Abstract
Intraorbital and transorbital injuries are included in the group of head injuries with low frequency. In particular, such injuries rarely result in infectious processes in the brain parenchyma. This case presents a case where a 57-year-old man reported to the neurosurgery department that he had sustained an injury to the conjunctiva of the upper eyelid a month earlier. The patient was injured by a tree branch, which he removed on his own initiative. After persistent eye abduction palsy, an MRI was performed, which showed a compressive mass in the frontal lobe of the brain. A surgical procedure was indicated, which found a piece of twig 3 mm long inside the abscess. Surgical intervention and antibiotic therapy led to the complete recovery of the patient.
1. Introduction
Incidents of head injuries that exhibit initial absences of apparent consequences are a common occurrence in clinical settings, necessitating the recognition of the potential gravity associated with even minor trauma. Baiden et al. [1] underscore the significant burden of head injuries, with motor vehicle accidents contributing to about 70% of cases. The anticipated yearly incidence exhibits variability, with estimates ranging from 64 to 75 million cases [2]. Intraorbital and transorbital injuries, although relatively uncommon, occur in the context of head injuries [3]. Despite their superficial nature, these injuries lacking ocular and bulbomotoric impairment may initially seem inconsequential, often failing to present symptoms indicative of deeper-seated damage. However, it is essential to consider the intricate anatomical features of the orbital walls, especially the delicate nature of the upper wall, making it vulnerable to penetration by low-pressure forces [3].
The precise identification and effective management of transorbital injuries necessitate a profound comprehension of the intricate orbital anatomy [4]. Transorbital injuries occur when foreign objects penetrate the eye and its surrounding structures, necessitating a comprehensive grasp of orbital anatomy for precise diagnosis and effective treatment. Transorbital injuries arise from the penetration of foreign objects into the eye and its surrounding structures, demanding a comprehensive understanding of orbital anatomy for accurate diagnosis and successful treatment. The orbit comprises a complex configuration of bones, muscles, nerves, blood vessels, and connective tissues, housing critical components, including the eyeball, extraocular muscles, lacrimal apparatus, and fat pads, all of which are susceptible to damage in cases of transorbital trauma [5].
The orbital region is composed of a bony framework comprising the frontal, ethmoid, sphenoid, lacrimal, zygomatic, and maxillary bones, providing crucial structural support and safeguarding the internal structures. A thorough understanding of the precise positions and inter-relationships of these bones aids in assessing fractures and potential routes for foreign object penetration into the orbit [6,7,8]. The extraocular muscles and their attachments enable intricate eye movements and are pivotal in maintaining visual function. Injuries to these muscles can result in impaired eye movement, double vision, and other visual disturbances. Knowledge of the anatomical pathways, innervation, and function of these muscles is imperative for evaluating the extent of muscle involvement and planning appropriate interventions. Neurovascular structures within the orbit, such as the optic nerve, ophthalmic artery, and their respective branches, are prone to damage from transorbital injuries. Familiarity with their anatomical course, relationships, and vascular supply is crucial for identifying potential vascular compromise or optic nerve injuries [9,10]. A comprehensive understanding of orbital anatomy enables the timely detection of injuries, facilitating prompt intervention to preserve visual function and prevent additional complications.
The following report elucidates a specific case of transorbital injury that subsequently led to the development of a frontal lobe abscess in the brain. This case highlights the significant implications of recognizing potential complications and long-term ramifications associated with transorbital injuries, even in the absence of immediate symptomatic neurological manifestations. In addition to presenting the case study, a comprehensive review of the medical literature was conducted to analyze documented cases of transorbital injuries resulting in the subsequent development of brain abscesses.
2. Case Description
A 57-year-old male patient was referred to the neurosurgery department by his family physician. The patient had suffered a fall from a crouching position around 27 days earlier, resulting in an injury to his right upper eyelid caused by a twig. He attempted to self-remove the twig, after which he started experiencing persistent headaches and restricted eye movement. Additionally, the patient reported experiencing persistent headaches and diplopia.
