The Prostate Is Not a Pill and Therefore Has No Capsule
Abstract
1. Introduction
2. Materials and Methods
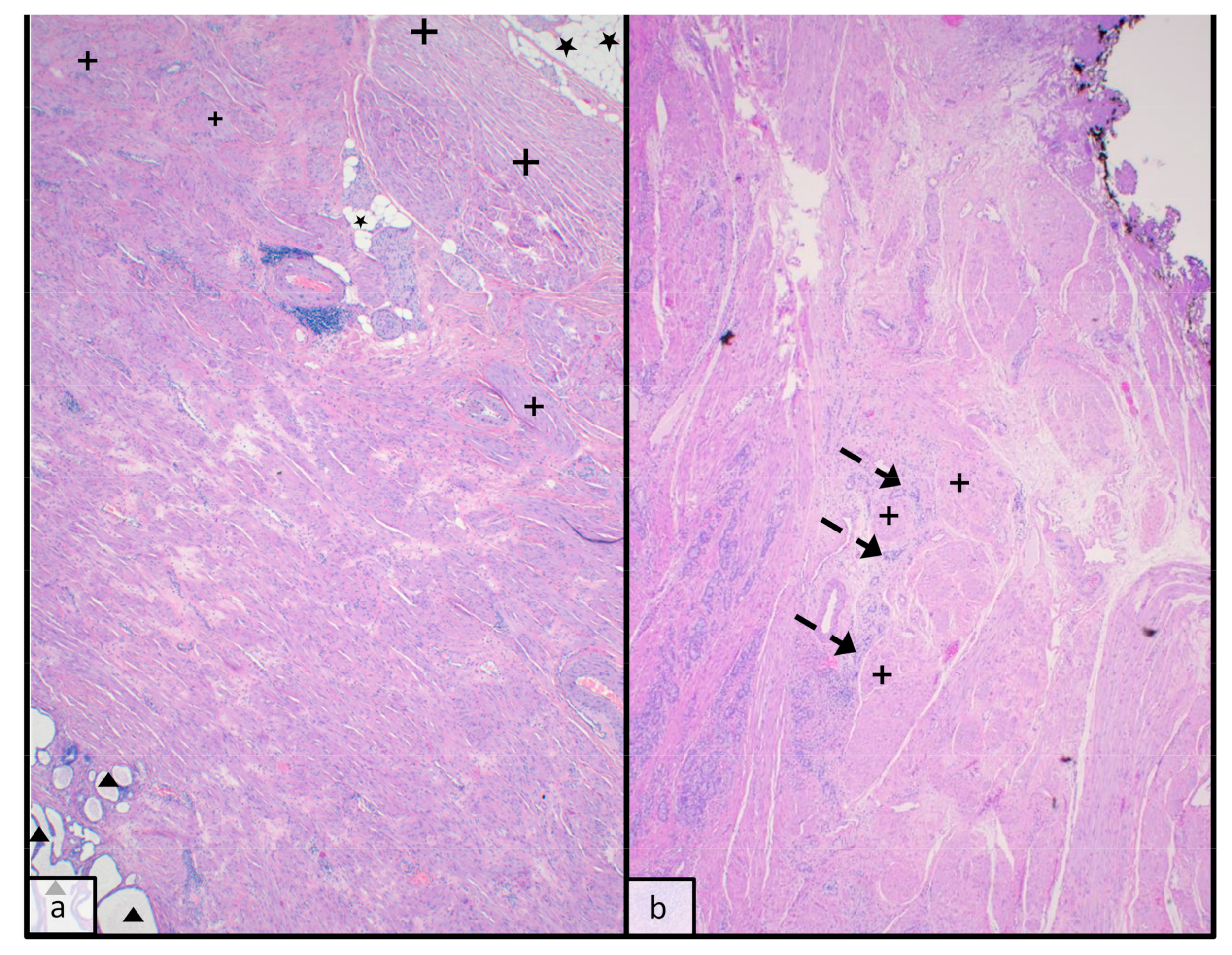
3. The Base and Anterior Surface of the Prostate
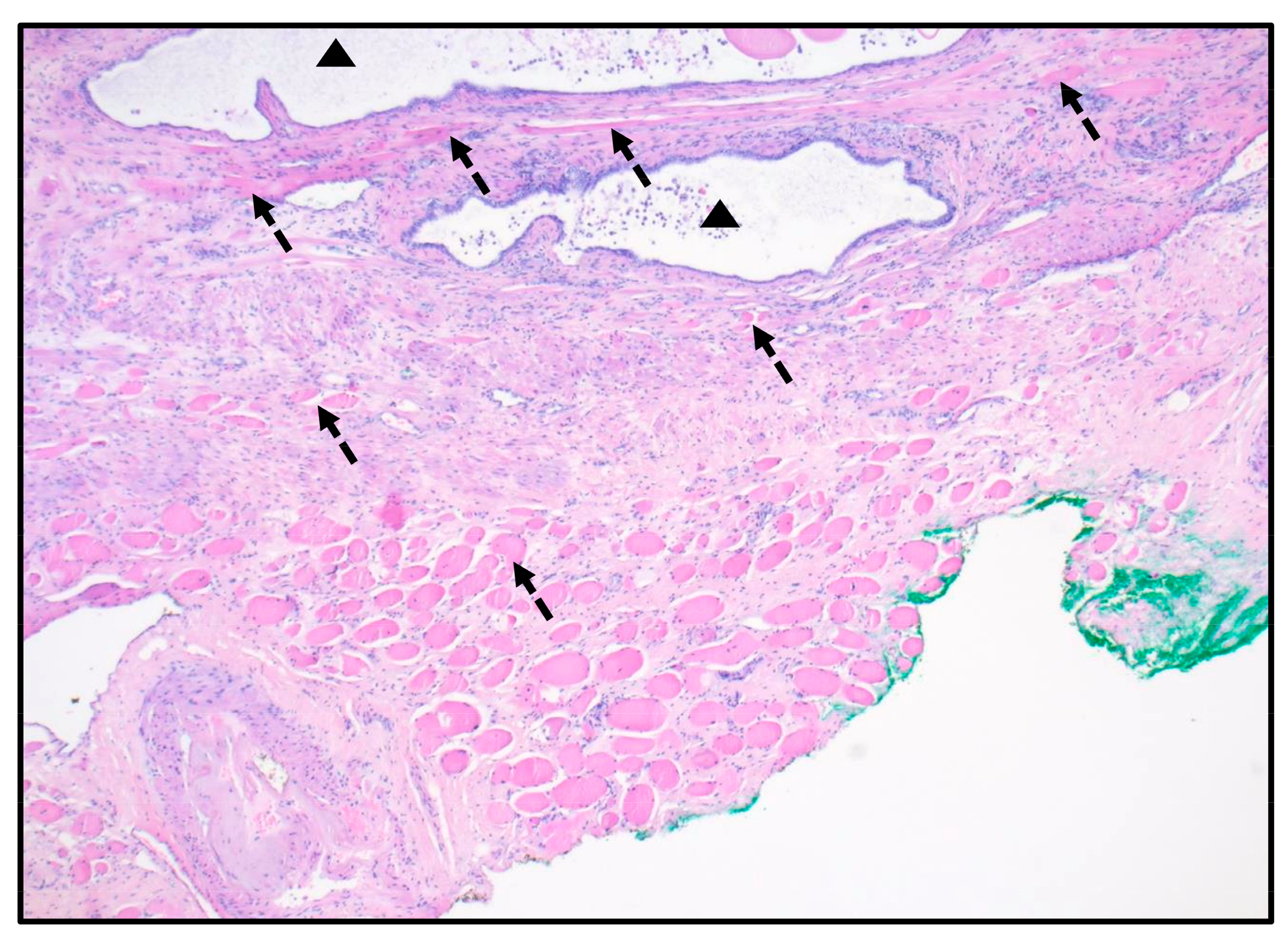
4. The Apex
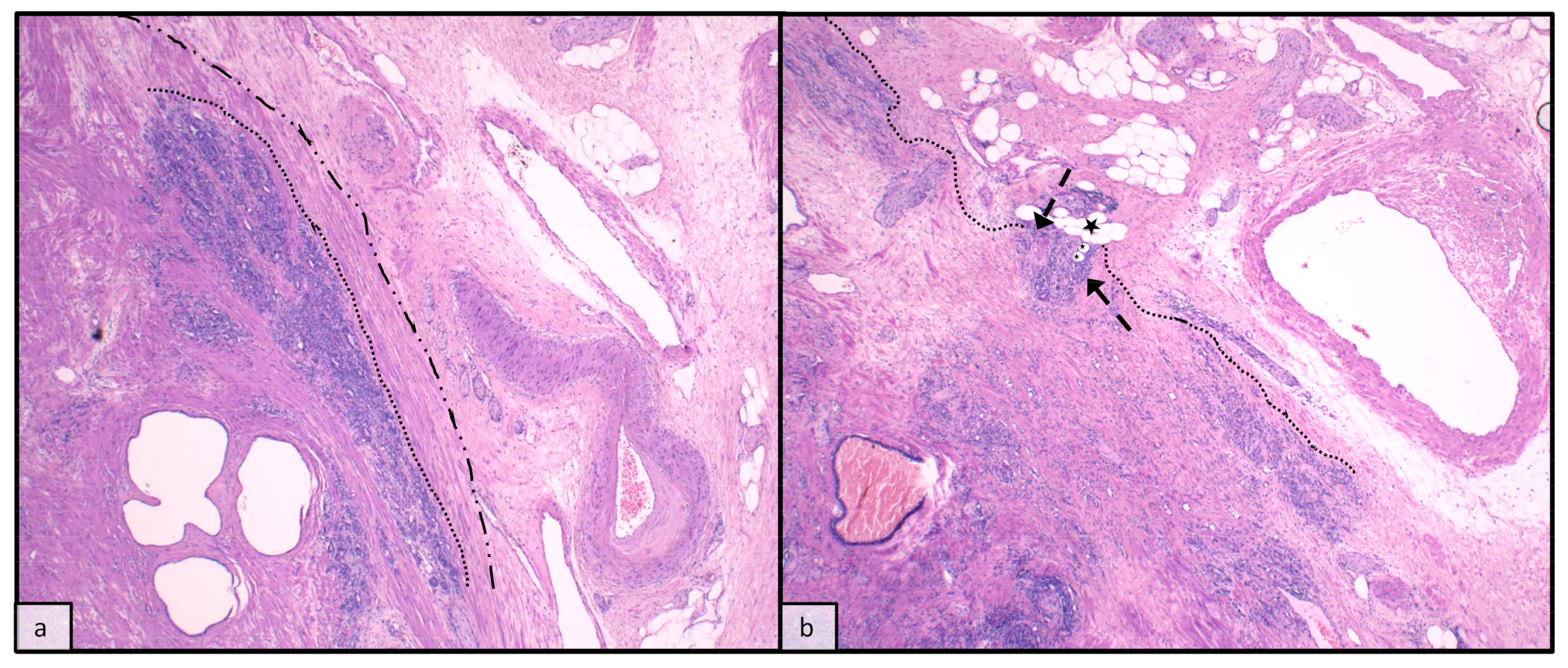
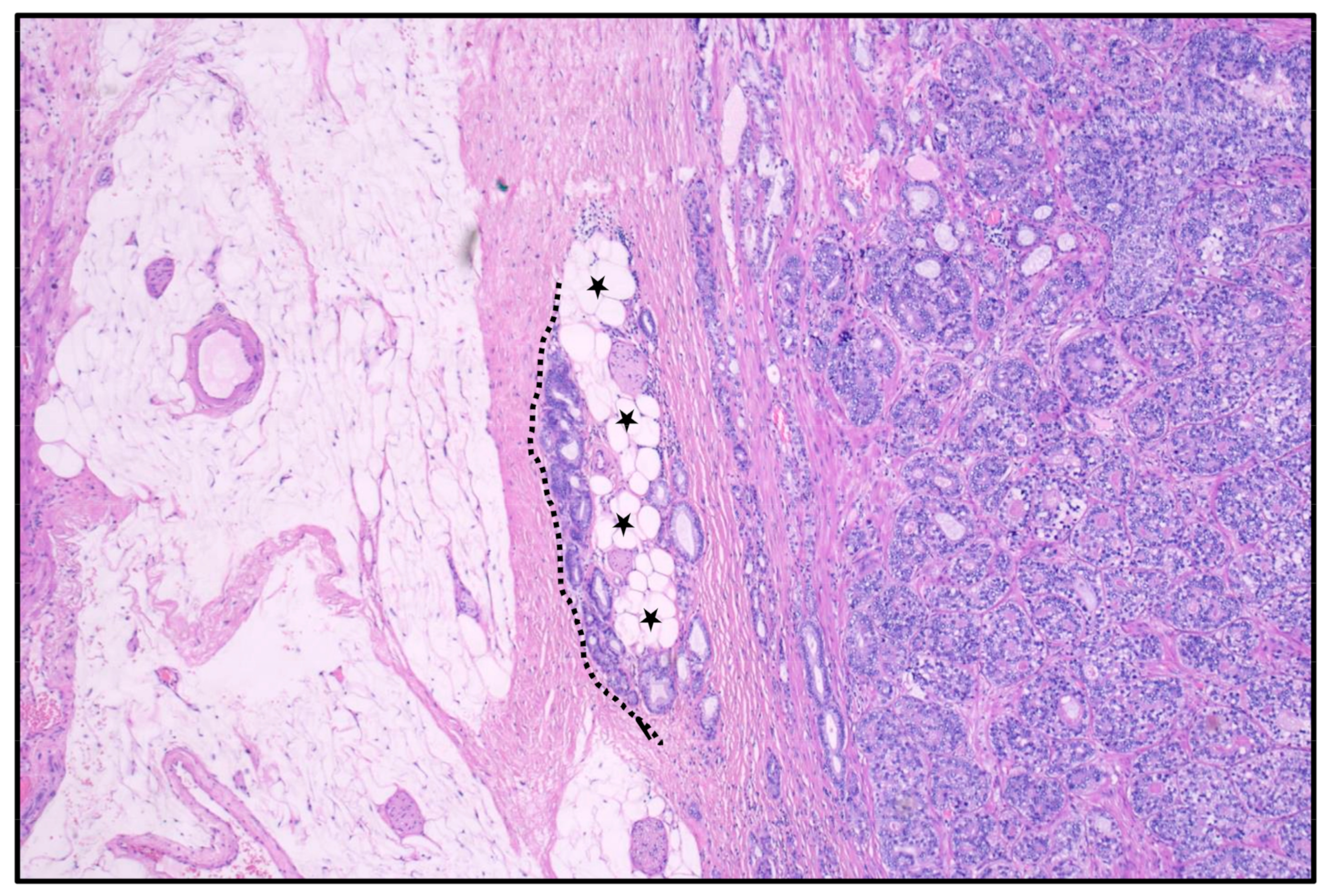
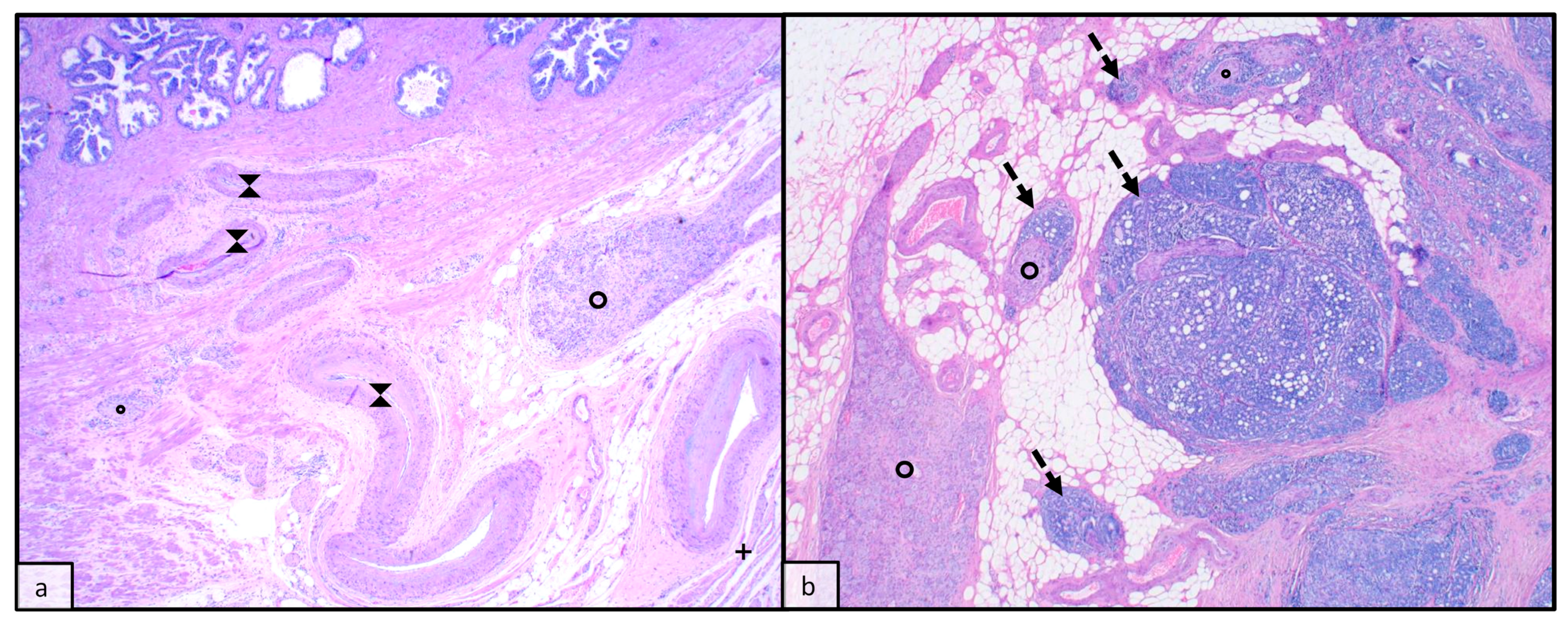
5. The Lateral and Dorsal Surface with Seminal Vesicles
6. Extraprostatic Growth and Oncological Implications
7. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mottet, N.; van den Bergh, R.C.N.; Briers, E.; Van den Broeck, T.; Cumberbatch, M.G.; De Santis, M.; Fanti, S.; Fossati, N.; Gandaglia, G.; Gillessen, S.; et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer—2020 Update. