Hamstring Strain Injury Risk in Soccer: An Exploratory, Hypothesis-Generating Prediction Model
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Data Collection, Testing Protocol and Injury Registration
2.4. Data Treatment and Statistical Analysis
2.5. Development of the Logistic Regression Model
2.6. Planned Model Evaluation Performance
2.7. Planned Stability and Robustness Analyses
3. Results
3.1. Injury Incidence
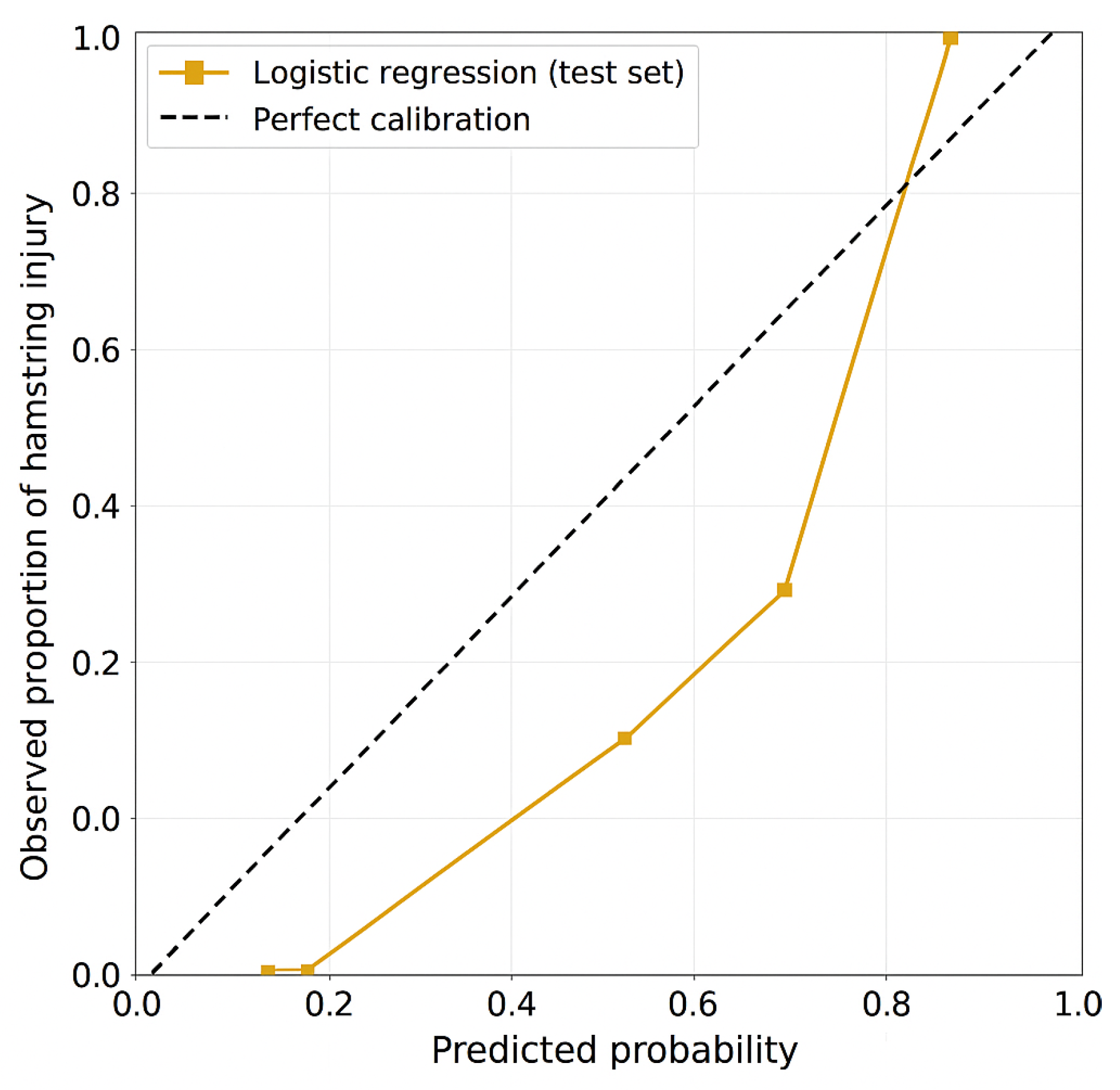
3.2. Model Performance
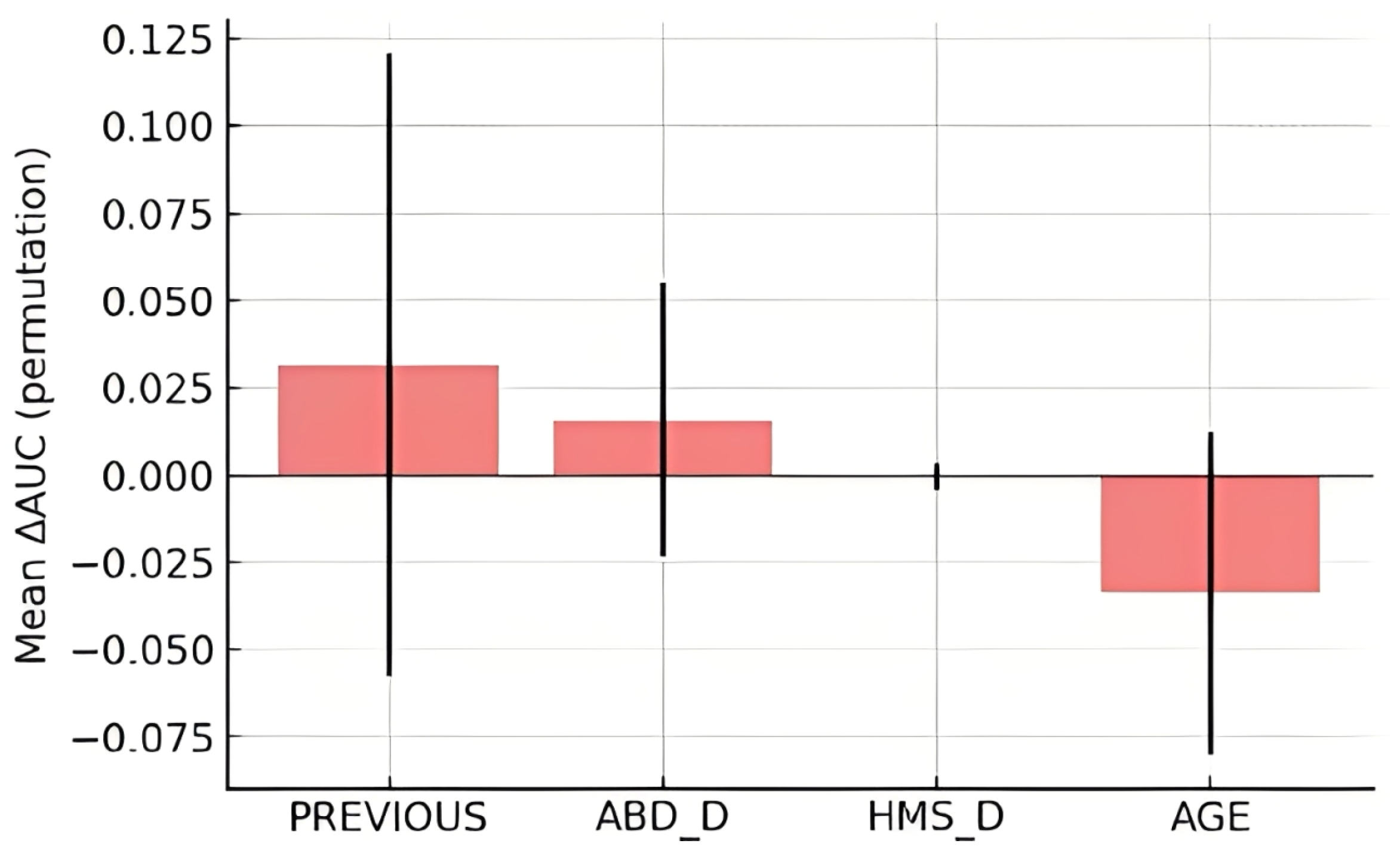
3.3. Predictor Importance
3.4. Stability Analyses
4. Discussion
4.1. The Predictive Value of Machine Learning Algorithms
4.2. Strengths and Limitations
4.3. Future Directions
4.4. Clinical Relevance
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kekelekis, A.; Manuel Clemente, F.; Kellis, E. Muscle Injury Characteristics and Incidence Rates in Men’s Amateur Soccer: A One Season Prospective Study. Res. Sports Med. 2024, 32, 411–424. [Google Scholar] [CrossRef] [PubMed]
- López-Valenciano, A.; Ruiz-Pérez, I.; Garcia-Gómez, A.; Vera-Garcia, F.J.; Croix, M.D.S.; Myer, G.D.; Ayala, F. Epidemiology of Injuries in Professional Football: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2020, 54, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Al Attar, W.S.A.; Husain, M.A. Effectiveness of Injury Prevention Programs with Core Muscle Strengthening Exercises to Reduce the Incidence of Hamstring Injury Among Soccer Players: A Systematic Review and Meta-Analysis. Sports Health 2023, 15, 805–813. [Google Scholar] [CrossRef]
- Ekstrand, J.; Bengtsson, H.; Waldén, M.; Davison, M.; Khan, K.M.; Hägglund, M. Hamstring Injury Rates Have Increased during Recent Seasons and Now Constitute 24% of All Injuries in Men’s Professional Football: The UEFA Elite Club Injury Study from 2001/02 to 2021/22. Br. J. Sports Med. 2023, 57, 292–298. [Google Scholar] [CrossRef]
- Eliakim, E.; Morgulev, E.; Lidor, R.; Meckel, Y. Estimation of Injury Costs: Financial Damage of English Premier League Teams’ Underachievement Due to Injuries. BMJ Open Sport. Exerc. Med. 2020, 6, e000675. [Google Scholar] [CrossRef]
- Green, B.; Bourne, M.N.; Van Dyk, N.; Pizzari, T. Recalibrating the Risk of Hamstring Strain Injury (HSI): A 2020 Systematic Review and Meta-Analysis of Risk Factors for Index and Recurrent Hamstring Strain Injury in Sport. Br. J. Sports Med. 2020, 54, 1081–1088. [Google Scholar] [CrossRef]
