Abstract
Background/Objectives: Philadelphia has experienced a surge in illicit fentanyl adulterated with alpha-2 agonist sedatives. Initially, xylazine (“tranq”) was the predominant adulterant, and a novel multimodal withdrawal protocol was effective at mitigating symptoms. However, since mid-2024, medetomidine—a more potent sedative—has largely supplanted xylazine. Clinicians have reported more severe, treatment-resistant opioid withdrawal during this transition. To assess whether a previously effective withdrawal management protocol retained efficacy after the emergence of medetomidine as the primary fentanyl adulterant in a community. Methods: We conducted a retrospective cohort study of patients receiving protocol-based opioid withdrawal treatment at two emergency departments in Philadelphia between September 2022 and April 2025. Patients were divided into the xylazine era (September 2022–July 2024) and medetomidine era (August 2024–April 2025). The primary outcome was a change in Clinical Opioid Withdrawal Scale (COWS) score from pre- to post-treatment. Secondary outcomes included rates of discharge against medical advice (AMA) and ICU admission, as well as the impact of a revised treatment protocol. Results: Among 1269 encounters with full data, 616 occurred during the xylazine era and 770 during the medetomidine era. Median COWS reduction was greater in the xylazine group (−9.0 vs. −4.0 points, p < 0.001), with more patients achieving symptom relief (COWS ≤ 4: 65.6% vs. 14.2%, p < 0.001). ICU admission occurred in 8.5% of xylazine era patients and 16.8% of medetomidine era patients (p < 0.001). Rates of AMA were higher during the medetomidine era as well (6.5% vs. 3.6%) (p = 0.038). Revision of treatment protocols showed promise. Conclusions: The protocol was significantly less effective during the medetomidine era, though a protocol change may be helping. Findings highlight the need to adapt withdrawal treatment protocols in response to changes in the illicit drug supply.
Keywords:
opioid withdrawal; xylazine; medetomidine; OUD; fentanyl; adulterant; Philadelphia; tranq dope; demon dope 1. Introduction
Philadelphia remains at the leading edge of the opioid crisis, with high rates of fentanyl use and associated morbidity. In recent years, the local illicit opioid supply has been increasingly adulterated with potent sedatives, intensifying the clinical challenges associated with withdrawal management [1]. Xylazine—a veterinary alpha-2 adrenergic agonist—emerged in 2022 as a frequent fentanyl adulterant, becoming present in up to 99% of the publicly checked dope samples by 2023 [2]. The combination of potent synthetic opioids and alpha-2 agonists wrought a series of challenges, including increasing reports of precipitated withdrawal, a serious and previously rare side effect when starting the medication buprenorphine [3]. This promoted the creation of emergency department (ED) protocols specifically tailored to manage the resulting complex withdrawal syndrome [4].
A multimodal opioid withdrawal treatment protocol was implemented at two Philadelphia EDs to address xylazine-associated withdrawal. This approach used multiple pharmacologic classes targeting distinct symptom domains: short-acting opioids (e.g., oxycodone, hydromorphone) for opioid cravings and bridging to partial agonists (low dose buprenorphine), ketamine for NMDA antagonism and analgesia, droperidol or olanzapine for anxiolytic and antiemetic effects, and alpha-2 agonists (tizanidine or guanfacine) for replacement of the xylazine. In an early evaluation, the protocol produced a median COWS score reduction from 12 to 4, with only 3.9% of patients leaving AMA compared to a 10.7% historical baseline [4].
In mid-2024, toxicology surveillance and clinical observations indicated a shift in adulterants, with medetomidine supplanting xylazine as the dominant alpha-2 agonist in the local fentanyl supply [5]. Medetomidine, an alpha-2 agonist sedative up to 200 times more potent than xylazine [6,7], entered the fray, possibly related to the scheduling of xylazine as a controlled substance by the Commonwealth of Pennsylvania [8]. Clinicians noted increasingly severe and atypical withdrawal symptoms, including profound vomiting, hypertensive crises, tremor without clonus or seizure, hypoactive encephalopathy, and refractory symptoms to conventional treatment [9]. These presentations often required ICU care and were poorly responsive to the previously successful xylazine focused protocol. Clinicians hypothesized that medetomidine-related withdrawal could mimic dexmedetomidine discontinuation syndrome, a well-documented phenomenon of sympathetic overactivity [10].
This study evaluated whether the novel opioid withdrawal protocol maintained effectiveness during and after the transition from the xylazine era (XE) to the medetomidine era (ME) in Philadelphia. We compared outcomes from the xylazine and medetomidine eras, hypothesizing a significant decline in treatment efficacy and increased rates of severe clinical secondary outcomes, following the emergence of medetomidine.
