Diagnosis of Psychosocial Risk Determinants and the Prioritization of Organizational Intervention Objects among Medical Occupational Groups in a Public Healthcare Institution †
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Stress and Occupational Groups
3.2. Psychosocial Risk Determinants and Occupational Group
- —
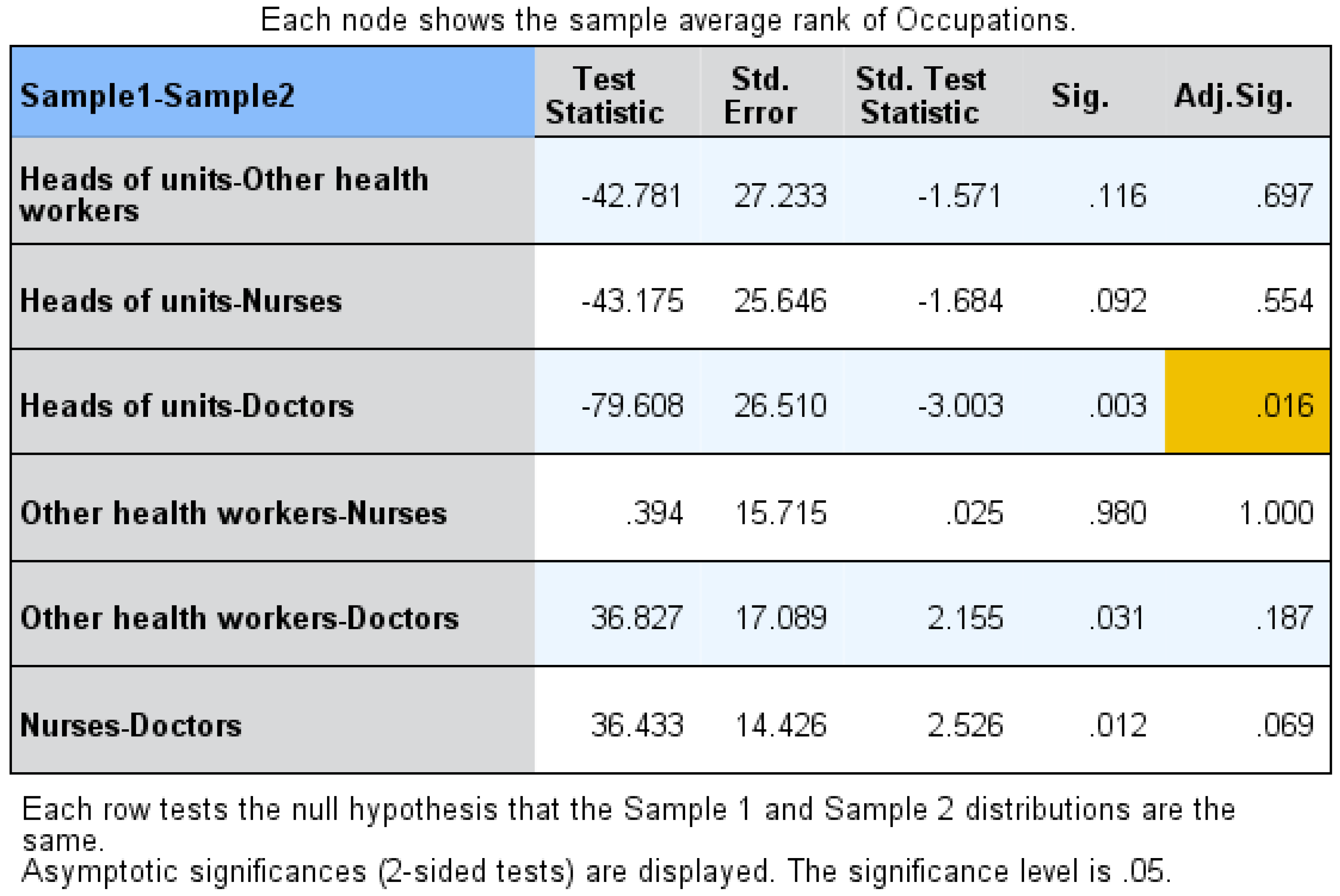
- Work overload scores between doctors (263.63) and heads of the units (187.41) (p = 0.028) and doctors and other health workers (211.15) (p = 0.015) (Figure 2).
- —
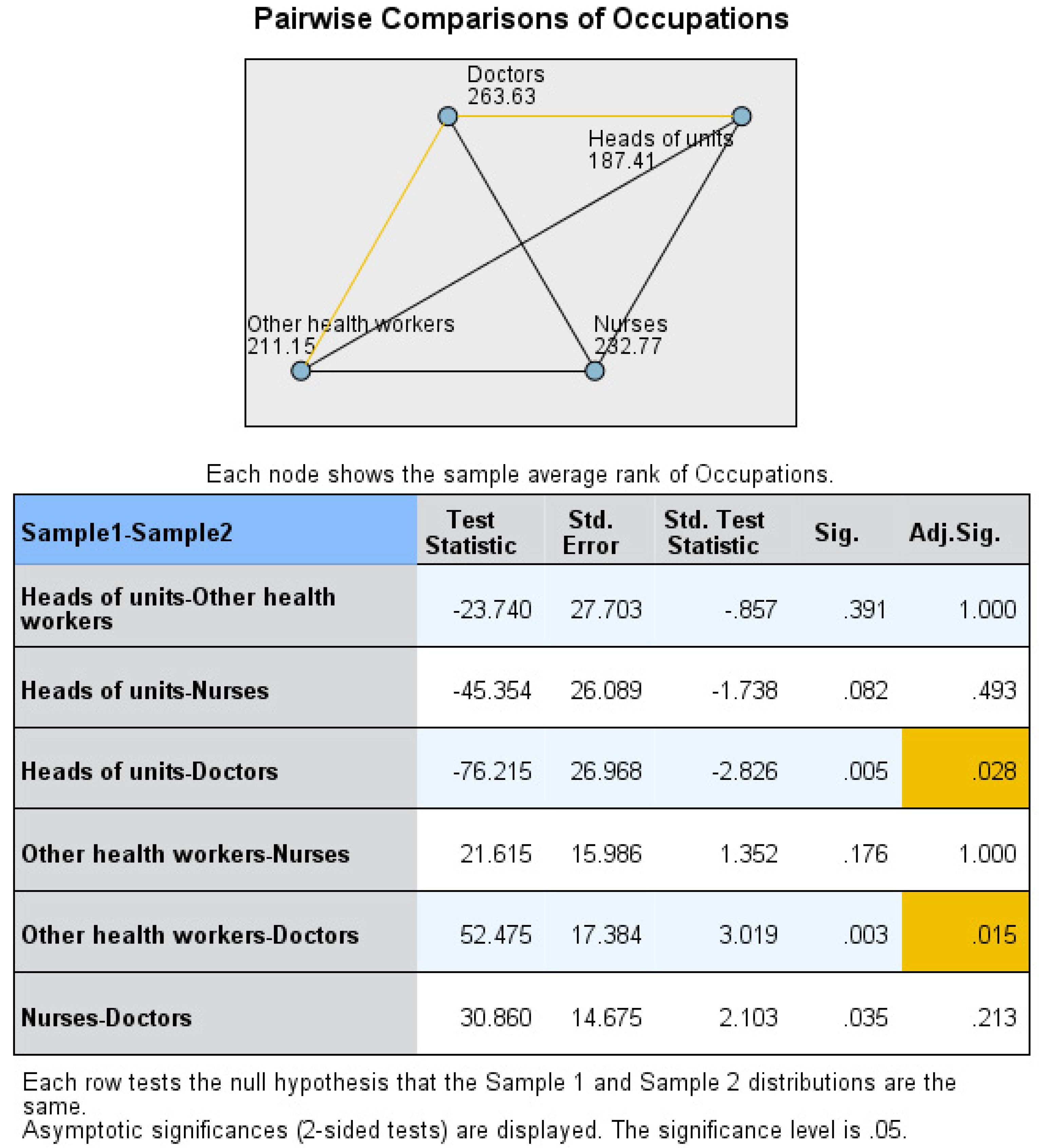
- Overtime scores between doctors (263.42) and other health workers (200.73) (p = 0.001) (Figure 3).
