Abstract
Gestational anemia, characterized by a decrease in red blood cell mass during pregnancy, remains a pervasive global health concern, affecting maternal well-being and fetal development. We have described the physiological changes inherent in pregnancy that predispose women to iron deficiency, emphasizing the increased demand for iron to support the growing fetus and the expansion of maternal blood volume. We explored the challenges in diagnosing and managing gestational anemia, considering the nuanced interplay of genetic, dietary, and socioeconomic factors that influence iron status, based on the national guideline recommendations. By enhancing our understanding of these complex dynamics, we aim to provide a comprehensive schematization of the national guideline for improved preventive strategies, early detection, and targeted interventions to optimize maternal and neonatal health outcomes.
Introduction
Gestational anemia is defined as a hemoglobin (Hb) serum value of less than 11 g/dl in the first and third trimester, less than 10.5 g/dl in the second trimester or less than 10 g/dl in the postpartum period [1]. Regarding the incidence, the World Health Organization estimates that in 2019 37% of pregnant women were affected by gestational anemia, summing 32 million women worldwide [2]. During pregnancy, there are physiological changes in the plasma, respectively an expansion in the plasma volume followed by an expansion of the erythrocyte mass, that decreases blood viscosity, fact that is generally thought to improve the oxygen and nutrient delivery from the mother to the fetus [3]. This expansion generates a physiologic anemia, but when the hemoglobin level decreases below 11 g/dl in the first and third trimester or below 10.5 g/dl in the second trimester, other causes of anemia should be explored [4].
Gestational anemia is determined in most cases by iron or folate deficiency; in rare cases pregnant patients present aplastic anemia, hemolytic anemia, thalassemia or sickle cell disease. 75% of cases of gestational anemia represent a consequence of iron deficiency [5].
Iron deficiency, as well as gestational anemia, has been associated with small for gestational age fetuses, prematurity, a low iron deposit of the newborn, preeclampsia or even postpartum bleeding. In addition, newborns also have a higher risk of perinatal mortality and an elevated risk of neonatal infections. In the postpartum period, patients with gestational anemia can present a decrease in mental performance as well as a decrease in their cognitive abilities and insufficient lactation [6,7]. A retrospective study published in 2022 on more than 18 million pregnancies in China [8] has established that gestational anemia was associated with placental abruption, severe postpartum hemorrhage, maternal shock, preterm birth, admission in the intensive care unit for the parturient women. This association that was correlated with the severity of the anemia: for example, patients with severe anemia presented an adjusted odds ratio of 3.35 of developing placental abruption and a 15.65 adjusted odds ratio of developing severe postpartum bleeding. Another study conducted in the United States [9] and published in 2021 concluded that anemic patients present a twofold incremented risk of developing severe maternal morbidities such as eclampsia, maternal death, necessitating an emergency hysterectomy or transfusion or being admitted in the intensive care unit after birth. The morbidity caused by anemia affects also the newborns, as they presented higher ratios of acute fetal distress or neonatal intensive care unit admissions. Regarding the long-term pregnancy outcome, maternal anemia diagnosed before the 30th pregnancy week was associated with higher rates of autism spectrum disorder, intellectual disability or attention deficit hyperactivity disorder pathologies in the offsprings.
