Abstract
We studied the role of adherence to antihypertensive drug therapy (AHT) in blood pressure (BP) control in a type 2 diabetes (T2D) population treated in secondary care in the DIAbetes and LifEstyle Cohort Twente-1 (DIALECT-1). In addition, intensification of AHT was assessed. Adherence was determined by using the medication possession ratio (MPR), calculated with pharmacy dispensing data for a period of two years following baseline. Adherence was defined as an MPR ≥ 80%. The proportion of adherent patients was compared between patients who had BP-on target (BP-OT) and BP-not on target (BP-NOT). Of the 385 patients included, 56% achieved their BP target. The proportion of adherent patients did not differ between BP-OT and BP-NOT (96% vs. 96%; p = 0.91). Intensification of AHT, including ‘increase in dosage’ and ‘start of a new drug’, was assessed in the two years following baseline. In only 37% of patients with uncontrolled BP during follow-up was AHT intensified. To conclude, adherence to AHT was high and there does not seem to be a relationship between adherence and BP control. There is an opportunity to improve AHT in patients who do not reach their BP target.
1. Introduction
Type 2 diabetes (T2D) was responsible for an estimated 1.5 million deaths worldwide in 2019 [1] and is a major risk factor for cardiovascular disease [2]. In patients with T2D, hypertension is a common comorbidity, and is associated with a 57% increase for the risk of any cardiovascular event [3]. However, about half of patients with diabetes fail to achieve blood pressure (BP) targets [4]; meanwhile, achievement of this target could prevent occurrence of cardiovascular events such as myocardial infarction, heart failure and stroke [3]. After excluding white-coat hypertension, true treatment-resistant hypertension is uncommon and estimated at 8% of patients [5]. It is of vital importance to explore why treatment targets are not reached, because only then can BP treatment be improved effectively. Clinical inertia, defined as the failure of health care providers to initiate or intensify therapy when indicated [6], is identified as a major problem in the management of hypertension [7]. Previously, we reported that suboptimal treatment regimens and non-adherence to lifestyle recommendations such as sodium restriction (≤6 g/day) play an important role in uncontrolled BP [4]. Inadequate adherence to antihypertensive drugs may be an important contributor to not achieving the target BP, as shown by Burnier et al. [8]. Adherence to antihypertensive drugs is typically reported to be less than 50% [9,10]. However, we previously demonstrated in patients with T2D treated in secondary care in the Netherlands that adherence, at least to statins, was much higher (89%) [11] than reported in other populations (18–79%) [12]. It is unknown whether adherence to antihypertensive drugs in our population is also higher than reported elsewhere. In addition, adherence to antihypertensive drugs and other possible causes for uncontrolled BP such as suboptimal treatment regimens are often investigated separately. Adherence rates among studies differ due to differences in the study populations [13]. Adherence rates [14] and prescription patterns for antihypertensive drugs [15] are also dependent on the country where the study is performed. This makes it challenging to draw conclusions on the major cause of uncontrolled BP in a particular population and to identify the best target for improving BP treatment.
Therefore, we aim to assess the role of both adherence to antihypertensive drugs and clinical inertia in blood pressure control.
2. Results
2.1. Patient Inclusion
We included 385 of the 435 patients in DIALECT-1 for analyses. Reasons for exclusion were “no updated informed consent for collecting pharmacy data available” (n = 12), “no pharmacy data available” (n = 19), “no baseline BP measurement available” (n = 14) and “no BP target determination possible due to unknown albuminuria status at baseline” (n = 5). Pharmacy data were not available for some patients because their pharmacies refused to cooperate. Baseline BP measurements were not available for some patients due to technical problems during the BP measurement.
2.2. Descriptive Data
Mean age was 63 ± 9 years and 58% of patients were men (Table 1). Mean duration of diabetes on baseline was 13 ± 9 years. Mean systolic BP was 136 ± 15 mmHg and mean diastolic BP was 74 ± 9 mmHg. The majority (59%) of patients had a BP target < 140/85 mmHg. In total, 56% of patients had BP-OT and 44% BP-NOT. Significantly more patients used a calcium antagonist in BP-NOT compared to BP-OT (28% vs. 19%, p = 0.04). Moreover, significant differences (p < 0.001) in BP target distribution were seen between BP-OT and BP-NOT (BP < 140/85 mmHg 67% vs. 49%, BP ≤ 140/90 mmHg 16% vs. 6% and BP ≤ 130/80 17% vs. 46%, respectively). The proportion of patients using an automated medication dispensing system was not different (6% vs. 10%, p = 0.14) between BP-OT and BP-NOT. In BP-NOT, 17% of patients did not use any antihypertensive drug.

Table 1.
Baseline characteristics divided by achievement of blood pressure target at baseline.
