-
 Outcomes of Tiopronin and D-Penicillamine Therapy in Pediatric Cystinuria: A Clinical Comparison of Two Cases
Outcomes of Tiopronin and D-Penicillamine Therapy in Pediatric Cystinuria: A Clinical Comparison of Two Cases -
 A Case Report of Tissue Mosaicism in 45,X0/46,XY: Diagnostic Complexity in a Newborn with Ambiguous Genitalia
A Case Report of Tissue Mosaicism in 45,X0/46,XY: Diagnostic Complexity in a Newborn with Ambiguous Genitalia -
 A Rare Case of First-Time Seizure Induced by Cerebral Venous Sinus Thrombosis Following the Use of Tranexamic Acid for Menorrhagia
A Rare Case of First-Time Seizure Induced by Cerebral Venous Sinus Thrombosis Following the Use of Tranexamic Acid for Menorrhagia -
 Metabolism-Guided LATTICE Radiotherapy in an Elderly Patient with Locally Advanced Head and Neck Cancer Treated with Curative Aim: A Case Report
Metabolism-Guided LATTICE Radiotherapy in an Elderly Patient with Locally Advanced Head and Neck Cancer Treated with Curative Aim: A Case Report
Journal Description
Reports — Clinical Practice and Surgical Cases
Reports
— Clinical Practice and Surgical Cases is an international, peer-reviewed, open access journal about the medical cases, images, and videos in human medicine, published quarterly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), PubMed, PMC, FSTA, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 21 days after submission; acceptance to publication is undertaken in 3.1 days (median values for papers published in this journal in the second half of 2025).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
Impact Factor:
0.6 (2024)
Latest Articles
Bilateral Acute Angle-Closure Crisis Associated with Oral Tramadol Use After Robotic-Assisted Hysterectomy: A Case Report
Reports 2026, 9(1), 24; https://doi.org/10.3390/reports9010024 - 13 Jan 2026
Abstract
Background and Clinical Significance: Tramadol-associated acute angle-closure crisis is rare and has been reported only once previously following subcutaneous administration. Acute angle closure may occur in anatomically predisposed individuals in the setting of perioperative physiological stress, with medications acting as contributory factors.
[...] Read more.
Background and Clinical Significance: Tramadol-associated acute angle-closure crisis is rare and has been reported only once previously following subcutaneous administration. Acute angle closure may occur in anatomically predisposed individuals in the setting of perioperative physiological stress, with medications acting as contributory factors. Case Presentation: A 38-year-old woman developed a bilateral acute angle-closure crisis shortly after initiating oral tramadol for postoperative pain relief following an uncomplicated robotic-assisted laparoscopic hysterectomy. Within 24 h, she experienced headache, nausea, vomiting, periocular pain, and blurred vision. Ophthalmic examination revealed markedly elevated intraocular pressure (45 mmHg OD, 39 mmHg OS), corneal epithelial edema, mid-dilated pupils, and completely closed angles on gonioscopy. Prompt intraocular pressure–lowering therapy followed by bilateral Nd:YAG laser peripheral iridotomy resulted in full anatomical and functional recovery, with visual acuity returning to baseline within 48 h. Conclusions: In this case, extreme anatomical susceptibility due to significant hyperopia and very short axial lengths likely played a dominant role, with perioperative physiological factors contributing to pupillary dilation. Oral tramadol may have acted as a permissive factor lowering the threshold for angle closure rather than as a sole causative agent. Awareness of this potential association is important to facilitate early ophthalmic referral and prevent unnecessary diagnostic evaluations.
Full article
(This article belongs to the Section Ophthalmology)
►
Show Figures
Open AccessCase Report
Breast Hemangioma with Slow Growth over 11 Years: A Case Report
by
Anna Tabei, Tomoyuki Fujioka, Kazunori Kubota, Kumiko Hayashi, Tomoyuki Aruga, Iichiroh Onishi and Ukihide Tateishi
Reports 2026, 9(1), 23; https://doi.org/10.3390/reports9010023 - 11 Jan 2026
Abstract
Background and Clinical Significance: Breast hemangioma is an extremely rare benign vascular tumor of the breast. Its imaging findings are nonspecific, and differentiation from malignant tumors such as encapsulated papillary carcinoma, mucinous carcinoma or angiosarcoma is often difficult. We report a case
[...] Read more.
Background and Clinical Significance: Breast hemangioma is an extremely rare benign vascular tumor of the breast. Its imaging findings are nonspecific, and differentiation from malignant tumors such as encapsulated papillary carcinoma, mucinous carcinoma or angiosarcoma is often difficult. We report a case of breast hemangioma that showed slow growth over an 11-year period. Case Presentation: A woman in her 50s presented with a well-defined 11 mm mass in the upper outer quadrant of the left breast detected by ultrasonography. A core needle biopsy revealed a benign lesion, and follow-up was recommended. Eleven years later, the mass had increased to 27 mm. Magnetic resonance imaging showed high signal intensity on T2-weighted images and a fast-plateau enhancement pattern extending from the periphery to the center. Although malignancy was suspected, vacuum-assisted biopsy revealed a hemangioma. Conclusions: Breast hemangioma can show slow enlargement over a long period. Recognition of a characteristic peripheral-to-central enhancement pattern may aid in distinguishing this benign vascular lesion from malignant tumors.
Full article
(This article belongs to the Section Oncology)
►▼
Show Figures