2. Materials and Methods
2.1. Study Design and Setting
We conducted a pragmatic retrospective cohort study of two urban EDs in Philadelphia, Pennsylvania, one academic and one community. The academic hospital, which sees approximately 76,000 visits annually, is a level 1 trauma center. The community hospital, which sees approximately 34,000 visits annually, is a stand-alone center 2.5 miles from the main hospital. Both sites serve large urban populations and care for a high volume of patients with opioid use disorder (OUD). Both hospitals were clinical sites for the retrospective analysis establishing evidence of order set efficacy, with the orders built into the electronic health record (EPIC Systems, Madison, WI, USA) [4].
The study protocol adhered to STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines for observational research, utilizing the guidelines prior to the development of the project. Institutional Review Board approval was obtained (IRB #1269), with a waiver of informed consent due to the retrospective nature and negligible risk of the study.
Two temporal cohorts were defined using 1 August 2024 as a transition point based on public health data identifying a shift from xylazine to medetomidine as the dominant fentanyl adulterant [5]. The XE cohort included encounters from 1 September 2022, when the order set debuted, to 31 July 2024. The ME cohort included encounters from 1 August 2024 to 30 April 2025.
On 11 February 2025, in response to local trends, the order sets were updated to address medetomidine adulteration. While education had been performed as early as December 2024 related to this adulterant change, this date represents the alteration of the treatment order sets. Doses of short-acting opioids were doubled (oxycodone 10 mg > 20 mg, hydromorphone 2 mg > 4 mg), and clonidine was added due to the rates of hypertensive crises (0.3 mg orally and 0.3 mg transdermal). Education about this change was made to staff during the standing faculty meeting and resident didactics as well as through virtual/asynchronous communication. While this period still represents part of the ME, given this defined change, it was analyzed as a subgroup.
2.2. Population
This study included adult patients (≥18 years) treated in the ED who received medications from the withdrawal protocol during the study period (1 September 2022–30 April 2025). This represents the total cohort and includes all patients who were present on the database report.
The final cohort are those from the total who had both pre- and post-treatment COWS scores and a disposition documented in their charts. Exclusion criteria included missing outcome data, pregnancy, and active enrollment in methadone or buprenorphine maintenance therapy (the latter of which were ineligible for order set usage).
Detection of xylazine and medetomidine exposure in humans is difficult and not performed routinely. Due to the conjoined nature of opioids and alpha-2 agonists in Philadelphia, fentanyl urine toxicology testing is used as a marker of street “dope” exposure. Adulterant classification was therefore based largely on temporal trends rather than individual toxicology testing, which was unavailable in the ED setting, aside from fentanyl testing. A small cohort did undergo liquid chromatography tandem mass spectrometry testing. A total of 59/59 individuals tested positive for 3-OH-medetomidine metabolite in their urine samples, following glucuronidase pre-treatment. A full accounting of toxicology analysis will be published separately; a subgroup was previously described [9].
2.3. Exposure Classification
Era classification was based on date of presentation and the predominant local adulterant, as identified through citywide drug surveillance. Xylazine predominated before 1 August 2024, while medetomidine became the dominant adulterant thereafter. A subgroup analysis of patients treated after a protocol revision on 11 February 2025 was also performed, as this represents when default orders were changed for providers.
2.4. Outcomes
The primary outcome was a change in Clinical Opioid Withdrawal Scale (COWS) score from pre- to post-treatment. COWS is a multi-item scale used as the standardized means of assessing withdrawal severity in the United States [11]. Notably, there are not standardized withdrawal severity tools for alpha-2 agonist withdrawal [12]. The initial study solely utilized COWS scores for holistic withdrawal evaluation, given that anxiety and vital sign abnormalities common in alpha-2 agonist withdrawal are included in COWS. There was an association of the order sets between both reducing COWS scores and reducing the risk of AMA disposition in the first study, indicating that it may be a reasonable alternative [4]. In the absence of other standardized withdrawal assessments, COWS was used as the sole criterion for fentanyl, xylazine, and medetomidine withdrawal severity. Secondary outcomes included the following: (1) percentage of patients with COWS ≤ 4 post-treatment (which signifies no longer classifying as having withdrawal); (2) disposition from the ED, including AMA discharge, hospital admission, and ICU transfer; and (3) occurrence of serious adverse events during ED care.
2.5. Measurements and Analysis
Data for this study were obtained by an automated database report. This report contains visit demographics, chief complaint, and diagnostic data (urine fentanyl screen results), pre- and post-treatment COWS scores, and disposition data.