- —
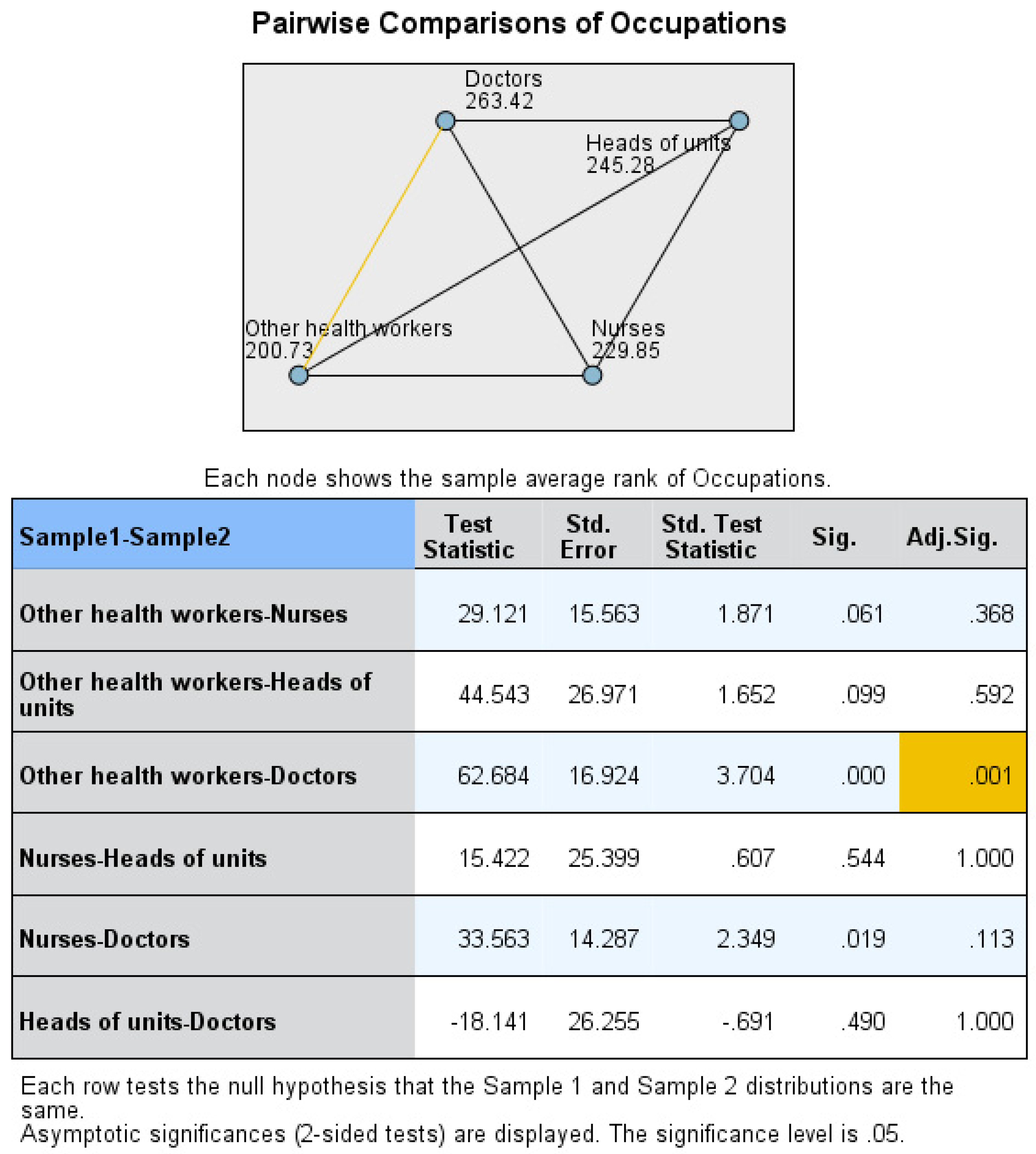
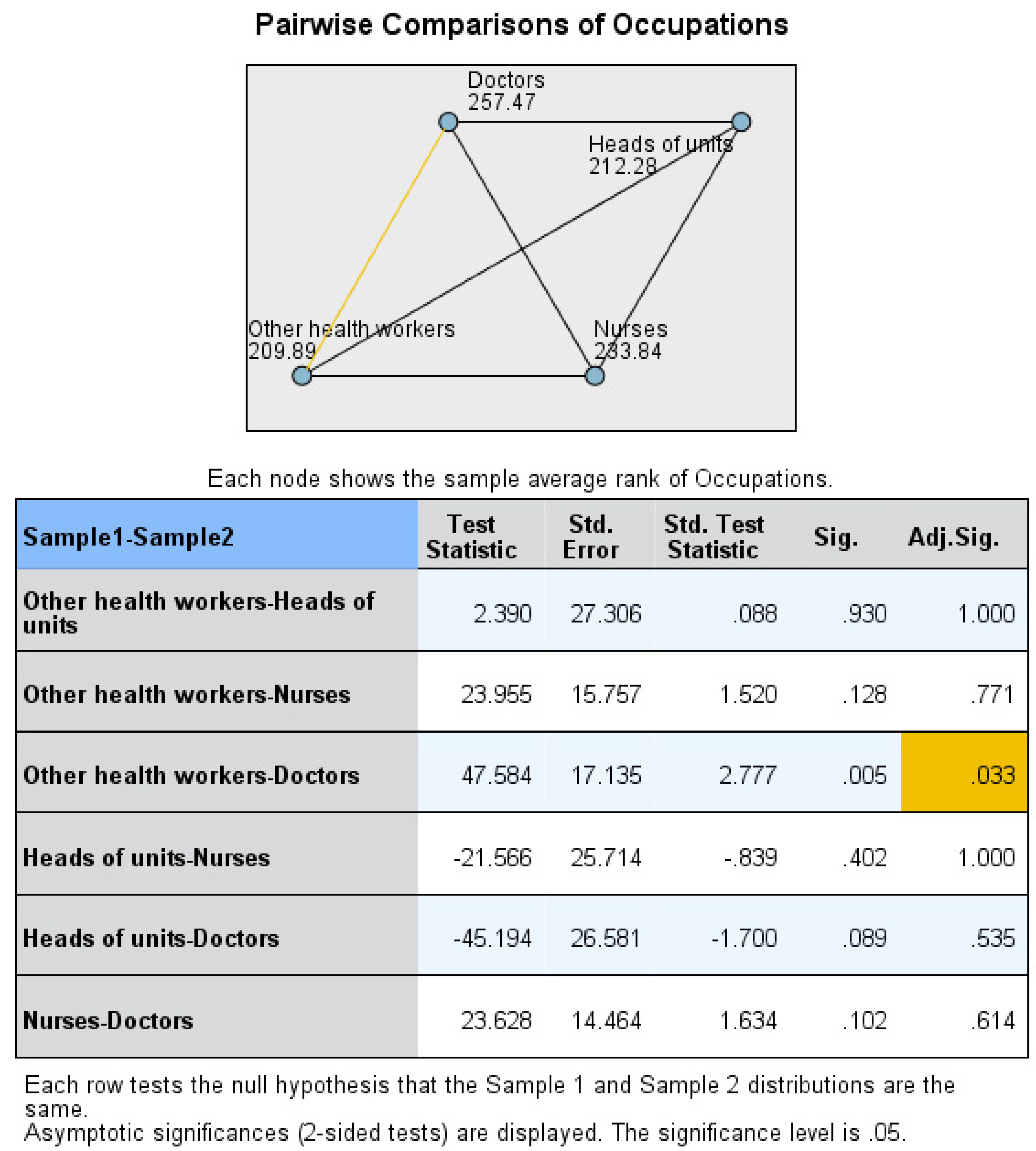
- Tight deadlines scores between doctors (257.47) and other health workers (209.89) (p = 0.033) (Figure 4).
- —
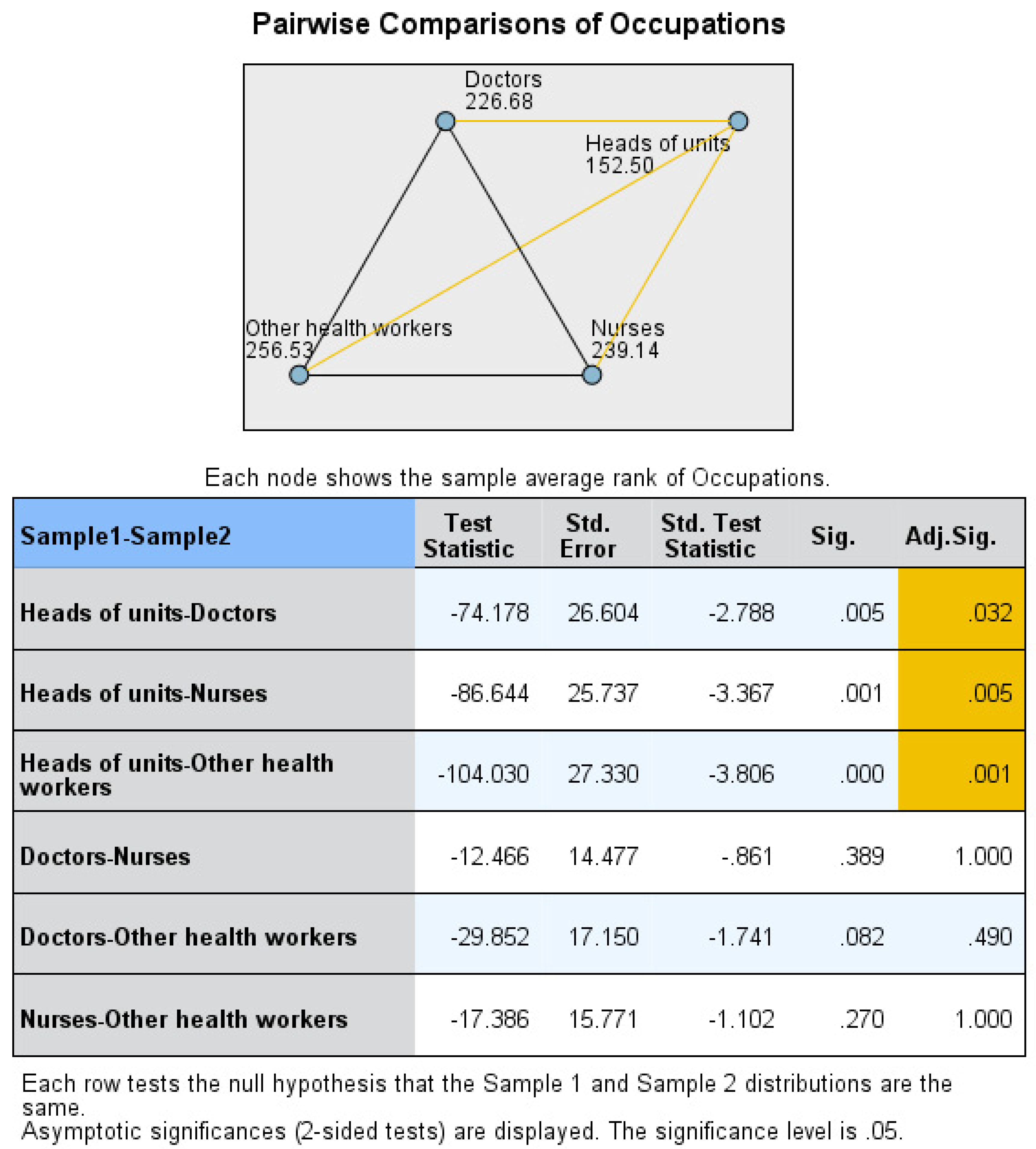
- Unclear role scores between heads of the units (152.50) and doctors (226.68) (p = 0.032), heads of the units and nurses (239.14) (p = 0.005), and heads of the units and other health workers (256.53) (p = 0.001) (Figure 5).
