Partial Androgen Insensitivity Syndrome and Congenital Adrenal Hyperplasia—A Case Report of the Coexistence of Two Rare Diseases in One Patient
Abstract
1. Introduction and Clinical Significance
2. Case Presentation
2.1. Neonatal Period
2.2. Infant
2.3. Childhood
2.4. Adolescence
2.5. Adulthood
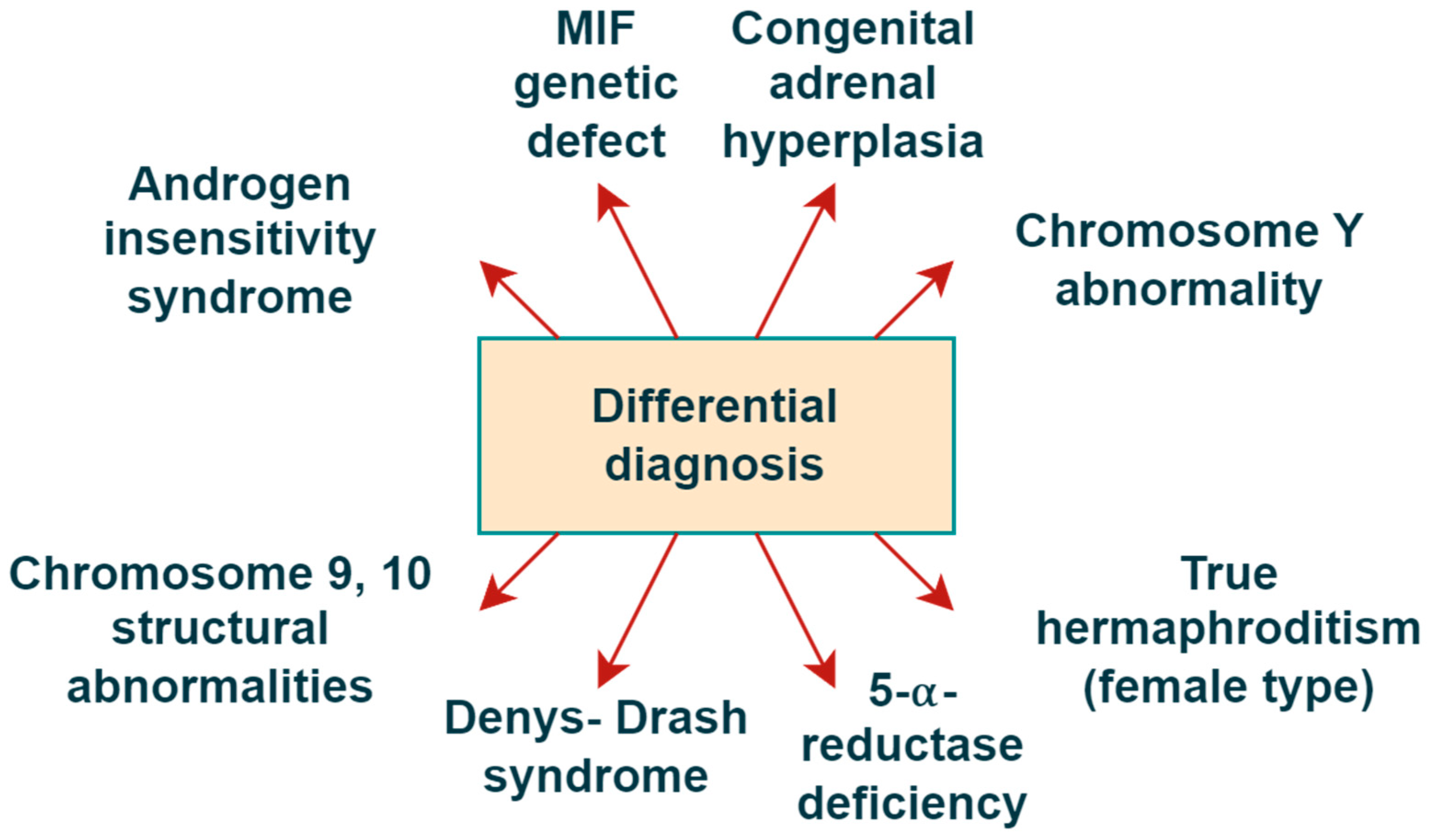
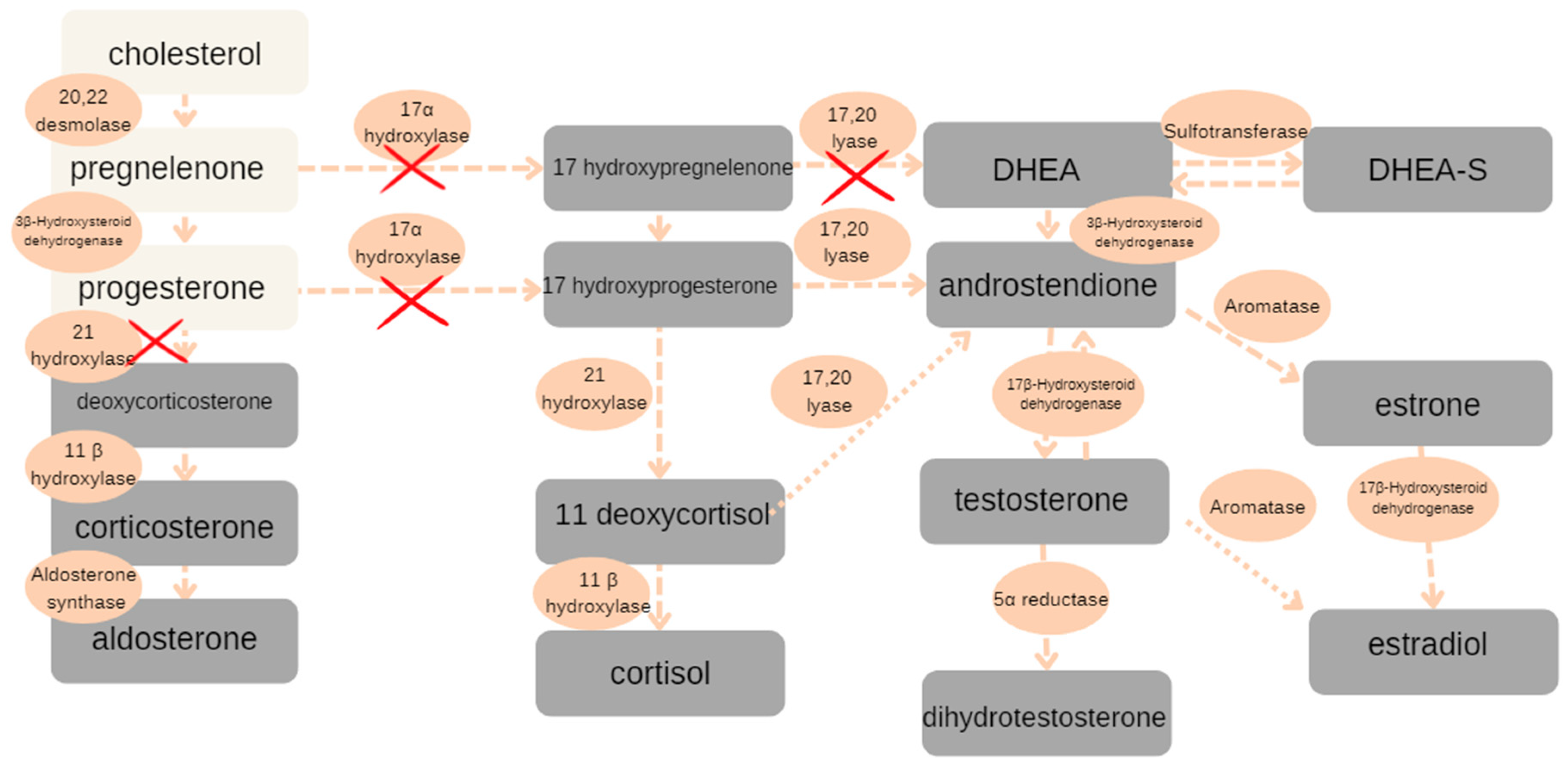
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hughes, I.A.; Houk, C.; Ahmed, S.F.; Lee, P.A. Consensus statement on management of intersex disorders. J. Pediatr. Urol. 2006, 2, 148–162. [Google Scholar] [CrossRef]
- Ono, H.; Saitsu, H.; Horikawa, R.; Nakashima, S.; Ohkubo, Y.; Yanagi, K.; Nakabayashi, K.; Fukami, M.; Fujisawa, Y.; Ogata, T. Partial androgen insensitivity syndrome caused by a deep intronic mutation creating an alternative splice acceptor site of the AR gene. Sci. Rep. 2018, 8, 2287. [Google Scholar] [CrossRef]
- Galani, A.; Kitsiou-Tzeli, S.; Sofokleous, C.; Kanavakis, E.; Kalpini-Mavrou, A. Androgen insensitivity syndrome: Clinical features and molecular defects. Hormones 2008, 7, 217–229. [Google Scholar] [CrossRef] [PubMed]
- Chávez, B.; Méndez, J.P.; Ulloa-Aguirre, A.; Larrea, F.; Vilchis, F. Eight novel mutations of the androgen receptor gene in patients with androgen insensitivity syndrome. J. Hum. Genet. 2001, 46, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Bevan, C.L.; Brown, B.B.; Davies, H.R.; Evans, B.A.; Hughes, I.A.; Patterson, M.N. Functional analysis of six androgen receptor mutations identified in patients with partial androgen insensitivity syndrome. Hum. Mol. Genet. 1996, 5, 265–273. [Google Scholar] [CrossRef]
- Berglund, A.; Johannsen, T.H.; Stochholm, K.; Viuff, M.H.; Fedder, J.; Main, K.M.; Gravholt, C.H. Incidence, prevalence, diagnostic delay, and clinical presentation of female 46, XY disorders of sex development. J. Clin. Endocrinol. Metab. 2016, 101, 4532–4540. [Google Scholar] [CrossRef]
- Fraga, N.R.; Minaeian, N.; Kim, M.S. Congenital Adrenal Hyperplasia. Pediatr. Rev. 2024, 45, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Ovidiu, B.; Marcu, D.R.; Mischianu, D.L.; Poiana, C.; Diaconu, C.C.; Bungau, S.G.; Tit, D.M.; Cumpanas, A.; Bohiltea, R. The challenges of androgen insensitivity syndrome. Arch. Med. Sci. 2022, 18, 881. [Google Scholar] [CrossRef]