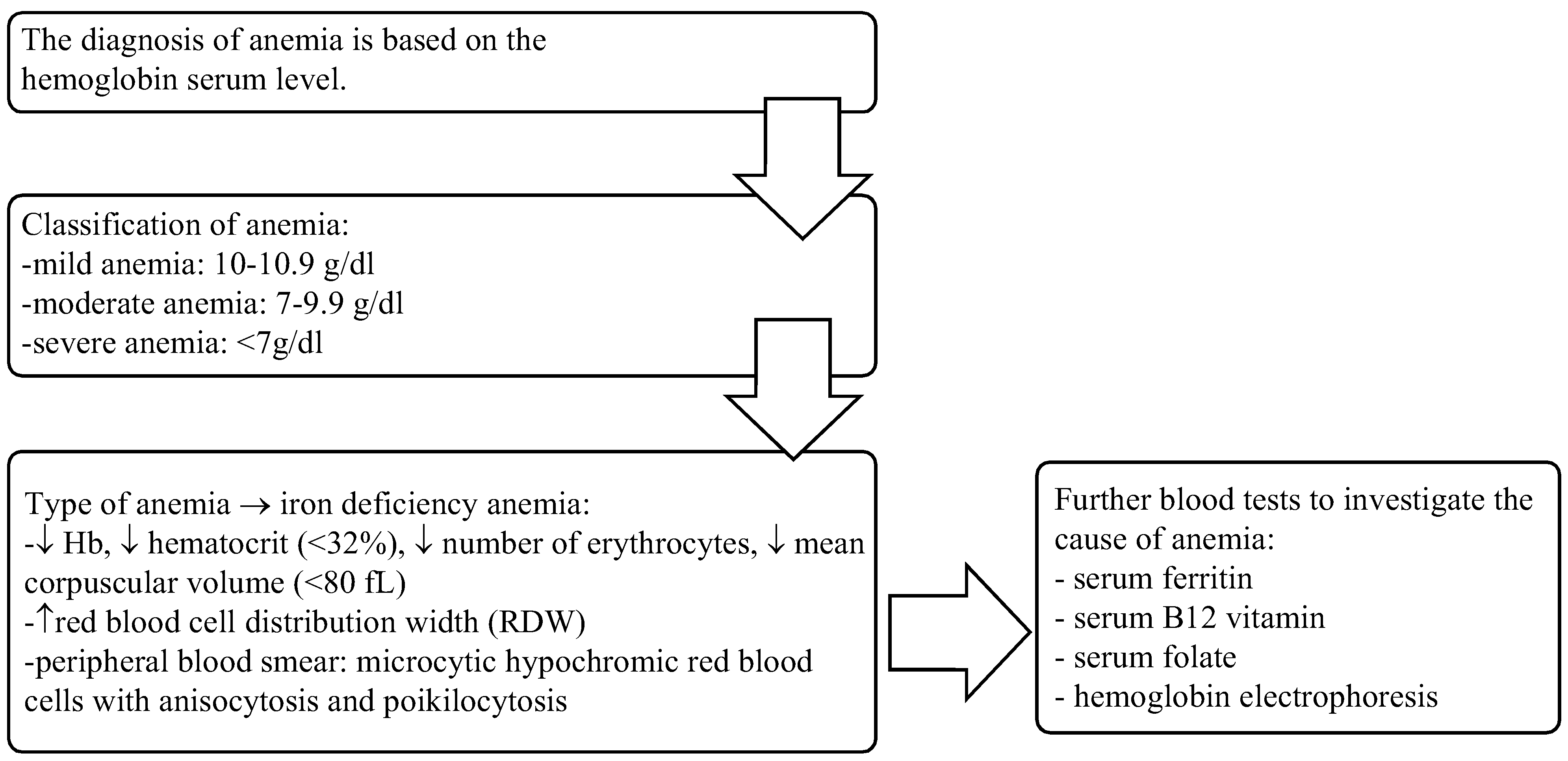
The Romanian ‘Iron Deficiency Anemia in Pregnancy’ Guideline was elaborated in 2019 and revised in 2023 [11]. The aim of this guideline is to support general practitioners and gynecologists in the prophylaxis and treatment of iron deficiency anemia in pregnant women. Based on these guideline recommendations, we elaborated a diagnosis algorithm detailed in Figure 1.
Figure 1.
Diagnosis, classification and investigation of anemia.
The guideline [11] recommends introducing the value of serum ferritin among the standard prenatal care in anemic patients, in non-anemic patients at risk of iron depletion and non-anemic patients who require an estimation of iron reserves. These categories are summarised in Table 1. In order to evaluate the iron deficit, a serum ferritin value is necessary. When encountering a patient with anemia, a serum value of ferritin less than 30 ng/ml defines an iron deficiency anemia. Severe iron deficit is characterised by a ferritin level <30 ng/ml while a ferritin value between 30 and 100 ng/ml describe a moderate iron deficit [11].

Table 1.
Patients requiring iron reserves investigation.
