Trousseau’s Syndrome and Marantic Endocarditis in a Patient with Pulmonary Adenocarcinoma: A Case Report and a Brief Review of the Literature
Abstract
1. Introduction and Clinical Significance
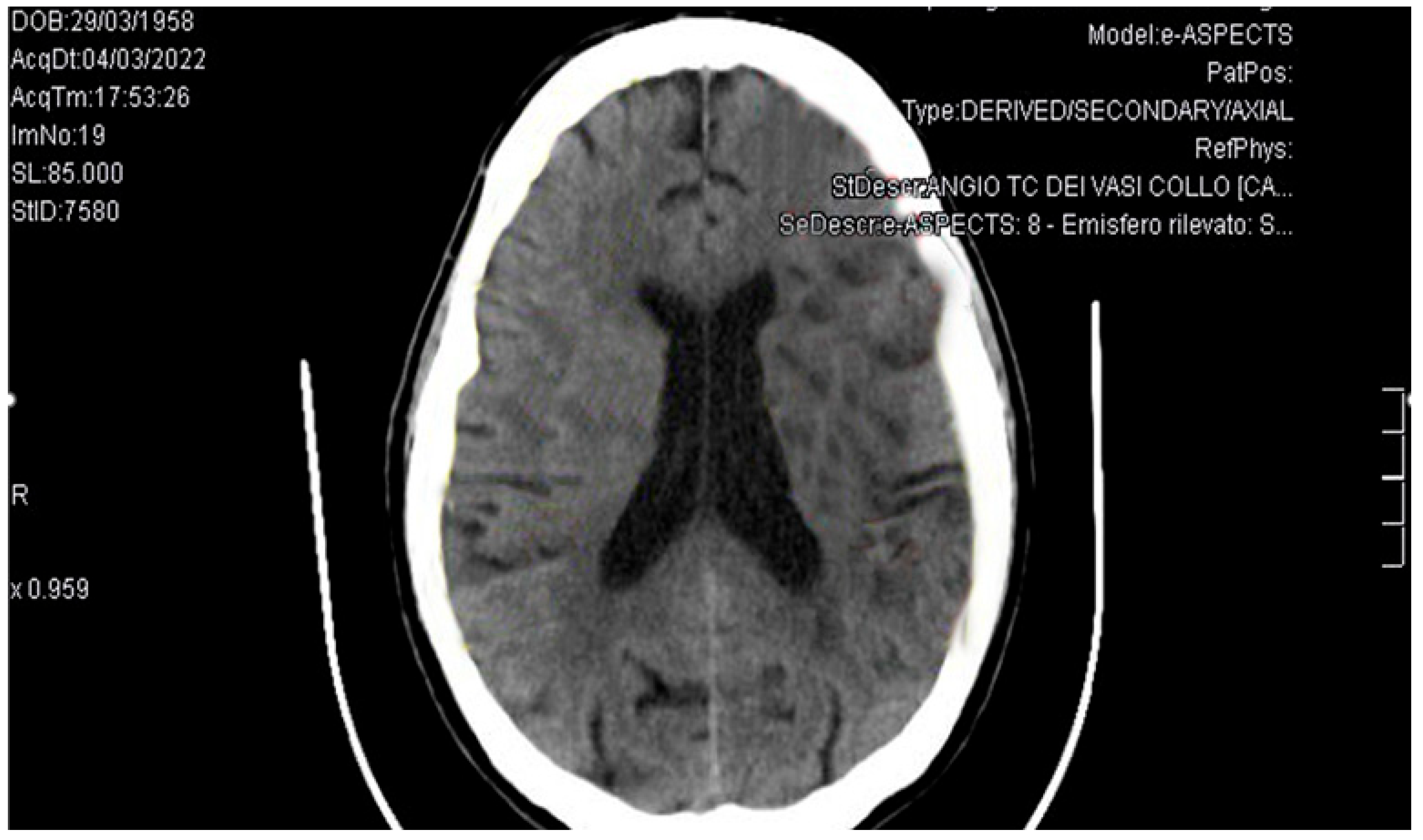
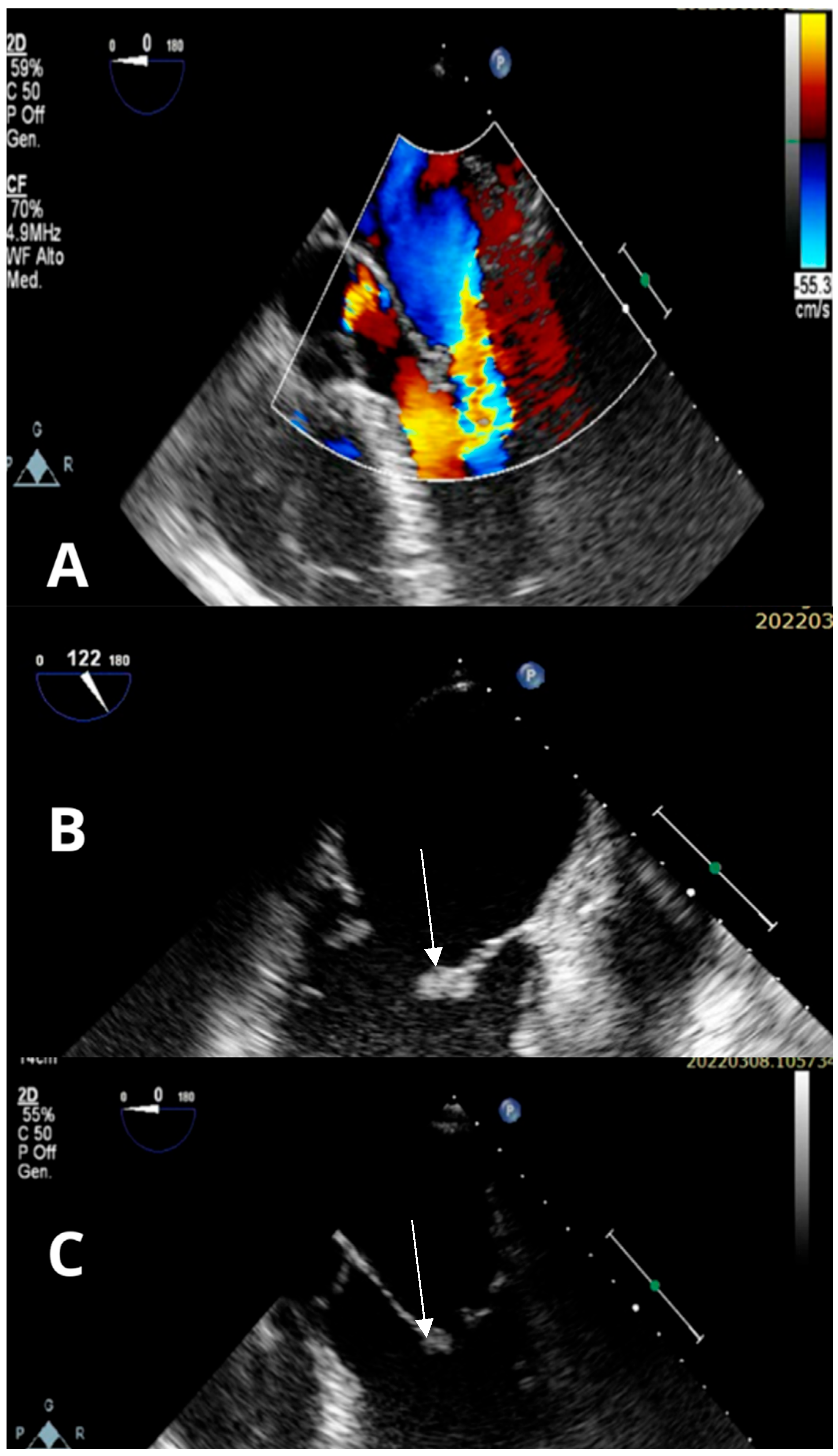
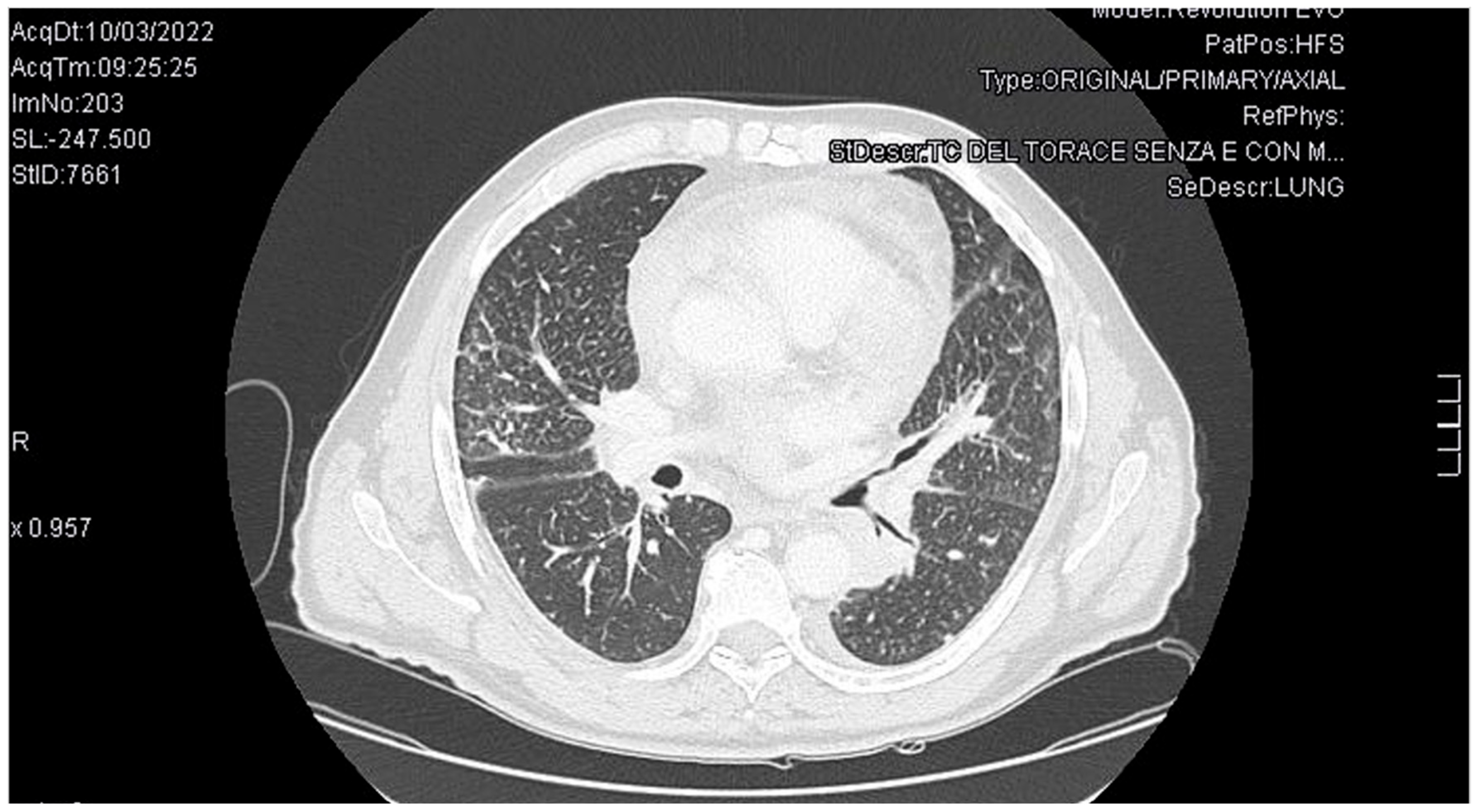
2. Case Presentation
3. Discussion
| Therapy | Indications | Advantages | Limitations/Contraindications |
|---|---|---|---|
| Low Molecular Weight Heparin (LMWH) | First-line for treatment and prevention of VTE in cancer patients. | Proven efficacy, reduced VTE vs. warfarin, easy dosing | Injection route, bleeding risk, impaired renal function. |
| Direct Oral Anticoagulants (DOACs) (edoxaban, rivaroxaban, apixaban) | Alternative to LMWH in selected patients. | Oral administration, non-inferior efficacy. Apixaban does not increase bleeding risk. | Avoid in unresected GI/GU cancers, CrCl < 15, platelets < 50 k, recent surgery, bleeding risk |
| Vitamin K Antagonists (VKAs) | Alternative if DOACs/LMWH not suitable | Oral, long experience | Drug–food interactions, INR monitoring required, less preferred |
| Unfractionated Heparin (UFH) | Hospitalized patients, rapid reversal needed | Short half-life, reversible | Requires monitoring (aPTT), IV route |
| Anticoagulation Duration | ≥6 months recommended (individualized) | Reduces recurrence | Reassess bleeding periodically, especially in advanced cancer |
4. Conclusions and Take-Home Messages
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ANA | antinuclear antibodies |
| ASCO | American Society of Clinical Oncology |
| CAT | Cancer associated thromboses |
| CRP | C-reactive protein |
| CVC | Central Venous Catheter |
| DDIs | drug–drug interactions |
| DOAC | Direct oral anticoagulant |
| ED | Emergency department |
| ENA | extractable nuclear antigens |
