Abstract
We have developed an approach to reprogramming immune cells by inhibiting the MAPK/ERK pathway through MEKi and the PD-1/PD-L1 immune checkpoint signaling pathway. We hypothesized that reprogramming of spleen CD8+ T-cells could also create a population of immune cells with high antitumor activity. We reprogrammed CD8+ T-cells derived from the spleen of C57BL/6 mice (rsCD8+T-cells). In the orthotopic LLC model, cell therapy with rsCD8+T-cells increased the amount of proliferating CD8+ and CD4+ T-cells in blood and lung tissue from mice. The amount of cancer stem cells (CSC) decreased in the blood and lung of mice treated with rsCD8+ T-cells. A morphological study revealed a decrease in the number of metastases in lung tissue. The antitumor effects of rsCD8+T-cells are based on the activation of the host immune response by increasing the populations of CD8+ and CD4+ T-cells and apoptosis of CSCs.
1. Introduction
Despite advances in therapeutic strategies, our understanding of risks, and its immunologic control, lung cancer is the second most common malignancy [1]. Understanding the mechanisms of immunosuppression development has formed the basis for modern cancer immunotherapy. Immunotherapy has successfully been used in cancer treatment in the last time. However, some immunotherapies, including immune checkpoint inhibitors, have demonstrated limited efficacy in solid tumors [2]. It is noted that additional activation of the immune system after immunotherapy increases the risk of developing autoimmune diseases [2]. Reprogramming T-cell metabolism is critical for enhancing the antitumor immune response. However, immunotherapy has been mainly on CD8 T-cells because they can directly kill cancer cells [3]. In recent years, the role of CD4 T-cells in anti-tumor immunity has received more attention. However, the exact mechanism is less clear.
With the advent of different reprogramming strategies mediated, it was interesting to investigate whether reprogramming can be used to induce the activity of CD8+ T-cells from dissimilar tissues. We have previously shown that reprogrammed CD8+ T-cells isolated from mouse bone marrow have high cytotoxicity and anti-tumor effects [4]. It has been proposed that spleen T-cell reprogramming could be used to rejuvenate exhausted CD8+ T-cells too. In this study, we assessed the effects of cell therapy with reprogrammed CD8+ T-cells isolated from the spleen (rsCD8+ cells) in a Lewis lung cancer (LLC) orthotopic lung tumor.
2. Materials and Methods
2.1. Animals
Male C57BL/6 mice that were 8–10 weeks old (nursery of the Experimental BioModels Department of the Tomsk National Research Medical Center) were selected.
2.2. Lewis Lung Carcinoma Cell Line and Tumor Model
Lewis lung cancer (LLC) cells were purchased from the CLS Cell Lines (Service, GmbH, Germany) [4]. The orthotopic model of LLC was described previously [4]. d7 after LLC cell implantation animals were euthanized.
2.3. Isolation of Mononuclear Cells
Mononuclear cells from blood, lungs, and spleen were isolated, as described previously [4,5].
2.4. Flow Cytometry
The surface markers and intracellular receptors on mononuclear cells derived from blood and lungs were analyzed via flow cytometry [4]. The cell suspension was stained with fluorophore-conjugated monoclonal antibodies: CD3 PerCP, CD4 FITC, CD8 BV510, CD44 APC-Cy™7, CD62L APC, CD90 APC, EGF (F4/80) Alexa Fluor® 647, CD274 (PD-L1) PE, CCR7 PE, and CD279 (PD-1) BV421 and for the intracellular staining Sox2 PE and Ki-67 APC (all—BD Biosciences, San Jose, CA, USA). The relevant isotype controls were used. FACSCanto II flow cytometer with FACSDiva software was used for analysis.
2.5. Magnetic Separation of CD8+ T-Cells
The magnetic sorting of mononuclear cells from the spleen was performed using EasySepTM Mouse Naive CD8+ T-Cell Isolation Kit (StemCell Technologies, Vancouver, BC, Canada).
2.6. Reprogramming of Spleen CD8+ T-Cells
The CD8+ T-cells isolated from the spleen were reprogrammed, as described earlier [4]. The reprogramming of CD8+T-cells was performed using monoclonal antibodies nivolumab (Bristol-Myers Squibb Company, New York, NY, USA) and MEK1/2i (Sigma-Aldrich, St. Louis, MO, USA). To evaluate the population, stability was carried out in vitro exhaustion of rsCD8+ T-cells [3].
