Managing Gallstone Ileus and Surgical Considerations in Resource-Limited Settings: A Case Series from the Amazon Jungle
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CT | Computer Tomography |
| ICU | Intensive Care Unit |
| OR | Odds Ratio |
References
- Reisner, R.M.; Cohen, J.R. Gallstone ileus: A review of 1001 reported cases. Am. Surg. 1994, 60, 441–446. [Google Scholar] [PubMed]
- Lassandro, F.; Romano, S.; Ragozzino, A.; Rossi, G.; Valente, T.; Ferrara, I.; Romano, L.; Grassi, R. Role of helical CT in diagnosis of gallstone ileus and related conditions. Am. J. Roentgenol. 2005, 185, 1159–1165. [Google Scholar] [CrossRef] [PubMed]
- Masannat, Y.; Masannat, Y.; Shatnawei, A. Gallstone ileus: A review. Mt. Sinai J. Med. 2006, 73, 1132–1134. [Google Scholar] [PubMed]
- Ayantunde, A.A.; Agrawal, A. Gallstone ileus: Diagnosis and management. World J. Surg. 2007, 31, 1292–1297. [Google Scholar] [CrossRef] [PubMed]
- Muthukumarasamy, G.; Venkata, S.P.; Shaikh, I.A.; Somani, B.K.; Ravindran, R. Gallstone ileus: Surgical strategies and clinical outcome. J. Dig. Dis. 2008, 9, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Halabi, W.J.; Kang, C.Y.; Ketana, N.; Lafaro, K.J.; Nguyen, V.Q.; Stamos, M.J.; Imagawa, D.K.; Demirjian, A.N. Surgery for gallstone ileus: A nationwide comparison of trends and outcomes. Ann. Surg. 2014, 259, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Nuño-Guzmán, C.M.; Marín-Contreras, M.E.; Figueroa-Sánchez, M.; Corona, J.L. Gallstone ileus, clinical presentation, diagnostic and treatment approach. World J. Gastrointest. Surg. 2016, 8, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Clavien, P.A.; Richon, J.; Burgan, S.; Rohner, A. Gallstone ileus. Br. J. Surg. 1990, 77, 737–742. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Sanjuán, J.C.; Casado, F.; Fernández, M.J.; Morales, D.J.; Naranjo, A. Cholecystectomy and fistula closure versus enterolithotomy alone in gallstone ileus. Br. J. Surg. 1997, 84, 634–637. [Google Scholar] [CrossRef] [PubMed]
- Jakubauskas, M.; Luksaite, R.; Sileikis, A.; Strupas, K.; Poskus, T. Gallstone Ileus: Management and Clinical Outcomes. Medicina 2019, 55, 598. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Louis, M.; Gibson, B.; Jones, L.; Singh, H. Mechanical Small Bowel Obstruction Due to Gallstone Ileus: Diagnostic Challenges and Surgical Management. Cureus 2023, 15, e44153. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Neary, P.M.; Dowdall, J.F. Evolution of entero-biliary fistula following gallstone ileus management. BMJ Case Rep. 2012, 2012, bcr2012006929. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tsang, C.F. A rare case of gallstone ileus-the unanswered question. J. Surg. Case Rep. 2021, 2021, rjab164, Erratum in: J. Surg. Case Rep. 2021, 2021, rjab250. https://doi.org/10.1093/jscr/rjab250. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Helmy, N.A.; Ryska, O. Gallstone Ileus Post-cholecystectomy: A Case Review. Cureus 2023, 15, e33345. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yang, D.; Wang, Z.; Duan, Z.J.; Jin, S. Laparoscopic treatment of an upper gastrointestinal obstruction due to Bouveret’s syndrome. World J. Gastroenterol. 2013, 19, 6943–6946. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Elshaer, M.; Gravante, G.; Thomas, K.; Sorge, R.; Al-Hamali, S.; Ebdewi, H. Subtotal cholecystectomy for difficult gallbladders: Systematic review and meta-analysis. JAMA Surg. 2015, 150, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, K.; Suzuki, K.; Takada, T.; Strasberg, S.M.; Asbun, H.J.; Endo, I.; Iwashita, Y.; Hibi, T.; Pitt, H.A.; Umezawa, A.; et al. Tokyo Guidelines 2018: Flowchart for the management of acute cholecystitis. J. Hepato-Biliary-Pancreat. Sci. 2018, 25, 55–72. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.W.; Lin, Y.; Ntakiyiruta, G.; Mutabazi, Z.A.; Davis, W.A.; Morris, M.A.; Smink, D.S.; Riviello, R.; Yule, S. Contextual Challenges to Safe Surgery in a Resource-limited Setting: A Multicenter, Multiprofessional Qualitative Study. Ann. Surg. 2018, 267, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Platt, R.; Davis, R.; Finkelstein, J.; Go, A.S.; Gurwitz, J.H.; Roblin, D.; Soumerai, S.; Ross-Degnan, D.; Andrade, S.; Goodman, M.J.; et