2.3. Adherence and Baseline BP
In total, 334 out of 385 (87%) patients were prescribed one or more antihypertensive drugs (Table 2). In those patients, 96% was adherent (MPR ≥ 80). There was no difference in the proportion of patients adherent between BP-OT and BP-NOT (96% vs. 96%, p = 0.91). Mean MPR rate was 99 ± 9% in BP-OT and 100 ± 10% in BP-NOT (p = 0.13). An MPR > 100% was seen in 41% of patients in BP-OT and in 50% of patients in BP-NOT. The difference between these groups was not significant (p = 0.10). In the sensitivity analysis, in which patients with an automated medication dispensing system were excluded, no significant difference in the proportion of adherent patients (95% vs. 96%, p = 0.98) was seen between BP-OT and BP-NOT. In the secondary analysis, in which follow-up BP measurements were used to divide patients in BP-OT and BP-NOT, there also did not seem to be a difference between the proportion of adherent patients (95% vs. 95%) in BP-OT and BP-NOT.

Table 2.
Adherence by BP control.
2.4. Adherence to Individual Antihypertensive Drug Classes
Adherence to individual antihypertensive drug classes was invariably high: The proportion of adherent patients was about 95% (Figure 1). The lowest adherence was seen for loop diuretics (90%).
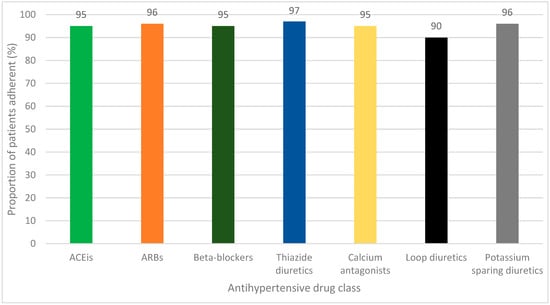
Figure 1.
Adherence in individual different antihypertensive drug classes. ACEi: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker.
2.5. Intensification of Antihypertensive Drug Therapy and BP Course
Two or more follow-up BP measurements after baseline were available for 202 patients. The mean number of available follow-up BP measurements per patient was 6 ± 3. The mean number of BP measurements NOT was 3 ± 3. Of the 202 patients, 126 (62%) patients had two or more follow-up BP measurements NOT (BP-NOT) consecutively in the two years following baseline, of which 60 (48%) patients had BP-OT and 66 (52%) patients had BP-NOT at baseline. The proportion of patients with ‘any intensification’ during follow-up was significantly higher in BP-NOT compared to BP-OT (37% vs. 21%, p = 0.02), see Table 3. The proportion of patients with an ’increase in dosage’ (20% vs. 8%, p = 0.02) and ‘start of a new antihypertensive drug’ (25% vs. 17%, p = 0.21) was higher in BP-NOT compared to BP-OT but the difference only reached statistical significance for ‘increase in dosage’.

Table 3.
Intensification of antihypertensive drug therapy.
2.6. Uncontrolled BP and Role of Adherence and Clinical Inertia
To obtain an overview of potential causes for uncontrolled BP in our study population, we provided an overview of the proportion of patients with BP-NOT, according to baseline BP, who were non-adherent (4%) and the proportion of patients with BP-NOT, according to follow-up BP data, who did not have intensification of AHT (63%) during follow-up (Figure 2).
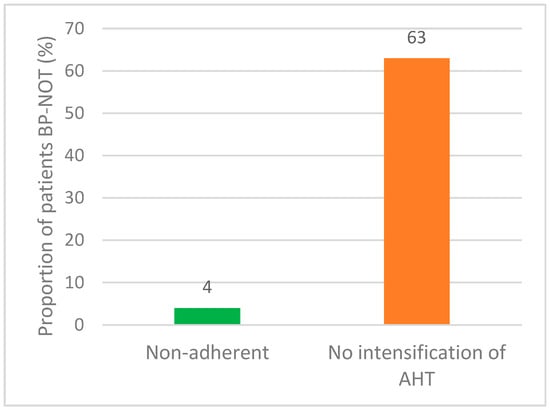
Figure 2.
Potential causes of uncontrolled BP.
3. Discussion
We analyzed whether low adherence to antihypertensive drug therapy plays a role in suboptimal blood pressure control in a T2D population treated in secondary care. We found that patient adherence to antihypertensive drugs was very high for all types of antihypertensive drugs. Nevertheless, the BP target was not achieved in 44% of patients. As adherence is also very high in BP-NOT, adherence to antihypertensive drug therapy in this cohort is not a major factor that determines the success of blood pressure control. In contrast, clinical inertia possibly contributes to the failure of achieving blood pressure targets.
The proportion of patients that did not reach their BP target in our population (44%) is comparable to the literature, demonstrating that approximately 50% of patients have uncontrolled BP [3,16]. In contrast, adherence found in our study was markedly higher compared to most of the literature. A meta-analysis in high-income countries that assessed adherence to antihypertensive drugs, based on pharmacy prescription refill data, in hypertensive patients receiving AHT for primary prevention of coronary heart disease found an adherence of 50% [17]. The mean adherence ranged from 42% for diuretics to 61% for ARBs [17]. On the other hand, adherence rates ranging from 73% to 90% have also been reported in a study in which MPR was calculated from a nationwide database in the United States [18]. The high adherence found in our study is in line with previous research in DIALECT-1 where a high proportion (89%) of patients was found to be adherent to statins [11]. An explanation for the high adherence in our study can be found in previous studies demonstrating that both the presence of diabetes [19], and treatment by an internist were associated with higher adherence [20]. Furthermore, long-standing hypertension is an independent predictor of higher adherence [14]. As the patients in our population complied with those three characteristics, this might explain why adherence was very high. In addition, we hypothesize that patients treated in secondary care feel a greater inclination to adhere to instructions as they have more comorbidities such as kidney failure, or cardiovascular disease, compared to patients treated in primary care. For example, in our study, 30% of patients already had albuminuria, a serious consequence of diabetes. Another reason for the high adherence in this study could be the well-organized pharmacy services in the Netherlands, where pharmacies make use of proactive medication deliveries. The MPR method used possibly contributes to high adherence rates because this method uses a cut-off value of ≥80%. Every patient with an MPR ≥80% was considered to be adherent. Moreover, 28 patients had an automated medication dispensing system and thus had an MPR of 100% because they automatically receive their medication. When we performed our analysis excluding patients with an automated medication dispensing system, this did not influence the results.