2.7. CD8+ T-Cells Injection
To assess the migration of rsCD8+ T-cells into the lungs of mice with LLC, CFSE-labeled rsCD8+T-cells were injected intravenously at 106 cells in 0.1 mL of PBS per dose. The rsCD8+ T-cells were stained by CFSE, as described earlier [4]. To assess the antitumor and antimetastatic activity, rsCD8+T-cells were injected intravenously into mice with LLC (1 × 106 cells in 0.1 mL of PBS per dose) on the d4 and d6 after LLC implantation.
2.8. Detection of the CCR7 Expression, Cytotoxicity, and Apoptosis of rsCD8+T-cells in Vitro
Cytation 5 instrument with Gen5™ data-analysis software (BioTek, Instruments, Friedrichshall, Germany) was used for the analysis of cells images, as described earlier [4]. The CCR7 expression on CD8+ T-cells, cytotoxicity, and apoptosis of rsCD8+ T-cells were studied, as described previously [4].
2.9. Histology of the Lungs
Histological examination of lung was carried out on d7, as described previously [4,6].
2.10. Assessment of Tumor Growth
The effect of cell therapy with rsCD8+ cells on the growth of LLC was evaluated via statistical comparison of the tumor nodes volume in the control and experimental groups at the d7, according to the tumor growth retardation and tumor growth inhibition index (TGII) [4,7].
where Vc and Ve are the average volumes of the nodes in the control and experimental groups.
TGII = (Vc − VO)/Ve × 100%
2.11. Assessment of Tumor Volume
Tumor dimensions were measured by digital calipers at d7, and the tumor volume was calculated as follows [8]:
V = π/6 × length × width × height
2.12. Statistical Analysis
Data are presented as mean ± SEM. Differences between groups were identified using the Mann–Whitney test by the SPSS 12.0 software. Under all circumstances, p < 0.05 was considered significant.
3. Results
3.1. Study of Detection of the CCR7 Expression, Cytotoxicity, and Apoptosis of rsCD8+T-Cells In Vitro
The rsCD8+ T-cells had higher expression levels of chemokine receptor CCR7 than naive spleen CD8+ T-cells in CD8+ T-cell culture (Figure S1). The CCR7 expression by rsCD8+ T-cells did not change after the exhaustion, which indicates that the changes induced by the MEKi and nivolumab are stable (Figure S1). The rsCD8+ T-cells were more resistant to the cytotoxic effect of LLC cells than the naive spleen CD8+ T-cells. The rsCD8+ T-cells are more stable under cultivation: the apoptosis level of rsCD8+ T-cells was more in 2 times higher than naive spleen CD8+ T-cells. The cytotoxicity of rsCD8+ T-cells was higher than the cytotoxicity of naive spleen CD8+ T-cells in the same ratios (Figure S2).
3.2. Migration of rsCD8+ T-Cells Isolated from Mouse Spleen into the Lungs of Mice with LLC
RsCD8+ T-cells migrated actively to the lungs of mice with LLC 60 min after intravenous injection of CFSE-labeled rsCD8+ T-cells.
3.3. Lung Histology and Tumor Growth after Cell Therapy with rsCD8+ T-Cells
3.3.1. Lung Histology
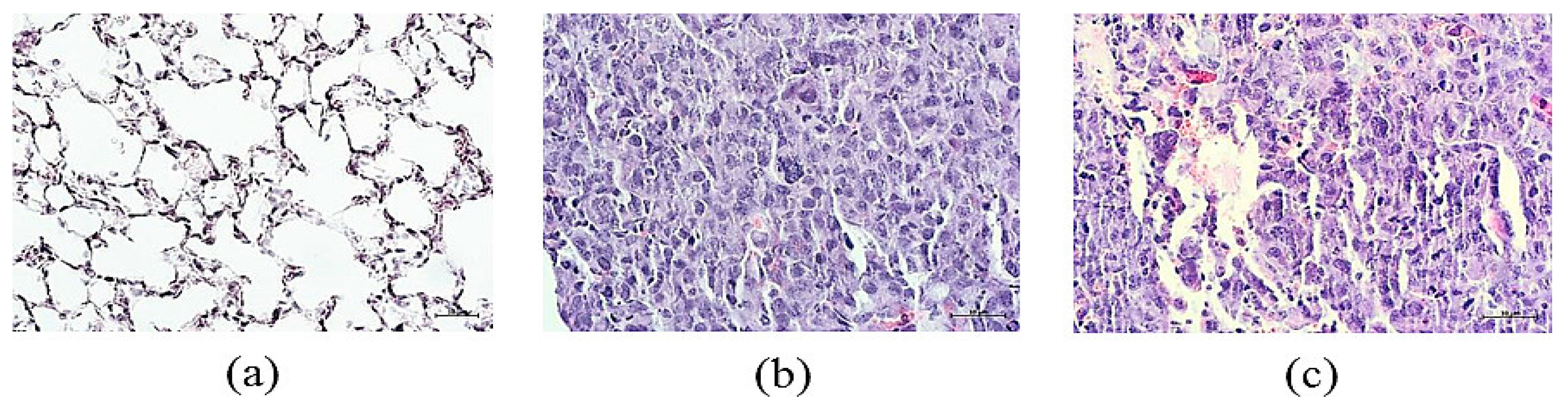