al. Multicenter epidemiologic and health services research on therapeutics in the HMO Research Network Center for Education and Research on Therapeutics. Pharmacoepidemiol. Drug Saf. 2001, 10, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Vu, T.; MacDougall, D. Rural Health Care Planning Initiatives and Frameworks: Technology Review [Internet]; Canadian Agency for Drugs and Technologies in Health: Ottawa, ON, Canada, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK602612/ (accessed on 11 December 2025).
- Wang, Y.; Hu, X.J.; Wang, H.H.X.; Duan, H.Y.; Chen, Y.; Li, Y.T.; Luo, Z.L.; Li, X.; Wang, J.J.; Mercer, S.W. Follow-up care delivery in community-based hypertension and type 2 diabetes management: A multi-centre, survey study among rural primary care physicians in China. BMC Fam. Pract. 2021, 22, 224. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Sex | F | F | M | F |
| Age | 75 | 79 | 75 | 72 |
| Medical History | Type II Diabetes mellitus, arterial hypertension, overweight | COPD | Type II Diabetes mellitus, arterial hypertension, basal pneumonia, diverticulosis, CKD, overweight | Overweight |
| Timelapse to develop symptoms | 2 days | 5 days | 2 days | 3 days |
| BMI | 26.6 | 24.2 | 29.6 | 28.2 |
| Leukocytes (4000–10,000 /µL) | 12,100 | 15,600 | 13,770 | 11,000 |