Statistical analysis was performed using R Version 4.4.3 statistical software (R Core Team, 2023). Descriptive statistics were calculated utilizing demographic information documented in the codebook, including standard deviations for non-parametric data.
Continuous variables were summarized as medians with interquartile ranges and compared using Mann–Whitney U and Wilcoxon signed-rank tests. Categorical variables were reported as frequencies and compared using chi-square tests. A two-sided p-value < 0.05 was considered statistically significant. Monthly COWS trends and responder rates were graphed, with key inflection points noted.
3. Results
3.1. Patient Characteristics
A total of 1269 patient encounters met inclusion criteria, out of 2158 total encounters having received medications from the protocol during the period. Of the final cohort, 616 encounters were in the XE cohort (September 2022–July 2024) and 770 in the ME cohort (August 2024–April 2025); see Figure 1. The two cohorts were similar in demographic makeup both in their total and final cohort forms. Full demographics data, including race/ethnicity, are included in Table 1.
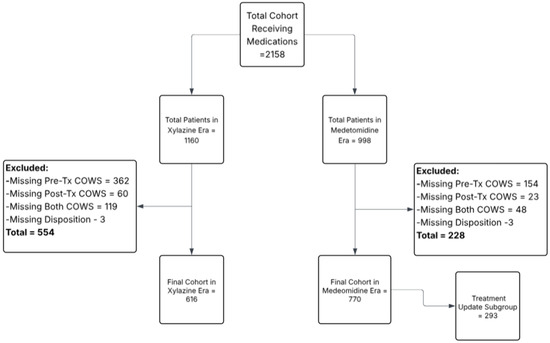
Figure 1.
CONSORT diagram of recruitment and exclusions.

Table 1.
Demographic characteristics by era and cohort.
Notably, xylazine is well known to be associated with severe skin ulceration and eventual infection [11]. The chief complaints of all presentations are shown in Table 2. They have been simplified for categorization sake; please see Appendix A for a full list of chief complaints and in which categories they were placed. It is therefore quite telling that rates of visits for skin and soft tissue visits fell from 33.3% to 15.0% (p < 0.001) between the eras, and that volume was made up for with a commensurate rise in visits purely for opioid withdrawal (13.7% to 31.3%, p < 0.001).

Table 2.
Chief complaints of presentations between the xylazine and medetomidine eras.
At presentation, median initial COWS scores were higher in the medetomidine cohort (15.0, IQR 10–21) than in the xylazine cohort (13.0, IQR 7–17), which was statistically significant (p < 0.001). Of note, there were also significantly more presentations per month in the ME than in the XE. See full COWS scores and encounter details in Table 3.

Table 3.
Withdrawal severity and treatment response by era.
3.2. Withdrawal Treatment and COWS Outcomes
The primary outcome of withdrawal severity improvement, measured by the change in COWS, differed markedly between the two eras. Figure 2 illustrates the COWS scores before and after treatment for each cohort (median and IQR). In the XE cohort, withdrawal scores improved substantially with protocol treatment. The median COWS decreased from 13.0 (IQR 10–17) on arrival to 4.0 (IQR 1–6) after treatment, a median reduction of −9 points (p < 0.001 for within-cohort pre/post comparison). This supports the efficacy of the protocol in mitigating withdrawal signs and symptoms in the XE, consistent with previously published outcomes [4].
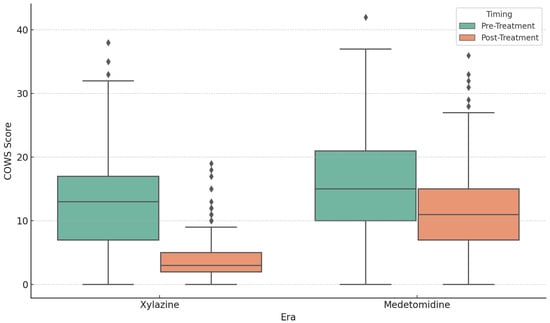
Figure 2.
Box plot of COWS scores pre- and post-treatment by era, showing significantly higher ME post-treatment COWS and reduced overall efficacy.
In Figure 3 and Figure 4, a large majority of XE patients achieved a post-treatment COWS score of <5 (65.6%, indicating relief from withdrawal). In contrast, the ME cohort experienced more modest improvements. The median COWS in this group was 15.0 (IQR 10–21) before treatment and 11.0 (IQR 7–15) post-treatment, for a median reduction of only −4 points. While this reduction was still statistically significant compared to pre-treatment scores (p < 0.001), the magnitude of improvement was clearly smaller. Only 16.4% during the ME attained a post-treatment COWS < 5 (p < 0.001 vs. XE). The between-cohort comparison of ∆COWS was highly significant (p < 0.001), indicating that the protocol’s effectiveness in reducing objective withdrawal scores was significantly blunted in the ME.