We evaluated the lung histology on d7 in response to treatment with LLC injection. The vehicle-treated lung of mice displayed lung tumors characterized by scattered tumor cells with cellular and nuclear polymorphism. Multinucleated giant cells are organized in clusters or aligned along the alveolar walls (Figure 1). The histological picture of the lungs from tumor-bearing mice treated with rsCD8+T-cells only displayed growth deceleration but not regression of tumor (Figure 1c) and showed a decrease in the number of tumor emboli in the vessels and perivascular and peribronchial metastases.
Figure 1.
Representative hematoxylin-eosin staining of tissue sections from (a) mice of intact control; (b) mice with LLC; (c) mice with LLC treated with rsCD8+T-cells on d7. ×400. Scale bar 10 μm.
3.3.2. Tumor Growth
The rsCD8+T-cell therapy caused an increase in TGII. The value of TGII after cell therapy with rsCD8+T-cells was 54.7 %. Moreover, we observed an increase in tumor volume and the average number of metastases (Table 1).

Table 1.
The effect of cell therapy with rsCD8+ T-cells on tumor growth in mice with LLC on d7 (M ± m).
3.4. The rsCD8+ T-Cells Change the Amount of Cancer Cells and Cancer Stem Cells in the Lungs and Blood of Tumor-Bearing Mice
We observed a significant increase in the number of CSCs with different phenotypes in the lungs of tumor-bearing mice on the d7 after LLC injection: EGF+Sox2+, CD44+Sox2+, CD274+Ki67+ (Figure S3). At the same time, all populations of cancer cells were increased in the blood of tumor-bearing mice compared to mice of intact control. The rsCD8+ T-cells injection significantly reduced the number of cancer cells and CSCs population (EGF+Sox2+, CD44hiCD90+Sox2+, CD90+Sox2+, CD279+Ki67+) in the lungs and blood of tumor-bearing mice on the d7 (Figure S3). However, the population of proliferating CD274+ cells in the lung was increased after rsCD8+ T-cell injection. At the same time, the number of CD44+Sox2+ cells in the blood and the amount of CD44hiCD90+ cells in the lung were changed weakly.
3.5. Effect of rsCD8+ T-Cells on the Content of CD8+ T-Cells in the Lungs and Blood of Tumor-Bearing Mice
It was shown that the frequency of circulating T-cells was significantly decreased in patients with cancer versus normal controls [9]. We observed a reduction in the different CD8+ T-cells populations in the blood of tumor-bearing mice compared with mice without LLC on the d7: CD3+CD4−CD8+, CD3+CD8+PD-1(CD279)+, CD3+CD8+PD-L1+, CD3+CD8+PD-1(CD279)hi, CD8+CCR7+, CD8+CD62L−CD44+, CD8+CD62LhiCD44low, and CD8+CD62+CD44+ (Figure S4). At the same time, the amount of proliferating CD8+T-cell populations with phenotype CD3+CD4-CD8+ and CD3+CD8+PD-1(CD279)+ increased in the blood of tumor-bearing mice. The rsCD8+T-cells administration caused an increase in a significant number of CD8+T-cell populations (CD8+CCR7+, CD3+CD4-CD8+Ki67+, CD3+CD8+PD-1(CD279)+, and CD3+CD8+PD-L1+) in the blood of tumor-bearing mice compared to tumor-bearing mice without treatment.
