Will (Radio)Theranostics Hold Up in the 21st Century—and Why?
A topical collection in Pharmaceuticals (ISSN 1424-8247). This collection belongs to the section "Radiopharmaceutical Sciences".
Viewed by 1463Editors
Interests: radiopharmaceutical drug development; radiopharmaceutical sciences; medicinal radiochemistry; radionuclide theranostics; targeted endoradiotherapy; noninvasive molecular imaging; PET; SPECT
Special Issues, Collections and Topics in MDPI journals
Interests: nuclear medicine; radiochemistry; positron emission tomography; molecular imaging; radiopharmaceutical sciences; cancer; diabetes; fibrosis; drug development; inflammation
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
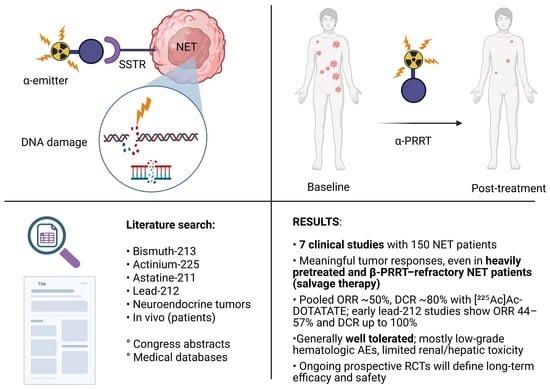
Modern theranostics is rapidly evolving and encompasses a variety of approaches that merge precision diagnostics with targeted therapies. This includes (radio)theranostics, which combines radionuclide imaging with radiotherapy or other therapeutic modalities. The therapies incorporate surgical interventions, pharmacological treatments, as well as exo- and endoradiotherapy.
As we stand at the intersection of diagnostic innovation and therapeutic advancement, the paradigm of (radio)theranostics is reshaping personalized medicine and challenging established clinical workflows. The field has experienced substantial growth over the past decade, driven by remarkable success in academically driven clinical studies targeting somatostatin receptors and prostate-specific membrane antigens. This progress has spurred prospective clinical trials and subsequently the commercialization of corresponding radiopharmaceuticals and the broader adoption of radiotheranostic technology. However, the future development of (radio)theranostics will be shaped by a complex interplay of factors, both advancing and challenging its continued evolution.
On one hand, these hybrid approaches are opening new avenues for individualized treatment, leveraging cutting-edge imaging technologies to precisely localize disease and tailor therapy to each patient’s unique profile. This convergence promises improved outcomes through more accurate diagnoses and optimized treatment strategies, reducing side effects and enhancing overall efficacy.
On the other hand, significant hurdles remain. The integration of diverse diagnostic modalities with multiple treatment forms raises complex issues related to technological compatibility, regulatory oversight, and economic feasibility. As the field broadens beyond traditional radionuclide applications, it demands robust infrastructure, interdisciplinary collaboration, and innovative research to fully realize its potential.
We invite authors to contribute their insights, critical analyses, and innovative perspectives on the future of modern theranostics. Whether your focus is on the continued development of radiopharmaceuticals and radionuclide production, the technical and technological advancements, clinical implications, or the regulatory and socio-economic challenges of integrating precision diagnostics with various therapeutic modalities, your contribution will help illuminate the multifaceted dynamics that will determine whether this paradigm can endure the tests of the 21st century.
Prof. Dr. Klaus Kopka
Dr. Irina Velikyan
Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Pharmaceuticals is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2900 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- (radio)theranostics
- precision imaging
- molecular imaging
- targeted (radio)therapies
- personalized medicine
- diagnostic innovation
- economic feasibility
- regulatory challenges
- interdisciplinary collaboration
- clinical adoption
- technological advancements
- socio-economic impact
- healthcare infrastructure
- diagnostic and therapeutic radionuclide production
- radiopharmaceutical development
- positron emission tomography
- single photon emission tomography
- dosimetry