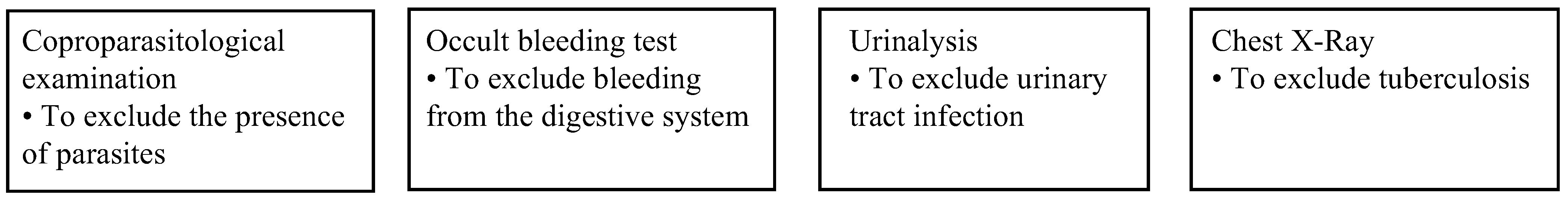
Iron deficiency can also be represented by a ferritin serum value of <50 ng/ml in association with a serum transferrin saturation (STS) value of more than 20%. Regarding the fact that ferritin is an acute phase reactant, whose value grows in inflammation, when suspecting an inflammation, it is necessary to determine the value of C-reactive protein and STS. A normal value of ferritin does not exclude an iron deficiency anemia in the presence of inflammation. Patients suffering from a chronic bowel pathology, chronic kidney disease or chronic heart failure, are at high risk of developing iron deficiency anemia. In these cases, a STS value of less than 20% is necessary to confirm iron deficiency [11]. Further investigations are summarised in Figure 2.
Figure 2.
Complementary examinations.
The standard recommendation is that physicians should advise all pregnant women at risk of developing anemia, to receive iron supplements if the serum ferritin value is decreased, not to mention the risk of developing perinatal complications both for the mother and the fetus in case of iron deficiency or anemia. Iron is also indispensable for cell multiplication, organ development and particularly in the normal development of the fetal central nervous system [11]. Certain studies have demonstrated that iron supplementation should debut before the conception in order to prevent fetal growth restriction as well as prematurity [12]. This implies a thorough preconceptional counselling, that could be difficult to offer or even absent in disadvantaged areas of the country due to the socio-economic status of the population in the respective areas.
A patient with a high serum level of ferritin should be oriented to further investigations. The most common causes of a high serum ferritin value are represented by inflammation, obesity and daily alcohol consumption. The differential diagnosis should include hemochromatosis, Still’s disease, rheumatoid arthritis, type 2 diabetes mellitus, hyperthyroidism, iron intoxication, Hodgkin’s lymphoma, leukemia, restless leg syndrome, multiple transfusions, hepatic pathologies [11,13,14].
The national guideline does not support prophylactic iron supplementation in pregnancy without a documented iron deficiency. Patients without anemia should be reevaluated in 8 weeks [11].
The prophylaxis of iron deficiency anemia should be made in patients with documented iron deficiency using oral iron supplements, informing the patients about the correct administration of oral iron drugs, including food, beverages or other drugs that could decrease the absorption of iron: the timing of the administration is important; on an empty stomach, or 2-3 hours after eating, with a source of vitamin C is ideal; dietary fibres, coffee, milk, tea, chocolate, sodas, cereals or soy food alter iron absorption; antiacids, anticonvulsant drugs, proton pump inhibitors decrease iron absorption [11].
The first treatment line in uncomplicated iron deficiency is represented by oral supplements based on ferrous and ferric salts and the patient should be informed about the most or less frequent secondary effects: constipation, diarrhea, altered appetite, metallic taste, abdominal cramps, nausea, vomiting, stomach discomfort, etc [11]. In case of side effects occurrence, the dosage can be adjusted, or an intermittent administration can be taken into consideration. If a persistence of the side effects is observed despite the modification of dosage or frequency of administration, another product should be administered. Ferrous sulphate combinations present the least adverse reactions and a better bioavailability. Parenteral iron treatment should be administered in cases of moderate or severe anemia, only in the second or third trimester of pregnancy. Oral treatment associated with parenteral treatment is not recommended; also, iron supplementation should not be made in the presence of an active infection [11].