We detected a growth of CD8+ T-cells migration from the blood to the lungs in response to tumor and exhaustion of CD8+ T-cells pool under tumor formation on d7 (CD3+CD4-CD8+, CD3+CD8+PD-1(CD279)+, CD3+CD8+PD-L1+, CD3+CD8+PD-1(CD279)hi, CD8+CCR7+, CD8+CD62LhiCD44low, and CD8+CD62L+CD44+) (Figure S4). The exception was proliferating CD3+CD4-CD8+ T-cells, effector T-cells (CD8+CD62LlowCD44hi), whose number significantly decreased in the lungs of mice with LLC. After rsCD8+T-cell therapy, the CD8+T-cell population in the lungs of tumor-bearing mice was lower in comparison with the mice with LLC without treatment (Figure S4). At the same time, populations of proliferating CD3+CD4−CD8+ cells and effector CD8+T-cells (CD8+CD62LhiCD44low and CD8+CD62L+CD44+) in the lung were increased after rsCD8+ T-cell injection.
3.6. Effect of rsCD8+ T-Cells on the Content of CD4+ T-Cells in the Blood and Lungs of Tumor-Bearing Mice
The LLC model caused a significant decrease in the number of CD4+ T-cells with different phenotypes in the mouse blood on the d7: CD3+CD4+CD8-, CD3-CD4+, CD3+CD4+CD8+, CD3+CD4+PD-1(CD279)+, CD3+CD4+PD-L1+, and proliferating CD3+CD4+PD-1(CD279)+ (Figure S5). Administration of rsCD8+T-cells caused an increase in a significant number of CD4+T-cell populations (CD3-CD4+, CD3+CD4+CD8+, CD3+CD4+PD-L1+, CD3+CD4+PD-1+, proliferating cells: CD3+CD4+PD-1+ and CD3+CD4+CD8-) in the blood of mice with LLC compared to untreated mice with LLC (d7). At the same time, the content of CD3+CD4+CD8- cells decreased even more during treatment in the blood.
We observed a significant decrease in the number of CD4 T-cells with different phenotypes in the lungs of mice on the d7: CD3+CD4+CD8-, CD3-CD4+, CD3+CD4+CD8+, CD3+CD4+PD-1(CD279)+, and proliferating CD3+CD4+CD8- and CD3+CD4+PD-1(CD279)+ cells (Figure S5). However, we observed an increase in double-positive CD3+CD4+CD8+ T-cells, the population of Treg (CD3+CD4+PD-1+) and CD3+CD4+PD-L1+ cells in the lungs of tumor-bearing mice compared to mice without tumor on the d7. The rsCD8+ T-cells injection significantly reduced the number of T-cells with phenotype CD3+CD4+CD8+, CD3+CD4+PD-L1+, CD3+CD4+CD279+ and proliferating CD3+CD4+CD279+ cells in the lungs. At the same time, the number of CD4+ T-cell populations with phenotype CD3+CD4+CD8-, CD3-CD4+, and proliferating cells CD3+CD4+CD8- increased in the lungs of mice with LLC. We clarify this by increasing the migration of these populations of CD4+ T-cells from the blood to the lungs in response to rsCD8+T-cells administration.
4. Conclusions
Prior studies [4,5] have analyzed the impacts of reprogramming by MEKi and blockade of the PD-1 on the activity of CD8+ T-cells derived from bone marrow or blood. In this study, we observed that reprogramming induced the activity of CD8+ T-cells isolated from the spleen. We presented evidence that reprogramming may have favorable CD8+ T-cells impacts and enhances the antitumor activity of CD8+ T-cells in the LLC orthotopic model. This strategy generated CD8+ T-cells with higher efficacy for cell therapy. The effect of rsCD8+ T-cell therapy has been associated with the activation of the host immune response by increasing the populations of CD8+ and CD4+ T-cells in mice, and the effect of rsCD8+ T-cells and mouse effector CD8+ T-cells on cancer cells and CSCs.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ECB2023-14132/s1, Figure S1: Study of Detection of the CCR7 Expression. (a) The count of naive, reprogrammed, and exhausted reprogrammed CD8+ T-cells of the spleen of C57BL/6 mice expressing the CCR7 marker in T-cell culture, (b) 20× images of T-cells stained with: Hoechst (blue) to identify cell nuclei; CD8 FITC (green); CCR7 AF555 (red); (Hoechst+CD8+CCR7) composite image using all three colors. Determination of the percentage of cells CD3+CD8+CCR7+ was made by assessing the ratio of cells counted in green and red channel to total cells counted in the blue (DAPI) channel. All scale bars are 1000 µm. *—for comparison with the naive spleen T-cells by Mann–Whitney test (p < 0.05); Figure S2: Cytotoxicity and apoptosis of naive and reprogrammed spleen CD8+ T-cells in the LLC culture. (a) The count of apoptotic tumor LLC cells after co-cultivation with reprogrammed spleen CD8+ T-cells (% from dead cells of LLC culture); (b) The count of apoptotic tumor LLC cells after cocultivation with spleen CD8+ T-cells (% from added cells); (c) Hoechst (blue) to identify cell nuclei; 7AAD (red); (Hoechst+7AAD+) composite image using all two colors; Figure S3: The amount of cancer cells and cancer stem cells in the mouse lung and blood on d7; Figure S4: The effect of rsCD8+ T-cell-therapy on CD8+ T-cell amount in mouse lung and blood on d7; Figure S5: The effect of rsCD8+ T-cell-therapy on CD4+ T-cell amount in the mouse lung and blood on d7.