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur. Urol. 2021, 79, 243–262. [Google Scholar] [CrossRef] [PubMed]
- Ayala, A.G.; Ro, J.Y.; Babaian, R.; Troncoso, P.; Grignon, D.J. The prostatic capsule: Does it exist? Its importance in the staging and treatment of prostatic carcinoma. Am. J. Surg. Pathol. 1989, 13, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Magi-Galluzzi, C.; Evans, A.J.; Delahunt, B.; I Epstein, J.; Griffiths, D.F.; van der Kwast, T.H.; Montironi, R.; Wheeler, T.M.; Srigley, J.R.; Egevad, L.L.; et al. International society of urological pathology (ISUP) consensus conference on handling and staging of radical prostatectomy specimens. working group 3: Extraprostatic extension, lymphovascular invasion and locally advanced disease. Mod. Pathol. 2011, 24, 26–38. [Google Scholar] [CrossRef] [PubMed]
- Epstein, J.I.; Amin, M.; Boccon-Gibod, L.; Egevad, L.; Humphrey, P.A.; Mikuz, G.; Newling, D.; Nilsson, S.; Sakr, W.; Srigley, J.R.; et al. Prognostic factors and reporting of prostate carcinoma in radical prostatectomy and pelvic lymphadenectomy specimens. Scand. J. Urol. Nephrol. 2005, 39, 34–63. [Google Scholar] [CrossRef] [PubMed]