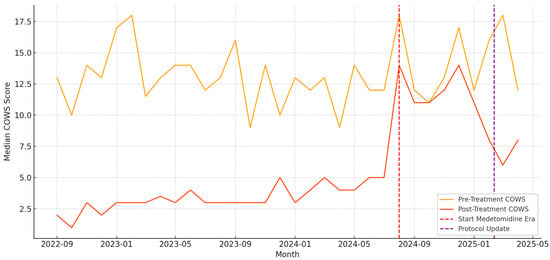
Figure 3.
Line graph of COWS scores pre- and post-treatment by month, with the first line delineating the month where medetomidine became dominant and the purple line demarcating the beginning of revised treatment protocols.
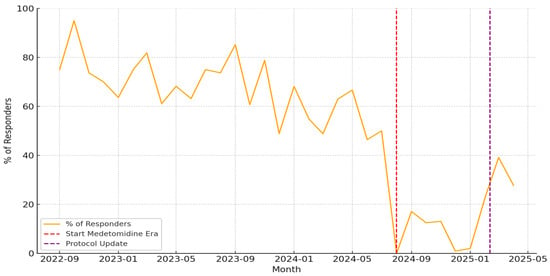
Figure 4.
Line graph trend of patients whose post-treatment COWS scores reached a level of resolution of withdrawal severity (COWS ≤ 4), per month, demonstrating a dramatic fall in the efficacy of treatment.
To account for any baseline differences, we performed a two-way analysis of variance on COWS scores, with time (pre vs. post) and era as factors. This analysis demonstrated a significant interaction effect (p < 0.001), corroborating that the improvement in COWS over time depended on the era (XE vs. ME). In essence, patients in the ME did not respond as robustly to the standardized regimen as those in the XE did.
3.3. Secondary Outcomes: Subgroup, Disposition, and Adverse Events
To assess the impact of the revised withdrawal protocol introduced on 11 February 2025, we performed a subgroup analysis of ME encounters before (BPC) and after the protocol change (APC). Among the 998 total encounters in the ME, 770 met criteria for inclusion in the analytic cohort, of which 293 (38.1%) occurred after the updated protocol was implemented. Patients in this subgroup demonstrated significantly greater improvement in COWS scores; the median reduction in COWS was −6.0 (IQR: −9 to −3) after the revision (APC), compared to −4.0 (IQR: −6 to −2) prior to the revision (BPC, p < 0.001). The proportion of patients achieving a post-treatment COWS score ≤ 4 increased from 11.0% to 21.1% following the protocol update (p = 0.003). Although response rates remained lower than in the xylazine era, these findings suggest partial restoration of protocol efficacy after the revision.
We also examined emergency department dispositions across eras (see Table 4). The incidence of patients leaving against medical advice (AMA) was higher in the medetomidine cohort before the protocol change (6.5%) compared to the xylazine cohort (3.6%), and this difference reached statistical significance (p = 0.036). After the protocol update, AMA rates modestly improved to 5.2%, though the change from the pre-revision medetomidine subgroup did not meet statistical significance (p = 0.056). ICU-level admission occurred substantially more frequently in the medetomidine cohort; 88 patients (18.4%) were admitted to the ICU before the protocol revision, compared to 35 patients (8.5%) in the xylazine era (p < 0.001). After the protocol change, ICU admission remained common at 48 patients (16.4%), though this represented a nonsignificant reduction compared to the earlier medetomidine period (p = 0.527). Overall admission rates in the post-protocol group were 76.1%.

Table 4.
Emergency department disposition by era (including post-protocol change cohort).
Hospital admissions for continued withdrawal management were more frequent in the ME. In the XE, nearly 30% of patients could be discharged home or to a treatment program after ED management. In contrast, in the ME cohort, only around 20% were discharged from the ED, while a significantly higher proportion (~75%) required inpatient admission for ongoing care of withdrawal, including almost double the amount who needed ICU care.
Regarding adverse events, the protocol was generally well-tolerated in both groups, with no serious adverse events directly attributable to the medications. There were zero instances of respiratory arrest or cardiac arrest due to the treatment in either era.
4. Discussion
This pragmatic, real world study demonstrates that the emergence of medetomidine as an adulterant in illicit fentanyl was associated with a decline in the effectiveness of a novel opioid withdrawal management protocol developed during the xylazine era. In the XE (September 2022–July 2024), the protocol was associated with reduced withdrawal severity, whereas during the ME (August 2024–April 2025) significantly smaller improvements in COWS scores were noted. Concurrently, ME patients had higher rates of intensive care unit (ICU) admission for withdrawal-related complications and more patients leaving the emergency department against medical advice (AMA).