- Timmins, R.G.; Bourne, M.N.; Shield, A.J.; Williams, M.D.; Lorenzen, C.; Opar, D.A. Short Biceps Femoris Fascicles and Eccentric Knee Flexor Weakness Increase the Risk of Hamstring Injury in Elite Football (Soccer): A Prospective Cohort Study. Br. J. Sports Med. 2016, 50, 1524–1535. [Google Scholar] [CrossRef]
- Schuermans, J.; Danneels, L.; Van Tiggelen, D.; Palmans, T.; Witvrouw, E. Proximal Neuromuscular Control Protects Against Hamstring Injuries in Male Soccer Players: A Prospective Study with Electromyography Time-Series Analysis during Maximal Sprinting. Am. J. Sports Med. 2017, 45, 1315–1325. [Google Scholar] [CrossRef]
- Heiderscheit, B.C.; Sherry, M.A.; Silder, A.; Chummanov, E.S.; Thelen, D.G. Hamstring Strain Injuries: Recommendations for Diagnosis, Rehabilitation, and Injury Prevention. J. Orthop. Sports Phys. Ther. Mov. Sci. Media 2010, 40, 67–81. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.Y.; Mok, K.-M.; Chan, H.C.K.; Yung, P.S.H.; Chan, K.-M. Eccentric Hamstring Strength Deficit and Poor Hamstring-to-Quadriceps Ratio Are Risk Factors for Hamstring Strain Injury in Football: A Prospective Study of 146 Professional Players. J. Sci. Med. Sport. 2018, 21, 789–793. [Google Scholar] [CrossRef]
- Henderson, G.; Barnes, C.A.; Portas, M.D. Factors Associated with Increased Propensity for Hamstring Injury in English Premier League Soccer Players. J. Sci. Med. Sport. 2010, 13, 397–402. [Google Scholar] [CrossRef]
- Delextrat, A.; Piquet, J.; Matthews, M.J.; Cohen, D.D. Strength-Endurance Training Reduces the Hamstrings Strength Decline Following Simulated Football Competition in Female Players. Front. Physiol. 2018, 9, 1059. [Google Scholar] [CrossRef]
- Mendiguchia, J.; Alentorn-Geli, E.; Brughelli, M. Hamstring Strain Injuries: Are We Heading in the Right Direction? Br. J. Sports Med. 2012, 46, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Wille, C.M.; Stiffler-Joachim, M.R.; Kliethermes, S.A.; Sanfilippo, J.L.; Tanaka, C.S.; Heiderscheit, B.C. Preseason Eccentric Strength Is Not Associated with Hamstring Strain Injury: A Prospective Study in Collegiate Athletes. Med. Sci. Sports Exerc. 2022, 54, 1271–1277. [Google Scholar] [CrossRef] [PubMed]