| ESC | European Society of Cardiology |
| EEU | Enzyme-Linked Immunosorbent Assay Equivalent Units |
| GI | gastrointestinal |
| GU | genitourinary |
| ICI | immune checkpoint inhibitor |
| LMWH | low-molecular-weight heparin |
| NBTE | non-bacterial thrombotic endocarditis |
| NIHSS | National Institutes of Health Stroke Scale |
| PAI-1 | plasminogen activator inhibitor |
| PE | pulmonary embolism |
| PICC | peripherally inserted central catheter |
| P-gp | P-glycoprotein |
| TF | tissue factor |
| TKIs | tyrosine kinase inhibitors |
| TEE | transesophageal echocardiogram |
| TTE | Transthoracic echocardiography |
| UFH | unfractionated heparin |
| VKA | vitamin K antagonists |
| VTE | venous thromboembolism |
| WBC | white blood cell |
References
- Lyon, A.R.; López-Fernández, T.; Couch, L.S.; Asteggiano, R.; Aznar, M.C.; Bergler-Klein, J.; Boriani, G.; Cardinale, D.; Cordoba, R.; Cosyns, B.; et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur. Heart J. 2022, 43, 4229–4361. [Google Scholar] [CrossRef]
- Mulder, F.I.; Carrier, M.; van Doormaal, F.; Robin, P.; Otten, H.M.; Salaun, P.Y.; Büller, H.R.; Le Gal, G.; van Es, N. Risk scores for occult cancer in patients with unprovoked venous thromboembolism: Results from an individual patient data meta-analysis. J. Thromb. Haemost. 2020, 18, 2622–2628. [Google Scholar] [CrossRef]
- Trousseau, A. Lectures on Clinical Medicine; The New Sydenham Society: London, UK, 1868; Volume 5, pp. 281–331. [Google Scholar]
- Varki, A. Trousseau’s syndrome: Multiple definitions and multiple mechanisms. Blood 2007, 110, 1723–1729. [Google Scholar] [CrossRef]
- Yoshimine, K.; Tobino, K.; Obata, Y.; Sogabe, S.; Uchida, K.; Murakami, Y.; Yamamoto, R. Trousseau’s Syndrome in Lung Cancer Patients: A Retrospective Study in a Japanese Community Hospital. Cureus 2024, 16, e68400. [Google Scholar] [CrossRef] [PubMed]