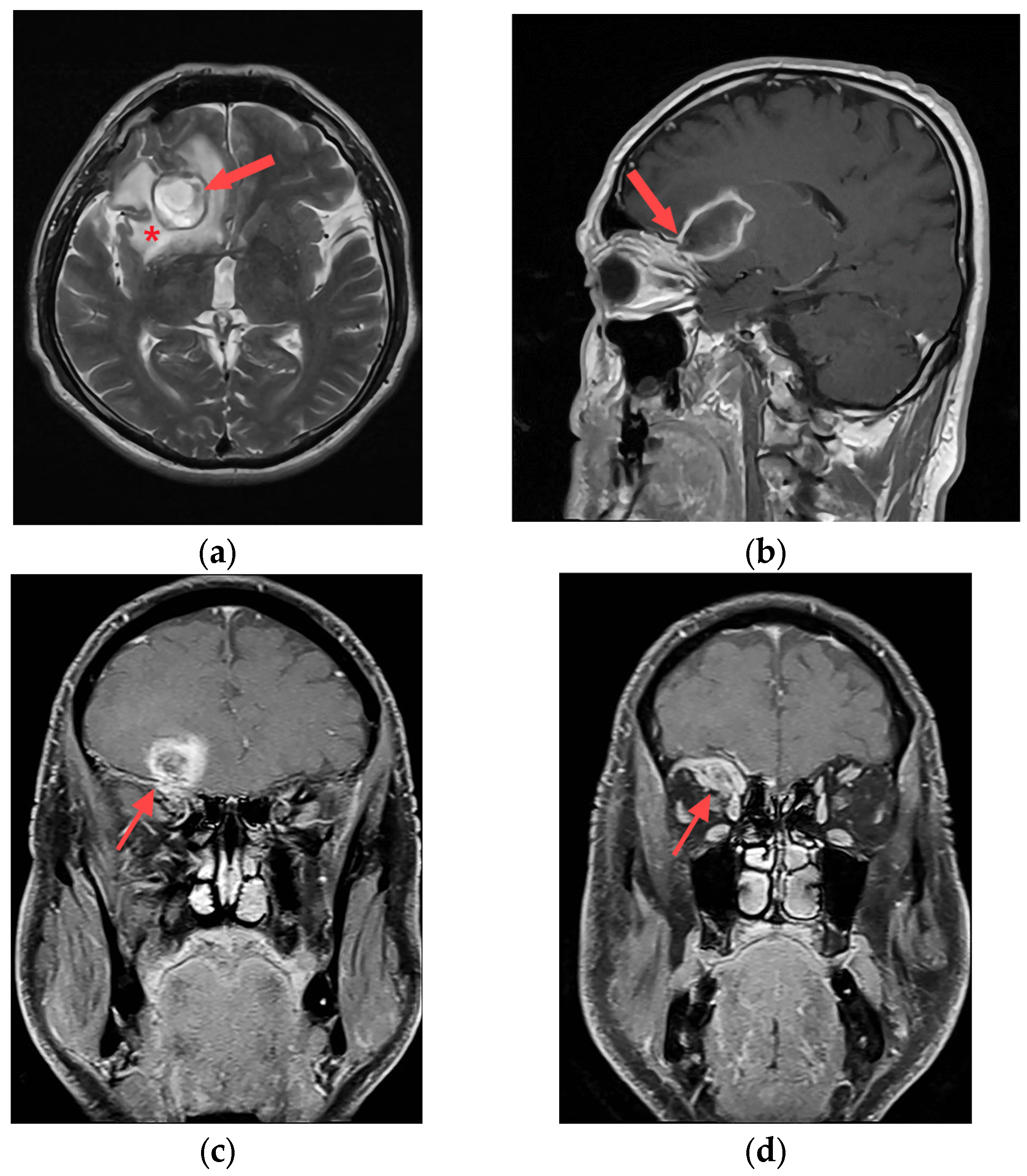
To investigate the underlying cause of the patient’s symptoms, magnetic resonance imaging (MRI) was performed using Siemens Magnetom Avanto 1.5 T in Erlangen, Germany. The MRI scan revealed a significant abnormality in the right frontal lobe, depicted in Figure 1a,b. Figure 1a displayed the presence of an abscess within the right frontal lobe. Additionally, periabscess edema and displacement of midline structures were evident, indicating compression of the surrounding tissue. Figure 1b illustrates the abscess attached to the orbital roof, and the trajectory of the injury from approximately one month earlier. The foreign body’s trajectory, which penetrated the upper part of the upper eyelid conjunctival region, followed a periosteal path along the orbital roof, ultimately reaching the posterior part of the orbital roof within the frontal lobe region, as shown in Figure 1c. An ophthalmologist confirmed the diagnosis of orbital cellulitis, as depicted in Figure 1d.
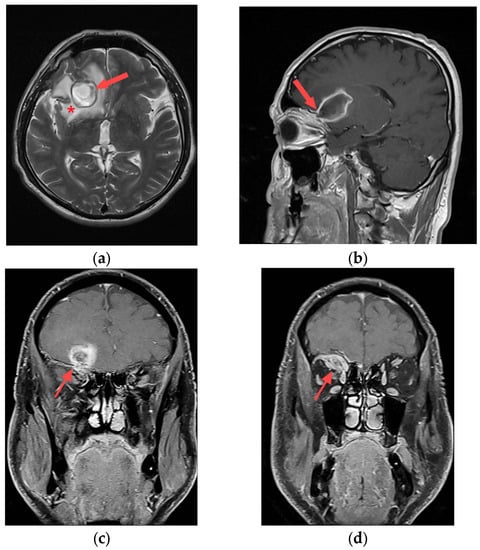
Figure 1.