These disparities suggest that medetomidine adulteration may be associated with clinical challenges not adequately addressed by a protocol tailored to manage opioid withdrawal with another potent alpha-2 agonist (xylazine). Xylazine, a veterinary alpha-2 agonist sedative, rose to prominence as a fentanyl adulterant in the mid-2010s and early 2020s. By 2019–2022, xylazine was detected in approximately 2.9–10.9% of fentanyl-involved overdose deaths in the United States [13]. Medetomidine—a pharmacologically similar but more potent alpha-2 agonist—has rapidly increased as a new adulterant over the past two years. The first confirmed cases of medetomidine exposure in U.S. overdose patients were reported in late 2023 [14]. Shortly thereafter, public health alerts in early 2024 announced the detection of medetomidine in local fentanyl supplies in Philadelphia and New York [15]. These alerts noted that medetomidine was identified in street “dope” samples alongside fentanyl and xylazine, and described overdose clusters involving profound sedation unresponsive to naloxone.
Forensic drug surveillance from mid-2024 further documented medetomidine’s proliferation, being identified in opioid samples across multiple states [16]. Medetomidine was almost invariably found in combination with xylazine [17], indicating a shift to an increasingly dynamic supply pattern in which fentanyl is co-mixed with multiple sedatives. This context likely contributed to the challenging clinical presentations observed during the ME. Patients were possibly exposed to two synergistic alpha-2 agonists (medetomidine plus xylazine) alongside fentanyl, a combination plausibly expected to produce more profound and prolonged CNS depression than either sedative alone [17]. It is plausible that illicit suppliers introduced medetomidine as a more potent or longer-acting replacement for xylazine once awareness and regulation of xylazine increased, thereby sustaining the enhanced sedative profile of adulterated fentanyl.
Medetomidine’s pharmacologic properties may help explain why its community presence may be associated with a reduction of withdrawal protocol effectiveness. Medetomidine produces similar effects to xylazine—including sedation, analgesia, bradycardia, and hypotension [18,19]—but tends to have a longer duration of action [20,21]. Given increased potency of medetomidine, it is unsurprising that the ME was therefore associated with an increase in ED presentations for withdrawal, as well as the increased need for ICU-level care, as patients often suffered more severe withdrawal, requiring higher intensity care.
In contrast to xylazine, which is notorious for causing necrotic skin ulcers in chronic users [22], medetomidine has not been linked to such tissue injury. Its chief hazards are systemic, exerting powerful sedating effects that complicate both overdose resuscitation and withdrawal management. This is notable given the decreased number of visits related to skin and soft tissue infections in the ME.
Chronic exposure to alpha-2 agonists can induce adaptive changes; abrupt cessation precipitates a rebound hyperadrenergic state. In the critical care literature, prolonged infusions of dexmedetomidine (the active enantiomer of medetomidine) have been shown to produce significant withdrawal symptoms upon discontinuation [23]. A recent meta-analysis reported that over one-third of patients developed hypertension and tachycardia after stopping long-term dexmedetomidine, and it advocated gradual weaning or adjunctive clonidine to mitigate such withdrawal effects [24,25]. By analogy, individuals using medetomidine-adulterated opioids may regularly develop dependence on this sedative. When they present to the ED in opioid withdrawal (having not used for several hours), they plausibly could simultaneously be in medetomidine withdrawal.
This scenario would likely manifest as severe autonomic hyperactivity (anxiety, vomiting, tremors, hypertension, tachycardia) that overlaps with opioid withdrawal but does not fully respond to opioid agonist therapy, which is exactly the impact that was demonstrated. Indeed, health officials have noted that frequent xylazine users experience a distinct withdrawal syndrome (irritability, anxiety, palpitations, and elevated blood pressure) when xylazine is discontinued [22]. It is likely that medetomidine causes a similar withdrawal phenomenon. Unrecognized alpha-2 agonist withdrawal in our ME patients is likely therefore a key factor in the blunted COWS score improvements—since certain withdrawal signs (e.g., tachycardia, diaphoresis, agitation) could persist due to persistent autonomic activation.
After appreciating these issues, we modified our ED withdrawal protocol in February 2025 to better address medetomidine co-exposure. While education regarding this challenge had been underway since December 2024, this change represents a tangible difference in the order sets providers utilized. Although detailed outcomes of the new protocol are beyond the scope of this discussion, and will be published separately, we observed the following associations in the APC compared to the BPC: withdrawal-symptom relief rates began to rise, and AMA discharge rates declined relative to earlier in the ME. While underpowered to determine causation, these associations should be assessed in future studies.