- Brice, P.; Bastion, Y.; Lepage, E.; Brousse, N.; Haioun, C.; Moreau, P.; Straetmans, N.; Tilly, H.; Tabah, I.; Solal-Céligny, P. Comparison in Low-Tumor-Burden Follicular Lymphomas Between an Initial No-Treatment Policy, Prednimustine, or Interferon Alfa: A Randomized Study From the Groupe D’Etude Des Lymphomes Folliculaires. J. Clin. Oncol. 1997, 15, 1110–1117. [Google Scholar] [CrossRef]
- Delgado, V.; Ajmone Marsan, N.; de Waha, S.; Bonaros, N.; Brida, M.; Burri, H.; Caselli, S.; Doenst, T.; Ederhy, S.; Erba, P.A.; et al. 2023 ESC Guidelines for the management of endocarditis. Eur. Heart J. 2023, 44, 3948–4042. [Google Scholar] [CrossRef]
- Lee, A.Y.Y.; Levine, M.N.; Baker, R.I.; Bowden, C.; Kakkar, A.K.; Prins, M.; Rickles, F.R.; Julian, J.A.; Haley, S.; Kovacs, M.J.; et al. Low-Molecular-Weight Heparin versus a Coumarin for the Prevention of Recurrent Venous Thromboembolism in Patients with Cancer. N. Engl. J. Med. 2003, 349, 146–153. [Google Scholar] [CrossRef]
- Woodruff, S.; Lee, A.Y.Y.; Carrier, M.; Feugère, G.; Abreu, P.; Heissler, J. Low-molecular-weight-heparin versus a coumarin for the prevention of recurrent venous thromboembolism in high- and low-risk patients with active cancer: A post hoc analysis of the CLOT Study. J. Thromb. Thrombolysis 2019, 47, 495–504. [Google Scholar] [CrossRef]
- Raskob, G.E.; van Es, N.; Verhamme, P.; Carrier, M.; Di Nisio, M.; Garcia, D.; Grosso, M.A.; Kakkar, A.K.; Kovacs, M.J.; Mercuri, M.F.; et al. Edoxaban for the Treatment of Cancer-Associated Venous Thromboembolism. N. Engl. J. Med. 2018, 378, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Young, A.M.; Marshall, A.; Thirlwall, J.; Chapman, O.; Lokare, A.; Hill, C.; Hale, D.; Dunn, J.A.; Lyman, G.H.; Hutchinson, C.; et al. Comparison of an Oral Factor Xa Inhibitor With Low Molecular Weight Heparin in Patients With Cancer With Venous Thromboembolism: Results of a Randomized Trial (SELECT-D). J. Clin. Oncol. 2018, 36, 2017–2023. [Google Scholar] [CrossRef] [PubMed]