- Orchard, J.; Marsden, J.; Lord, S.; Garlick, D. Preseason hamstring muscle weakness associated with hamstring muscle injury in Australian footballers. Am. J. Sports Med. 1997, 25, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Nordstrøm, A.; Bahr, R.; Clarsen, B.; Talsnes, O. Association Between Preseason Fitness Level and Risk of Injury or Illness in Male Elite Ice Hockey Players: A Prospective Cohort Study. Orthop. J. Sports Med. 2022, 10, 23259671221076849. [Google Scholar] [CrossRef] [PubMed]
- van Dyk, N.; Farooq, A.; Bahr, R.; Witvrouw, E. Hamstring and Ankle Flexibility Deficits Are Weak Risk Factors for Hamstring Injury in Professional Soccer Players: A Prospective Cohort Study of 438 Players Including 78 Injuries. Am. J. Sports Med. 2018, 46, 2203–2210. [Google Scholar] [CrossRef]
- Bourne, M.N.; Opar, D.A.; Williams, M.D.; Shield, A.J. Eccentric Knee Flexor Strength and Risk of Hamstring Injuries in Rugby Union. Am. J. Sports Med. 2015, 43, 2663–2670. [Google Scholar] [CrossRef]
- Heinert, B.L.; Kernozek, T.W.; Greany, J.F.; Fater, D.C. Hip abductor weakness and lower extremity kinematics during running. J. Sport. Rehabil. 2008, 17, 243–256. [Google Scholar] [CrossRef]
- Mucha, M.D.; Caldwell, W.; Schlueter, E.L.; Walters, C.; Hassen, A. Hip Abductor Strength and Lower Extremity Running Related Injury in Distance Runners: A Systematic Review. J. Sci. Med. Sport. 2017, 20, 349–355. [Google Scholar] [CrossRef]
- Alammari, A.; Spence, N.; Narayan, A.; Karnad, S.D.; Ottayil, Z.C. Effect of Hip Abductors and Lateral Rotators’ Muscle Strengthening on Pain and Functional Outcome in Adult Patients with Patellofemoral Pain: A Systematic Review and Meta-Analysis. J. Back. Musculoskelet. Rehabil. 2023, 36, 35–60. [Google Scholar] [CrossRef]
- Schuermans, J.; Van Tiggelen, D.; Palmans, T.; Danneels, L.; Witvrouw, E. Deviating Running Kinematics and Hamstring Injury Susceptibility in Male Soccer Players: Cause or Consequence? Gait Posture 2017, 57, 270–277. [Google Scholar] [CrossRef]
- Higashihara, A.; Nagano, Y.; Takahashi, K.; Fukubayashi, T. Effects of Forward Trunk Lean on Hamstring Muscle Kinematics during Sprinting. J. Sports Sci. 2015, 33, 1366–1375. [Google Scholar] [CrossRef]