The protocol revisions included measures to counteract medetomidine withdrawal, such as more aggressive management of autonomic symptoms by use of clonidine and sympatholysis with higher doses of short-acting opioids. Clonidine is a more potent oral alpha-2 agonist than tizanidine or guanfacine, up to 50 times more vasoactive [23]. In essence, we attempted to pharmacologically bridge the sudden loss of alpha-2 agonist input—an approach analogous to using clonidine to taper patients off dexmedetomidine or xylazine [24,25].
The association with partial restoration of efficacy in the APC supports the possibility that more aggressive management may improve outcomes. However, even with adjustments, ME outcomes did not return fully to the baseline seen in the XE, indicating that significant challenges remain. Patients with medetomidine exposure may require prolonged observation and higher levels of care to completely normalize their withdrawal trajectory. Further study is needed to determine optimal strategies for managing withdrawal in the context of medetomidine and similar sedative adulterants.
Overall, our findings highlight the necessity for clinicians to rapidly adapt withdrawal management protocols in response to changes in the adulterant profile of illicit opioids, as well as the importance of community-based drug testing programs. A protocol that was effective for “tranq dope” (fentanyl + xylazine) had to be recalibrated for what some have termed “demon dope” (fentanyl + medetomidine ± xylazine). These conclusions align with emerging guidance urging emergency and critical care providers to recognize and manage polysubstance opioid withdrawal, including the effects of alpha-2 agonist adulterants [5,9,22]. By integrating clinical findings with public health intelligence on drug-supply trends, healthcare systems can better prepare for and respond to the next evolution of the opioid crisis.
5. Limitations
This study has several important limitations. First, as a pragmatic, real world, retrospective analysis, it is inherently subject to confounding, selection bias, and limited generalizability beyond the two emergency departments studied. While both institutions serve a high volume of individuals with opioid use disorder in Philadelphia, the findings may not reflect experiences in other regions or healthcare systems.
Second, not all patients receiving withdrawal protocol treatment during the study period could be analyzed due to missing data. Specifically, patients lacking either pre- or post-treatment COWS scores or documented ED disposition were excluded from the final cohort, and more than a third of eligible cases were excluded for missing data. This may have introduced bias if these excluded encounters differed systematically from those included. Given the demographic and disposition data showing similar total and final cohorts, the impact of this is likely mild.
Third, individual toxicologic confirmation of xylazine or medetomidine exposure was not available. Neither compound is included in routine clinical toxicology screening, and their detection requires specialized analytical techniques that were not performed in real-time ED care. Era classification was therefore inferred based on temporal association with drug-supply trends reported by public health surveillance, which may misclassify some cases—especially during transition months. A small cohort that received LC-MS/MS confirmation of medetomidine exposure strengthens the data but does not replace full individual-level toxicology. It is also possible that the combination of xylazine and medetomidine is responsible, more so than just medetomidine itself. Future studies should assess individuals who are exposed to xylazine, medetomidine, and both and compare outcomes.
Fourth, all statistical analysis was performed using univariate analysis, rather than the use of a multivariate regression analysis. This increases the risk that the association described is confounded by other variables and limits interpretation. Given the pragmatic, retrospective, and limited nature of the dataset, it was felt that simple descriptive analysis was most appropriate, and future studies should assess other possible granular reasons for the observed findings.
Fifth, chief complaint data relied on structured text documentation, which introduces limitations in symptom categorization. Complaints related to opioid withdrawal may have been inconsistently documented or underreported if patients presented with overlapping symptoms such as vomiting or altered mental status. As a result, the frequency of opioid withdrawal presentations may be underrepresented in our analysis.
Additionally, the Clinical Opiate Withdrawal Scale (COWS) was the sole tool used to assess withdrawal severity, though it was developed for opioid withdrawal and may not fully capture the autonomic or neuropsychiatric features of alpha-2 agonist withdrawal. There are currently no validated tools for medetomidine or xylazine withdrawal, and this likely underestimates the true symptom burden in such patients.
Finally, while the protocol revision in February 2025 showed promising improvements, this subgroup was pragmatically inserted for patient care reasons, rather than as a focused research question. It was therefore both underpowered to determine accurate comparisons and purely exploratory. Further data are needed to confirm effectiveness and safety of any treatment protocol in the context of medetomidine exposure.