Preoperative MRI; (a) axial T2W slice with abscess in right frontal lobe (red arrow) and perifocal edema (*); (b) sagittal T1W slice with attachment of abscess to roof of orbit (red arrow); (c) coronal T1W slice with position of brain abscess and roof penetration (red arrow); (d) coronal T1W slice with intraorbital infective process presence (red arrow).
A comprehensive evaluation was performed, incorporating extensive laboratory tests and microbiological analyses, to investigate the presence of an active infection. Nevertheless, no evidence of infectious agents was detected. Based on the clinical findings, the progressive nature of the patient’s neurological symptoms, and the results of imaging studies, the neurosurgeon concluded that surgical intervention was warranted to address the underlying condition.
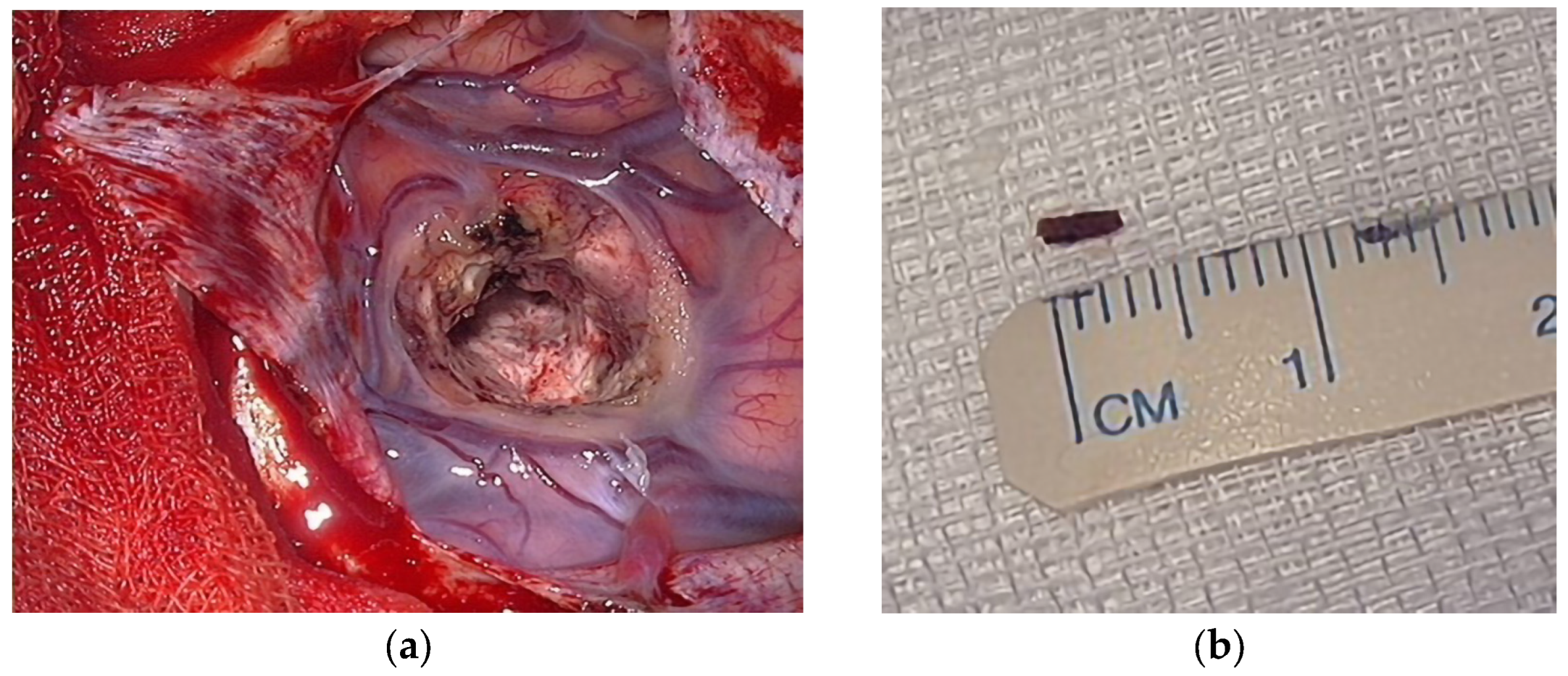
The surgical procedure was performed under general endotracheal anesthesia. Considering the size of the abscess, suspicion of a remaining portion of the twig, and the duration of symptoms, the neurosurgical team opted for the open aspiration and surgical excision of the abscess. The patient’s head was immobilized using a Marquet three-point fixation device, and the operative site underwent sterilization and isolation with sterile drapes. A bone flap was created in the right frontal region, and the dura mater was incised. A corticotomy was performed three centimeters from the sagittal line and five centimeters from the ciliary region. The surgeon proceeded with trajectory through the brain tissue, advancing in a forward and downward direction until reaching the site of the abscess (Figure 2a). The abscess cavity contained dense yellowish material and evidence of hematization of the lower wall. The abscess was carefully drained, and an irrigation solution containing ceftriaxone was used for thorough cleansing of the area. During the procedure, a three-millimeter wooden twig was discovered and subsequently removed from the abscess (Figure 2b).