Figure 1
Open AccessCase Report
Anterior Cruciate Ligament Rupture with Concurrent Gastrocnemius Tear: A Case Report of a Rare Pattern of Injury
by
Su Jin Lee, Khang Duy Ricky Le and Roger Davies
Reports 2026, 9(1), 22; https://doi.org/10.3390/reports9010022 - 9 Jan 2026
Abstract
►▼
Show Figures
Background, Clinical Significance: Anterior cruciate ligament (ACL) injuries are common, however the occurrence of concurrent gastrocnemius muscle tears is exceptionally rare. Given this, the diagnosis and management of this pattern of injury is poorly characterised, with lack of current clinically relevant classification systems
[...] Read more.
Background, Clinical Significance: Anterior cruciate ligament (ACL) injuries are common, however the occurrence of concurrent gastrocnemius muscle tears is exceptionally rare. Given this, the diagnosis and management of this pattern of injury is poorly characterised, with lack of current clinically relevant classification systems and evidence-based guidelines to guide treatment. Early recognition is essential. with advanced imaging critical to guiding the diagnosis and management of patients with this pattern of injury. Case presentation: A 39 year old man presented with acute right knee swelling, pain and difficulty weightbearing following a sports-related fall. Clinical examination was suspicious for an ACL injury. Magnetic Resonance Imaging (MRI) of the knee demonstrated the disrupted and displaced ACL fibres, with extensive peri-cruciate oedema around the expected position of the ACL. It was associated with partial avulsion of the medial gastrocnemius origin and incomplete avulsion of the lateral gastrocnemius origin. The patient was referred for an urgent orthopaedics review and is currently on trial of conservative management. Conclusions: In this case report and review of the literature, we evaluate the current understanding of the complexities of combined musculoskeletal injuries and limitations of existing classifications in providing accurate diagnosis and management strategies. Given the rarity of this presentation, the case underscores the lack of evidence-based recommendations for early management, particularly in young, active individuals who are at risk of significant long-term functional impact.
Full article

Figure 1
Open AccessCase Report
Cowden Syndrome in Childhood: Gastrointestinal Involvement in a Multisystem Genetic Disorder—A Case Report
by
Maria Rogalidou, Nikolaos Katzilakis, Kalliopi Stefanaki, Konstantina Dimakou, Dafni Margoni, Iordanis Pelagiadis, Alexandra Papadopoulou and Eftichia Stiakaki
Reports 2026, 9(1), 21; https://doi.org/10.3390/reports9010021 - 9 Jan 2026
Abstract
Background and Clinical significance: Cowden syndrome is an autosomal dominant disorder caused by germline loss-of-function mutations in the PTEN tumor suppressor gene. It is characterized by multiple hamartomas and an increased lifetime risk of malignancies affecting the breast, thyroid, endometrium, and gastrointestinal (GI)
[...] Read more.
Background and Clinical significance: Cowden syndrome is an autosomal dominant disorder caused by germline loss-of-function mutations in the PTEN tumor suppressor gene. It is characterized by multiple hamartomas and an increased lifetime risk of malignancies affecting the breast, thyroid, endometrium, and gastrointestinal (GI) tract. Pediatric presentations may include macrocephaly, scrotal tongue, and intellectual disability. Gastrointestinal involvement is frequent, with juvenile-like hamartomatous polyps occurring in at least half of patients and distributed throughout the GI tract, posing a risk for malignant transformation. Early diagnosis and surveillance are crucial for improving patient outcomes. Case Presentation: We report a case of a 10-year-old Caucasian female with Cowden syndrome, with a history of a malignant germ cell tumor of the ovary consisting of a yolk sac tumor and low-grade immature teratoma diagnosed at age six, and thyroidectomy at age nine. The patient has mild intellectual disability. Routine radiological surveillance revealed a right colon intraluminal mass, prompting referral for pediatric gastroenterology evaluation. Endoscopy identified multiple polyps throughout the colon, stomach, and small intestine. Polypectomy of larger lesions was performed, and histopathology confirmed juvenile-like hamartomatous polyps without dysplasia or malignancy. This case highlights the necessity of comprehensive gastrointestinal evaluation in pediatric Cowden syndrome patients. Endoscopic surveillance is essential for early detection and management of polyps. Conclusions: Given the multisystem involvement and elevated cancer risk associated with PTEN mutations, a multidisciplinary approach that includes genetic counseling, dermatologic evaluation, and ongoing oncologic monitoring is recommended. Increased awareness of gastrointestinal manifestations enables timely intervention and may reduce morbidity and mortality in this high-risk population.
Full article
(This article belongs to the Section Gastroenterology)
►▼
Show Figures

Figure 1
Open AccessCase Report
Persistent Vomiting and Epigastric Pain in an Adolescent: A Case of Superior Mesenteric Artery Syndrome Unmasked
by
Maria Rogalidou, Georgios Papagiannis, Konstantina Dimakou, Paraskevi Galina, Stavroula-Zoe Siska and Alexandra Papadopoulou
Reports 2026, 9(1), 20; https://doi.org/10.3390/reports9010020 - 9 Jan 2026
Abstract
Background and Clinical Significance: Superior mesenteric artery syndrome (SMAS) is a rare and often underdiagnosed cause of proximal intestinal obstruction, resulting from compression of the third portion of the duodenum between the SMA and the aorta. It typically occurs in individuals with significant
[...] Read more.
Background and Clinical Significance: Superior mesenteric artery syndrome (SMAS) is a rare and often underdiagnosed cause of proximal intestinal obstruction, resulting from compression of the third portion of the duodenum between the SMA and the aorta. It typically occurs in individuals with significant weight loss due to mesenteric fat depletion. CasePresentation: We report the case of a 14.5-year-old female presented with a 6-day history of intractable vomiting and epigastric pain, on a background of intermittent vomiting over the preceding six months associated with a 7 kg unintentional weight loss, culminating in inability to tolerate oral intake. Her clinical course was complicated by a transient episode of blurred vision, numbness, and incoherent speech, initially suspected to be a neurological event. Extensive gastrointestinal and neurological investigations were inconclusive. Elevated fecal calprotectin levels raised suspicion for inflammatory bowel disease, given her family history, though endoscopy and histopathology were unremarkable. Advanced imaging ultimately demonstrated a markedly reduced aortomesenteric angle (6°) and distance (4 mm), confirming the diagnosis of SMAS. The patient was initially managed conservatively with total parenteral nutrition (TPN), achieving partial weight gain of 5 kg after 8 weeks of TPN. Due to persistent duodenal compression, surgical intervention was required. At 7-month follow-up, the patient remained symptom-free with restored nutritional status and a good weight gain. Conclusions: This case highlights the importance of considering SMAS in adolescents with chronic upper gastrointestinal symptoms and significant weight loss. Early recognition and appropriate imaging are essential to diagnosis, and timely surgical management can lead to excellent outcomes when conservative treatment is insufficient.
Full article
(This article belongs to the Section Gastroenterology)
►▼
Show Figures