- —
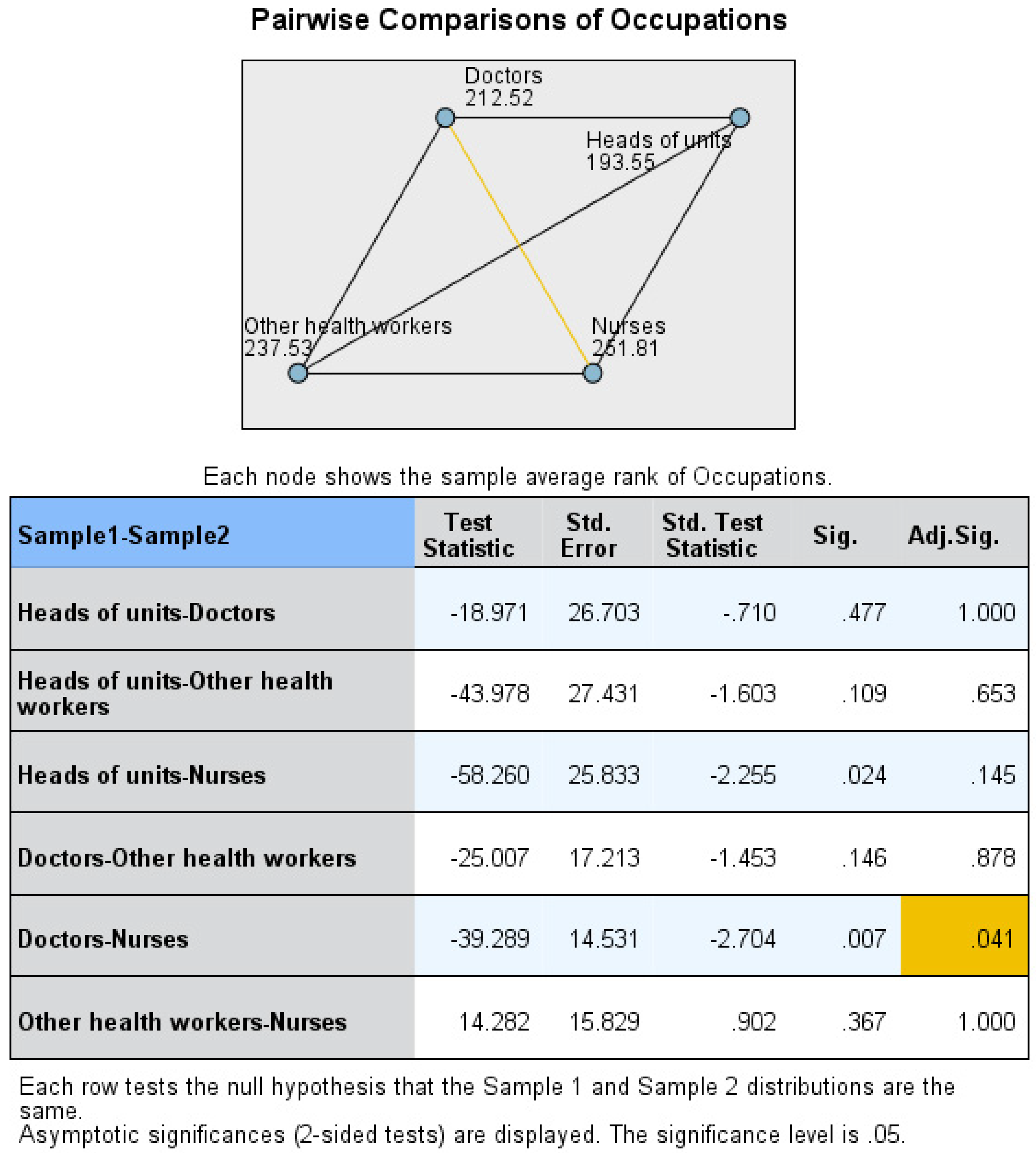
- Being under-skilled scores between doctors (212.52) and nurses (251.81) (p = 0.041) (Figure 6).
- —
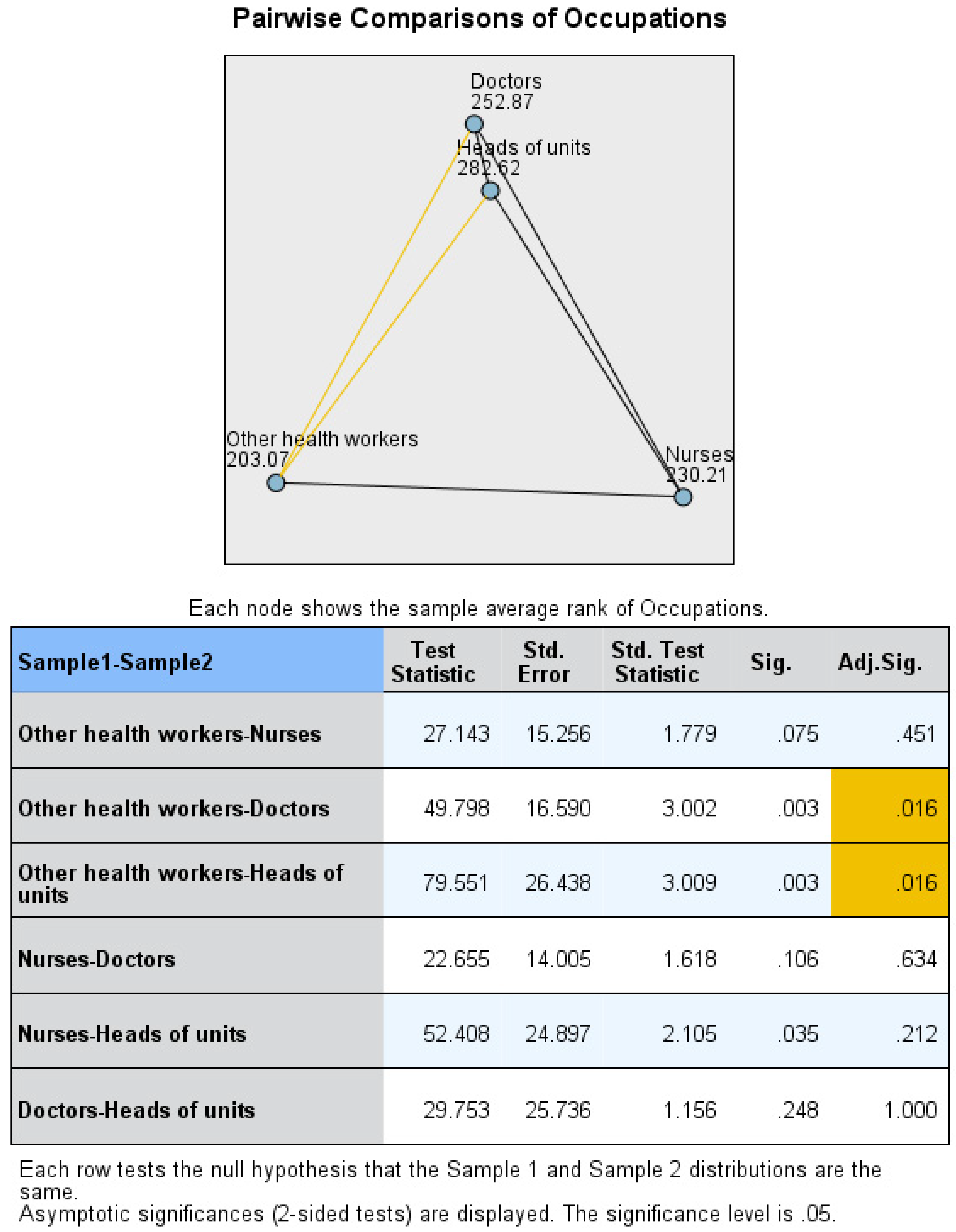
- Responsibility scores between other health workers (203.07) and doctors (252.87) (p = 0.016) and other health workers and heads of the units (282.62) (p = 0.016) (Figure 7).