A slightly lower adherence was seen for loop diuretics compared to other antihypertensive drug classes. The meta-analysis of Kronish et al. also found a lower adherence for loop diuretics [21]. This could be due to the fact that the official pharmacy prescription for diuretics often contains a fixed dose, whereas in reality patients are sometimes instructed to only take these drugs when necessary, for example after weight gain due to edema. Another explanation could be the side effects of loop diuretics, e.g., polyuria.
It is notable that in the BP-NOT group, there was a higher proportion of patients who had a more challenging BP target ≤130/80 mmHg (BP target for patients with albuminuria). Because the target BP is more stringent, it is more difficult for patients with albuminuria to achieve their target.
The large number of patients who are not prescribed any antihypertensive drug at baseline in BP-NOT is notable, and raises concern, given the well-known relationship between antihypertensive therapy, BP reduction and cardiovascular risk reduction [22,23]. A possible explanation for not starting AHT could be the fact that patients in DIALECT-1 already use an average of seven drugs per day and may be reluctant about increasing the number of drugs that they use. T2D patients use many drugs because the treatment of diabetes consists not only of BP control but also of glycemic control and treatment of dyslipidemia. It is unlikely that a strict indication for AHT was missed by the physician as the DIALECT population consist of patients with a high risk of cardiovascular diseases and physicians are aware of the importance of achieving BP targets to lower this risk.
During follow-up, AHT was intensified in 37% of patients with BP-NOT. This demonstrates that physicians are paying attention to optimizing AHT in our study. However, there is still a large number of patients with BP-NOT in whom AHT was not intensified. Clinical inertia is a well-known problem in hypertension management [24] and also in the management of T2D [25]. A Dutch study found a much higher clinical inertia rate, compared to our study, of 87% in uncontrolled hypertensive patients with one or two antihypertensive drugs treated in primary care [26]. They also found that diabetes and a BP measurement just above target were associated with clinical inertia. A study in patients with diabetes and inadequate glycemic control showed that intensification of glucose-lowering drugs was performed for 45% of patients in secondary care and 37% of patients in primary care [27]. An explanation for not intensifying AHT could be variable BP measurements over time [28] and doubt about the accuracy of an office BP measurement [24]. Other reasons for not intensifying AHT could be that patients might have experienced side effects to antihypertensive drugs in the past or are reluctant about increasing the number of drugs. It is also possible that physicians are reluctant to start new antihypertensive drugs because of renal dysfunction or fear of expected disbalance in electrolytes. Unfortunately, information on these considerations regarding AHT was not available in our database.
Given the high adherence measured in this study, adherence does not seem to be the reason for not achieving BP targets in almost half of our population. Therapy-resistant hypertension does not seem to be the reason either, as the majority (56%) of patients in BP-NOT in our study were not using more than two antihypertensive drugs at baseline. Suboptimal antihypertensive treatment could be part of the reason for not achieving BP targets in our population, as AHT was not intensified in more than half of patients despite follow-up BP-NOT. Another contributory factor is non-adherence to dietary guidelines as previous research in the same population showed that more than 90% of patients with BP-NOT did not meet the target of ≤ 6 g salt intake a day [4].
3.1. Strengths and Limitations
This study is unique because it not only assesses one possible cause of uncontrolled BP but investigates both adherence to antihypertensive drugs and clinical inertia as potential causes of uncontrolled BP. A strength of this study is that it was performed in a real-world setting and the participants were not aware that adherence would be assessed. Moreover, physicians were not aware of the fact that their prescription behavior would be assessed. The use of MPR is a generally accepted method of assessing medication adherence using pharmacy records [29]. The main limitation of this method is that it is not known whether medications that have been collected are actually ingested which could result in an overestimation of adherence [30]. However, we have previously performed urine analyses in the same patients which yielded an almost equally high adherence rate of 92% for antihypertensive drugs [31].
Although the baseline BP measurements were performed under standardized circumstances, it can be considered as a limitation of this study that baseline BP measurements were primarily used to classify patients into BP-OT and BP-NOT, while pharmacy dispensing data over two years following baseline were used to calculate adherence. Therefore, we cannot rule out that some patients would have been classified differently if follow-up BP measurements had been used. To address this, we have also performed analyses using follow-up BP measurements instead of baseline BP and these seem to render the same conclusions though it was not possible to test significance because of too few subjects in the non-adherent groups. Another reason for using baseline BP measurements in the primary analysis is that the original DIALECT study from which we included our patients was designed to measure baseline BP. Therefore, follow-up BP data are missing for a number of patients.