- Agnelli, G.; Becattini, C.; Meyer, G.; Muñoz, A.; Huisman, M.V.; Connors, J.M.; Cohen, A.; Bauersachs, R.; Brenner, B.; Torbicki, A.; et al. Apixaban for the Treatment of Venous Thromboembolism Associated with Cancer. N. Engl. J. Med. 2020, 382, 1599–1607. [Google Scholar] [CrossRef]
- Key, N.S.; Khorana, A.A.; Kuderer, N.M.; Bohlke, K.; Lee, A.Y.; Arcelus, J.I.; Wong, S.L.; Balaban, E.P.; Flowers, C.R.; Gates, L.E.; et al. Venous Thromboembolism Prophylaxis and Treatment in Patients With Cancer: ASCO Guideline Update. J. Clin. Oncol. 2023, 41, 2373–2390. [Google Scholar] [CrossRef]
- Mahé, I.; Carrier, M.; Mayeur, D.; Chidiac, J.; Vicaut, E.; Falvo, N.; Sanchez, O.; Grange, C.; Monreal, M.; López-Núñez, J.J.; et al. Extended Reduced-Dose Apixaban for Cancer-Associated Venous Thromboembolism. N. Engl. J. Med. 2025, 392, 1363–1373. [Google Scholar] [CrossRef]
- Key, N.S.; Khorana, A.A.; Kuderer, N.M.; Bohlke, K.; Lee, A.Y.; Arcelus, J.I.; Wong, S.L.; Balaban, E.P.; Flowers, C.R.; Francis, C.W.; et al. Venous Thromboembolism Prophylaxis and Treatment in Patients With Cancer: ASCO Clinical Practice Guideline Update. J. Clin. Oncol. 2019, 38, 496–520. [Google Scholar] [CrossRef]
- Khorana, A.A.; Kuderer, N.M.; Culakova, E.; Lyman, G.H.; Francis, C.W. Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 2008, 111, 4902–4907. [Google Scholar] [CrossRef]
- De Winter, M.A.; Dorresteijn, J.A.N.; Ageno, W.; Ay, C.; Beyer-Westendorf, J.; Coppens, M.; Klok, F.A.; Moustafa, F.; Riva, N.; Artacho, P.C.R.; et al. Estimating Bleeding Risk in Patients with Cancer-Associated Thrombosis: Evaluation of Existing Risk Scores and Development of a New Risk Score. Thromb. Haemost. 2022, 122, 818–829. [Google Scholar] [CrossRef]