3.3. Organizational Intervention Objects and Occupational Group
- —
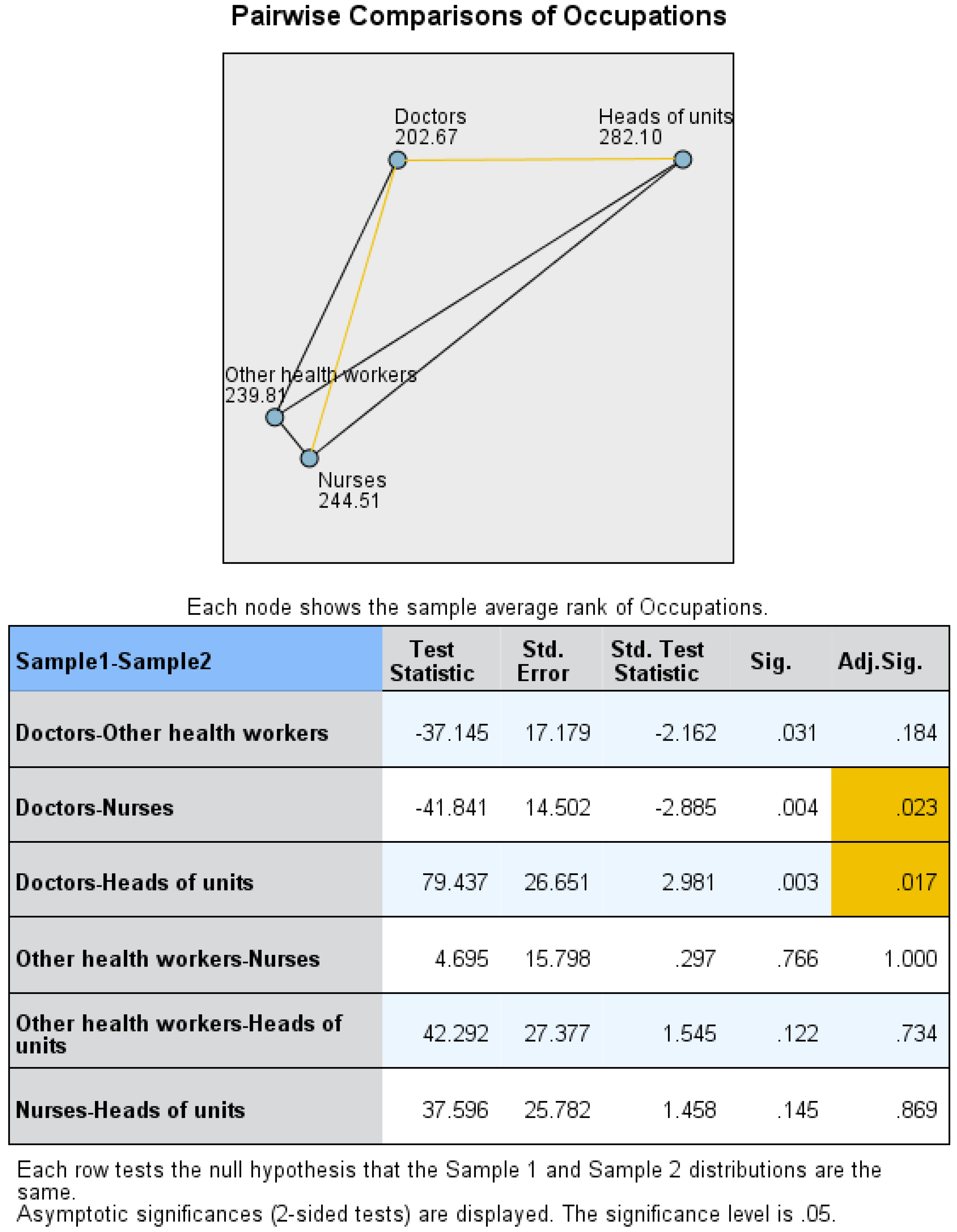
- Work–life balance scores between doctors (202.67) and heads of the units (282.10) (p = 0.017), and doctors and nurses (244.51) (p = 0.023) (Figure 8).
- —
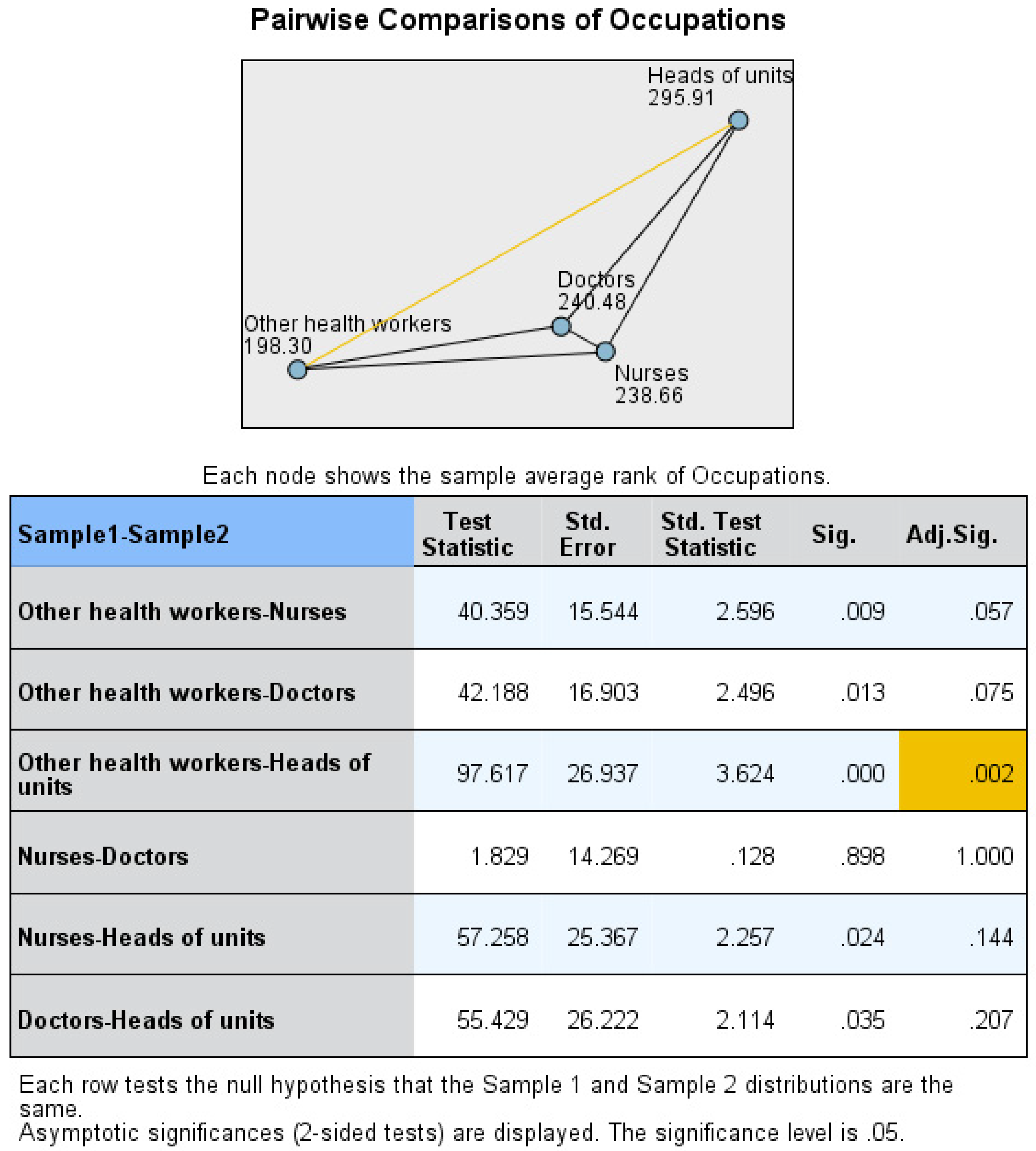
- Skills/abilities matching to the job demands scores between heads of the units (295.91) and other health workers (198.30) (p = 0.002) (Figure 9).
