- Systematic Review
Towards a Unified Terminology for Implant-Influenced Fractures: Implications for Musculoskeletal and Muscle–Implant Interaction Research
- Giacomo Papotto,
- Ignazio Prestianni and
- Rocco Ortuso
- + 7 authors
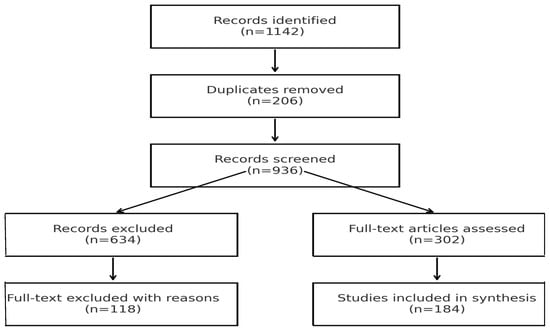
Background: The global increase in orthopedic implant use—both for trauma fixation and arthroplasty—has profoundly transformed musculoskeletal surgery. As a consequence, fractures occurring in the presence of implants have become more frequent and clinically relevant. Yet, these injuries are currently described using highly heterogeneous terminology, including periprosthetic (fracture occurring in the presence of a prosthetic joint replacement) peri-implant (fracture occurring around an osteosynthesis or fixation device), implant-related, and hardware-related fractures (umbrella terms encompassing both prosthetic and fixation devices, used descriptively rather than classificatorily). This coexistence of multiple, context-specific terminologies hinders clinical communication, complicates registry documentation, and limits research comparability across orthopedic subspecialties. Because fractures occurring in the presence of orthopedic implants significantly alter load transfer, muscle force distribution, and musculoskeletal biomechanics, a clear and unified terminology is also relevant for muscle-focused research addressing implant–tissue interaction and functional recovery. Objective: This systematic review aimed to critically analyze the terminology used to describe fractures influenced by orthopedic implants, quantify the heterogeneity of current usage across anatomical regions and publication periods, and explore the rationale for adopting a unified umbrella term—“artificial fracture.” Methods: A systematic search was performed in PubMed, Scopus, and Web of Science from January 2000 to December 2024, following PRISMA guidelines. Eligible studies included clinical investigations, reviews, registry analyses, and consensus statements explicitly employing or discussing terminology related to implant-associated fractures. Data were extracted on publication characteristics, anatomical site, terminology employed, and classification systems used. Quantitative bibliometric and qualitative thematic analyses were conducted to assess frequency patterns and conceptual trends. Results: Of 1142 records identified, 184 studies met the inclusion criteria. The most frequent descriptor in the literature was periprosthetic fracture (68%), reflecting its predominance in arthroplasty-focused studies, whereas broader and more practical terms such as implant-related and peri-implant fracture were more commonly used in musculoskeletal and fixation-related research. Terminological preferences varied according to anatomical site and implant type, and no universally accepted, cross-anatomical terminology was identified despite multiple consensus efforts. Discussion and Conclusions: The findings highlight persistent heterogeneity in terminology describing fractures influenced by orthopedic implants. A transversal, descriptive framework may facilitate communication across subspecialties and support registry-level harmonization. Beyond orthopedic traumatology, this approach may also benefit muscle and musculoskeletal research by enabling more consistent interpretation of data related to muscle–bone–implant interactions, rehabilitation strategies, and biomechanical adaptation.
15 January 2026