- Chumanov, E.S.; Heiderscheit, B.C.; Thelen, D.G. The Effect of Speed and Influence of Individual Muscles on Hamstring Mechanics during the Swing Phase of Sprinting. J. Biomech. 2007, 40, 3555–3562. [Google Scholar] [CrossRef]
- Kibler, W.B.; Press, J.; Sciascia, A. The Role of Core Stability in Athletic Function. Sports Med. 2006, 36, 189–198. [Google Scholar] [CrossRef]
- Shield, A.J.; Bourne, M.N. Hamstring Injury Prevention Practices in Elite Sport: Evidence for Eccentric Strength vs. Lumbo-Pelvic Training. Sports Med. 2018, 48, 513–524. [Google Scholar] [CrossRef] [PubMed]
- Wallden, M.; Walters, N. Does Lumbo-Pelvic Dysfunction Predispose to Hamstring Strain in Professional Soccer Players? J. Bodyw. Mov. Ther. 2005, 9, 99–108. [Google Scholar] [CrossRef]
- Bittencourt, N.F.N.; Meeuwisse, W.H.; Mendonça, L.D.; Nettel-Aguirre, A.; Ocarino, J.M.; Fonseca, S.T. Complex Systems Approach for Sports Injuries: Moving from Risk Factor Identification to Injury Pattern Recognition-Narrative Review and New Concept. Br. J. Sports Med. 2016, 50, 1309–1314. [Google Scholar] [CrossRef] [PubMed]
- Pudjihartono, N.; Fadason, T.; Kempa-Liehr, A.W.; O’Sullivan, J.M. A Review of Feature Selection Methods for Machine Learning-Based Disease Risk Prediction. Front. Bioinform. 2022, 2, 927312. [Google Scholar] [CrossRef]
- Kolodziej, M.; Groll, A.; Nolte, K.; Willwacher, S.; Alt, T.; Schmidt, M.; Jaitner, T. Predictive Modeling of Lower Extremity Injury Risk in Male Elite Youth Soccer Players Using Least Absolute Shrinkage and Selection Operator Regression. Scand. J. Med. Sci. Sports 2023, 33, 1021–1033. [Google Scholar] [CrossRef]
- Ayala, F.; López-Valenciano, A.; Gámez Martín, J.A.; De Ste Croix, M.; Vera-Garcia, F.J.; García-Vaquero, M.D.P.; Ruiz-Pérez, I.; Myer, G.D. A Preventive Model for Hamstring Injuries in Professional Soccer: Learning Algorithms. Int. J. Sports Med. 2019, 40, 344–353. [Google Scholar] [CrossRef]
- Rico-González, M.; Pino-Ortega, J.; Méndez, A.; Clemente, F.; Baca, A. Machine Learning Application in Soccer: A Systematic Review. Biol. Sport. 2023, 40, 249–263. [Google Scholar] [CrossRef] [PubMed]