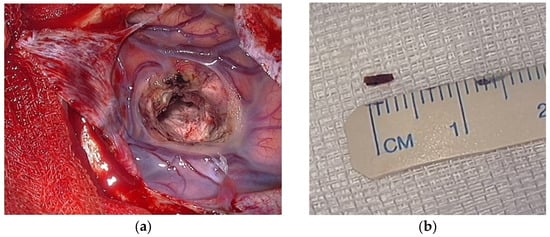
Figure 2.
Intraoperative findings; (a) abscess cavity; (b) the rest of the wooden twig.
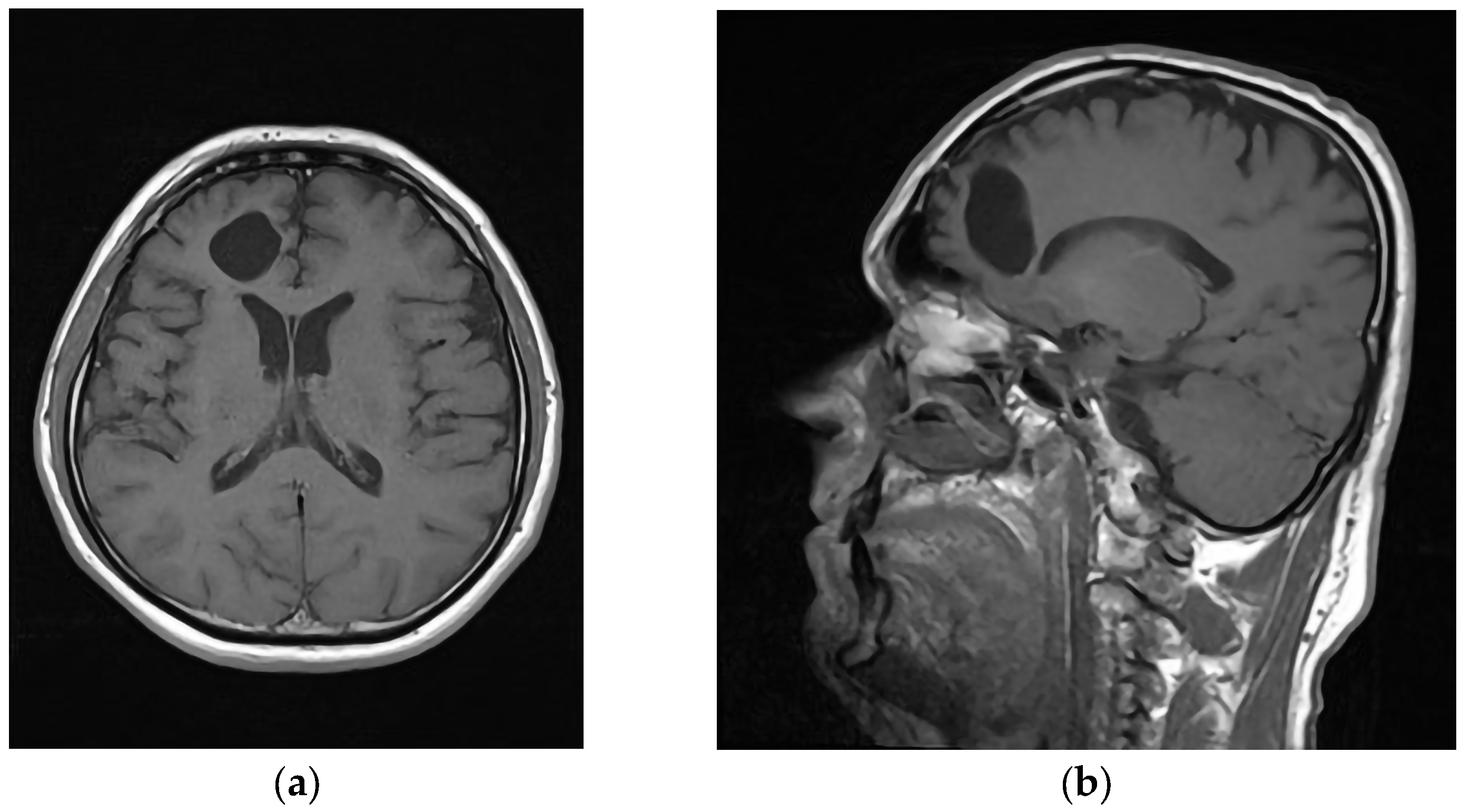
Following the closure of the wound, which involved the placement of an epicranial drain to facilitate drainage and prevent fluid accumulation, the patient underwent monitoring in the intensive care unit. Microbiological analysis of the purulent contents obtained from the abscess did not reveal the presence of any specific bacterial pathogens. The patient’s treatment plan included a 5-week course of intravenous meropenem. After the removal of the epicranial drain and a thorough neurological examination, which yielded normal findings, the patient’s condition demonstrated significant improvement. Consequently, the patient’s condition was deemed stable and appropriate for discharge from the hospital. A postoperative MRI scan was conducted to evaluate the structural changes in the patient’s brain. The MRI images clearly revealed the presence of a well-defined cavity at the surgical site, indicating the successful removal of the abscess (Figure 3a,b). Significantly, no pathological features or abnormalities were observed in the surrounding cerebral tissue. To ensure comprehensive postoperative care and monitor the patient’s neurological status, regular follow-up examinations were scheduled at 6-month intervals, with assessments conducted by both a neurologist and a neurosurgeon. These evaluations consistently demonstrated the absence of pathological sequelae or adverse outcomes.