There were a few patients who did not use antihypertensive drugs at baseline and started AHT during follow-up (n = 13). These subjects were included in the adherence analysis although they had been labeled BP-OT or BP-NOT according to the baseline BP measurements.
In our study, we did not correct for potential confounders such as number of drugs or severity of diabetes. However, most potential confounders were equally distributed between BP-OT and BP-NOT (Table 1). Therefore, we do not expect that correction of confounders will alter our conclusions. The biggest difference between groups was found for the BP target ≤ 130/80 mmHg which is the target for patients with albuminuria. An analysis was performed including only patients with the BP target ≤130/80 mmHg to assess whether this would render the same conclusions. This analysis did seem to render the same conclusions (Table A1). Unfortunately, it was not possible to determine significance because of too few subjects in the non-adherent group.
Another limitation of our study is that the BP targets used are not applicable anymore as BP targets have changed. The KDIGO 2021 guidelines recommend a systolic BP target of <120 mmHg for patients with chronic kidney disease, when tolerated, using standardized office BP measurements [32]. This target is substantially lower than the targets used in our study which were based on the KDIGO 2012 guidelines recommending a target of BP ≤140/90 mmHg for patients without albuminuria and eGFR <60 mL/min and a target of BP ≤130/80 mmHg for patients with albuminuria. However, the KDIGO 2021 guidelines also mention that there is less certainty about benefits outweighing the harms in patients with eGFR < 30 mL/min and in patients with diabetes. This makes it uncertain to what extent the KDIGO 2021 recommendations will be followed in daily practice in our population consisting of patients with diabetes. Moreover, our study population already has a high existing treatment burden which could have an impact on decisions about BP targets. The EASD 2019 guidelines recommend a systolic BP target of 130 mmHg for patients with T2D and a target of 130–140 mmHg for older patients (aged ≥ 65 years) [33]. The diastolic BP target is <80 mmHg for all patients with T2D according to the EASD 2019 guidelines. In our study, a target of BP <140/85 mmHg was applied for patients without chronic kidney disease based on the EASD 2013 guideline. To conclude, current BP targets are more strict than the BP targets applying at the time of this study. This further emphasizes the importance of optimizing AHT to achieve BP targets, which is supported by our results.
3.2. Clinical Implications
Physicians should determine the major target for improvement of BP control for each individual patient. Adherence is not always the main concern and optimizing AHT requires attention. To provide targeted advice to physicians regarding clinical inertia, it is important to understand the reasons behind it. Therefore, further research is necessary to investigate the specific causes of clinical inertia. For instance, if a patient is reluctant to take more tablets, the availability of combined tablets should be explored. Additionally, discussing treatment goals with the patient can help prioritize pharmacological treatment. Physicians should document considerations regarding therapy in the patient’s file. When patients are non-adherent to antihypertensive drugs, appropriate actions should be taken based on the cause of non-adherence. For example, an automated medication dispensing system could be helpful in cases of forgetfulness.
4. Materials and Methods
4.1. Study Design and Setting
This study was performed in the DIAbetes and LifEstyle Cohort Twente-1 (DIALECT)-1. DIALECT is an observational prospective cohort study performed at Ziekenhuis Groep Twente Hospital (Almelo and Hengelo, The Netherlands) and is designed to study the effect of pharmacological and non-pharmacological management in patients with T2D treated in secondary care. The primary goal of DIALECT is to optimize T2D treatment through identifying targets for improvement. Patients in DIALECT-1 were recruited between September 2009 and January 2016. This study is performed according to the guidelines of good clinical practice and the Declaration of Helsinki. Written informed consent was available for all patients before participation in the study. The study has been approved by the local institutional review boards (Medisch Ethische Toetsingscommissie Reg. Nos., NL57219.044.16 and 1009.68020) and is registered in the Netherlands Trial Register (NTR trial code 5855). Details of DIALECT-1 have been reported previously [4].
4.2. Participants
All patients with T2D and aged ≥18 years treated in secondary care were eligible for inclusion in DIALECT-1. Patients on renal replacement therapy, patients with insufficient knowledge of the Dutch language and patients who did not understand the informed consent procedure were excluded. The baseline date for the individual patient is the date of the first study visit of the patient in the outpatient clinic. During this visit, BP measurements took place, blood tests were taken and all relevant medical information was recorded in a database. For the current study, patients in DIALECT-1 were excluded when no pharmacy data after baseline were available or no BP measurements on baseline were available. Moreover, patients without available estimated glomerular filtration rate (eGFR) and albuminuria status on baseline were excluded because without these parameters it is not possible to determine the BP target for the individual patient.