Figure 1
Open AccessCase Report
Unusually Extensive Furuncular Myiasis in a Returning Traveller from Rural Ethiopia Complicated by Streptococcus Pyogenes Secondary Infection Following Albendazole Therapy
by
Diva Jhaveri, Alastair McGregor and Matthew J. W. Kain
Reports 2026, 9(1), 19; https://doi.org/10.3390/reports9010019 - 8 Jan 2026
Abstract
►▼
Show Figures
Background and Clinical Significance: Furuncular myiasis is a tropical parasitic skin infestation caused by dipterous fly larvae, most commonly affecting travellers to endemic regions. While returning travellers typically present with one or few lesions, extensive parasitism is rare. Increased global mobility and
[...] Read more.
Background and Clinical Significance: Furuncular myiasis is a tropical parasitic skin infestation caused by dipterous fly larvae, most commonly affecting travellers to endemic regions. While returning travellers typically present with one or few lesions, extensive parasitism is rare. Increased global mobility and expanding ecological range of myiasis-causing species underscores the need for clinicians in endemic and non-endemic regions to recognise, diagnose, and manage this condition promptly. Awareness of exposure risks—including soil contact, infested clothing, and poor living conditions—is essential to reducing morbidity and preventing complications like secondary bacterial infection. Case Presentation: A healthy male in his forties returned to the UK after a month-long visit to rural Ethiopia, during which he slept on dirt floors and hung his washing on a line. He developed pruritic papular lesions that progressed to erythematous furuncles with central puncta and purulent discharge, accompanied by sensations of movement. The patient self-extracted 12 larvae in Ethiopia and subsequently sought local medical attention, receiving Albendazole, after which emerging larvae were non-motile. On UK presentation, he had 27 lesions at varying stages, 3 with signs of secondary infection. Laboratory investigations revealed elevated inflammatory markers, and wound swabs grew scanty Streptococcus pyogenes. Management included wound occlusion and systemic antibiotics. No further larvae were retrieved, precluding definitive speciation. All lesions improved over subsequent reviews. Conclusions: This case illustrates an unusually extensive presentation of presumed Cordylobia spp. myiasis in a returning traveller, highlighting potential complications following larvicidal therapy. Clinicians should maintain a high index of suspicion for myiasis in patients with compatible cutaneous lesions and relevant history. Increasing travel and shifting vector distributions make familiarity with tropical dermatoses and provision of effective safety measures essential in clinical practice.
Full article

Figure 1
Open AccessCase Report
Delayed Neurologic Response to Dabrafenib and Trametinib in the Case of Mixed Histiocytosis (LCH/ECD): Case Report and Literature Review
by
Shinsaku Imashuku, Miyako Kobayashi, Takashi Miyoshi and Naoyuki Anzai
Reports 2026, 9(1), 18; https://doi.org/10.3390/reports9010018 - 7 Jan 2026
Abstract
Background and Clinical Significance: Histiocytosis encompasses Langerhans cell histiocytosis (LCH) and non-LCH, such as Erdheim–Chester disease (ECD). ECD or a mixed type of histiocytosis (LCH/ECD) may initially involve the central nervous system (CNS), resulting in a delayed diagnosis. More recently, dabrafenib and
[...] Read more.
Background and Clinical Significance: Histiocytosis encompasses Langerhans cell histiocytosis (LCH) and non-LCH, such as Erdheim–Chester disease (ECD). ECD or a mixed type of histiocytosis (LCH/ECD) may initially involve the central nervous system (CNS), resulting in a delayed diagnosis. More recently, dabrafenib and trametinib (Dab/Tra regimen) have become available in its treatment. Case Presentation: A 46-year-old woman with CNS involvement of mixed histiocytosis (BRAF V600E-positive LCH/ECD) was treated with combination therapy using a Dab/Tra regimen. At initial presentation, she exhibited central diabetes insipidus, dysarthria, and gait disturbance with mild spasticity and ataxia, requiring walking assistance even for short distances. The interval from the onset of central neurological symptoms to diagnosis of mixed histiocytosis was 4 years. The introduction of targeted therapy was 2 years later. After seven months of Dab/Tra therapy, partial neurological improvement was observed, as reflected by a decrease in the SARA score from 21/40 to 13/40 and the ICARS score from 33/100 to 28/100. However, further neurological recovery remained significantly delayed. Conclusions: We suspect that the limited improvement may be attributable to the delayed initiation of targeted therapy, in contrast to the more rapid and pronounced responses reported in cases where treatment was started earlier.
Full article
(This article belongs to the Section Haematology)
►▼
Show Figures