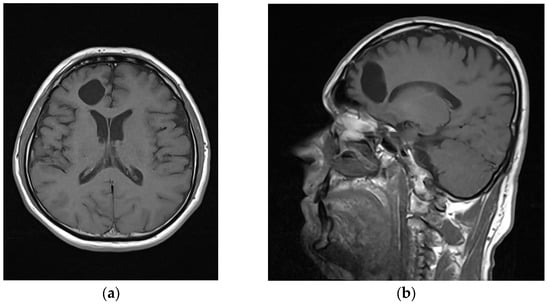
Figure 3.
Postoperative MRI; (a) axial T2 slice; (b) sagittal T2 slice.
3. Discussion
A brain abscess is a localized inflammatory response within the brain parenchyma characterized by the formation of a purulent collection [11]. Although relatively uncommon, it represents a significant and potentially severe complication that can arise following a transorbital-penetrating intracranial injury (TOPI) [12]. It should be noted that brain abscesses can develop even several decades after the initial head injury, as evidenced by a case study conducted by Kuromi et al. [13].
The temporal and frontal lobe were frequently reported as the sites of brain abscesses resulting from transorbital injuries. Notably, cerebellar abscesses were observed in cases involving extensive injuries where foreign bodies extended even into the cerebellum [13,14]. These findings underscore the varied distribution of abscesses associated with transorbital injuries and the significance of evaluating multiple brain regions when assessing such cases.
When it comes to the sequence of infection development, in four cases, a primary inflammatory process was observed intraorbitally, which subsequently spread to the brain [15,16,17]. Additionally, it is evident that an infectious process can originate primarily in the brain parenchyma [3,18,19] or occur postoperatively following foreign body removal [20].
The typical clinical presentation of a brain abscess often involves a triad of symptoms: headache, fever, and focal neurological deficits, which occur in approximately 20% of cases [21]. These symptoms arise as a result of the compressive effect exerted by the accumulated purulent material. While the manifestations may lack specificity, they frequently reflect signs of increased intracranial pressure. Headaches, in particular, tend to be more severe during nighttime and upon awakening, often accompanied by nausea and vomiting. Approximately 25% of patients experience a delayed onset of symptoms and clinical signs [22].
Surgical intervention is indicated when the brain abscess exceeds 3 cm in diameter, leading to significant mass effect, or when it is in close proximity to the brain ventricles. Moreover, surgical treatment is recommended when patients exhibit neurological symptoms or when multilocular abscesses demonstrate progressive growth despite conservative management [23]. Our team chose the open surgical approach due to the size of the abscess. The decision to opt for an open procedure was made based on the careful evaluation and consideration of the specific characteristics and extent of the abscess. Furthermore, following the open surgical approach as described by Gadgil et al. [24], there is a notable reduction in the need for additional imaging, surgical interventions, and prolonged antibiotic therapy. This approach is particularly relevant in resource-limited settings, which is the case in Bosnia and Herzegovina, where the excision of brain abscesses assumes a crucial role in patient management while ensuring favorable outcomes [25,26,27]. The adoption of this surgical technique not only optimizes the utilization of limited resources but also emphasizes the importance of tailored approaches to patient care based on the available healthcare infrastructure [27].
Neuroimaging techniques, such as CT and MRI, play a pivotal role in the diagnosis, complementing the thorough evaluation of the patient’s medical history and physical examination. These imaging modalities serve as highly effective diagnostic tools for assessing the presence and characteristics of brain abscesses [28,29,30].
A comprehensive analysis of the existing literature revealed 12 documented cases of brain abscesses that developed subsequent to transorbital injuries. Among these thirteen cases, which include the one presented in this report, nine involved male individuals. The age range of the affected patients spanned from 1 to 57 years (Table 1).

Table 1.