- Muazu Musa, R.; Abdul Majeed, A.P.P.; Taha, Z.; Abdullah, M.R.; Husin Musawi Maliki, A.B.; Azura Kosni, N. The Application of Artificial Neural Network and K-Nearest Neighbour Classification Models in the Scouting of High-Performance Archers from a Selected Fitness and Motor Skill Performance Parameters. Sci. Sports 2019, 34, e241–e249. [Google Scholar] [CrossRef]
- Rommers, N.; Rössler, R.; Verhagen, E.; Vandecasteele, F.; Verstockt, S.; Vaeyens, R.; Lenoir, M.; D’Hondt, E.; Witvrouw, E. A Machine Learning Approach to Assess Injury Risk in Elite Youth Football Players. Med. Sci. Sports Exerc. 2020, 52, 1745–1751. [Google Scholar] [CrossRef]
- Luu, B.C.; Wright, A.L.; Haeberle, H.S.; Karnuta, J.M.; Schickendantz, M.S.; Makhni, E.C.; Nwachukwu, B.U.; Williams, R.J.; Ramkumar, P.N. Machine Learning Outperforms Logistic Regression Analysis to Predict Next-Season NHL Player Injury: An Analysis of 2322 Players From 2007 to 2017. Orthop. J. Sports Med. 2020, 8, 2325967120953404. [Google Scholar] [CrossRef]
- Henriquez, M.; Sumner, J.; Faherty, M.; Sell, T.; Bent, B. Machine Learning to Predict Lower Extremity Musculoskeletal Injury Risk in Student Athletes. Front. Sports Act. Living 2020, 2, 576655. [Google Scholar] [CrossRef]
- Van Eetvelde, H.; Mendonça, L.D.; Ley, C.; Seil, R.; Tischer, T. Machine Learning Methods in Sport Injury Prediction and Prevention: A Systematic Review. J. Exp. Orthop. 2021, 8, 27. [Google Scholar] [CrossRef]
- Ruddy, J.D.; Shield, A.J.; Maniar, N.; Williams, M.D.; Duhig, S.; Timmins, R.G.; Hickey, J.; Bourne, M.N.; Opar, D.A. Predictive Modeling of Hamstring Strain Injuries in Elite Australian Footballers. Med. Sci. Sports Exerc. 2018, 50, 906–914. [Google Scholar] [CrossRef]
- Collins, G.S.; Dhiman, P.; Andaur Navarro, C.L.; Ma, J.; Hooft, L.; Reitsma, J.B.; Logullo, P.; Beam, A.L.; Peng, L.; Van Calster, B.; et al. Protocol for Development of a Reporting Guideline (TRIPOD-AI) and Risk of Bias Tool (PROBAST-AI) for Diagnostic and Prognostic Prediction Model Studies Based on Artificial Intelligence. BMJ Open 2021, 11, e048008. [Google Scholar] [CrossRef] [PubMed]
- Cuschieri, S. The STROBE Guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef] [PubMed]
- Kekelekis, A.; Kounali, Z.; Kofotolis, N.; Clemente, F.M.; Kellis, E. Epidemiology of Injuries in Amateur Male Soccer Players: A Prospective One-Year Study. Healthcare 2023, 11, 352. [Google Scholar] [CrossRef] [PubMed]