- —
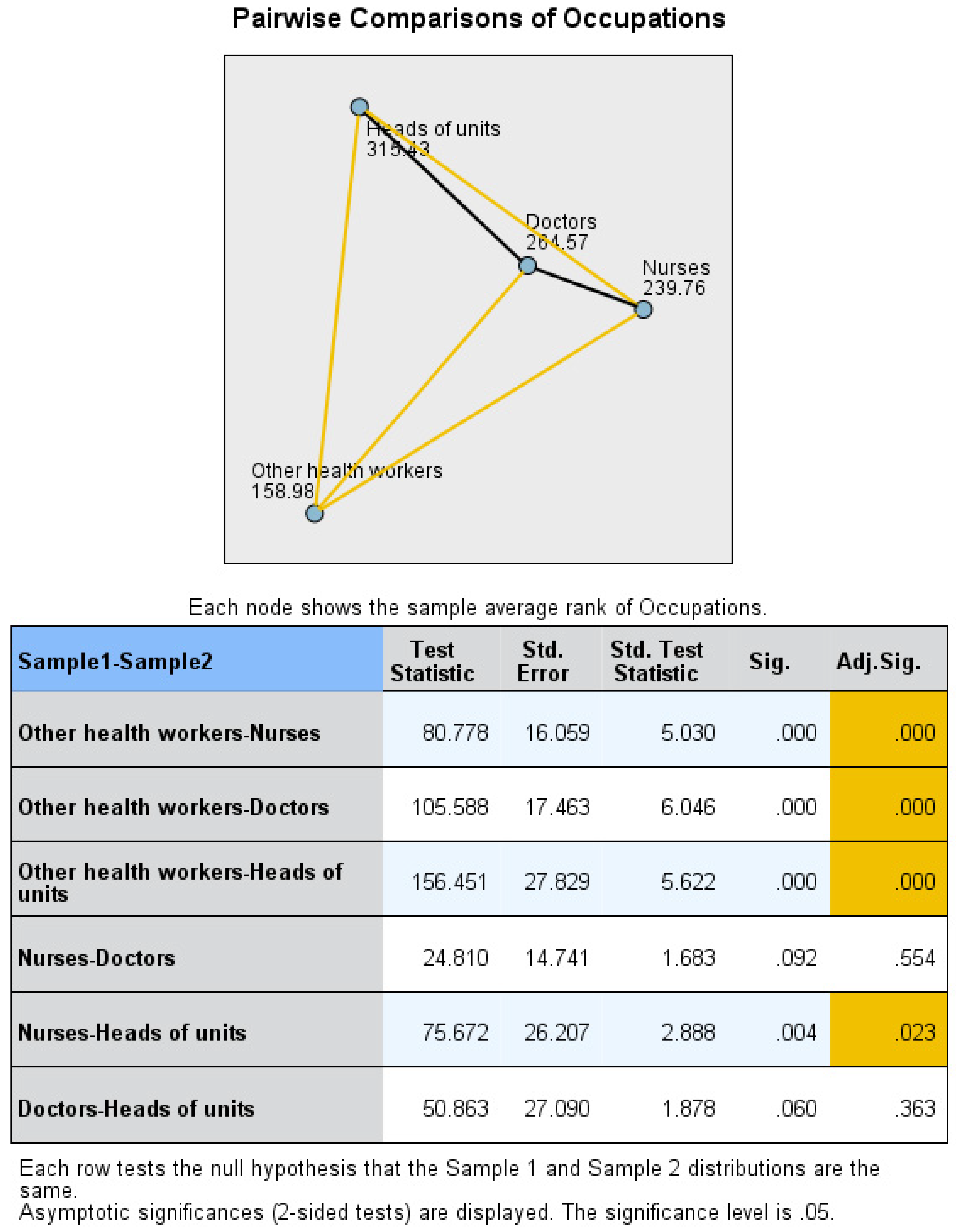
- Variety of tasks scores between other health workers (158.98) and doctors (264.57) (p < 0.001), other health workers and heads of the units (315.43) (p < 0.001), and other health workers and nurses (239.76) (p < 0.001); heads of the units and nurses (p = 0.023) (Figure 10).
- —
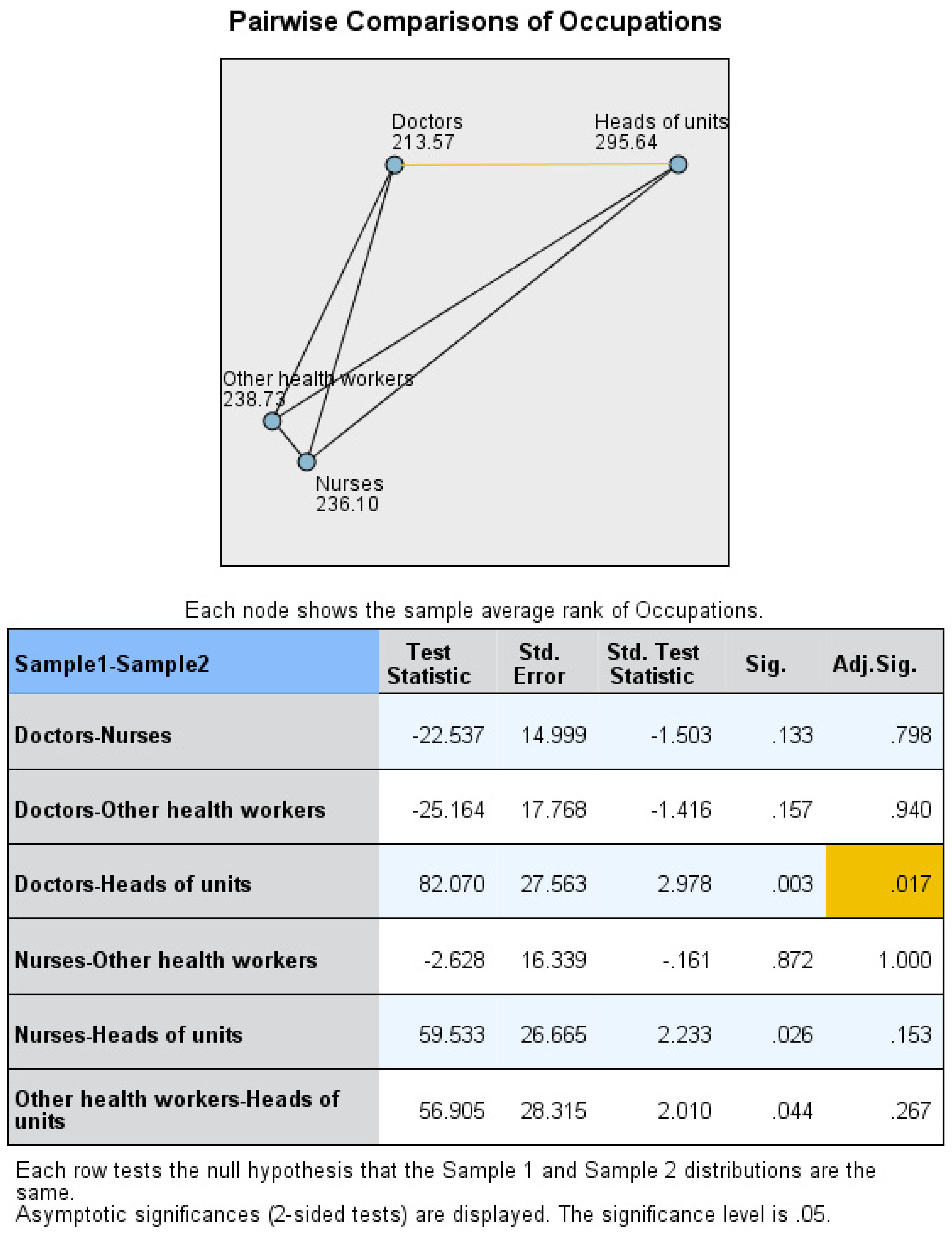
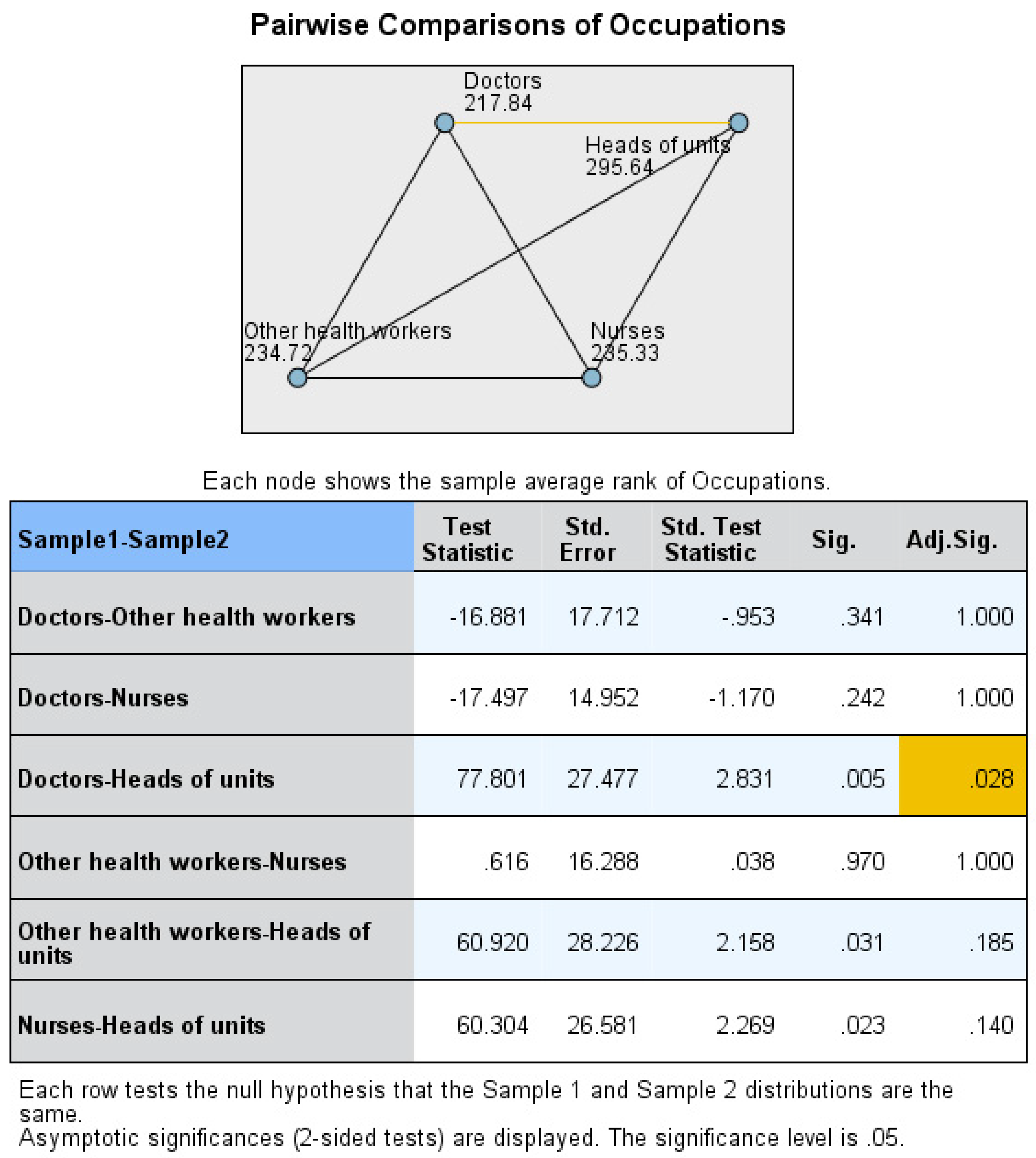
- Social support: scores between doctors (213.57) and heads of the units (295.64) (p = 0.017) (Figure 11).