Summary of literature review.
Transorbital penetrating injuries (TOPIs) can occur in various circumstances [34], including accidents during hiking [3], traffic collisions [22,23], falls from heights [28], and instances of inattention [14,17,18,19,20,32,33]. Bamboo twigs have been frequently identified as the primary foreign bodies associated with TOPI, as observed in studies conducted by Kuromi et al. [13], Maruya et al. [3], and Amano et al. [14]. Additionally, wooden twigs [20,32,33], chopsticks [16,18], and pencils [15] have also been reported as common foreign objects in TOPI cases.
TOPI often results in the migration of foreign bodies from the upper eyelid into various orbital walls, posing a significant risk for the development of brain abscesses. Streptococcus anginosus and Staphylococcus aureus have been identified as the most commonly implicated bacteria in TOPI-associated brain abscesses, as reported by De Andres Crespo et al. [21]. However, it is noteworthy that the precise bacterial cause is frequently undetermined, despite purulent content sampling from the abscess. Streptococcus intermedius [16], Alpha-hemolytic Streptococcus [17], Enterobacter agglomerans [20], and Escherichia coli [14] have been isolated in some TOPI cases.
When considering the diagnostic process, laboratory findings, along with the patient’s medical history, can provide some assistance, but it is the radiological findings that hold crucial importance. Table 1 demonstrates that three out of thirteen subjects exhibited abnormal laboratory values, such as elevated white blood cell count, increased C-reactive protein levels, or accelerated sedimentation rate. However, CT findings serve as the primary diagnostic tool due to their accessibility and rapid assessment. Additionally, the analysis of cerebrospinal fluid can provide valuable diagnostic information [18]. Timely diagnosis and treatment are of paramount importance, as they significantly enhance the chances of survival, given that delayed diagnosis is associated with higher mortality rates [5].
The treatment approach for TOPI-induced brain abscesses involves a combination of surgical and conservative strategies. Among the thirteen cases reviewed, twelve required surgical intervention, commonly involving drainage and stereotaxic aspiration techniques. In cases with multiple fractures, an open surgical approach becomes necessary to address the complex nature of the injury [23]. The choice of conservative treatment varies depending on the specific case. Ceftriaxone has frequently been employed as the primary antimicrobial agent, either as monotherapy or in combination with other drugs such as metronidazole [17,32]. Additionally, vancomycin, amikacin, penicillin, ceftazidime, and fosfomycin have been utilized in various cases. The duration of antibiotic therapy ranges from 8 days to 6 weeks, depending on individual circumstances. In the present case, the intravenous administration of meropenem for a duration of five weeks was chosen, as it had demonstrated positive outcomes in previous research studies [35,36,37].
4. Conclusions
This study presents a comprehensive analysis of a unique case of transorbital injury resulting in the development of a frontal brain abscess. The therapeutic approach involved surgical intervention, including abscess debridement and the administration of intravenous meropenem, a broad-spectrum antibiotic. The distinctiveness of this case lies in the detailed description of the abscess attachment to the orbital roof and the trajectory of the injury, highlighting the potential consequences of such injuries due to anatomical configurations. The literature review conducted in this study enhances our understanding of the relationship between transorbital injuries and brain abscess formation. Importantly, this case contributes novel insights by emphasizing the need to recognize and address the potential complications and long-term implications associated with transorbital injuries, even in the absence of immediate symptomatic manifestations. The findings provide valuable information for healthcare professionals involved in the management of similar cases.
Author Contributions
Conceptualization, H.B. and E.B.; methodology, E.B. and M.P.; software, E.B.; resources, A.J., M.P. and E.S.; writing—original draft preparation, H.B., E.B., R.S. and L.Č.; writing—review and editing, M.P. and E.S.; visualization, H.B.; supervision, R.S. and A.J.; project administration, A.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Cantonal Hospital Zenica (protocol code 00-03-35-1125-12/22 on 27 December 2022).