| Creatinine (0.6–1.3 mg/dL) | 1.4 | 1.16 | 1.81 | 1.1 |
| Glucose Levels (70–200 mg/dL) | 312 | 124 | 107 | 199 |
| Total Bilirubin (0.2–1.2 mg/dL) | N/A | 1.14 | 0.6 | 2.19 |
| Direct Bilirubin (0.0–0.3 mg/dL) | N/A | 0.24 | 0.22 | 0.9 |
| Preoperative Diagnosis | Acute appendicitis | Gallstone ileus | Gallstone ileus | Gallstone ileus |
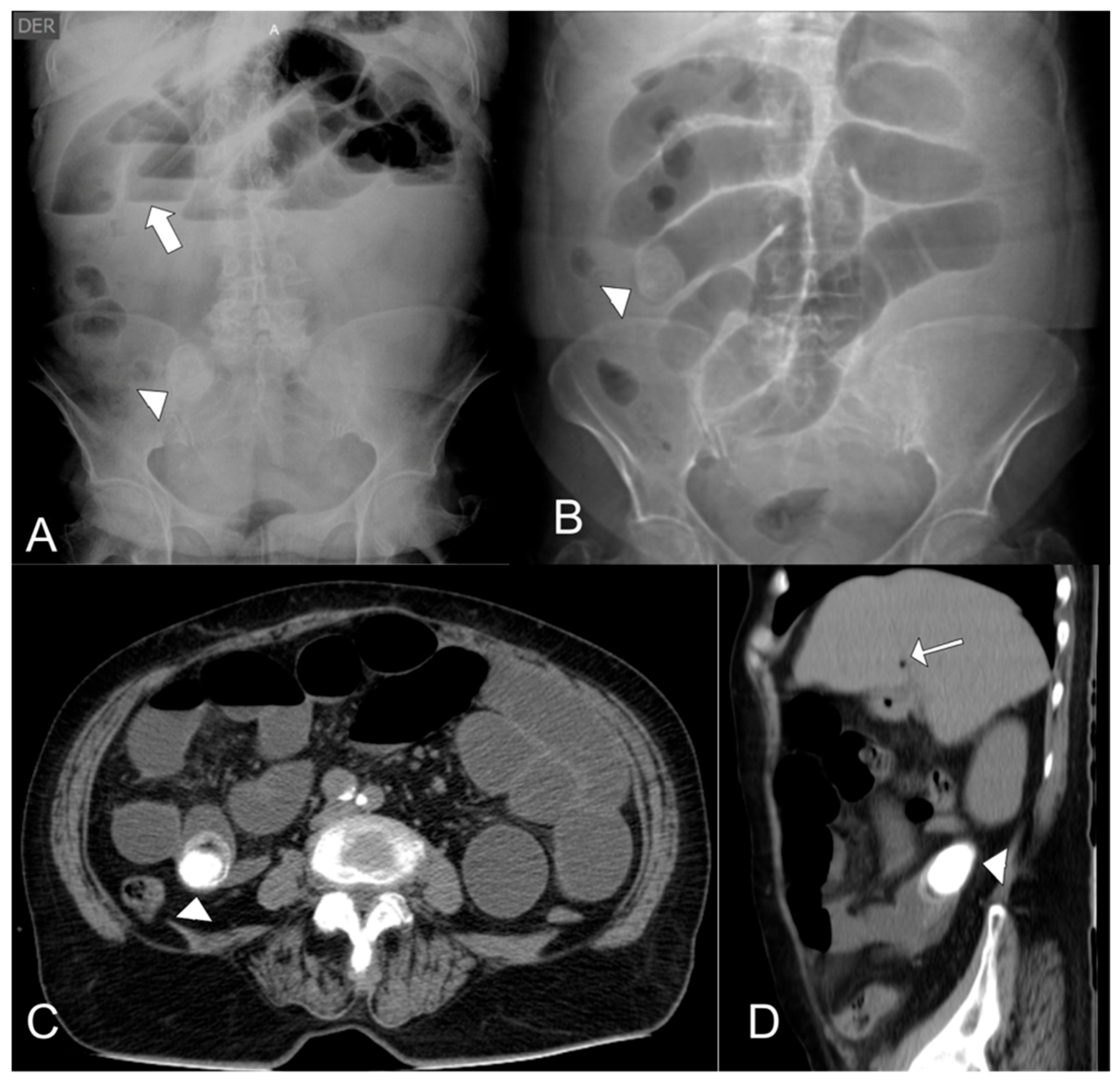
| CT | No | Gallstone ileus | Dilated proximal bowel loops. Collapse of ileal loops. Suspected biliary fistula. | Pneumobilia. Gallstones in the gallbladder and ileum. |
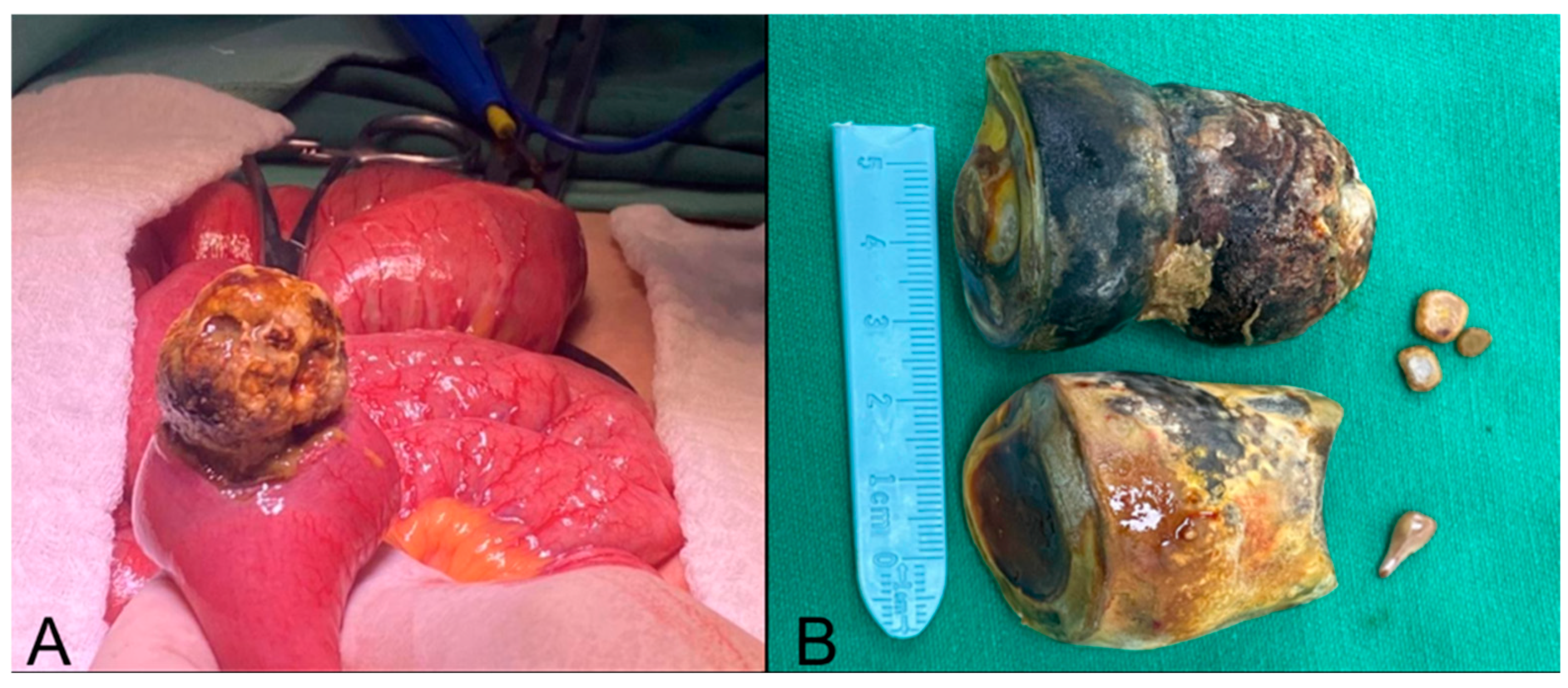
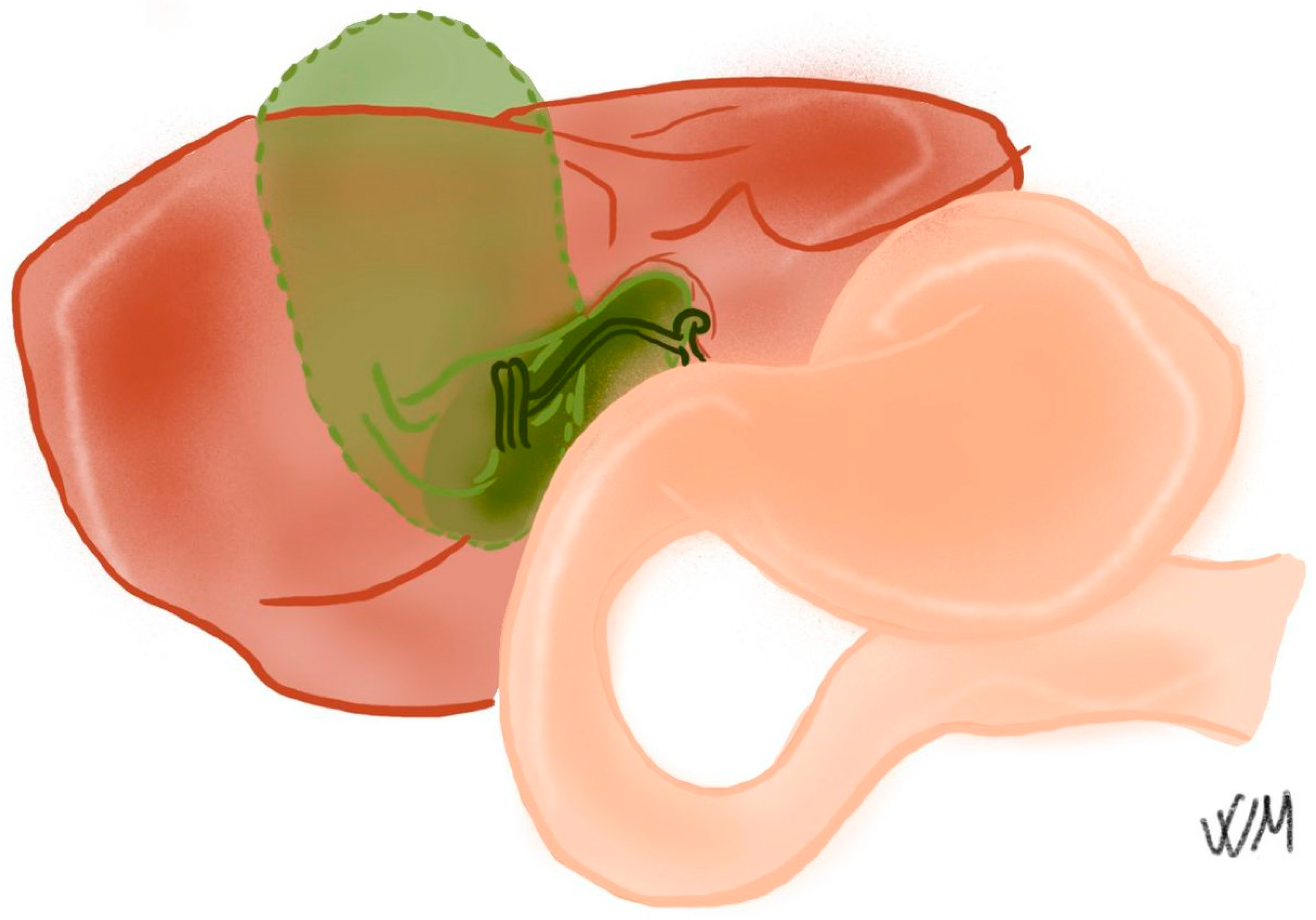
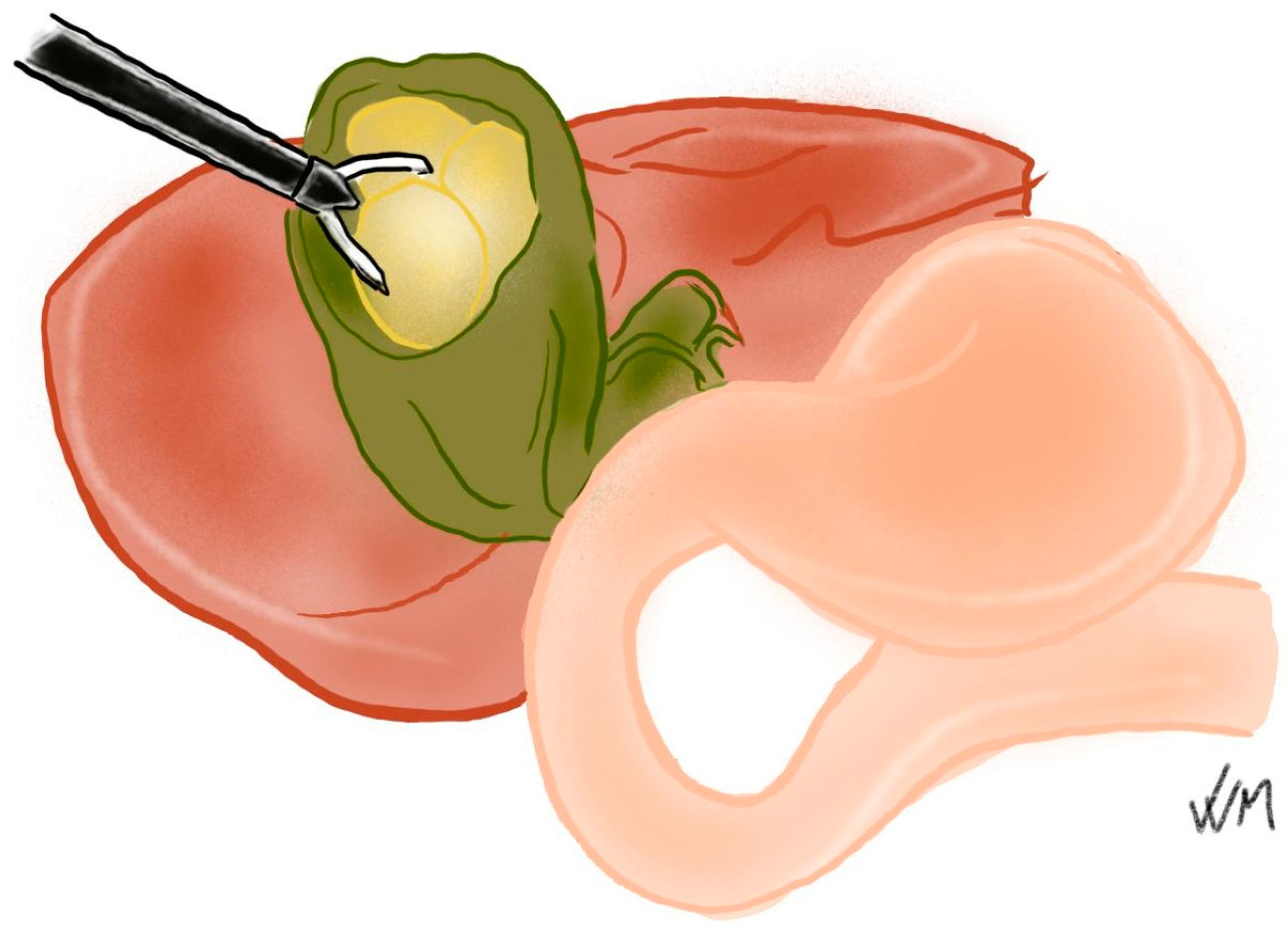
| Surgical Findings | Sclero-atrophic gallbladder. Mirizzi syndrome Type V with biliary fistula. Impacted gallstone in the proximal ileum. | Gallstone ileus, a calculus measuring 5 × 3.2 × 2.5 cm in diameter, located in the terminal ileum. Dilated bowel loops with signs of distress. | Gallstone obstructing the lumen of the ileum. Jejunal diverticula. | Gallstone ileus. Cholecystoduodenal fistula. Gallstones measuring 5 × 4 cm located in the gallbladder. Gallstone obstructing the ileum. |
| Surgical procedure | Enterotomy and gallstone extraction. Subtotal cholecystectomy. | Enterotomy and gallstone extraction. | Enterotomy and gallstone extraction. | Enterotomy and gallstone extraction. Subtotal cholecystectomy. |