- —
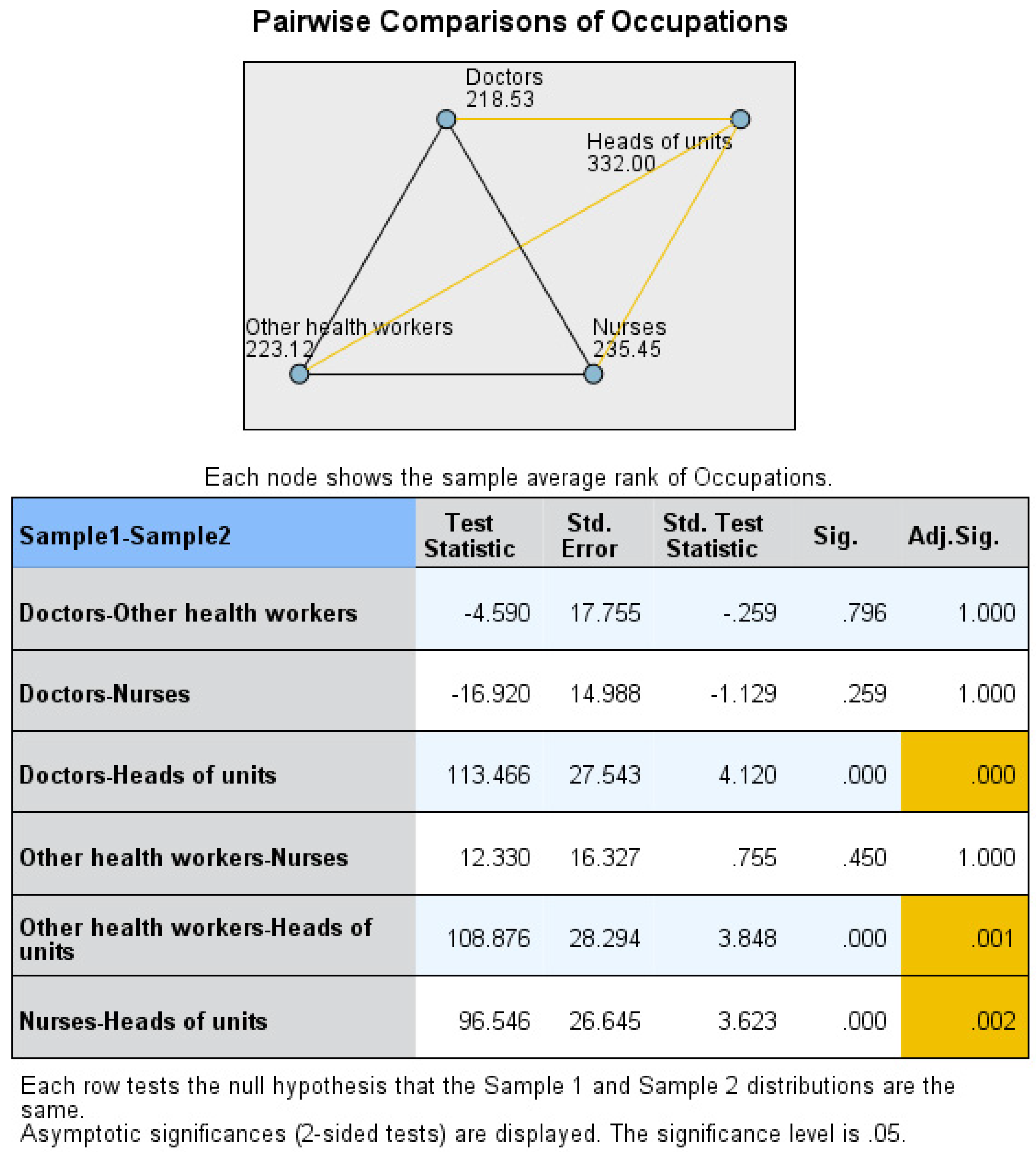
- Organizational support scores between heads of the units (332.00) and doctors (218.53) (p < 0.001), heads of the units and nurses (235.45) (p = 0.002), and heads of the units and other health workers (223.12) (p = 0.001) (Figure 12).
- —
- Participation in decision making scores between heads of the units (295.64) and doctors (217.84) (p = 0.028) (Figure 13).
- —
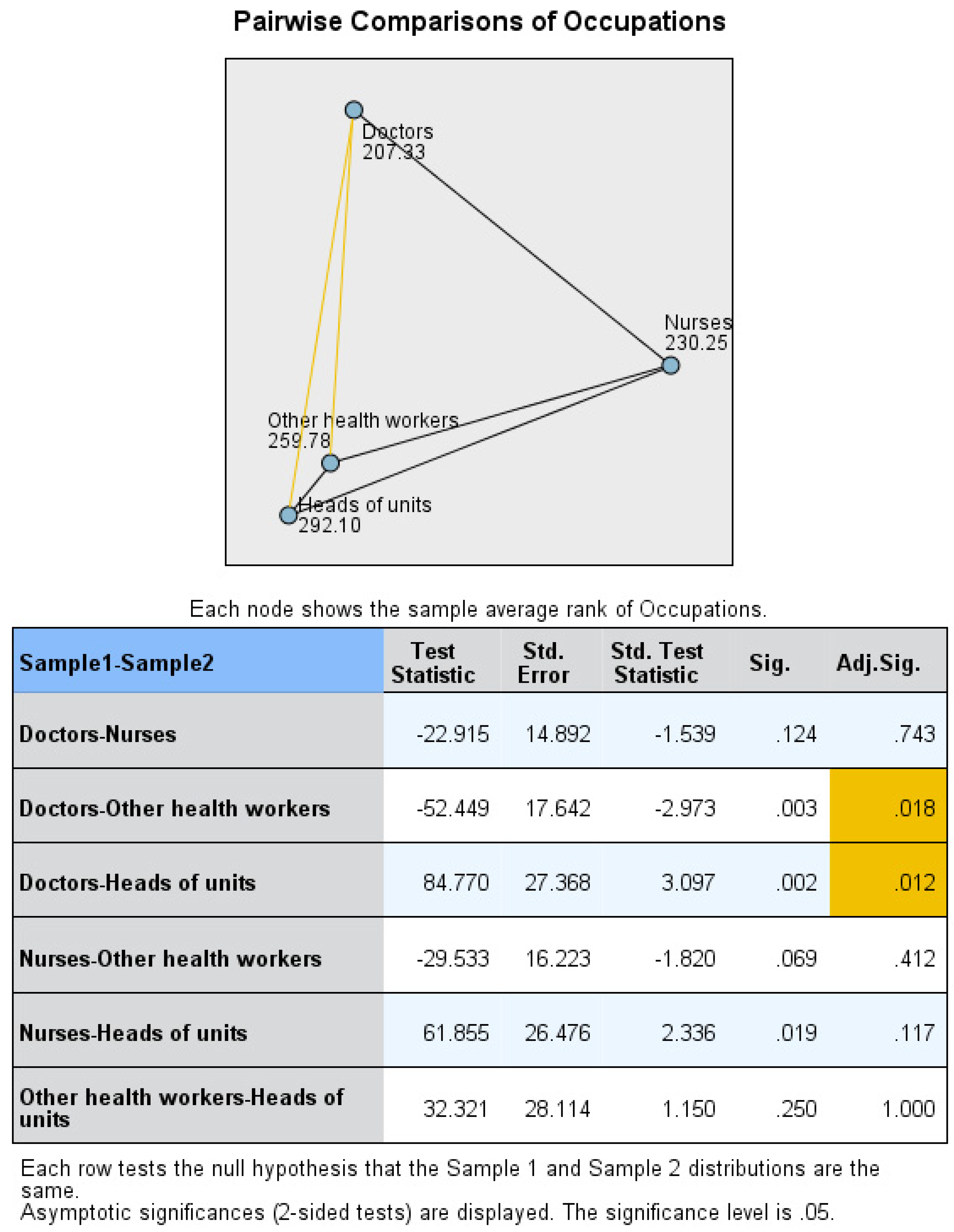
- Justice of reward scores between doctors (207.33) and heads of the units (292.10) (p = 0.012), and doctors and other health workers (259.78) (p = 0.018) (Figure 14).