- Wan, T.; Song, J.; Zhu, D. Cancer-associated venous thromboembolism: A comprehensive review. Thromb. J. 2025, 23, 35. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, H.T.; Mellemkjaer, L.; Olsen, J.H.; Baron, J.A. Prognosis of cancers associated with venous thromboembolism. N. Engl. J. Med. 2000, 343, 1846–1850. [Google Scholar] [CrossRef] [PubMed]
- Lobato-Delgado, B.; Ruiz, M.; Fonte, C.; Pachón, V.; Castellón, V.; Martínez-Marín, V.; Salgado, M.; Martínez, E.; Calzas, J.; Ortega, L.; et al. Cancer-associated venous thromboembolism and its impact on survival in the ONCOTHROMB12-01 cohort study. IJC Heart Vasc. 2025, 60, 101754. [Google Scholar] [CrossRef] [PubMed]
- Ikushima, S.; Ono, R.; Fukuda, K.; Sakayori, M.; Awano, N.; Kondo, K. Trousseau’s syndrome: Cancer-associated thrombosis. Jpn. J. Clin. Oncol. 2016, 46, 204–208. [Google Scholar] [CrossRef]
- Wrzeszcz, K.; Rhone, P.; Kwiatkowska, K.; Ruszkowska-Ciastek, B. Hypercoagulability State Combined with Post-Treatment Hypofibrinolysis in Invasive Breast Cancer: A Seven-Year Follow-Up Evaluating Disease-Free and Overall Survival. Life 2023, 13, 1106. [Google Scholar] [CrossRef]
- Fioretti, A.M.; Scicchitano, P.; La Forgia, D.; De Luca, R.; Campello, E.; Tocchetti, C.G.; Di Nisio, M.; Oliva, S. Drug-Drug Interactions of Direct Oral Anticoagulants (DOACs): From Pharmacological to Clinical Practice. Pharmaceutics 2022, 14, 1120. [Google Scholar] [CrossRef]
- Fioretti, A.M.; Scicchitano, P.; La Forgia, D.; De Luca, R.; Campello, E.; Tocchetti, C.G.; Di Nisio, M.; Oliva, S. Prevention of Peripherally Inserted Central Catheter (PICC)-Associated Vein Thrombosis in Cancer: A Narrative Review. Biomedicines 2025, 13, 786. [Google Scholar] [CrossRef]