6. Conclusions
In summary, this retrospective cohort analysis found that our opioid withdrawal protocol was significantly less effective during the period when fentanyl was adulterated with medetomidine, compared to the earlier xylazine-dominant era. Patients in the ME experienced poorer withdrawal symptom relief and higher rates of ICU admission and AMA disposition, indicating more severe and complex withdrawal presentations. Implementation of a revised protocol (in February 2025), which incorporated adjustments to address medetomidine’s alpha-2 agonist effects, was associated with partial restoration of efficacy. This suggests that adapting treatment strategies to account for medetomidine co-exposure can mitigate some of the negative impact.
However, even after protocol changes, medetomidine-exposed patients remained more difficult to treat than those in the XE, underscoring the formidable challenge posed by this new adulterant. For medical practice, these findings highlight the importance of dynamic protocol revisions in the face of an evolving drug supply. Standard opioid-centric withdrawal management approaches may fail when confronted with novel adulterants that produce additional non-opioid pharmacologic effects (such as profound sedation or autonomic instability). Clinicians should be alert to regional drug trends and be prepared to modify withdrawal treatment plans accordingly.
Looking ahead, enhanced surveillance of illicit drugs is crucial for early identification of emerging adulterants. Timely toxicological analysis of overdose cases and drug samples, coupled with rapid information-sharing through public health alerts, will enable clinicians to anticipate changes in withdrawal patient presentations [13]. Future research should focus on developing tailored withdrawal protocols for multi-substance exposures. This includes investigating optimal management of alpha-2 agonist withdrawal in patients with OUD—such as the role of clonidine or other sympatholytics in treating medetomidine/xylazine withdrawal—and determining best practices to reduce ICU utilization and prevent AMA dispositions in these complex cases. In conclusion, a proactive, evidence-based approach to new opioid adulterants is needed to maintain effective withdrawal care. Ongoing collaboration between clinicians and addiction medicine and toxicology experts, as well as public health authorities, will be essential to stay ahead of emerging trends and to safeguard the outcomes of patients with opioid use disorder.
Author Contributions
Conceptualization, K.S.L., J.L.K. and P.D.; methodology, K.S.L.; software, K.S.L.; validation, K.S.L. and K.A.; formal analysis, K.S.L.; investigation, K.S.L.; resources, K.S.L.; data curation, K.S.L.; writing—original draft preparation, K.S.L.; writing—review and editing, K.S.L., T.W.-S., J.L.K., P.D. and K.A.; visualization, K.S.L.; supervision, K.S.L.; project administration, K.S.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Thomas Jefferson University (protocol code IRB #1269 and date of approval 14 December 2022).
Informed Consent Statement
Informed consent was waived due to the retrospective nature and negligible risk of the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Acknowledgments
During the preparation of this manuscript/study, the authors used ChatGPT, version 4.o for the purposes of assisting with formatting and literature review. The authors have reviewed and edited the output and take full responsibility for the content of this publication.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ED | Emergency Department |
| ME | Medetomidine Era |
| XE | Xylazine Era |
| OUD | Opioid Use Disorder |
| COWS | Clinical Opioid Withdrawal Scale |
| MDPI | Multidisciplinary Digital Publishing Institute |
| DOAJ | Directory of open access journals |
Appendix A. Categorization of Chief Complaints by Assigned Presentation Category
| Chief Complaint | Assigned Category |
| ABDOMINAL INJURY | Trauma |
| ABDOMINAL PAIN | General Medical/Other |
| ABNORMAL LAB | General Medical/Other |
| ABRASION | Trauma |
| ABSCESS | Skin/Soft Tissue Infection |
| ABSCESS DRAINAGE | Skin/Soft Tissue Infection |
| ALCOHOL INTOXICATION | Psychiatric, Behavioral, and Social Needs |
| ALTERED MENTAL STATUS | General Medical/Other |
| ANGIOEDEMA | General Medical/Other |