- Guaragna-Filho, G.; Castro, C.C.T.D.S.; De Carvalho, R.R.; Coeli, F.B.; Ferraz, L.F.C.; Petroli, R.J.; De Mello, M.P.; Sewaybricker, L.E.; Lemos-Marini, S.H.V.; D’Souza-Li, L.F.R.; et al. 46, XX DSD and Antley-Bixler syndrome due to novel mutations in the cytochrome P450 oxidoreductase gene. Arq. Bras. De Endocrinol. Metabol. 2012, 56, 578–585. [Google Scholar] [CrossRef]
- Giwercman, Y.L.; Nordenskjöld, A.; Ritzén, E.M.; Nilsson, K.O.; Ivarsson, S.A.; Grandell, U.; Wedell, A. An androgen receptor gene mutation (E653K) in a family with congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency as well as in partial androgen insensitivity. J. Clin. Endocrinol. Metab. 2002, 87, 2623–2628. [Google Scholar] [CrossRef]
- Miller, W.L. Mechanisms in Endocrinology: Rare defects in adrenal steroidogenesis. Eur. J. Endocrinol. 2018, 179, R125–R141. [Google Scholar] [CrossRef]
- Nguyen, L.S.; Prifti, E.; Ichou, F.; Leban, M.; Funck-Brentano, C.; Touraine, P.; Salem, J.E.; Bachelot, A. Effect of congenital adrenal hyperplasia treated by glucocorticoids on plasma metabolome: A machine-learning-based analysis. Sci. Rep. 2020, 10, 8859. [Google Scholar] [CrossRef]
- Krone, N.; Hanley, N.A.; Arlt, W. Age-specific changes in sex steroid biosynthesis and sex development. Best Pract. Res. Clin. Endocrinol. Metab. 2007, 21, 393–401. [Google Scholar] [CrossRef]
- Miller, W.L. Disorders of androgen synthesis—From cholesterol to dehydroepiandrosterone. Med. Princ. Pract. 2005, 14, 58–68. [Google Scholar] [CrossRef]
- Fluck, C.; Pandey, A.; Huang, N.; Agrawal, V.; Miller, W. P450 oxidoreductase deficiency—A new form of congenital adrenal hyperplasia. Endocr. Dev. 2008, 13, 67. [Google Scholar] [CrossRef]
- Dean, B.; Chrisp, G.L.; Quartararo, M.; Maguire, A.M.; Hameed, S.; King, B.R.; Munns, C.F.; Torpy, D.J.; Falhammar, H.; Rushworth, R.L. P450 Oxidoreductase Deficiency: A Systematic Review and Meta-analysis of Genotypes, Phenotypes, and Their Relationships. J. Clin. Endocrinol. Metab. 2020, 105, e42–e52. [Google Scholar] [CrossRef]
- Batista, R.L.; Costa, E.M.F.; Rodrigues, A.D.S.; Gomes, N.L.; Faria, J.A., Jr.; Nishi, M.Y.; Arnhold, I.J.P.; Domenice, S.; Mendonca, B.B.D. Androgen insensitivity syndrome: A review. Arch. Endocrinol. Metab. 2018, 62, 227–235. [Google Scholar] [CrossRef]