- —
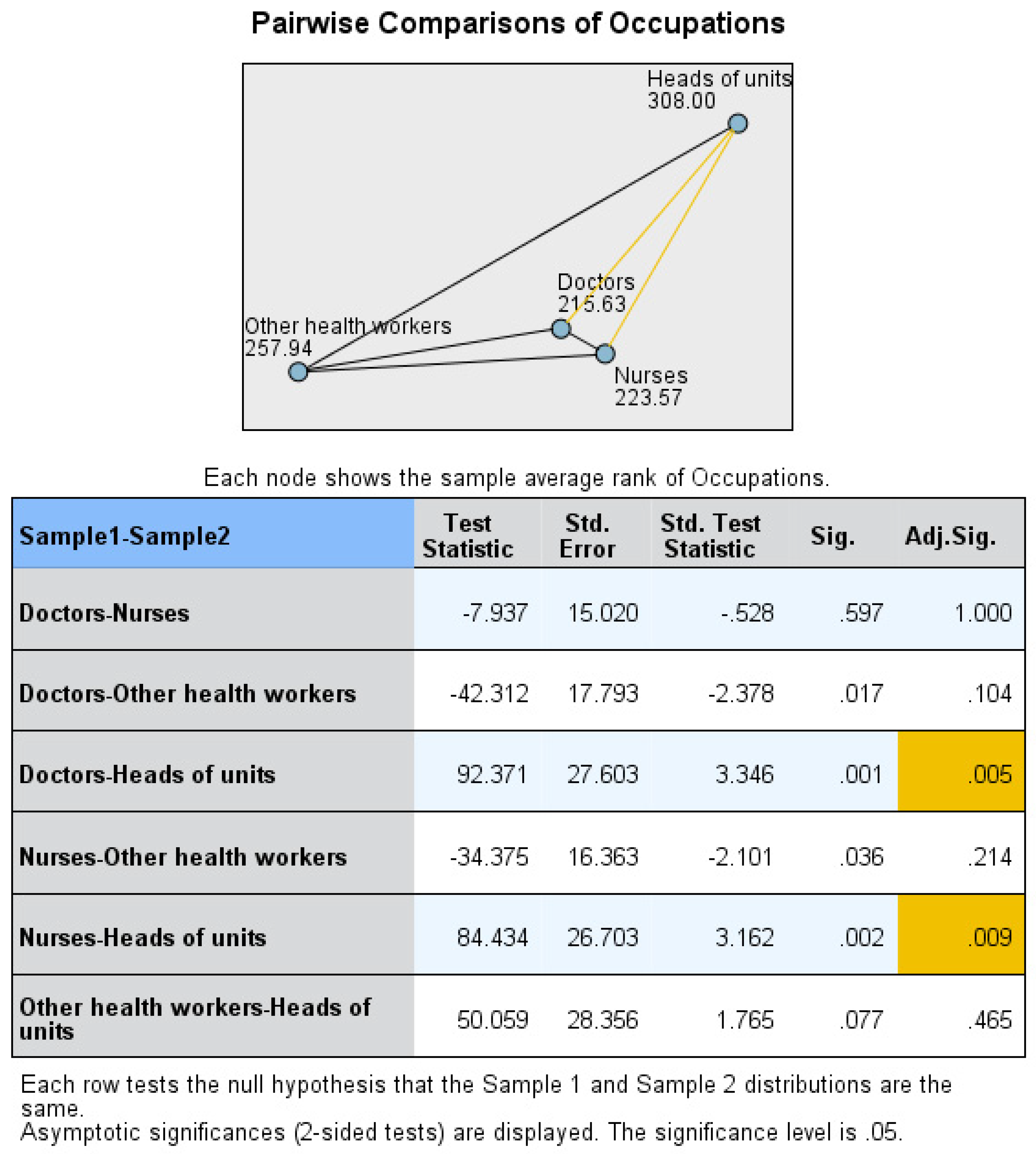
- Manager feedback scores between heads of the units (308.00) and doctors (215.63) (p = 0.005) and heads of the units and nurses (223.57) (p = 0.009) (Figure 15).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- European Comission. Flash Eurobarometer 398, Working Conditions. 2014. Available online: https://ec.europa.eu/commfrontoffice/publicopinion/flash/fl_398_en.pdf (accessed on 10 January 2019).
- Third European Survey of Enterprises on New and Emerging Risks (ESENER 3). European Agency for Safety and Health at Work. 2019. Available online: https://osha.europa.eu/lt/publications/thirdeuropean-survey-enterprises-new-and-emerging-risks-esener-3/view (accessed on 22 January 2020).
- Fishta, A.; Backé, E.M. Psychosocial stress at work and cardiovascular diseases: An overview of systematic reviews. Int. Arch. Occup. Environ. Health 2015, 88, 997–1014. [Google Scholar] [CrossRef] [PubMed]
- Allesøe, K.; Hundrup, Y.A.; Thomsen, J.F.; Osler, M. Psychosocial work environment and risk of ischaemic heart disease in women: The Danish Nurse Cohort Study. Occup. Environ. Med. 2010, 67, 318–322. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Jarczok, M.N.; Loerbroks, A.; Schöllgen, I.; Siegrist, J.; Bosch, J.A.; Wilson, M.G.; Mauss, D.; Fischer, J.E. Work stress is associated with diabetes and prediabetes: Crosssectional results from the MIPH Industrial Cohort Studies. Int. J. Behav. Med. 2013, 20, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Bonde, J.P. Psychosocial factors at work and risk of depression: A systematic review of the epidemiological evidence. Occup. Environ. Med. 2008, 65, 438–445. [Google Scholar] [CrossRef]
- Tomioka, K.; Morita, N.; Saeki, K.; Okamoto, N.; Kurumatani, N. Working hours, occupational stress and depression among physicians. Occup. Med. 2011, 61, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Åkerstedt, T.; Garefelt, J.; Richter, A.; Westerlund, H.; Magnusson Hanson, L.L.; Sverke, M.; Kecklund, G. Work and sleep—A prospective study of psychosocial work factors, physical work factors, and work scheduling. Sleep 2015, 38, 1129–1136. [Google Scholar] [CrossRef]
- Bernal, D.; Campos-Serna, J.; Tobias, A.; Vargas-Prada, S.; Benavides, F.G.; Serra, C. Work-related psychosocial risk factors and musculoskeletal disorders in hospital nurses and nursing aides: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2015, 52, 635–648. [Google Scholar] [CrossRef] [PubMed]
- Sterud, T.; Tynes, T. Work-related psychosocial and mechanical risk factors for low back pain: A 3-year follow-up study of the general working population in Norway. Occup. Environ. Med. 2013, 70, 296–302. [Google Scholar] [CrossRef]
- Béjean, S.; Sultan-Taïeb, H. Modeling the economic burden of diseases imputable to stress at work. Eur. J. Health Econ. 2005, 6, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Florea, R. Individual and Organizational Implications of Work-related Stress. Econ. Transdiscip. Cogn. 2006, 19, 28–33. [Google Scholar]
- Gilboa, S.; Shirom, A.; Fried, Y.; Cooper, C. A meta-analysis of work demand stressors and job performance: Examining main and moderating effects. Pers. Psychol. 2008, 61, 227–271. [Google Scholar] [CrossRef]
- Cox, T.; Taris, T.W.; Nielsen, K. Organizational interventions: Issues and challenges. Work Stress 2010, 24, 217–218. [Google Scholar] [CrossRef]
- Johnson, S.; Cox, T.; Cartwright, S.; Donald, I.; Taylor, P.; Millet, C. The experience of work-related stress across occupations. J. Manag. Psychol. 2005, 20, 178–187. [Google Scholar] [CrossRef]
- Chan, K.B.; Lai, G.; Ko, Y.C.; Boey, K.W. Work stress among six professional groups: The Singapore experience. J. Soc. Sci. Med. 2000, 50, 1415–1432. [Google Scholar] [CrossRef]
- Dudutienė, D.; Juodaitė-Račkauskienė, A.; Stukas, R. Developing Stress Management Programs in a Public Primary Healthcare Institution: Should We Consider Health Workers’ Sociodemographic Groups? Medicina 2020, 56, 162. [Google Scholar] [CrossRef] [PubMed]
- Scott, T.; Mannion, R.; Davies, H.T.O.; Marshall, M.N. Implementing culture change in health care: Theory and practice. Int. J. Qual. Health Care 2003, 15, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Bandzienė, A. Kompleksinis Streso Darbe Valdymas (Complex Stress Management at Work). Ph.D. Thesis, ISM Vadybos ir Ekonomikos Universitetas, Kaunas, Lithuania, 2009. [Google Scholar]
- Žutautienė, R.; Radišauskas, R.; Ustinavičienė, R.; Kirvaitienė, J.; Rakutytė, K. Gydytojų psichosocialiniai darbo aplinkos veiksniai ir jų sąsajos su gyvenimo kokybe. Sveikatos Mokslai 2019, 29, 53–59. [Google Scholar] [CrossRef][Green Version]
- Heponiemi, T.; Kouvonen, A.; Aalto, A.M.; Elovainio, M. Psychosocial factors in GP work: The effects of taking a GP position or leaving GP work. Eur. J. Public Health 2012, 23, 361–366. [Google Scholar] [CrossRef][Green Version]
- Nikolic, D.; Višnjic, A. Mobbing and Violence at Work as Hidden Stressors and Work Ability among Emergency Medical Doctors in Serbia. Medicina 2020, 56, 31. [Google Scholar] [CrossRef] [PubMed]
- Boran, A.; Shawaheen, M.; Khader, Y.; Amarin, Z.; Rice, V.H. Work-related stress among health professionals in northern Jordan. Occup. Med. 2012, 62, 145–147. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health Care Management (NIHCM) Foundation. Physician Burnout & Moral Injury: The Hidden Health Care Crisis. 2021. Available online: https://nihcm.org/publications/physician-burnout-suicide-the-hidden-health-care-crisis (accessed on 22 November 2021).
