- Review
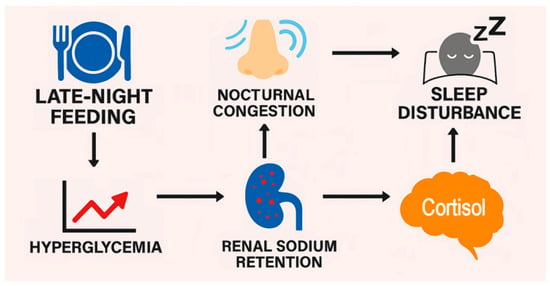
Late-night feeding, defined in the present review as feeding after 8:00 pm when evening insulin secretion and sensitivity are low, is increasingly prevalent in Western society and is recognized as a disruptor of metabolic homeostasis. Yet health problems related to late-night feeding are largely ignored in time-restricted feeding studies that generally do not extend past an 8:00 pm feeding window. This paper proposes a novel cascade linking late-night hyperglycemia with sleep disturbances and nasal congestion mediated by renal sodium retention, increased plasma osmolarity, and stress hormone release by hypothalamic–pituitary–adrenal axis activation. The narrative describes the circadian decline in insulin sensitivity, which amplifies postprandial glucose surges following late-night feeding. Elevated glucose levels drive renal glucose reabsorption via sodium–glucose cotransporters, promoting sodium retention independent of insulin. Increased sodium retention raises extracellular osmolarity, activating hypothalamic osmoreceptors and stimulating the hypothalamic–pituitary–adrenal axis. Cortisol release promotes alertness, while fluid retention and mucosal edema contribute to nasal congestion and early waking. Supine fluid redistribution during sleep further exacerbates airway narrowing, increasing the risk of sleep fragmentation and obstructive sleep apnea. The present paper fills a gap in current time-restricted feeding literature by integrating renal, osmotic, and neuroendocrine pathways that may be overlooked as underlying mechanisms of dysregulated glucose control and hormone dysfunction. Reviewed evidence suggests that symptoms such as nocturnal congestion and sleep disruption are not merely incidental to late-night feeding but frame late night feeding as a risk factor with underlying physiological stressors that could contribute to cardiometabolic risk.
24 December 2025