4.3. Measurement of Adherence to Antihypertensive Drugs
Adherence to antihypertensive drugs was calculated by using the medication possession ratio (MPR), which is an adequate and well-accepted method to calculate adherence based on pharmacy dispensing data [29]. The MPR is the proportion of time that prescribed medication is available for the patient and is defined as the ratio between the sum of days’ supply for all fills in a certain period and the number of days in that period [30]. After inclusion in DIALECT-1, patients were re-approached in 2016 and 2017 to obtain an informed consent for collecting pharmacy dispensing data. Pharmacies were approached to provide the medication dispensing history of the patient from the baseline date of DIALECT-1 up to that day. Analysis of the medication dispensing data was performed for a period of 24 months starting from baseline (Figure 3). For each chronic medication, the first dispensing date after baseline was noted. The end date was defined as the date of the day before the last collection. Information about the amount of medication dispensed between the first dispensing date and end date, prescribed dose and dosage strength dispensed was noted. These data were all available in the pharmacy dispensing data. Temporarily used antihypertensive drugs were included in the analyses if they were used for at least six months with at least three dispenses. For patients starting AHT after baseline, adherence was also calculated. The following antihypertensive drug classes were distinguished: ACEis, ARBs, beta-blockers, thiazide diuretics, calcium antagonists, loop diuretics, potassium sparing diuretics and ‘other antihypertensive drugs’. For each type of antihypertensive drug the MPR was calculated, as was the average MPR of all antihypertensive drugs per patient. Good adherence was defined as an MPR ≥80% [30]. An MPR above 100% could indicate that patients take more medication than prescribed or have a stock at home. It is also possible that the physician lowered the dose of a drug but did not change the prescription immediately. Patients with an automated medication dispensing system (e.g., Baxter Healthcare) were considered adherent as they automatically received their medication and had an MPR of 100%.
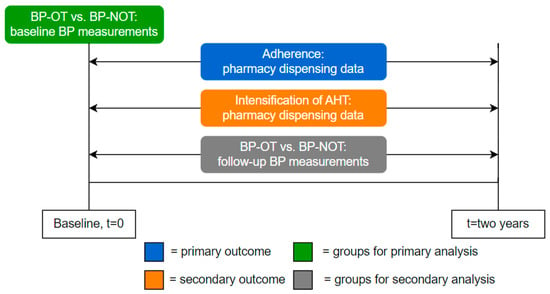
Figure 3.
Study design. BP, blood pressure; BP-OT, Blood Pressure-On Target; BP-NOT, Blood Pressure-Not On Target; AHT, antihypertensive drug therapy.
4.4. Intensification of Antihypertensive Drug Therapy
Intensifications of AHT during the two years following baseline were documented (Figure 3) and divided into three categories for each antihypertensive drug class: ‘start of a new antihypertensive drug’, ‘increase in dosage’ and ‘any intensification’ which is the sum of both categories. A switch within the same antihypertensive drug class was not documented as ‘start of a new drug’. For each patient, intensifications in all antihypertensive drug classes were added and analyzed together. Intensifications in the three categories were reported as the proportion of patients with at least one intensification. When both intensifications and reductions occurred in the same patient, this was classified as an intensification because an attempt to improve BP control was made.
4.5. BP Targets
BP targets were based on international guidelines applying during this study [34,35]. These guidelines were published in 2012 and 2013 but those BP targets were most compatible with daily practice in our population in the study period 2009–2012. In patients with chronic kidney disease, the BP target was determined according to the Kidney Diseases Improving Global Outcomes (KDIGO) guidelines [34]. For patients without chronic kidney disease, the European Association for the Study of Diabetes (EASD) guidelines were used [35]. Patients were divided in three BP target groups based on eGFR and albuminuria status at baseline: BP < 140/85 mmHg for patients without chronic kidney disease [35], BP ≤ 140/90 mmHg for patients without albuminuria and eGFR < 60 mL/min, and BP ≤ 130/80 mmHg for patients with albuminuria [34]. Albuminuria was defined as a 24-h urinary albumin excretion >30 mg/day. Patients were in the BP-on target (BP-OT) group when both systolic and diastolic BP was on target. Patients with systolic and/or diastolic BP not on target were categorized in the BP-not on target (BP-NOT) group.
4.6. Baseline BP Measurements
In the primary analysis of adherence, baseline BP measurements were used to determine whether patients were in the BP-OT or BP-NOT group (Figure 3). These BP measurements were performed at the baseline visit of DIALECT-1 in standardized circumstances using an automated device (Dinamap®; GE Medical systems, Milwaukee, WI, USA). Patients were in a supine position and measurements took place during 15 min with a 1-min interval. The mean systolic and diastolic BP of the last three measurements were used for the primary analysis.
4.7. Follow-Up BP Measurements
In the secondary analyses of adherence and intensification of AHT, follow-up BP measurements over a period of two years following baseline were used to divide patients into BP-OT and BP-NOT (Figure 3). BP measurements from all disciplines in secondary care were included except measurements during hospital admission and home BP measurements. Home BP measurements were excluded because they cannot be compared to BP measurements in office, though they are more accurate. The majority of included BP measurements were single, manual, office BP measurements. In the case of repeated office BP measurements, the last measurement was used. For each patient, the following information was available: number of BP measurements and number of BP measurements NOT. Patients were included in the secondary analysis when they had at least two available follow-up BP measurements. We defined not achieving BP target during follow-up as two or more consecutive BP measurements categorized as BP-NOT because physicians do not often rely on one abnormal BP value in daily practice as BP values can fluctuate and office BP measurements can be falsely higher (the white-coat effect) [36,37]. To determine if follow-up BP measurements were on target, the baseline BP target was used because follow-up data on albuminuria were not available. Therefore, it is not possible to rule out that patients changed to another BP target in the two years following baseline because their eGFR declined or they developed albuminuria.