- Walz, J.; Burnett, A.L.; Costello, A.J.; Eastham, J.A.; Graefen, M.; Guillonneau, B.; Menon, M.; Montorsi, F.; Myers, R.P.; Rocco, B.; et al. A Critical Analysis of the Current Knowledge of Surgical Anatomy Related to Optimization of Cancer Control and Preservation of Continence and Erection in Candidates for Radical Prostatectomy. Eur. Urol. 2010, 57, 179–192. [Google Scholar] [CrossRef] [PubMed]
- Hoeh, B.; Wenzel, M.; Hohenhorst, L.; Köllermann, J.; Graefen, M.; Haese, A.; Tilki, D.; Walz, J.; Kosiba, M.; Becker, A.; et al. Anatomical Fundamentals and Current Surgical Knowledge of Prostate Anatomy Related to Functional and Oncological Outcomes for Robotic-Assisted Radical Prostatectomy. Front. Surg. 2022, 8, 825183. [Google Scholar] [CrossRef]
- Srigley, J.R.; Amin, M.B.; Epstein, J.I.; Grignon, D.J.; Humphrey, P.A.; Renshaw, A.A.; Wheeler, T.M. Updated protocol for the examination of specimens from patients with carcinomas of the prostate gland. Arch. Pathol. Lab. Med. 2006, 130, 936–946. [Google Scholar] [CrossRef]
- Fanghänel, J.; Pera, F.; Anderhuber, F. Waldeyer Anatomie des Menschen; Walter de Gruyter GmbH&Co.KG: Berlin, Germany, 2009. [Google Scholar]
- McKenny, J.K.; Fine, S.W. Prostate. In Histology for Pathologists; Mills, S., Ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2019; pp. 964–979. [Google Scholar]
- McKenny, J.K. Prostate and Seminal Vesicles. In Rosai and Ackerman’s Surgical Pathology; Elsevier Health Sciences: Amsterdam, The Netherlands, 2018; pp. 1097–1121. [Google Scholar]
- Walz, J.; Epstein, J.I.; Ganzer, R.; Graefen, M.; Guazzoni, G.; Kaouk, J.; Menon, M.; Mottrie, A.; Myers, R.P.; Patel, V.; et al. A Critical Analysis of the Current Knowledge of Surgical Anatomy of the Prostate Related to Optimisation of Cancer Control and Preservation of Continence and Erection in Candidates for Radical Prostatectomy: An Update. Eur. Urol. 2016, 70, 301–311. [Google Scholar] [CrossRef]
- FIPAT. Federative International Programme for Anatomical Terminology, 2nd ed. 2019. Available online: https://fipat.library.dal.ca/ta2/ (accessed on 4 July 2023).