- Toda, Y.; Kano, Y. Three-territory sign in Trousseau’s syndrome. BMJ Case Rep. 2022, 15, e250640. [Google Scholar] [CrossRef]
- Sanfilippo, K.M.; Wang, T.F.; Gage, B.F.; Luo, S.; Riedell, P.; Carson, K.R. Incidence of Venous Thromboembolism in Patients with Non-Hodgkin Lymphoma. Thromb. Res. 2016, 143, 86–90. [Google Scholar] [CrossRef]
- Ahmed, O.; King, N.E.; Qureshi, M.A.; Choudhry, A.A.; Osama, M.; Zehner, C.; Ali, A.; Hamzeh, I.R.; Palaskas, N.L.; Thompson, K.A.; et al. Non-bacterial thrombotic endocarditis: A clinical and pathophysiological reappraisal. Eur. Heart J. 2025, 46, 236–249. [Google Scholar] [CrossRef]
- Lee, Z.X.; Cheng, J.O.S.; Sharip, M.T.; Hlaing, H.H.; Allison, M. Trousseau’s syndrome with non-bacterial thrombotic endocarditis (NBTE) in a patient with advanced pancreatic cancer. Clin. Med. 2023, 23, 36–37. [Google Scholar] [CrossRef]
- Celeng, C.; Takx, R.A.P. Cancer-associated marantic endocarditis: A rare but relevant complication. Eur. Heart J. Cardiovasc. Imaging 2023, 24, 1627–1628. [Google Scholar] [CrossRef] [PubMed]
- Pengo, V.; Denas, G.; Zoppellaro, G.; Jose, S.P.; Hoxha, A.; Ruffatti, A.; Andreoli, L.; Tincani, A.; Cenci, C.; Prisco, D.; et al. Rivaroxaban vs. Warfarin in High-Risk Patients with Antiphospholipid Syndrome. Blood 2018, 132, 1365–1371. [Google Scholar] [CrossRef] [PubMed]
- Zmaili, M.; Alzubi, J.; Lo Presti Vega, S.; Ababneh, E.; Xu, B. Non-bacterial thrombotic endocarditis: A state-of-the-art contemporary review. Prog. Cardiovasc. Dis. 2022, 74, 99–110. [Google Scholar] [CrossRef]
| Parameter | Result at Admission | Reference Range |
|---|---|---|
| WBC count | 9670/μL | 4000–10,000/μL |
| Hemoglobin | 11 g/dL | 13–17 g/dL |
| Platelet count | 170,000/μL | 150,000–400,000/μL |
| D-dimer | 21,268 EEU | 0–500 EEU |
| Serum creatinine | 0.76 mg/dL | 0.6–1.2 mg/dL |
| CRP | Negative | Negative |