4.8. Statistical Analysis
Statistical analyses were performed using IBM SPSS for Windows (version 28.0; IBM Corp., Armonk, NY, USA). Normally distributed data are presented as mean ± SDs. Skewed variables are presented as median (interquartile ranges (IQRs)). Dichotomous variables are presented as numbers (percentages). The normality of data was assessed by visually inspecting the frequency histograms of each variable. For the primary analysis, the proportion of adherent patients was compared between BP-OT and BP-NOT. A sensitivity analysis was performed excluding patients with an automated medication dispensing system. For the secondary analyses, the proportion of adherent patients and the proportion of patients with an intensification of AHT was compared between patients who did not reach target BP during follow-up and patients who did. Differences between BP groups were tested with the independent-samples Student’s t-test for normally distributed data and with the χ2 test for dichotomous variables. A two tailed p value < 0.05 was considered statistically significant.
5. Conclusions
We found that in our population, almost all patients with T2D were adherent to antihypertensive drug therapy; thus, non-adherence did not contribute to low achievement of target BP. Antihypertensive drug treatment was intensified in only a third of patients not on target BP. Therefore, clinical inertia might be associated with poor BP control. Taken together, BP target achievement in patients with T2D is low, so attention to optimizing antihypertensive drug therapy is needed to improve BP control and reduce the risk for cardiovascular complications.
Author Contributions
S.L.D.: methodology, formal analysis, investigation, writing—original draft preparation, and visualization; H.M.M.-H.: investigation, resources, and writing—review and editing; C.M.G.: conceptualization, methodology, investigation, resources, and writing—review and editing; R.M.N.: investigation and resources; W.J.K.-K.: writing—review and editing; S.J.L.B.: writing—review and editing; G.D.L.: conceptualization, methodology, resources, data curation, writing—review and editing, supervision, and project administration. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by local institutional review boards (Medisch Ethische Toetsingscommissie Reg. Nos., NL57219.044.16 and 1009.68020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The data presented in this study are available on valid request from the corresponding author. The data are not publicly available because DIALECT-1 was not set up as an open-source study.
Acknowledgments
We thank Heleen Binnenmars for her general contributions to DIALECT, including patient inclusion. We thank Annis Jalving and Jelle Beernink for their contribution to the collection of pharmacy dispensing data. We thank Milou Oosterwijk for her contributions to the database.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Adherence in patients with albuminuria.
Table A1.
Adherence in patients with albuminuria.
| Total Population | BP-OT | BP-NOT | p | |
|---|---|---|---|---|
| Patients with albuminuria * | 108 | 35 (32.4) | 73 (67.6) | <0.001 |
| Adherent (MPR ≥ 80%) | 102 (94.4) | 34 (97.1) | 68 (93.2) | ** |
* Based on BP target ≤ 130/80 mmHg and only including patients with a prescription for an antihypertensive drug. ** Not possible to calculate significance because of expected count less than 5 in 2 cells.
References
- VizHub—GBD Results. Available online: https://vizhub.healthdata.org/gbd-results/ (accessed on 9 January 2023).
- Caussy, C.; Aubin, A.; Loomba, R. The Relationship Between Type 2 Diabetes, NAFLD, and Cardiovascular Risk. Curr. Diabetes Rep. 2021, 21, 15. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; McAlister, F.A.; Walker, R.L.; Hemmelgarn, B.R.; Campbell, N.R.C. Cardiovascular Outcomes in Framingham Participants With Diabetes. Hypertension 2011, 57, 891–897. [Google Scholar] [CrossRef] [PubMed]
- Gant, C.M.; Binnenmars, S.H.; van den Berg, E.; Bakker, S.J.L.; Navis, G.; Laverman, G.D. Integrated Assessment of Pharmacological and Nutritional Cardiovascular Risk Management: Blood Pressure Control in the DIAbetes and LifEstyle Cohort Twente (DIALECT). Nutrients 2017, 9, 709. [Google Scholar] [CrossRef] [PubMed]