- Byar, D.P.; Mostofi, F.K. Carcinoma of the prostate: Prognostic evaluation of certain pathologic features in 208 radical prostatectomies. Examined by the step-section technique. Cancer 1972, 30, 5–13. [Google Scholar] [CrossRef]
- Walsh, P.C.; Lepor, H. The role of radical prostatectomy in the management of prostatic cancer. Cancer 1987, 60, 526–537. [Google Scholar] [CrossRef]
- Tanaka, M.; Suzuki, N.; Nakatsu, H.; Murakami, S.; Matsuzaki, O.; Shimazaki, J. Significance of capsular attachment and invasion of cancer tissues in prostate cancer. Int. J. Urol. 2003, 10, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Rehman, A.; El-Zaatari, Z.M.; Han, S.H.; Shen, S.S.; Ayala, A.G.; Miles, B.; Divatia, M.K.; Ketcham, M.S.; Chung, B.M.; Rogers, J.T.; et al. Seminal vesicle invasion combined with extraprostatic extension is associated with higher frequency of biochemical recurrence and lymph node metastasis than seminal vesicle invasion alone: Proposal for further pT3 prostate cancer subclassification. Ann. Diagn. Pathol. 2020, 49, 151611. [Google Scholar] [CrossRef] [PubMed]
- Billis, A.; Meirelles, L.L.; Freitas, L.L.L.; Magna, L.A.; Reis, L.O.; Ferreira, U. Influence of focal and diffuse extraprostatic extension and positive surgical margins on biochemical progression following radical prostatectomy. Int. Braz. J. Urol. 2012, 38, 175–184. [Google Scholar] [CrossRef][Green Version]
- Jeong, B.C.; Chalfin, H.J.; Lee, S.B.; Feng, Z.; Epstein, J.I.; Trock, B.J.; Partin, A.W.; Humphreys, E.; Walsh, P.C.; Han, M. The relationship between the extent of extraprostatic extension and survival following radical prostatectomy. Eur. Urol. 2015, 67, 342–346. [Google Scholar] [CrossRef]
- Teramoto, Y.; Numbere, N.; Wang, Y.; Miyamoto, H. The Clinical Significance of pT3a Lesions as Well as Unilateral Versus Bilateral Invasion into the Seminal Vesicle in Men with pT3b Prostate Cancer. Arch. Pathol. Lab. Med. 2022. [Google Scholar] [CrossRef] [PubMed]
- McNeal, J.E.M.; Villers, A.A.M.; Redwine, E.A.B.; Freiha, F.S.M.; Stamey, T.A.M. Capsular penetration in prostate cancer: Significance for natural history and treatment. Am. J. Surg. Pathol. 1990, 14, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Epstein, J.I.; Carmichael, M.J.; Pizovt, G.; Walsh, P.C. Influence of capsular penetration on progression following radical prostatectomy: A study of 196 cases with long-term followup. J. Urol. 1993, 150, 135–141. [Google Scholar] [CrossRef]
- Wheeler, T.M.; Dillioglugil, O.; Kattan, M.W.; Arakawa, A.; Soh, S.; Suyama, K.; Ohori, M.; Scardino, P.T. Clinical and pathological significance of the level and extent of capsular invasion in clinical stage T1-2 prostate cancer. Hum. Pathol. 1998, 29, 856–862. [Google Scholar] [CrossRef]
- Sung, M.T.; Lin, H.; Koch, M.O.; Davidson, D.D.; Cheng, L. Radial distance of extraprostatic extension measured by ocular micrometer is an independent predictor of prostate-specific antigen recurrence: A new proposal for the substaging of pT3a prostate cancer. Am. J. Surg. Pathol. 2007, 31, 311–318. [Google Scholar] [CrossRef]
- Bostwick, D.G.; Foster, C.S. Predictive factors in prostate cancer: Current concepts from the 1999 College of American Pathologists Conference on Solid Tumor Prognostic Factors and the 1999 World Health Organization Second International Consultation on Prostate Cancer. Semin. Urol. Oncol. 1999, 17, 222–272. [Google Scholar]