Figure 1
Open AccessCase Report
Pain That Challenges Survival: A Novel SCN9A Variant (p.Leu1623Gln) Causing Carbamazepine-Refractory Paroxysmal Extreme Pain Disorder in a Chinese Family — Case Report
by
Man-Kwan Yip, Chun-Ying Janice Liu and Wing-Tat Poon
Reports 2026, 9(1), 17; https://doi.org/10.3390/reports9010017 - 5 Jan 2026
Abstract
Background and Clinical Significance: Paroxysmal extreme pain disorder (PEPD) is an extremely rare autosomal dominant sodium channelopathy caused by SCN9A gain-of-function variants. It is characterized by infantile-onset excruciating paroxysmal pain, typically in rectal, ocular, or mandibular regions, triggered by innocuous stimuli and accompanied
[...] Read more.
Background and Clinical Significance: Paroxysmal extreme pain disorder (PEPD) is an extremely rare autosomal dominant sodium channelopathy caused by SCN9A gain-of-function variants. It is characterized by infantile-onset excruciating paroxysmal pain, typically in rectal, ocular, or mandibular regions, triggered by innocuous stimuli and accompanied by autonomic flares. Carbamazepine is dramatically effective in most reported cases. To date, only two genetically confirmed cases have been documented in Chinese patients, and fewer than 20 disease-causing variants are reported worldwide. We report the third Chinese case harboring a novel likely pathogenic SCN9A variant (p.Leu1623Gln), notable for its unusually severe, progressive, and carbamazepine-refractory phenotype, as well as life-threatening psychiatric sequelae, highlighting phenotypic heterogeneity and the devastating impact when standard therapy fails. Case Presentation: A Chinese male proband with positive family history presented with lifelong trigger-induced catastrophic burning and tearing pain in the perineum and lower limbs, associated with erythema, swelling, and occasional non-epileptic seizures. Attacks worsened with age despite escalating polypharmacy, including high-dose opioids, benzodiazepines, topical lidocaine and carbamazepine. Both the proband and his father developed profound psychosocial sequelae including severe depression and suicidal attempts. Next-generation sequencing in the proband revealed a novel heterozygous likely pathogenic variant NM_001365536.1 (SCN9A): c.4868T>A p.(Leu1623Gln). Conclusions: This third reported ethnic Chinese PEPD case expands the genotypic and phenotypic spectrum of SCN9A-related channelopathies, demonstrating that some variants can produce carbamazepine-refractory, progressive, and profoundly disabling disease with high suicidality risk. Early genetic diagnosis is critical in family planning and cascade testing, and has the potential in guiding targeted therapy that is under active research.
Full article
(This article belongs to the Section Neurology)
►▼
Show Figures

Figure 1
Open AccessReview
Neutrophil–Galectin-9 Axis Linking Innate and Adaptive Immunity in ATL, Sézary Syndrome, COVID-19, and Psoriasis: An AI-Assisted Integrative Review
by
Toshio Hattori
Reports 2026, 9(1), 16; https://doi.org/10.3390/reports9010016 - 31 Dec 2025
Abstract
Beyond their traditional role as short-lived antimicrobial cells, neutrophils are increasingly recognized as key regulators of adaptive immunity and tumor progression. This AI-assisted integrative review investigated the neutrophil–T-cell axis, particularly the role of Galectin-9 (Gal-9), across adult T-cell leukemia/lymphoma (ATL), Sézary syndrome
[...] Read more.
Beyond their traditional role as short-lived antimicrobial cells, neutrophils are increasingly recognized as key regulators of adaptive immunity and tumor progression. This AI-assisted integrative review investigated the neutrophil–T-cell axis, particularly the role of Galectin-9 (Gal-9), across adult T-cell leukemia/lymphoma (ATL), Sézary syndrome (SS), coronavirus disease 2019 (COVID-19), and psoriasis. Leveraging AI tools (GPT-5 and Adobe Acrobat AI Assistant) for literature synthesis (2000–2025) and expert validation, we aimed to identify common immunological mechanisms. Across all conditions, neutrophils displayed persistent activation, elevated Gal-9 expression, and modulated T-cell interactions. In ATL and SS, neutrophilia correlated with poor survival and TCR signaling dysregulation, suggesting Gal-9-mediated immune modulation. In COVID-19 and psoriasis, neutrophil-derived Gal-9-linked innate hyperactivation to T-cell exhaustion and IL-17-driven inflammation. These findings define a recurring neutrophil–Gal-9 regulatory module connecting innate and adaptive immune responses. This study underscores the feasibility of combining AI-driven literature synthesis with expert review to identify unifying immunological mechanisms and therapeutic targets across malignancy and inflammation.
Full article
(This article belongs to the Section Allergy/Immunology)
►▼
Show Figures

Figure 1
Open AccessCase Report
Idiopathic Hypertrophic Pachymeningitis with Elevated Anti-Thyroglobulin Antibodies—A Case Report
by
Paweł Pobudejski, Mateusz Toś, Katarzyna Zawiślak-Fornagiel and Joanna Siuda
Reports 2026, 9(1), 15; https://doi.org/10.3390/reports9010015 - 31 Dec 2025
Abstract
Background and clinical significance: Idiopathic hypertrophic pachymeningitis (IHPM) is a rare inflammatory disorder characterized by diffuse or focal dural thickening and heterogeneous presentations. We report a corticosteroid-responsive IHPM with elevated anti-thyroglobulin (anti-Tg) antibodies despite oncologic control after thyroidectomy. This case suggests that
[...] Read more.
Background and clinical significance: Idiopathic hypertrophic pachymeningitis (IHPM) is a rare inflammatory disorder characterized by diffuse or focal dural thickening and heterogeneous presentations. We report a corticosteroid-responsive IHPM with elevated anti-thyroglobulin (anti-Tg) antibodies despite oncologic control after thyroidectomy. This case suggests that systematic assessment for autoimmunity should be a standard component of the IHPM work-up. Case presentation: A 77-year-old woman presented with recurrent vertigo, imbalance, and headaches. Brain MRI showed diffuse pachymeningeal thickening with mild heterogeneous enhancement, radiologically stable over >2 years. Extensive evaluation excluded infectious, neoplastic (including paraneoplastic), cerebrospinal fluid hypotension and systemic autoimmune causes; findings did not support IgG4-related disease. Thyroid work-up revealed hypothyroidism with multinodular goiter; total thyroidectomy was performed, and there was no indication for adjuvant radioiodine therapy. Despite oncologic control, anti-Tg antibodies remained markedly elevated, while anti-thyroid peroxidase antibodies (anti-TPO) declined. Symptoms repeatedly improved with oral methylprednisolone and recurred on taper; adverse effects were mild and manageable. The patient remains under clinical and oncologic surveillance with symptom-guided steroid re-challenge. Conclusions: IHPM may exhibit a dissociation between clinical response and radiologic course. Persistently elevated anti-Tg after thyroidectomy can coexist with IHPM and may signal ongoing autoimmunity rather than active cancer.
Full article
(This article belongs to the Section Neurology)
►▼
Show Figures