Author Contributions
Conceptualization, E.G.S., E.P.; methodology, E.G.S., O.P. and N.E.; software, E.P.; validation, E.G.S., O.P., A.P., N.E. and E.P.; formal analysis, E.G.S., O.P. and N.E.; investigation, O.P., A.P., N.E., M.Z., E.P., L.S. and L.K.; resources, E.G.S.; data curation, E.G.S.; writing—original draft preparation, O.P.; writing—review and editing, E.G.S. and D.W.; visualization, O.P., N.E., A.P., E.P. and L.S.; supervision, E.G.S.; project administration, E.G.S., A.D., N.K., S.M. and A.K.; funding acquisition, A.D., N.K., S.M. and A.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the IACUC of Goldberg ED Research Institute of Pharmacology and Regenerative Medicine, Tomsk NRMC (protocol code 189092021).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is contained within the article or Supplementary Material.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Stapelfeld, C.; Dammann, C.; Maser, E. Sex-specificity in lung cancer risk. Int. J. Cancer 2020, 146, 2376–2382. [Google Scholar] [CrossRef] [PubMed]
- Poncette, L.; Bluhm, J.; Blankenstein, T. The role of CD4 T cells in rejection of solid tumors. Curr. Opin. Immunol. 2022, 74, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Raskov, H.; Orhan, A.; Christensen, J.P.; Gögenur, I. Cytotoxic CD8+ T-cells in cancer and cancer immunotherapy. Br. J. Cancer. 2021, 124, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Skurikhin, E.G.; Pershina, O.; Ermakova, N.; Pakhomova, A.; Widera, D.; Zhukova, M.; Pan, E.; Sandrikina, L.; Kogai, L.; Kushlinskii, N.; et al. Reprogrammed CD8+ T-Lymphocytes Isolated from Bone Marrow Have Anticancer Potential in Lung Cancer. Biomedicines. 2022, 10, 1450. [Google Scholar] [CrossRef] [PubMed]
- Skurikhin, E.G.; Pershina, O.; Ermakova, N.; Pakhomova, A.; Zhukova, M.; Pan, E.; Sandrikina, L.; Widera, D.; Kogai, L.; Kushlinskii, N.; et al. Cell Therapy with Human Reprogrammed CD8+ T-Cells Has Antimetastatic Effects on Lewis Lung Carcinoma in C57BL/6 Mice. Int. J. Mol. Sci. 2022, 23, 15780. [Google Scholar] [CrossRef] [PubMed]
- Cardiff, R.D.; Miller, C.H.; Munn, R.J. Manual hematoxylin and eosin staining of mouse tissue sections. Cold Spring Harb. Protoc. 2014, 2014, 655–658. [Google Scholar] [CrossRef] [PubMed]
- Hather, G.; Liu, R.; Bandi, S.; Mettetal, J.; Manfredi, M.; Shyu, W.C.; Donelan, J.; Chakravarty, A. Growth rate analysis and efficient experimental design for tumor xenograft studies. Cancer Inform. 2014, 13, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Tomayko, M.M.; Reynolds, C.P. Determination of subcutaneous tumor size in athymic (nude) mice. Cancer Chemother. Pharmacol. 1989, 24, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Czystowska, M.; Gooding, W.; Szczepanski, M.J.; Lopez-Abaitero, A.; Ferris, R.L.; Johnson, J.T.; Whiteside, T.L. The immune signature of CD8(+)CCR7(+) T cells in the peripheral circulation associates with disease recurrence in patients with HNSCC. Clin. Cancer Res. 2013, 19, 889–899. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).