- Kekelekis, A.; Musa, R.M.; Nikolaidis, P.T.; Clemente, F.M.; Kellis, E. Hip Muscle Strength Ratios Predicting Groin Injury in Male Soccer Players Using Machine Learning and Multivariate Analysis—A Prospective Cohort Study. Muscles 2024, 3, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Kang, H. Sample Size Determination and Power Analysis Using the G*Power Software. J. Educ. Eval. Health Prof. 2021, 18, 17. [Google Scholar] [CrossRef]
- Opar, D.A.; Williams, M.D.; Shield, A.J. Hamstring Strain Injuries: Factors That Lead to Injury and Re-Injury. Sports Med. 2012, 42, 209–226. [Google Scholar] [CrossRef]
- Van Dyk, N.; Bahr, R.; Whiteley, R.; Tol, J.L.; Kumar, B.D.; Hamilton, B.; Farooq, A.; Witvrouw, E. Hamstring and Quadriceps Isokinetic Strength Deficits Are Weak Risk Factors for Hamstring Strain Injuries. Am. J. Sports Med. 2016, 44, 1789–1795. [Google Scholar] [CrossRef] [PubMed]
- Maliki, A.B.H.M.; Abdullah, M.R.; Juahir, H.; Abdullah, F.; Abdullah, N.A.S.; Musa, R.M.; Mat-Rasid, S.M.; Adnan, A.; Kosni, N.A.; Muhamad, W.S.A.W.; et al. A Multilateral Modelling of Youth Soccer Performance Index (YSPI). In Proceedings of the IOP Conference Series: Materials Science and Engineering, Melbourne, Australia, 15–16 September 2018; Institute of Physics Publishing: Bristol, UK, 2018; Volume 342. [Google Scholar] [CrossRef]
- Cohen, J. A Power Primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Babyak, M.A. What You See May Not Be What You Get: A Brief, Nontechnical Introduction to Overfitting in Regression-Type Models. Biopsychosoc. Sci. Med. 2004, 66, 411–421. [Google Scholar]
- Olds, M.; McLaine, S.; Magni, N. Validity and Reliability of the Kinvent Handheld Dynamometer in the Athletic Shoulder Test. J. Sport. Rehabil. 2023, 32, 764–772. [Google Scholar] [CrossRef]
- de Almeida, M.B.; Oliveira, C.; Ornelas, G.; Soares, T.; Souto, J.; Póvoa, A.R.; Ferreira, L.M.A.; Ricci-Vitor, A.L. Intra-Rater and Inter-Rater Reliability of the Kinvent Hand-Held Dynamometer in Young Adults. Med. Sci. Forum 2023, 22, 12. [Google Scholar] [CrossRef]
- Florencio, L.L.; Martins, J.; da Silva, M.R.B.; da Silva, J.R.; Bellizzi, G.L.; Bevilaqua-Grossi, D. Knee and Hip Strength Measurements Obtained by a Hand-Held Dynamometer Stabilized by a Belt and an Examiner Demonstrate Parallel Reliability but Not Agreement. Phys. Ther. Sport. 2019, 38, 115–122. [Google Scholar] [CrossRef]