| Complications | Punctiform injury of the biliary tract and surgical site infection. | No | No | Pneumonia |
| Length of Stay (days) | 13 | 9 | 6 | 10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Suárez-Gómez, S.A.; Velasco-Muñoz, V.; Escobar, N.; Escobar Castañeda, F.; Guevara, O. Managing Gallstone Ileus and Surgical Considerations in Resource-Limited Settings: A Case Series from the Amazon Jungle. Complications 2026, 3, 2. https://doi.org/10.3390/complications3010002
Suárez-Gómez SA, Velasco-Muñoz V, Escobar N, Escobar Castañeda F, Guevara O. Managing Gallstone Ileus and Surgical Considerations in Resource-Limited Settings: A Case Series from the Amazon Jungle. Complications. 2026; 3(1):2. https://doi.org/10.3390/complications3010002
Chicago/Turabian StyleSuárez-Gómez, Santiago Andrés, Valentina Velasco-Muñoz, Nicolás Escobar, Fernando Escobar Castañeda, and Oscar Guevara. 2026. "Managing Gallstone Ileus and Surgical Considerations in Resource-Limited Settings: A Case Series from the Amazon Jungle" Complications 3, no. 1: 2. https://doi.org/10.3390/complications3010002
APA StyleSuárez-Gómez, S. A., Velasco-Muñoz, V., Escobar, N., Escobar Castañeda, F., & Guevara, O. (2026). Managing Gallstone Ileus and Surgical Considerations in Resource-Limited Settings: A Case Series from the Amazon Jungle. Complications, 3(1), 2. https://doi.org/10.3390/complications3010002







