4–6 h) on tumor-to-background contrast and visual analog scale (DQS) scores. Results: Prolonged fasting was associated with elevated cortisol levels (correlation +0.54, p < 0.001), while hyperglycemia significantly reduced tumor SUVmax by up to 20% (r = −0.35, p = 0.012). Strict fasting and glucose control resulted in improved tumor-to-background contrast and DQS scores (r = +0.83, p < 0.001). Glioblastomas exhibited the highest SUVmax (9.1 ± 3.5), indicating aggressive metabolic activity, whereas meningiomas showed elevated cortisol levels (20.5 ± 6.8 µg/dL) linked to disruption of the hypothalamic–pituitary axis. Regression analysis confirmed that both cortisol and glucose levels independently degraded image quality (β = −0.25 and −0.18, respectively; p < 0.05). Conclusions: The findings highlight the necessity for harmonized patient preparation protocols. Recommendations are in alignment with the SNMMI Procedure Standard/EANM Practice Guideline for Brain [18F] FDG PET imaging.
5 February 2026