Figure 1
Open AccessCase Report
Dual Tumor Pathogenesis in the Gastrointestinal Tract: Synchronous Rectal Schwannoma and Gallbladder Papillary Adenocarcinoma—A Case Report
by
Adrian Cotovanu, Catalin Dumitru Cosma, Calin Molnar, Simona Gurzu, Marius-Alexandru Beleaua, Vlad Olimpiu Butiurca and Marian Botoncea
Reports 2026, 9(1), 14; https://doi.org/10.3390/reports9010014 - 31 Dec 2025
Abstract
Background and Clinical Significance: Synchronous gastrointestinal tumors are exceptionally rare, particularly when combining histologically distinct benign and malignant components. Schwannomas represent uncommon mesenchymal tumors of the gastrointestinal tract, most frequently arising in the stomach, while rectal localization is exceedingly unusual. Papillary adenocarcinoma
[...] Read more.
Background and Clinical Significance: Synchronous gastrointestinal tumors are exceptionally rare, particularly when combining histologically distinct benign and malignant components. Schwannomas represent uncommon mesenchymal tumors of the gastrointestinal tract, most frequently arising in the stomach, while rectal localization is exceedingly unusual. Papillary adenocarcinoma of the gallbladder is an aggressive malignant entity derived from intracholecystic papillary–tubular neoplasms (ICPNs). The coexistence of these two unrelated neoplasms has not been previously reported, making this case of dual tumor pathogenesis clinically and academically significant. Case Presentation: A 68-year-old female was admitted for surgical management of grade IV uterovaginal prolapse. Preoperative imaging incidentally revealed a well-circumscribed rectal wall mass and gallstones. A combined abdominopelvic operation was performed, including total hysterectomy with bilateral adnexectomy (Wiart procedure), rectosigmoid resection with colorectal anastomosis, and bipolar cholecystectomy. Intraoperatively, a firm intramural rectal lesion and a friable papillary mass in the gallbladder fundus were identified. Histopathologic examination confirmed a benign rectal schwannoma (S-100 positive, CD117/DOG-1 negative) and a papillary adenocarcinoma of the gallbladder, pT3N0M0, with clear resection margins and no lymphovascular or perineural invasion. The postoperative course was uneventful, and the patient remained disease-free at six-month follow-up. Conclusions: This case represents an exceedingly rare benign–malignant synchronous tumor association. The simultaneous occurrence of rectal schwannoma and gallbladder papillary adenocarcinoma underscores the importance of thorough intraoperative exploration and histopathologic evaluation. Complete resection with negative margins and multidisciplinary follow-up remains crucial for optimal outcomes and contributes to understanding dual tumor pathogenesis within the gastrointestinal tract.
Full article
(This article belongs to the Section Surgery)
►▼
Show Figures

Figure 1
Open AccessCase Report
Post-Transplant Double Malignancy: Multiple Myeloma and Papillary Renal Cell Carcinoma—A Case Report
by
Aleksandar Petrov, Miroslava Benkova, Yavor Petrov, Yana Dimieva and Mari Ara Hachmeriyan
Reports 2026, 9(1), 13; https://doi.org/10.3390/reports9010013 - 30 Dec 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: Kidney transplant recipients have a 2–4-fold higher cancer risk than the general population. The sequential occurrence of multiple myeloma (MM) and native-kidney renal cell carcinoma (RCC) is rare and creates competing priorities between anti-myeloma efficacy and allograft preservation. Case
[...] Read more.
Background and Clinical Significance: Kidney transplant recipients have a 2–4-fold higher cancer risk than the general population. The sequential occurrence of multiple myeloma (MM) and native-kidney renal cell carcinoma (RCC) is rare and creates competing priorities between anti-myeloma efficacy and allograft preservation. Case Presentation: A 54-year-old woman with a 2020 living-donor kidney transplant presented in 2024 with bone pain and shoulder swelling. Low-dose whole-body CT showed multiple punched-out osteolytic lesions. Work-up revealed IgG-κ M-protein 38.5 g/L and 25% clonal plasma cells; cytogenetics showed a complex karyotype (R-ISS III). First-line bortezomib/cyclophosphamide/dexamethasone (VCd) was given while maintaining tacrolimus plus low-dose steroid. After four cycles, she achieved very good partial response (M-protein 42.3 to 5.6 g/L) with stable graft function. Follow-up imaging detected a large exophytic mass in the native right kidney; nephrectomy confirmed papillary RCC, type II. Later, the myeloma progressed with epidural extension causing cord compression. Second-line daratumumab/carfilzomib/dexamethasone (DKd) and palliative spine radiotherapy were initiated. The course was complicated by opportunistic infection and pancytopenia, and the patient died in January 2025. Conclusions: Vigilant post-transplant cancer surveillance—including native-kidney RCC—tailored immunosuppression, and multidisciplinary coordination are critical. VCd with tacrolimus may be feasible when graft preservation is prioritized; however, relapsed high-risk MM on DKd carries substantial infectious risk and a guarded prognosis.
Full article

Figure 1
Open AccessCase Report
Immune Myositis Complicating Follicular Lymphoma: Case Report
by
George Sarin Zacharia, Saran Lal Ajai Mokan Dasan and Chinazor Iwuaba
Reports 2026, 9(1), 12; https://doi.org/10.3390/reports9010012 - 29 Dec 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: Idiopathic inflammatory myopathies are a heterogeneous group of autoimmune disorders that may present as paraneoplastic syndromes. Although most frequently associated with solid-organ malignancies, hematological neoplasia, particularly lymphomas, is also likely linked. Case Presentation: We describe a sexagenarian
[...] Read more.
Background and Clinical Significance: Idiopathic inflammatory myopathies are a heterogeneous group of autoimmune disorders that may present as paraneoplastic syndromes. Although most frequently associated with solid-organ malignancies, hematological neoplasia, particularly lymphomas, is also likely linked. Case Presentation: We describe a sexagenarian female with progressive proximal muscle weakness, myalgias, and lymphadenopathy. Laboratory evaluation revealed markedly elevated creatine phosphokinase and myositis-specific antibodies: anti-Mi-2α and anti-EJ. Magnetic resonance imaging of the thighs confirmed active myositis. Lymph node biopsy reported follicular lymphoma. The patient was initiated on methotrexate and rituximab, with which she reported significant symptomatic relief. Conclusions: Inflammatory myopathy is an exceedingly rare presentation of follicular lymphoma. This case emphasizes that lymphomas can closely mimic other disease processes and present significant diagnostic challenges, and they should be included in the differential diagnosis of myopathies. Improved awareness and early diagnosis of lymphoproliferative neoplasia often yield better overall clinical outcomes.
Full article