- National Academy of Medicine: Action Collaborative on Clinician well-Being and Resilience. 2021. Available online: https://nam.edu/initiatives/clinician-resilience-and-well-being/ (accessed on 25 November 2021).
- Moustaka, E.; Constantinidis, T.C. Sources and effects of Work-related stress in nursing. Health Sci. J. 2010, 4, 210–216. [Google Scholar]
- Currie, G.; Finn, R.; Martin, G. Role transition and the interaction of relational and social identity: New nursing roles in the English NHS. Organ Stud. 2010, 31, 941–961. [Google Scholar] [CrossRef]
- Chen, T.; Hao, S.; Ding, K.; Feng, X.; Li, G.; Liang, X. The impact of organizational support on employee performance. Empl. Relat. 2020, 42, 166. [Google Scholar] [CrossRef]
- Institute of Work, Health & Organisations. Towards the Development of a European Framework for Psychosocial Risk Management at the Workplace; Institute of Work, Health & Organisations: Nottingham, UK, 2008. [Google Scholar]
| Groups | N | Mean Rank | χ2(3) | p |
|---|---|---|---|---|
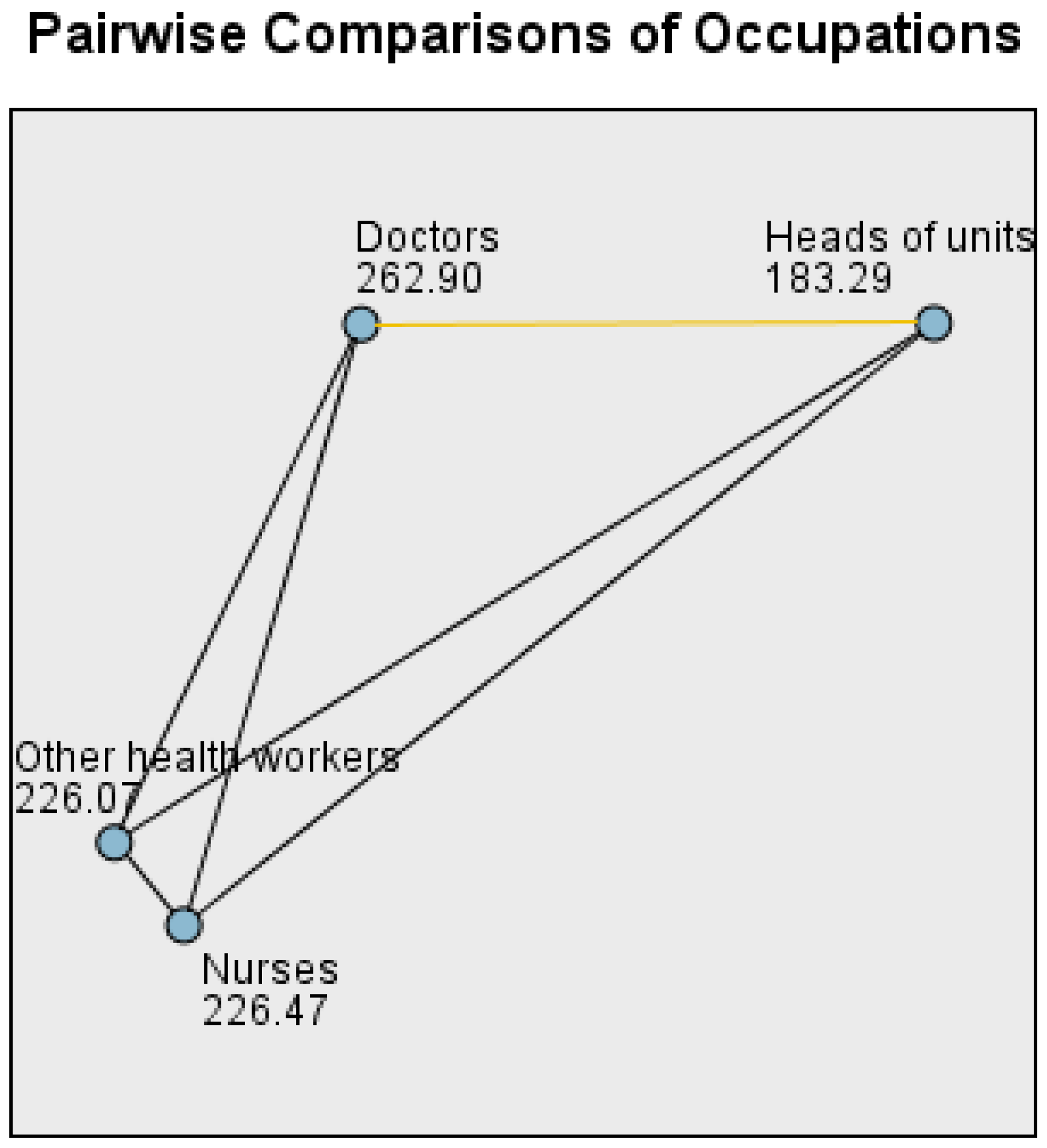
| Heads of units | 29 | 183.29 | 12.14 | <0.01 |
| Doctors | 132 | 262.90 | ||
| Nurses | 205 | 226.47 | ||
| Other health workers | 101 | 226.07 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dudutienė, D.; Račkauskienė, A.J.; Stukas, R. Diagnosis of Psychosocial Risk Determinants and the Prioritization of Organizational Intervention Objects among Medical Occupational Groups in a Public Healthcare Institution. Med. Sci. Forum 2021, 6, 8. https://doi.org/10.3390/IECMD2021-10312
Dudutienė D, Račkauskienė AJ, Stukas R. Diagnosis of Psychosocial Risk Determinants and the Prioritization of Organizational Intervention Objects among Medical Occupational Groups in a Public Healthcare Institution. Medical Sciences Forum. 2021; 6(1):8. https://doi.org/10.3390/IECMD2021-10312
Chicago/Turabian StyleDudutienė, Daiva, Audronė Juodaitė Račkauskienė, and Rimantas Stukas. 2021. "Diagnosis of Psychosocial Risk Determinants and the Prioritization of Organizational Intervention Objects among Medical Occupational Groups in a Public Healthcare Institution" Medical Sciences Forum 6, no. 1: 8. https://doi.org/10.3390/IECMD2021-10312
APA StyleDudutienė, D., Račkauskienė, A. J., & Stukas, R. (2021). Diagnosis of Psychosocial Risk Determinants and the Prioritization of Organizational Intervention Objects among Medical Occupational Groups in a Public Healthcare Institution. Medical Sciences Forum, 6(1), 8. https://doi.org/10.3390/IECMD2021-10312