- Wei, F.F.; Zhang, Z.Y.; Huang, Q.F.; Yang, W.Y.; Staessen, J.A. Resistant Hypertension. Kardiol. Pol. 2018, 76, 1031–1042. [Google Scholar] [CrossRef]
- Phillips, L.S.; Branch, J.; Cook, C.B.; Doyle, J.P.; El-Kebbi, I.M.; Gallina, D.L.; Miller, C.D.; Ziemer, D.C.; Barnes, C.S. Clinical Inertia. Ann. Intern. Med. 2001, 135, 825–834. [Google Scholar] [CrossRef]
- Milman, T.; Joundi, R.A.; Alotaibi, N.M.; Saposnik, G. Clinical Inertia in the Pharmacological Management of Hypertension: A Systematic Review and Meta-Analysis. Medicine 2018, 97, e11121. [Google Scholar] [CrossRef]
- Burnier, M.; Egan, B.M. Adherence in Hypertension. Circ. Res. 2019, 124, 1124–1140. [Google Scholar] [CrossRef]
- Hill, M.N.; Miller, N.H.; DeGeest, S. ASH Position Paper: Adherence and Persistence with Taking Medication to Control High Blood Pressure. J. Clin. Hypertens. 2010, 12, 757–764. [Google Scholar] [CrossRef]
- Vrijens, B.; Vincze, G.; Kristanto, P.; Urquhart, J.; Burnier, M. Adherence to Prescribed Antihypertensive Drug Treatments: Longitudinal Study of Electronically Compiled Dosing Histories. BMJ 2008, 336, 1114–1117. [Google Scholar] [CrossRef]
- Beernink, J.M.; Oosterwijk, M.M.; van Boven, J.F.M.; Heerspink, H.J.L.; Bakker, S.J.L.; Navis, G.; Nijboer, R.M.; Gant, C.M.; Haverkate, H.; Kruik-Kollöffel, W.J.; et al. Adherence to Statin Therapy and Attainment of LDL Cholesterol Targets in an Outpatient Population of Type 2 Diabetes Patients: Analysis in the DIAbetes and LifEstyle Cohort Twente (DIALECT). Front. Pharmacol. 2022, 13, 888110. [Google Scholar] [CrossRef]
- Hope, H.F.; Binkley, G.M.; Fenton, S.; Kitas, G.D.; Verstappen, S.M.M.; Symmons, D.P.M. Systematic Review of the Predictors of Statin Adherence for the Primary Prevention of Cardiovascular Disease. PLoS ONE 2019, 14, e0201196. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Kwon, O.D.; Han, E.B.; Lee, C.M.; Oh, S.W.; Joh, H.K.; Oh, B.; Kwon, H.; Cho, B.; Choi, H.C. Impact of Number of Medications and Age on Adherence to Antihypertensive Medications: A Nationwide Population-Based Study. Medicine 2019, 98, e17825. [Google Scholar] [CrossRef] [PubMed]
- Uchmanowicz, B.; Jankowska, E.A.; Uchmanowicz, I.; Morisky, D.E. Self-Reported Medication Adherence Measured With Morisky Medication Adherence Scales and Its Determinants in Hypertensive Patients Aged ≥60 Years: A Systematic Review and Meta-Analysis. Front. Pharmacol. 2019, 10, 168. [Google Scholar] [CrossRef] [PubMed]
- Alencar de Pinho, N.; Levin, A.; Fukagawa, M.; Hoy, W.E.; Pecoits-Filho, R.; Reichel, H.; Robinson, B.; Kitiyakara, C.; Wang, J.; Eckardt, K.U.; et al. Considerable International Variation Exists in Blood Pressure Control and Antihypertensive Prescription Patterns in Chronic Kidney Disease. Kidney Int. 2019, 96, 983–994. [Google Scholar] [CrossRef] [PubMed]
- Gyberg, V.; Bacquer, D.; Backer, G.; Jennings, C.; Kotseva, K.; Mellbin, L.; Schnell, O.; Tuomilehto, J.; Wood, D.; Rydén, L.; et al. On behalf of the EUROASPIRE Investigators. Patients with Coronary Artery Disease and Diabetes Need Improved Management: A Report from the EUROASPIRE IV Survey: A Registry from the EuroObservational Research Programme of the European Society of Cardiology. Cardiovasc. Diabetol. 2015, 14, 1–11. [Google Scholar] [CrossRef]
- Naderi, S.H.; Bestwick, J.P.; Wald, D.S. Adherence to Drugs That Prevent Cardiovascular Disease: Meta-Analysis on 376,162 Patients. Am. J. Med. 2012, 125, 882–887.e1. [Google Scholar] [CrossRef]
- Elliott, W.J.; Plauschinat, C.A.; Skrepnek, G.H.; Gause, D. Persistence, Adherence, and Risk of Discontinuation Associated with Commonly Prescribed Antihypertensive Drug Monotherapies. J. Am. Board Fam. Med. 2007, 20, 72–80. [Google Scholar] [CrossRef]
- Jankowska-Polańska, B.; Karniej, P.; Polański, J.; Seń, M.; Świątoniowska-Lonc, N.; Grochans, E. Diabetes Mellitus Versus Hypertension—Does Disease Affect Pharmacological Adherence? Front. Pharmacol. 2020, 11, 1157. [Google Scholar] [CrossRef]
- Lee, C.Y.; Huang, C.C.; Shih, H.C.; Huang, K.H. Factors Influencing Antihypertensive Medication Compliance in Taiwan: A Nationwide Population-Based Study. Eur. J. Prev. Cardiol. 2013, 20, 930–937. [Google Scholar] [CrossRef]
- Kronish, I.M.; Woodward, M.; Sergie, Z.; Ogedegbe, G.; Falzon, L.; Mann, D.M. Meta-Analysis: Impact of Drug Class on Adherence to Antihypertensives. Circulation 2011, 123, 1611–1621. [Google Scholar] [CrossRef]