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Baiden, F.; Anto-Ocrah, M.; Adjei, G.; Gyaase, S.; Abebrese, J.; Punguyire, D.; Owusu-Agyei, S.; Moresky, R.T. Head Injury Prevalence in a Population of Injured Patients Seeking Care in Ghana, West Africa. Front. Neurol. 2022, 13, 917294. [Google Scholar] [CrossRef] [PubMed]
- Dewan, M.C.; Rattani, A.; Gupta, S.; Baticulon, R.E.; Hung, Y.C.; Punchak, M.; Agrawal, A.; Adeleye, A.O.; Shrime, M.G.; Rubiano, A.M.; et al. Estimating the global incidence of traumatic brain injury. J. Neurosurg. 2018, 130, 1080–1097. [Google Scholar] [CrossRef] [PubMed]
- Maruya, J.; Yamamoto, K.; Wakai, M.; Kaneko, U. Brain abscess following transorbital penetrating injury due to bamboo fragments—Case report. Neurol. Med. Chir. 2002, 42, 143–146. [Google Scholar] [CrossRef] [PubMed]
- Koenen, L.; Waseem, M. Orbital Floor Fracture. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2023. [Google Scholar]
- Lethaus, B.; Weigl, S.; Kloss-Brandstätter, A.; Kloss, F.R.; Kessler, P.; Hölzle, F.; Bangard, C. Looking for landmarks in medial orbital trauma surgery. Int. J. Oral Maxillofac. Surg. 2013, 42, 209–213. [Google Scholar] [CrossRef]
- Ghosh, S.K.; Narayan, R.K. Fractures involving bony orbit: A comprehensive review of relevant clinical anatomy. Transl. Res. Anat. 2021, 24, 100125. [Google Scholar] [CrossRef]
- Xu, L.; Xu, F.; Li, L.; Liu, W.; Kit Leung, G.K.; Liu, B. The Surgical Strategies and Techniques of Transorbital Nonmissile Brain Injury. World Neurosurg. 2020, 144, e856–e865. [Google Scholar] [CrossRef]
- Reinshagen, K.L.; Massoud, T.F.; Cunnane, M.B. Anatomy of the Orbit. Neuroimaging Clin. N. Am. 2022, 32, 699–711. [Google Scholar] [CrossRef]
- Liu, S.; Yan, W.; Wang, G.; Zhao, R.; Qiu, H.; Cao, L.; Wang, H. Topographic Anatomy of the Zygomatico-Orbital Artery: Implications for Improving the Safety of Temporal Augmentation. Plast. Reconstr. Surg. 2021, 148, 19e–27e. [Google Scholar] [CrossRef]
- Apaydin, N.; Kendir, S.; Karahan, S.T. The Anatomical Relationships of the Ocular Motor Nerves with an Emphasis on Surgical Anatomy of the Orbit. Anat. Rec. 2019, 302, 568–574. [Google Scholar] [CrossRef]
- Alvis Miranda, H.; Castellar-Leones, S.M.; Elzain, M.A.; Moscote-Salazar, L.R. Brain abscess: Current management. J. Neurosci. Rural Pract. 2013, 4, S67–S81. [Google Scholar] [CrossRef]
- Prasetyo, E.; Oley, M.C.; Sumual, V.; Faruk, M. Transorbital-penetrating intracranial injury due to a homemade metal arrow: A case report. Ann. Med. Surg. 2020, 57, 183–189. [Google Scholar] [CrossRef]
- Kuromi, Y.; Sato, T.; Ando, H.; Matsumoto, Y.; Oda, K.; Ito, E.; Ichikawa, M.; Watanabe, T.; Sakuma, J.; Saito, K. Removal of bamboo fragments transorbitally penetrated into the cerebellum and temporal lobe 30 years after the injury. Neurol. Surg. 2012, 40, 979–983. [Google Scholar]
- Amano, K.; Kamano, S. Cerebellar abscess due to penetrating orbital wound. J. Comput. Assist. Tomogr. 1982, 6, 1163–1166. [Google Scholar] [CrossRef] [PubMed]
- Abdulbaki, A.; Al-Otaibi, F.; Almalki, A.; Alohaly, N.; Baeesa, S. Transorbital Craniocerebral Occult Penetrating Injury with Cerebral Abscess Complication. Case Rep. Ophthalmol. Med. 2012, 2012, 742186. [Google Scholar] [CrossRef] [PubMed]
- Abdulrazeq, H.; Walek, K.; Sampath, S.; Shaaya, E.; Beqiri, D.; Woo, A.; Sampath, P. Development of posttraumatic frontal brain abscess in association with an orbital roof fracture and odontogenic abscess: A case report. Surg. Neurol. Int. 2022, 13, 539. [Google Scholar] [CrossRef] [PubMed]
- Seider, N.; Gilboa, M.; Lautman, E.; Miller, B. Delayed presentation of orbito-cerebral abscess caused by pencil-tip injury. Ophthalmic Plast. Reconstr. Surg. 2006, 22, 316–317. [Google Scholar] [CrossRef]
- Di Roio, C.; Jourdan, C.; Mottolese, C.; Convert, J.; Artru, F. Craniocerebral injury resulting from transorbital stick penetration in children. Childs Nerv. Syst. 2000, 16, 503–506; discussion 507. [Google Scholar] [CrossRef]
- Aulino, J.M.; Gyure, K.A.; Morton, A.; Cole, J.W. Temporal lobe intraparenchymal retained foreign body from remote orbital trauma. AJNR Am. J. Neuroradiol. 2005, 26, 1855–1857. [Google Scholar]
