- Article
Impact of Attending Surgeon Experience on Resident-Performed Cataract Surgery Outcomes
- Paras P. Shah,
- Jamie M. Nord and
- Isha Cheela
- + 3 authors
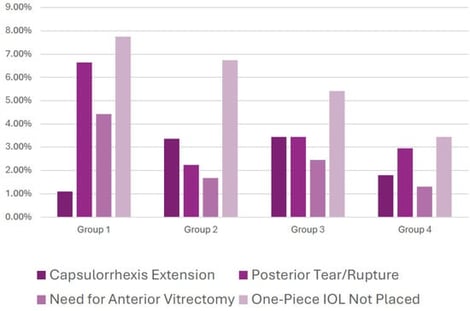
Purpose: This study evaluates the association between supervising attending surgeons’ post-residency experience and complication rates during resident-performed phacoemulsification (cataract extraction) surgeries, and to determine whether this relationship changes as the academic year progresses. Methods: A retrospective analysis of 1263 cataract surgeries performed by eight PGY-4 residents under 14 board-certified attendings was conducted at a New York City residency program over two years. Attendings were divided into four groups based on years of post-residency experience. Primary complications included posterior capsule (PC) tears, anterior vitrectomy (AV), capsulorrhexis extensions (CE), and inability to place a one-piece intraocular lens (IOL). Chi-square analyses compared complication rates between attending groups overall, and between the first and second halves of the academic year. Results: A total of 167 primary complications (13.2%) were identified. Attendings with the fewest years of experience (Group 1) supervised significantly more cases with PC tears (χ2 = 8.173, p = 0.004), AV usage (χ2 = 7.748, p = 0.005), and inability to place a one-piece IOL (χ2 = 4.753, p = 0.029), particularly during the first half of the academic year. Notably, supervising attending experience was not correlated with resident complications in the second half of the academic year. Conclusions: Early in the academic year, less experienced attendings supervised cases with higher complication rates, underscoring the critical role of strategic case assignment and targeted mentorship during early surgical training. These findings suggest that aligning resident progression with appropriate supervision can enhance outcomes and support skill development, optimizing both education and patient safety.
30 January 2026