- Thyen, U.; Lanz, K.; Holterhus, P.M.; Hiort, O. Epidemiology and initial management of ambiguous genitalia at birth in Germany. Horm. Res. 2006, 66, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Cools, M.; Nordenström, A.; Robeva, R.; Hall, J.; Westerveld, P.; Flück, C.; Köhler, B.; Berra, M.; Springer, A.; Schweizer, K.; et al. Caring for individuals with a difference of sex development (DSD): A Consensus Statement. Nat. Rev. Endocrinol. 2018, 14, 415–429. [Google Scholar] [CrossRef] [PubMed]
- Gusmano, C.; Cannarella, R.; Crafa, A.; Barbagallo, F.; La Vignera, S.; Condorelli, R.A.; Calogero, A.E. Congenital adrenal hyperplasia, disorders of sex development, and infertility in patients with POR gene pathogenic variants: A systematic review of the literature. J. Endocrinol. Investig. 2023, 46, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Stikkelbroeck, N.M.; Otten, B.J.; Pasic, A.; Jager, G.J.; Sweep, C.F.; Noordam, K.; Hermus, A.R. High prevalence of testicular adrenal rest tumors, impaired spermatogenesis, and Leydig cell failure in adolescent and adult males with congenital adrenal hyperplasia. J. Clin. Endocrinol. Metab. 2001, 86, 5721–5728. [Google Scholar] [CrossRef]
- Oelschlager, A.M.A.; Debiec, K. Vaginal Dilator Therapy: A Guide for Providers for Assessing Readiness and Supporting Patients Through the Process Successfully. J. Pediatr. Adolesc. Gynecol. 2019, 32, 354–358. [Google Scholar] [CrossRef]
- Bennecke, E.; Strandqvist, A.; De Vries, A.; Kreukels, B.P. Psychological support for individuals with differences of sex development (DSD). J. Psychosom. Res. 2024, 179, 111636. [Google Scholar] [CrossRef]
- Babu, R.; Shah, U. Gender identity disorder (GID) in adolescents and adults with differences of sex development (DSD): A systematic review and meta-analysis. J. Pediatr. Urol. 2021, 17, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Moleiro, C.; Pinto, N. Sexual orientation and gender identity: Review of concepts, controversies and their relation to psychopathology classification systems. Front. Psychol. 2015, 6, 1511. [Google Scholar] [CrossRef]
- Scheim, A.I.; Bauer, G.R. Sex and gender diversity among transgender persons in ontario, Canada: Results from a respondent-driven sampling survey. J. Sex Res. 2015, 52, 1–14. [Google Scholar] [CrossRef]