- Santoreneos, S.; Hanieh, A.; Moore, L. ‘Splinter in the mind’: A case of penetrating periorbital injury. J. Clin. Neurosci. 1997, 4, 255–257. [Google Scholar] [CrossRef]
- De Andres Crespo, M.; McKinnon, C.; Halliday, J. What you need to know about brain abscesses. Br. J. Hosp. Med. 2020, 81, 1–7. [Google Scholar] [CrossRef]
- Brouwer, M.C.; van de Beek, D. Epidemiology, diagnosis, and treatment of brain abscesses. Curr. Opin. Infect. Dis. 2017, 30, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Seydoux, C.; Francioli, P. Bacterial brain abscesses: Factors influencing mortality and sequelae. Clin. Infect. Dis. 1992, 15, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Gadgil, N.; Patel, A.J.; Gopinath, S.P. Open craniotomy for brain abscess: A forgotten experience? Surg. Neurol. Int. 2013, 4, 34. [Google Scholar] [CrossRef]
- Mampalam, T.J.; Rosenblum, M.L. Trends in the management of bacterial brain abscesses: A review of 102 cases over 17 years. Neurosurgery 1988, 23, 451–458. [Google Scholar] [CrossRef]
- Ratnaike, T.E.; Das, S.; Gregson, B.A.; Mendelow, A.D. A review of brain abscess surgical treatment—78 years: Aspiration versus excision. World Neurosurg. 2011, 76, 431–436. [Google Scholar] [CrossRef]
- Cavuşoglu, H.; Kaya, R.A.; Türkmenoglu, O.N.; Colak, I.; Aydin, Y. Brain abscess: Analysis of results in a series of 51 patients with a combined surgical and medical approach during an 11-year period. Neurosurg. Focus 2008, 24, E9. [Google Scholar] [CrossRef]
- Elmallawany, M.; Ashry, A.; Alsawy, M.F. Endoscopic treatment of brain abscess. Surg. Neurol. Int. 2021, 12, 36. [Google Scholar] [CrossRef]
- Feraco, P.; Donner, D.; Gagliardo, C.; Leonardi, I.; Piccinini, S.; Del Poggio, A.; Franciosi, R.; Petralia, B.; van den Hauwe, L. Cerebral abscesses imaging: A practical approach. J. Popul. Ther. Clin. Pharmacol. 2020, 27, e11–e24. [Google Scholar] [CrossRef]
- Beculić, H.; Begagić, E.; Skomorac, R.; Jusic, A.; Čejvan, L. Seemingly innocuous trauma on the neurosurgical table: A rare case of brain abscess. In Proceedings of the 8th Annual Meeting of Serbian Neurosurgery Society, Beograd, Serbia, 8–10 December 2022. [Google Scholar]
- Hiraishi, T.; Tomikawa, M.; Kobayashi, T.; Kawaguchi, T. Delayed brain abscess after penetrating transorbital injury. Neurol. Surg. 2007, 35, 481–486. [Google Scholar]
- Rahman, N.U.; Jamjoom, A.; Jamjoom, Z.A.; Abu el-Asrar, A. Orbito-cranial injury caused by penetrating metallic foreign bodies: Report of two cases. Int. Ophthalmol. 1997, 21, 13–17. [Google Scholar] [CrossRef]
- Potapov, A.A.; Eropkin, S.V.; Kornienko, V.N.; Arutyunov, N.V.; Yeolchiyan, S.A.; Serova, N.K.; Kravtchuk, A.D.; Shahinian, G.G. Late diagnosis and removal of a large wooden foreign body in the cranio-orbital region. J. Craniofac. Surg. 1996, 7, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Rupa, R.; Vladimirov, T.; Pojskic, M.; Nimsky, C.; Voellger, B. Dynamics in the Neurotrauma Catchment Area of a German University Hospital during the COVID-19 Pandemic. Healthcare 2022, 10, 1376. [Google Scholar] [CrossRef] [PubMed]
- Efendić, A.; Bečulić, H.; Skomorac, R.; Jusić, A.; Selimović, E.; Begagić, E.; Juković-Bihorac, F. Infrequent case of cavum septi pellucidi empyema and principles of neurosurgical management: Case report and literature review. Medica Jadertina 2023, 53, 55–60. [Google Scholar] [CrossRef]
- Alic, F.; Jusic, A.; Beculic, H.; Barucija, N.; Ibrahimagic-Suljic, E. Successful management of subdural intracranial empyema linked with cerebral abscess as a consequence of pansinusitis. Medeniyet Med. J. 2018, 33, 140–143. [Google Scholar] [CrossRef]
- Martin-Canal, G.; Saavedra, A.; Asensi, J.M.; Suarez-Zarracina, T.; Rodriguez-Guardado, A.; Bustillo, E.; Fierer, J.; Carton, J.A.; Collazos, J.; Asensi, V. Meropenem monotherapy is as effective as and safer than imipenem to treat brain abscesses. Int. J. Antimicrob. Agents 2010, 35, 301–304. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).