- Fuller, C.W.; Ekstrand, J.; Junge, A.; Andersen, T.E.; Bahr, R.; Dvorak, J.; Hägglund, M.; McCrory, P.; Meeuwisse, W.H. Consensus Statement on Injury Definitions and Data Collection Procedures in Studies of Football (Soccer) Injuries. Br. J. Sports Med. March 2006, 40, 193–201. [Google Scholar] [CrossRef]
- Tokutake, G.; Kuramochi, R.; Murata, Y.; Enoki, S.; Koto, Y.; Shimizu, T. The Risk Factors of Hamstring Strain Injury Induced by High-Speed Running. J. Sports Sci. Med. 2018, 17, 650–655. [Google Scholar]
- Wolski, L.; Pappas, E.; Hiller, C.; Halaki, M.; Fong Yan, A. Is There an Association between High-Speed Running Biomechanics and Hamstring Strain Injury? A Systematic Review. Sports Biomech. 2021, 23, 1313–1339. [Google Scholar] [CrossRef] [PubMed]
- Croisier, J.L.; Ganteaume, S.; Binet, J.; Genty, M.; Ferret, J.M. Strength Imbalances and Prevention of Hamstring Injury in Professional Soccer Players: A Prospective Study. Am. J. Sports Med. 2008, 36, 1469–1475. [Google Scholar] [CrossRef] [PubMed]
- Bullock, G.S.; Mylott, J.; Hughes, T.; Nicholson, K.F.; Riley, R.D.; Collins, G.S. Just How Confident Can We Be in Predicting Sports Injuries? A Systematic Review of the Methodological Conduct and Performance of Existing Musculoskeletal Injury Prediction Models in Sport. Sports Med. 2022, 52, 2469–2482. [Google Scholar] [CrossRef] [PubMed]
- Steyerberg, E.W.; Uno, H.; Ioannidis, J.P.A.; van Calster, B.; Ukaegbu, C.; Dhingra, T.; Syngal, S.; Kastrinos, F. Poor Performance of Clinical Prediction Models: The Harm of Commonly Applied Methods. J. Clin. Epidemiol. 2018, 98, 133–143. [Google Scholar] [CrossRef]
- Shiferaw, K.B.; Roloff, M.; Waltemath, D.; Zeleke, A.A. Guidelines and Standard Frameworks for AI in Medicine: Protocol for a Systematic Literature Review. JMIR Res. Protoc. 2023, 12, e47105. [Google Scholar] [CrossRef]
- Christodoulou, E.; Ma, J.; Collins, G.S.; Steyerberg, E.W.; Verbakel, J.Y.; Van Calster, B. A Systematic Review Shows No Performance Benefit of Machine Learning over Logistic Regression for Clinical Prediction Models. J. Clin. Epidemiol. 2019, 110, 12–22. [Google Scholar] [CrossRef]



| Metric | Mean | SD | Description |