- Tang, X.Y.; Zhang, N.; Ding, J.X.; Hua, K.Q. Quality of life among postoperative patients with disorders of sex development: A long-term perspective. Int. J. Clin. Exp. Med. 2017, 10, 13760–13765. [Google Scholar]
- Ahmad, A.; Ayub, F.; Saleem, I.; Ahmad, N. Initial assessment of a child with suspected disorder of sex development. J. Pak. Med. Assoc. 2019, 69, 711–717. [Google Scholar] [PubMed]
- Hiort, O.; Marshall, L.; Bacia, A.; Bouteleux, M.; Wünsch, L. Differences of sex development in children and adolescents: Principles. diagnostics and management. Monatsschrift Kinderheilkd. 2019, 167, 598–606. [Google Scholar] [CrossRef]
- Alderson, J.; Hamblin, R.P.; Crowne, E.C. Psychological Care of Children and Families with Variations or Differences in Sex Development. Horm. Res. Paediatr. 2023, 96, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Bennecke, E.; Bernstein, S.; Lee, P.; van de Grift, T.C.; Nordenskjöld, A.; Rapp, M.; Simmonds, M.; Streuli, J.C.; Thyen, U.; Wiesemann, C. Early Genital Surgery in Disorders/Differences of Sex Development: Patients’ Perspectives. Arch. Sex Behav. 2021, 50, 913–923. [Google Scholar] [CrossRef]
- Mouriquand, P.D.; Gorduza, D.B.; Gay, C.L.; Meyer-Bahlburg, H.F.; Baker, L.; Baskin, L.S.; Bouvattier, C.; Braga, L.H.; Caldamone, A.C.; Duranteau, L.; et al. Surgery in disorders of sex development (DSD) with a gender issue: If (why), when, and how? J. Pediatr. Urol. 2016, 12, 139–149. [Google Scholar] [CrossRef]
- Bumbulienė, Ž.; Bužinskienė, D.; Banuškevičienė, G.; Šidlovska, E.; Preikšaitienė, E.; Utkus, A. Challenges in the Diagnosis of XY Differences of Sexual Development. Medicina 2022, 58, 1736. [Google Scholar] [CrossRef]
- Lee, P.A.; Nordenström, A.; Houk, C.P.; Ahmed, S.F.; Auchus, R.; Baratz, A.; Baratz Dalke, K.; Liao, L.M.; Lin-Su, K.; Mazur, T.; et al. Global Disorders of Sex Development Update since 2006: Perceptions, Approach and Care. Horm. Res. Paediatr. 2016, 85, 158–180. [Google Scholar] [CrossRef] [PubMed]
- Nordenström, A.; Ahmed, S.F.; van den Akker, E.; Blair, J.; Bonomi, M.; Brachet, C.; Broersen, L.H.A.; Claahsen-Van Der Grinten, H.L.; Dessens, A.B.; Gawlik, A.; et al. Pubertal induction and transition to adult sex hormone replacement in patients with congenital pituitary or gonadal reproductive hormone deficiency: An Endo-ERN clinical practice guideline. Eur. J. Endocrinol. 2022, 186, G9–G49. [Google Scholar] [CrossRef] [PubMed]