Figure 1
Open AccessCase Report
Lymphoepithelial Cyst “En Crypto”: A Case Report of a Rare Localization in the Superior Pole of the Palatine Tonsil
by
Constantinos Papadopoulos, Konstantina Dinaki, Anastasia Sarafidou, Maria Peponi and Rafail Ioannidis
Reports 2026, 9(1), 11; https://doi.org/10.3390/reports9010011 - 29 Dec 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: Lymphoepithelial cysts are uncommon benign lesions of the head and neck, rarely encountered within the oral cavity and exceedingly infrequent in the palatine tonsils. Their nonspecific clinical presentation and ability to mimic more common benign entities often render diagnosis
[...] Read more.
Background and Clinical Significance: Lymphoepithelial cysts are uncommon benign lesions of the head and neck, rarely encountered within the oral cavity and exceedingly infrequent in the palatine tonsils. Their nonspecific clinical presentation and ability to mimic more common benign entities often render diagnosis challenging. Case Presentation: We report the case of a 68-year-old woman with a four-year history of persistent foreign-body sensation in the oropharynx despite multiple normal otolaryngologic examinations. Flexible nasoendoscopy was non-diagnostic, as the lesion was deeply concealed within the superior tonsillar pole between the palatine pillars. Targeted tonsillar manipulation ultimately revealed a small pedunculated mass and contrast-enhanced computed tomography demonstrated a well-circumscribed, non-enhancing cystic lesion confined to the tonsillar parenchyma. Surgical excision under general anesthesia confirmed an oral lymphoepithelial cyst on histopathologic analysis. The patient remained asymptomatic with no recurrence at four months. Conclusions: This case underscores the rarity of tonsillar lymphoepithelial cysts, highlights the diagnostic limitations of endoscopic evaluation for cryptic superior-pole lesions and emphasizes the importance of meticulous dynamic oropharyngeal examination. Complete surgical excision is both definitive and curative, with an excellent prognosis.
Full article

Figure 1
Open AccessCase Report
From MAiD Referral to Targeted Therapy Success: A Case of BRAF-Mutated Anaplastic Thyroid Cancer
by
Brett Stubbert, Paul Stewart, Eric Winquist, Matthew Cecchini and Claire Browne
Reports 2026, 9(1), 10; https://doi.org/10.3390/reports9010010 - 28 Dec 2025
Abstract
Background and Clinical Significance: Anaplastic thyroid cancer (ATC) is a rare and aggressive malignancy with a poor prognosis, where median survival typically ranges from 4 to 10 months. Advances in genetic profiling, particularly the identification of BRAF mutations, offer new opportunities for
[...] Read more.
Background and Clinical Significance: Anaplastic thyroid cancer (ATC) is a rare and aggressive malignancy with a poor prognosis, where median survival typically ranges from 4 to 10 months. Advances in genetic profiling, particularly the identification of BRAF mutations, offer new opportunities for targeted therapy. Case Presentation: This case report details the journey of a woman in her late 50s diagnosed with symptomatic ATC. Initial immunohistochemistry (IHC) testing for BRAF mutations returned negative results, leaving the patient with limited treatment options and prompting her to pursue medical assistance in dying (MAiD). However, next-generation sequencing (NGS) confirmed a V600EBRAF mutation, and a basis for targeted therapy. The patient began treatment with dabrafenib-trametinib, followed by pembrolizumab as second-line therapy, ultimately extending her life by nearly seven months. Conclusions: This case underscores the importance of rapid and comprehensive diagnostic approaches, particularly the higher sensitivity of NGS over IHC for detecting BRAF mutations. The complexities of accessing newer therapies in Canada’s single-payer healthcare system are also emphasized. The utilization of newer rapid diagnostic technologies can have a direct impact on directing treatment for ATC and other aggressive malignancies.
Full article
(This article belongs to the Section Oncology)
►▼
Show Figures