In cases requiring blood transfusions, it is mandatory to inform the patient about the potential risks (infectious agents’ transmission, circulatory system overload, important hemolytic reactions associated with transfusions, etc) [11].
Conclusion
In conclusion, iron deficiency anemia, represents a public healthcare concern, as the perinatal effects are often neglected. Early detection of iron deficiency, followed by proper prophylaxis, before the occurrence of the clinical signs, as well as prenatal counselling are essential to improve the pregnancy outcome; each and every pregnant woman should benefit from an accurate pregnancy monitoring, being thoroughly counselled regarding the diagnosis, effects, potential complications and treatment of gestational anemia.
References
- Anemia in Pregnancy: ACOG Practice Bulletin, Number 233. Obstet Gynecol. 2021, 138, e55–e64. [CrossRef]
- WHO. Anaemia. 2023. Available at https://www.who.int/news-room/fact-sheets/detail/anaemia.
- Stangret, A.; Skoda, M.; Wnuk, A.; Pyzlak, M.; Szukiewicz, D. Mild anemia during pregnancy upregulates placental vascularity development. Med Hypotheses 2017, 102, 37–40. [Google Scholar] [CrossRef] [PubMed]
- Means, R.T. Iron Deficiency and Iron Deficiency Anemia: Implications and Impact in Pregnancy, Fetal Development, and Early Childhood Parameters. Nutrients 2020, 12, 447. [Google Scholar] [CrossRef] [PubMed]
- Sifakis, S.; Pharmakides, G. Anemia in pregnancy. Ann N Y Acad Sci. 2000, 900, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.; Rahman, M.; Moniruddin, A.B.M. Anemia in Pregnancy. Medicine Today. 2014, 26, 49–52. [Google Scholar] [CrossRef]
- Yokoi, K.; Konomi, A. Iron deficiency without anaemia is a potential cause of fatigue: meta-analyses of randomised controlled trials and cross-sectional studies. Br J Nutr. 2017, 117, 1422–1431. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Chen, L.; Wang, Y.; Sun, M.; Guo, Y.; Ma, S.; Wang, X.; Jiang, H.; Wang, X.; Lu, J.; Ge, L.; Dong, S.; Zhuang, Y.; Zhao, Y.; Wei, Y.; Ma, X.; Qiao, J. Severity of Anemia During Pregnancy and Adverse Maternal and Fetal Outcomes. JAMA Netw Open. 2022, 5, e2147046. [Google Scholar] [CrossRef] [PubMed]
- Harrison, R.K.; Lauhon, S.R.; Colvin, Z.A.; McIntosh, J.J. Maternal anemia and severe maternal morbidity in a US cohort. Am J Obstet Gynecol MFM. 2021, 3, 100395. [Google Scholar] [CrossRef] [PubMed]
- Wiegersma, A.M.; Dalman, C.; Lee, B.K.; Karlsson, H.; Gardner, R.M. Association of Prenatal Maternal Anemia With Neurodevelopmental Disorders. JAMA Psychiatry. 2019, 76, 1294–1304. [Google Scholar] [CrossRef] [PubMed]
- Romanian Society of Obstetrics and Gynecology. Iron deficiency anemia in pregnancy national guideline. Availabe at https://sogr.ro/wp-content/uploads/2023/05/19.-Anemia-feripriva-la-gravida-revizuit-2023.pdf.
- Scholl, T.O. Maternal iron status: relation to fetal growth, length of gestation, and iron endowment of the neonate. Nutr Rev. 2011, 69 (Suppl 1), S23–S29. [Google Scholar] [CrossRef] [PubMed]
- Fleming, R.E.; Ponka, P. Iron overload in human disease. N Engl J Med. 2012, 366, 348–359. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Knovich, M.A.; Coffman, L.G.; Torti, F.M.; Torti, S.V. Serum ferritin: Past, present and future. Biochim Biophys Acta. 2010, 1800, 760–769. [Google Scholar] [CrossRef]
© 2023 by the author. The materials published in RJMP are protected by copyright. No part of this publication may be reproduced, copied or transmitted in any form or purpose. The manuscripts sent to the RJMP become the property of the publication and the authors declare on their own responsibility that the materials sent are original and have not been sent to other publishing houses.