| ANA, ENA, Anticardiolipin antibodies, β2-microglobulin | Negative | Negative |
| Category | Risk Factors |
|---|---|
| Patient-related | Older age, immobility, comorbidities (e.g., hypertension), history of thrombosis |
| Tumor-related | Histological type (especially adenocarcinoma), tumor burden, metastasis |
| Biological mediators | Tissue factor (TF), mucins, PAI-1, cytokines, hypoxia |
| Treatment-related | Chemotherapy (e.g., platinum compounds), hormonal therapy, antiangiogenics |
| Drug interactions | DOAC metabolism affected by CYP3A4/P-gp inhibitors (e.g., tyrosine kinase inhibitors) |
| Procedural | Central venous catheters (CVCs), recent surgery |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cosco, L.; Padeletti, M.; Sorrentino, A.; Milli, M.; Marcucci, R. Trousseau’s Syndrome and Marantic Endocarditis in a Patient with Pulmonary Adenocarcinoma: A Case Report and a Brief Review of the Literature. Reports 2025, 8, 215. https://doi.org/10.3390/reports8040215
Cosco L, Padeletti M, Sorrentino A, Milli M, Marcucci R. Trousseau’s Syndrome and Marantic Endocarditis in a Patient with Pulmonary Adenocarcinoma: A Case Report and a Brief Review of the Literature. Reports. 2025; 8(4):215. https://doi.org/10.3390/reports8040215
Chicago/Turabian StyleCosco, Leandro, Margherita Padeletti, Andrea Sorrentino, Massimo Milli, and Rossella Marcucci. 2025. "Trousseau’s Syndrome and Marantic Endocarditis in a Patient with Pulmonary Adenocarcinoma: A Case Report and a Brief Review of the Literature" Reports 8, no. 4: 215. https://doi.org/10.3390/reports8040215
APA StyleCosco, L., Padeletti, M., Sorrentino, A., Milli, M., & Marcucci, R. (2025). Trousseau’s Syndrome and Marantic Endocarditis in a Patient with Pulmonary Adenocarcinoma: A Case Report and a Brief Review of the Literature. Reports, 8(4), 215. https://doi.org/10.3390/reports8040215