Figure 1
Open AccessCase Report
Fatal Suicide Attempt with Upadacitinib (Rinvoq®) in an Adolescent: A Case Report
by
Silviya Stoykova, Ivo Ivanov, Evgeniya Byrzashka and Vasil Atanasov
Reports 2026, 9(1), 9; https://doi.org/10.3390/reports9010009 - 24 Dec 2025
Abstract
Background and Clinical Significance: Upadacitinib, a selective Janus kinase 1 (JAK1) inhibitor, is increasingly prescribed for autoimmune and inflammatory diseases. Although its therapeutic safety profile is well established, fatal intoxications have not been reported to date. Case Presentation: We describe the
[...] Read more.
Background and Clinical Significance: Upadacitinib, a selective Janus kinase 1 (JAK1) inhibitor, is increasingly prescribed for autoimmune and inflammatory diseases. Although its therapeutic safety profile is well established, fatal intoxications have not been reported to date. Case Presentation: We describe the first fatal case of upadacitinib overdose in a 13-year-old girl. Following ingestion of approximately 600 mg (40 × 15 mg tablets Rinvoq®), the patient presented with deep coma, profound bradycardia (~40 bpm) with third-degree atrioventricular block, conduction delay, hypotension, hypothermia, and metabolic acidosis. Laboratory tests showed hyperglycemia (17.8 mmol/L) and only minimal elevations in cardiac biomarkers (CK 57.03 U/L, CK-MB 30.64 U/L, troponin 0.003 ng/mL). Despite advanced resuscitation, the patient succumbed within a few hours. Forensic toxicology revealed extremely high concentrations of upadacitinib, 1.84 µg/mL (~1840 ng/mL) in blood and 70.3 µg/mL in gastric contents, far exceeding reported therapeutic plasma levels (Cmax 36.0 ± 8.8 ng/mL). This case establishes the first reported value for a lethal upadacitinib concentration in humans. The combination of conduction abnormalities, refractory shock, and minimal biomarker changes is consistent with an acute electrophysiological and hemodynamic collapse rather than myocardial infarction. Conclusions: The toxicity of upadacitinib in this case is characterized by profound central nervous system depression, severe cardiovascular (electrophysiological and hemodynamic) disturbances, and metabolic abnormalities (acidosis and hyperglycemia). These findings provide essential reference data for clinical and forensic toxicology, highlight the fatal potential of upadacitinib in overdose, and underscore the importance of secure medication storage and pharmacovigilance in households with adolescents.
Full article
(This article belongs to the Section Critical Care/Emergency Medicine/Pulmonary)
►▼
Show Figures
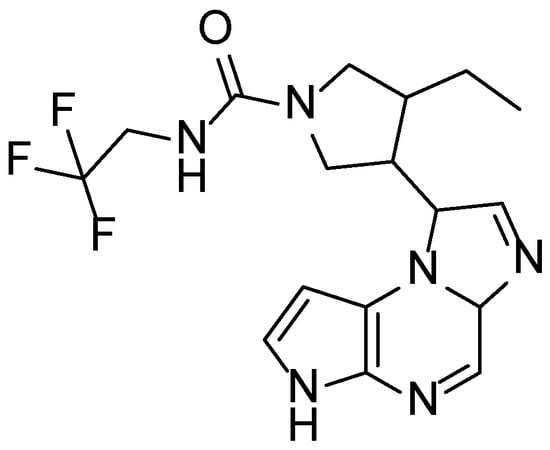
Figure 1
Open AccessCase Report
A Case Report: Immediate Implant Placement with PRF, Photogrammetry-Guided Workflow, and Monolithic Zirconia Full-Arch Restoration
by
Przemysław Bolesław Grzesiak and Adam Aleksander Nowicki
Reports 2026, 9(1), 8; https://doi.org/10.3390/reports9010008 - 24 Dec 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: This case presents immediate implant placement combined with PRF (A-PRF+) and a photogrammetry-based workflow, illustrating predictable full-arch implant-supported rehabilitation. Case Presentation: Main clinical findings included compromised abutment teeth and patient dissatisfaction with aesthetics. Interventions included extractions, immediate implants, PRF
[...] Read more.
Background and Clinical Significance: This case presents immediate implant placement combined with PRF (A-PRF+) and a photogrammetry-based workflow, illustrating predictable full-arch implant-supported rehabilitation. Case Presentation: Main clinical findings included compromised abutment teeth and patient dissatisfaction with aesthetics. Interventions included extractions, immediate implants, PRF socket management, and digital provisional and definitive restorations. Outcomes demonstrated stable occlusion, satisfactory aesthetics, and high patient satisfaction. Conclusions: Immediate placement with PRF and photogrammetry provides reliable outcomes in complex full-arch cases.
Full article

Figure 1
Open AccessCase Report
Statin-Associated Headache: A Rare and Underrecognized Clinical Presentation: A Case Report
by
Mohammad. I. Ullah and Sadeka Tamanna
Reports 2026, 9(1), 7; https://doi.org/10.3390/reports9010007 - 24 Dec 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: Statins are widely prescribed for cardiovascular risk reduction and generally demonstrate a favorable safety profile. While myalgia and elevations in liver enzymes are well-recognized adverse effects, headaches are less commonly reported and often underrecognized in clinical practice.
[...] Read more.
Background and Clinical Significance: Statins are widely prescribed for cardiovascular risk reduction and generally demonstrate a favorable safety profile. While myalgia and elevations in liver enzymes are well-recognized adverse effects, headaches are less commonly reported and often underrecognized in clinical practice. This may result in unnecessary diagnostic evaluations, increased healthcare costs, and delayed identification of the underlying cause. Case Presentation: We describe an adult patient who developed intractable headaches that emerged after many years of statin therapy. The headaches persisted despite conventional analgesic treatment and resolved completely following discontinuation of the statin. Secondary causes were excluded, and comorbid conditions were systematically ruled out. Statin-associated headache is uncommon but clinically relevant. Proposed mechanisms include nitric-oxide-mediated vasodilation, central effects of lipophilic statins, and mitochondrial involvement. In this case, the patient was taking metoprolol succinate, lisinopril, simvastatin, clopidogrel, and tamsulosin. Except for lisinopril, none of the other comedications are strongly linked to new-onset headaches. Holding it did not resolve his headache, making simvastatin the most plausible contributor. This was confirmed by resolution of headache through its discontinuation. Because such headaches may be overlooked, clinicians should consider a statin-related cause when symptoms begin after initiation and may manage this by switching to a hydrophilic statin or using alternative lipid-lowering therapy. Conclusions: Clinicians should remain vigilant about the possibility of statin-induced headache, even in long-term users. Early recognition can prevent unnecessary diagnostic investigations, expedite symptom resolution, and support optimal management of both cardiovascular risk and treatment-related adverse effects.
Full article