- Brown, M.J.; Palmer, C.R.; Castaigne, A.; De Leeuw, P.W.; Mancia, G.; Rosenthal, T.; Ruilope, L.M. Morbidity and Mortality in Patients Randomised to Double-Blind Treatment with a Long-Acting Calcium-Channel Blocker or Diuretic in the International Nifedipine GITS Study: Intervention as a Goal in Hypertension Treatment (INSIGHT). Lancet 2000, 356, 366–372. [Google Scholar] [CrossRef]
- Dahlöf, B.; Devereux, R.B.; Kjeldsen, S.E.; Julius, S.; Beevers, G.; De Faire, U.; Fyhrquist, F.; Ibsen, H.; Kristiansson, K.; Lederballe-Pedersen, O.; et al. Cardiovascular Morbidity and Mortality in the Losartan Intervention For Endpoint Reduction in Hypertension Study (LIFE): A Randomised Trial against Atenolol. Lancet 2002, 359, 995–1003. [Google Scholar] [CrossRef] [PubMed]
- Josiah Willock, R.; Miller, J.B.; Mohyi, M.; Abuzaanona, A.; Muminovic, M.; Levy, P.D. Therapeutic Inertia and Treatment Intensification. Curr. Hypertens. Rep. 2018, 20, 4. [Google Scholar] [CrossRef] [PubMed]
- Almigbal, T.H.; Alzarah, S.A.; Aljanoubi, F.A.; Alhafez, N.A.; Aldawsari, M.R.; Alghadeer, Z.Y.; Alrasheed, A.A. Clinical Inertia in the Management of Type 2 Diabetes Mellitus: A Systematic Review. Medicina 2023, 59, 182. [Google Scholar] [CrossRef] [PubMed]
- Ali, D.H.; Kiliç, B.; Hart, H.E.; Bots, M.L.; Biermans, M.C.J.; Spiering, W.; Rutten, F.H.; Hollander, M. Therapeutic Inertia in the Management of Hypertension in Primary Care. J. Hypertens. 2021, 39, 1238–1245. [Google Scholar] [CrossRef] [PubMed]
- Shah, B.R.; Hux, J.E.; Laupacis, A.; Zinman, B.; Van Walraven, C. Clinical Inertia in Response to Inadequate Glycemic Control: Do Specialists Differ from Primary Care Physicians? Diabetes Care 2005, 28, 600–606. [Google Scholar] [CrossRef]
- Schutte, A.E.; Kollias, A.; Stergiou, G.S. Blood Pressure and Its Variability: Classic and Novel Measurement Techniques. Nat. Rev. Cardiol. 2022, 19, 643–654. [Google Scholar] [CrossRef]
- Steiner, J.F.; Prochazka, A.V. The Assessment of Refill Compliance Using Pharmacy Records: Methods, Validity, and Applications. J. Clin. Epidemiol. 1997, 50, 105–116. [Google Scholar] [CrossRef]
- Anghel, L.A.; Farcas, A.M.; Oprean, R.N. An Overview of the Common Methods Used to Measure Treatment Adherence. Med. Pharm. Rep. 2019, 92, 117. [Google Scholar] [CrossRef]
- Beernink, J.M.; Oosterwijk, M.M.; Khunti, K.; Gupta, P.; Patel, P.; van Boven, J.F.M.; Lambers Heerspink, H.J.; Bakker, S.J.L.; Navis, G.; Nijboer, R.M.; et al. Biochemical Urine Testing of Medication Adherence and Its Association with Clinical Markers in an Outpatient Population of Type 2 Diabetes Patients: Analysis in the DIAbetes and LifEstyle Cohort Twente (DIALECT). Diabetes Care 2021, 44, 1419. [Google Scholar] [CrossRef]
- Cheung, A.K.; Chang, T.I.; Cushman, W.C.; Furth, S.L.; Hou, F.F.; Ix, J.H.; Knoll, G.A.; Muntner, P.; Pecoits-Filho, R.; Sarnak, M.J.; et al. KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int. 2021, 99, S1–S87. [Google Scholar] [CrossRef] [PubMed]
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: The Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD). Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef] [PubMed]
- Becker, G.J.; Wheeler, D.C.; De Zeeuw, D.; Fujita, T.; Furth, S.L.; Holdaas, H.; Mendis, S.; Oparil, S.; Perkovic, V.; Saad Rodrigues, C.I.; et al. Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int. Suppl. 2012, 2, 337–414. [Google Scholar] [CrossRef]
- Rydén, L.; Grant, P.J.; Anker, S.D.; Berne, C.; Cosentino, F.; Danchin, N.; Deaton, C.; Escaned, J.; Hammes, H.P.; Huikuri, H.; et al. ESC Guidelines on Diabetes, Pre-Diabetes, and Cardiovascular Diseases Developed in Collaboration with the EASD: The Task Force on Diabetes, Pre-Diabetes, and Cardiovascular Diseases of the European Society of Cardiology (ESC) and Developed in Collaboration with the European Association for the Study of Diabetes (EASD). Eur. Heart J. 2013, 34, 3035–3087. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.S.; Choi, H.S.; Bae, E.H.; Kim, S.W.; Ma, S.K. Optimal Blood Pressure Target and Measurement in Patients with Chronic Kidney Disease. Korean J. Intern. Med. 2019, 34, 1181–1187. [Google Scholar] [CrossRef]
- Hebert, S.A.; Ibrahim, H.N. Hypertension Management in Patients with Chronic Kidney Disease. Methodist DeBakey Cardiovasc. J. 2022, 18, 41. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).