- Wisniewski, A.B.; Batista, R.L.; Costa, E.M.; Finlayson, C.; Sircili, M.H.P.; Dénes, F.T.; Domenice, S.; Mendonca, B.B. Management of 46, XY Differences/Disorders of Sex Development (DSD) throughout Life. Endocr. Rev. 2019, 40, 1547–1572. [Google Scholar] [CrossRef]
- Skordis, N.; Kyriakou, A.; Dror, S.; Mushailov, A.; Nicolaides, N.C. Gender dysphoria in children and adolescents: An overview. Hormones 2020, 19, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Baetens, L.; Dhondt, K. Psychosocial challenges and hormonal treatment in gender diverse children and adolescents. A narrative review. Int. J. Impot. Res. 2021, 33, 217–227. [Google Scholar] [CrossRef]


| Time (Days) | Testosterone (pg/mL) | Estradiol (pg/mL) | SHBG (nmol/L) | DHEA-SO4 (ng/mL) | Androstendione (ng/dL) |
|---|---|---|---|---|---|
| 1 | <50 | <5.5 | 141 | 92 | 12 |
| 3 | 621 | <5.5 | x | x | x |
| 5 | 532 | <5.5 | 139 | 121 | 10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krzyścin, M.; Brodowska, A.; Furtak, G.; Pietrzyk, D.; Zając, K.; Oder, B.; Przepiera, A.; Sowińska-Przepiera, E. Partial Androgen Insensitivity Syndrome and Congenital Adrenal Hyperplasia—A Case Report of the Coexistence of Two Rare Diseases in One Patient. Reports 2025, 8, 212. https://doi.org/10.3390/reports8040212
Krzyścin M, Brodowska A, Furtak G, Pietrzyk D, Zając K, Oder B, Przepiera A, Sowińska-Przepiera E. Partial Androgen Insensitivity Syndrome and Congenital Adrenal Hyperplasia—A Case Report of the Coexistence of Two Rare Diseases in One Patient. Reports. 2025; 8(4):212. https://doi.org/10.3390/reports8040212
Chicago/Turabian StyleKrzyścin, Mariola, Agnieszka Brodowska, Gabriela Furtak, Dominika Pietrzyk, Katarzyna Zając, Bartosz Oder, Adam Przepiera, and Elżbieta Sowińska-Przepiera. 2025. "Partial Androgen Insensitivity Syndrome and Congenital Adrenal Hyperplasia—A Case Report of the Coexistence of Two Rare Diseases in One Patient" Reports 8, no. 4: 212. https://doi.org/10.3390/reports8040212
APA StyleKrzyścin, M., Brodowska, A., Furtak, G., Pietrzyk, D., Zając, K., Oder, B., Przepiera, A., & Sowińska-Przepiera, E. (2025). Partial Androgen Insensitivity Syndrome and Congenital Adrenal Hyperplasia—A Case Report of the Coexistence of Two Rare Diseases in One Patient. Reports, 8(4), 212. https://doi.org/10.3390/reports8040212