Figure 1
Open AccessCase Report
Analysis of the Temporo-Spatial and Electromyographic Characteristics of Gait in a Hemiplegic Patient: A Single-Subject Case Report
by
Nohra Fernanda Nuñez Molano, Daniela Scarpetta Castrillon and Florencio Arias Coronel
Reports 2026, 9(1), 6; https://doi.org/10.3390/reports9010006 - 24 Dec 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: Hemiplegia following a cerebrovascular accident (CVA) disrupts gait symmetry and efficiency, compromising functional independence. The integration of surface electromyography (sEMG) and inertial measurement units (IMU) enables quantitative assessment of muscle activation and segmental dynamics, providing objective data for therapeutic
[...] Read more.
Background and Clinical Significance: Hemiplegia following a cerebrovascular accident (CVA) disrupts gait symmetry and efficiency, compromising functional independence. The integration of surface electromyography (sEMG) and inertial measurement units (IMU) enables quantitative assessment of muscle activation and segmental dynamics, providing objective data for therapeutic planning. Case presentation: A 57-year-old male with chronic right hemiplegia, eight years post-ischemic stroke of the left middle cerebral artery. The patient ambulated independently without assistive devices, exhibiting right lower-limb circumduction. Clinical assessment revealed the following scores: Barthel Index 85/100, Tinetti Performance-Oriented Mobility Assessment (POMA) 16/28, Timed Up and Go (TUG) test 13 s, and Modified Ashworth Scale (MAS) scores of 1 (upper limb) and 1+ (lower limb). Methods: Multichannel sEMG (Miotool 800®, 8 channels) was recorded form the lumbar erectors, gluteus medius and maximus, vastus medialis, vastus intermedius, vastus lateralis, biceps femoris, tibialis anterior, medial gastrocnemius, and lateral gastrocnemius. Ag/AgCI electrodes were positioned according to SENIAM recommendations: sampling rate: 1000 Hz; band-pass filter: 20–500 Hz; notch filter: 60 Hz; normalization to %MVC. Simultaneously, IMU signals (Xsens DOT®, 60 Hz) were collected from both ankles during slow, medium and fast walking (20 s each) and compared with a healthy control subject. Results: The patient exhibited reduced sEMG amplitude and increased peak irregularity on the affected side, particularly in the gluteus medius, tibialis anterior, and gastrocnemius, along with agonist desynchronication. IMU data revealed decreased range of motion and angular pattern irregularity, with inconsistent acceleration peaks in the right ankle compared to the control, confirming neuromuscular and kinematic asymmetry. Conclusions: The combined sEMG-IMU analysis identified deficits in selective motor control and propulsion on the affected hemibody, providing essential information to guide physiotherapeutic interventions targeting pelvic stability, dorsiflexion, and propulsive phase training, enabling objective follow-up beyond specialized laboratory settings.
Full article

Figure 1
Open AccessCase Report
An 8-Year-Old Female with Giardiasis-Associated Henoch–Schönlein Purpura: A Case Report and Literature Review
by
Konstantinos Miliordos, Dimitrios Kapnisis, Christodoulos Chatzigrigoriadis, Emmanouil Koufopoulos, Sokratis Tsantiris, Aris Bertzouanis, Eirini Kostopoulou and Despoina Gkentzi
Reports 2026, 9(1), 5; https://doi.org/10.3390/reports9010005 - 22 Dec 2025
Abstract
Background and Clinical Significance: Henoch–Schönlein purpura (HSP), also known as Immunoglobulin A (IgA) vasculitis (IgAV), is a common systemic vasculitis in children characterized by palpable purpura, abdominal pain, and joint and kidney involvement. While respiratory tract viral or bacterial infections are the most
[...] Read more.
Background and Clinical Significance: Henoch–Schönlein purpura (HSP), also known as Immunoglobulin A (IgA) vasculitis (IgAV), is a common systemic vasculitis in children characterized by palpable purpura, abdominal pain, and joint and kidney involvement. While respiratory tract viral or bacterial infections are the most common causes of HSP, parasitic infections, such as giardiasis, are occasionally reported. Giardia lamblia is the most common parasite infecting humans and a major cause of infectious diarrhea, which can lead to post-infection complications. To our knowledge, this is the first report in Greece describing a pediatric patient with HSP secondary to giardiasis. A review of pediatric HSP cases caused by parasitic infections is also included. Case presentation: An 8-year-old girl presented with a purpuric rash, joint tenderness, severe abdominal pain, and bloody diarrhea, raising suspicion of HSP. Laboratory tests revealed elevated IgA levels, and stool analysis tested positive for Giardia lamblia antigen. The diagnosis of HSP secondary to giardiasis was confirmed, and the patient was successfully treated with supportive care, metronidazole, and corticosteroids. Conclusion: This case report and literature review highlight parasitic infections as an underrecognized but important trigger of pediatric HSP. Although giardiasis is linked to various post-infectious complications, its association with HSP is rarely reported. Pediatricians should maintain a high level of suspicion for underlying infectious diarrhea, such as giardiasis, in patients with HSP, especially in children with prominent gastrointestinal symptoms. Early recognition can reduce complications and facilitate faster recovery. Further research is needed for the immunopathogenic mechanisms linking parasitic infections and HSP in children.
Full article
(This article belongs to the Section Allergy/Immunology)
►▼
Show Figures

Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Pharmaceuticals, Medical Sciences, JCM, Vision, Reports, Cells, IJMS
New Developments in Glaucoma Diagnostics and Therapeutics
Topic Editors: Shan C. Lin, Sunee ChansangpetchDeadline: 30 September 2026
Topic in
Brain Sciences, JCM, Healthcare, Reports, Information, NeuroSci
Applications of Virtual Reality Technology in Rehabilitation—2nd Edition
Topic Editors: Jorge Oliveira, Pedro GamitoDeadline: 30 November 2026
Topic in
Biomedicines, Diseases, JCM, JPM, Uro, Reports
Clinical, Translational, and Basic Research and Novel Therapy on Functional Bladder Diseases and Lower Urinary Tract Dysfunctions
Topic Editors: Hann-Chorng Kuo, Yao-Chi Chuang, Chun-Hou LiaoDeadline: 31 December 2026

Special Issues
Special Issue in
Reports
Artificial Intelligence in Clinical Medicine—Transforming Patient Care Through Innovation
Guest Editors: Ryo Ozuru, Yuji Oyamada, Toshio HattoriDeadline: 31 January 2026
Special Issue in
Reports
Epidemiology of Infectious Diseases: Time-Series Analysis and Nonlinear Dynamics
Guest Editor: Ayako SumiDeadline: 30 June 2026
Topical Collections
Topical Collection in
Reports
Health Threats of Climate Change
Collection Editors: Toshio Hattori, Yujiro Nakayama, Hiromu Ito, Kenzo Takahashi, Ayako Sumi, Takatoshi Kasai, Ichiro Onoyama, Shigeru Morinobu
Topical Collection in
Reports
Cardiovascular Disease and Sleep Disordered Breathing—Case Report
Collection Editor: Takatoshi Kasai