|---|---|---|---|
| Accuracy (%) | 69.9 | 3.8 | Proportion of all correctly classified cases |
| AUC | 0.792 | 0.064 | Area under the ROC curve |
| Sensitivity (Recall) | 0.700 | 0.073 | True positive rate (injured correctly class). |
| Precision | 0.901 | 0.053 | Positive predictive value |
| F1 Score | 0.787 | 0.040 | Harmonic mean of precision and recall |
| Predictor | β (SE) | OR | 95% CI | p-Value |
|---|---|---|---|---|
| Intercept | 0.963 (4.334) | 2.62 | 0.10–12.80 | 0.824 |
| Age (years) | −0.012 (0.050) | 0.99 | 0.90–1.09 | 0.808 |
| BMI (kg/m2) | 0.034 (0.136) | 1.03 | 0.79–1.35 | 0.805 |
| Previous hamstring injury | −1.283 (0.805) | 0.28 | 0.06–1.34 | 0.111 |
| Hip abduction (dominant leg) | −0.200 (0.083) | 0.82 | 0.70–0.96 | 0.016 * |
| Hip flexion (non-dominant leg) | 0.108 (0.067) | 1.11 | 0.98–1.27 | 0.109 |
| Hip adduction ratio (D/ND) | 0.939 (1.520) | 2.56 | 0.13–50.27 | 0.536 |
| Hip abduction ratio (D/ND) | −0.414 (1.121) | 0.66 | 0.07–5.95 | 0.712 |
| Hamstring ratio (D/ND) | −0.346 (1.541) | 0.71 | 0.04–14.51 | 0.822 |
| Hip flexion ratio (D/ND) | 2.304 (2.251) | 10.02 | 0.12–826.22 | 0.306 |
| Hip flexion/hamstring ratio (dominant leg) | −0.621 (0.947) | 0.54 | 0.08–3.44 | 0.512 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kekelekis, A.; Musa, R.M.; Nikolaidis, P.T.; Clemente, F.M.; Kellis, E. Hamstring Strain Injury Risk in Soccer: An Exploratory, Hypothesis-Generating Prediction Model. Muscles 2025, 4, 50. https://doi.org/10.3390/muscles4040050
Kekelekis A, Musa RM, Nikolaidis PT, Clemente FM, Kellis E. Hamstring Strain Injury Risk in Soccer: An Exploratory, Hypothesis-Generating Prediction Model. Muscles. 2025; 4(4):50. https://doi.org/10.3390/muscles4040050
Chicago/Turabian StyleKekelekis, Afxentios, Rabiu Muazu Musa, Pantelis T. Nikolaidis, Filipe Manuel Clemente, and Eleftherios Kellis. 2025. "Hamstring Strain Injury Risk in Soccer: An Exploratory, Hypothesis-Generating Prediction Model" Muscles 4, no. 4: 50. https://doi.org/10.3390/muscles4040050
APA StyleKekelekis, A., Musa, R. M., Nikolaidis, P. T., Clemente, F. M., & Kellis, E. (2025). Hamstring Strain Injury Risk in Soccer: An Exploratory, Hypothesis-Generating Prediction Model. Muscles, 4(4), 50. https://doi.org/10.3390/muscles4040050