- Kir, G.; Arikan, E.A.; Seneldir, H.; Ankarali, H.; Oznergiz, S.; Olgun, Z.C.; Yildirim, A. Determining the cut-off values of tumor diameter, degree of extraprostatic extension, and extent of surgical margin positivity with regard to biochemical recurrence of prostate cancer after radical prostatectomy. Ann. Diagn. Pathol. 2020, 44, 151431. [Google Scholar] [CrossRef] [PubMed]
- Farchoukh, L.; LaFramboise, W.A.; Nelson, J.B.; Bastacky, S.; Parwani, A.V.; Dhir, R. Multifocal Extraprostatic Extension of Prostate Cancer: A Third Subtype with Worse Prognosis Than Focal Prostate Cancer. Am. J. Clin. Pathol. 2020, 153, 548–553. [Google Scholar] [CrossRef] [PubMed]
- Park, C.K.; Chung, Y.S.; Choi, Y.D.; Ham, W.S.; Jang, W.S.; Cho, N.H. Revisiting extraprostatic extension based on invasion depth and number for new algorithm for substaging of pT3a prostate cancer. Sci. Rep. 2021, 11, 13952. [Google Scholar] [CrossRef] [PubMed]
- Samaratunga, H.; Egevad, L.; Yaxley, J.W.; Johannsen, S.; Le Fevre, I.K.; Perry-Keene, J.L.; Gianduzzo, T.; Chabert, C.; Coughlin, G.; Parkinson, R.; et al. Clinicopathologic Significance of Anterior Prostate Cancer: Comparison with Posterior Prostate Cancer in the Era of Multiparametric Magnetic Resonance Imaging. Am. J. Surg. Pathol. 2023, 47, 701–708. [Google Scholar] [CrossRef]
- Miyake, H.; Sakai, I.; Ishimura, T.; Hara, I.; Eto, H. Significance of cancer detection in the anterior lateral horn on systematic prostate biopsy: The effect on pathological findings of radical prostatectomy specimens. BJU Int. 2004, 93, 57–59. [Google Scholar] [CrossRef]
- Granja, M.; Pedraza, C.; Flórez, D.; Romero, J.; Palau, M.; Aguirre, D. Predicting extracapsular involvement in prostate cancer through the tumor contact length and the apparent diffusion coefficient. Radiologia 2017, 59, 313–320. [Google Scholar] [CrossRef]
- Li, W.; Shang, W.; Lu, F.; Sun, Y.; Tian, J.; Wu, Y.; Dong, A. Diagnostic Performance of Extraprostatic Extension Grading System for Detection of Extraprostatic Extension in Prostate Cancer: A Diagnostic Systematic Review and Meta-Analysis. Front. Oncol. 2022, 11, 792120. [Google Scholar] [CrossRef]
- Choi, M.H.; Kim, D.H.; Lee, Y.J.; Rha, S.E.; Lee, J.Y. Imaging features of the PI-RADS for predicting extraprostatic extension of prostate cancer: Systematic review and meta-analysis. Insights Imaging 2023, 14, 77. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kläger, J.; Wasinger, G.; Oszwald, A.; Compérat, E. The Prostate Is Not a Pill and Therefore Has No Capsule. Anatomia 2023, 2, 253-260. https://doi.org/10.3390/anatomia2030023
Kläger J, Wasinger G, Oszwald A, Compérat E. The Prostate Is Not a Pill and Therefore Has No Capsule. Anatomia. 2023; 2(3):253-260. https://doi.org/10.3390/anatomia2030023
Chicago/Turabian StyleKläger, Johannes, Gabriel Wasinger, André Oszwald, and Eva Compérat. 2023. "The Prostate Is Not a Pill and Therefore Has No Capsule" Anatomia 2, no. 3: 253-260. https://doi.org/10.3390/anatomia2030023
APA StyleKläger, J., Wasinger, G., Oszwald, A., & Compérat, E. (2023). The Prostate Is Not a Pill and Therefore Has No Capsule. Anatomia, 2(3), 253-260. https://doi.org/10.3390/anatomia2030023