| ANKLE PAIN | General Medical/Other |
| ANXIETY | Psychiatric, Behavioral, and Social Needs |
| ARM INJURY | Trauma |
| ARM PAIN | General Medical/Other |
| ARM SWELLING | Skin/Soft Tissue Infection |
| ASSAULT | Trauma |
| ASTHMA | General Medical/Other |
| BACK PAIN | General Medical/Other |
| BLACK OR BLOODY STOOL | General Medical/Other |
| BLOOD INFECTION | General Medical/Other |
| BURN | Trauma |
| CAST CHECK | General Medical/Other |
| CELLULITIS | Skin/Soft Tissue Infection |
| CHEST PAIN | General Medical/Other |
| CHEST TIGHTNESS | General Medical/Other |
| CHILLS | General Medical/Other |
| COLD EXPOSURE | Psychiatric, Behavioral, and Social Needs |
| CONSTIPATION | General Medical/Other |
| COUGH | General Medical/Other |
| COUGHING UP BLOOD | General Medical/Other |
| CYST | General Medical/Other |
| DEBRIDEMENT | General Medical/Other |
| DENTAL PAIN | General Medical/Other |
| DEPRESSION | Psychiatric, Behavioral, and Social Needs |
| DETOX | Opioid Withdrawal |
| DIALYSIS TREATMENT | General Medical/Other |
| DIARRHEA | General Medical/Other |
| DIFFICULTY WALKING | General Medical/Other |
| DIZZINESS | General Medical/Other |
| DRUG OVERDOSE | Psychiatric, Behavioral, and Social Needs |
| DRUG PROBLEM | Psychiatric, Behavioral, and Social Needs |
| DYSURIA | General Medical/Other |
| EARACHE | General Medical/Other |
| ELBOW PAIN | General Medical/Other |
| ENDOCARDITIS | General Medical/Other |
| EXTREMITY WEAKNESS | General Medical/Other |
| EYE DRAINAGE | General Medical/Other |
| EYE INFECTION | General Medical/Other |
| EYE PAIN | General Medical/Other |
| EYE PROBLEM | General Medical/Other |
| EYE TRAUMA | Trauma |
| FACIAL SWELLING | General Medical/Other |
| FAILURE TO THRIVE | Psychiatric, Behavioral, and Social Needs |
| FALL | Trauma |
| FEVER | General Medical/Other |
| FINGER INJURY | Trauma |
| FINGER PAIN | General Medical/Other |
| FLANK PAIN | General Medical/Other |
| FLU SYMPTOMS | General Medical/Other |
| FOOT BLISTER | General Medical/Other |
| FOOT INJURY | Trauma |
| FOOT PAIN | General Medical/Other |
| FOOT SWELLING | General Medical/Other |
| FOOT WOUND CHECK | General Medical/Other |
| FOREIGN BODY | General Medical/Other |
| FOREIGN BODY IN SKIN | General Medical/Other |
| FROSTBITE | Trauma |
| GENERALIZED BODY ACHES | General Medical/Other |
| GENITAL WARTS | General Medical/Other |
| GROIN PAIN | General Medical/Other |
| GROIN SWELLING | General Medical/Other |
| GUN SHOT WOUND | Trauma |
| HAND INFECTION | Skin/Soft Tissue Infection |
| HAND INJURY | Trauma |
| HAND PAIN | General Medical/Other |
| HEAD LICE | General Medical/Other |
| HEADACHE | General Medical/Other |
| HERNIA | General Medical/Other |
| HIP PAIN | General Medical/Other |
| HOMELESS | Psychiatric, Behavioral, and Social Needs |
| HYPERGLYCEMIA | General Medical/Other |
| HYPERTENSION | General Medical/Other |
| HYPOGLYCEMIA | General Medical/Other |
| INFECTION | Skin/Soft Tissue Infection |
| INGESTION | Psychiatric, Behavioral, and Social Needs |
| INTOXICATED | Psychiatric, Behavioral, and Social Needs |
| JAW PAIN | General Medical/Other |
| JOINT SWELLING | General Medical/Other |
| KNEE INJURY | Trauma |
| KNEE PAIN | General Medical/Other |
| LEG INJURY | Trauma |
| LEG PAIN | General Medical/Other |
| LEG PROBLEM | General Medical/Other |
| LEG SWELLING | General Medical/Other |
| MEDICAL COMPLAINT | General Medical/Other |
| MEDICATION REFILL | Psychiatric, Behavioral, and Social Needs |
| MOTOR VEHICLE vs. PEDESTRIAN | Trauma |
| MOTOR VEHICLE CRASH | Trauma |
| MRSA | Skin/Soft Tissue Infection |
| MULTIPLE SCLEROSIS | General Medical/Other |
| NASAL CONGESTION | General Medical/Other |
| NAUSEA | General Medical/Other |
| NECK INJURY | Trauma |
| NECK PAIN | General Medical/Other |
| NUMBNESS | General Medical/Other |
| OPEN WOUND | Skin/Soft Tissue Infection |
| OSTEOMYELITIS | General Medical/Other |
| OTHER | General Medical/Other |
| PAIN | General Medical/Other |
| PAIN WITH BREATHING | General Medical/Other |
| PALPITATIONS | General Medical/Other |
| PNEUMONIA | General Medical/Other |
| POOR APPETITE | General Medical/Other |
| POST-OP PROBLEM | General Medical/Other |
| PREGNANCY PROBLEM | General Medical/Other |
| PSYCHIATRIC EVALUATION | Psychiatric, Behavioral, and Social Needs |
| RAPID HEART RATE | General Medical/Other |
| RASH | General Medical/Other |
| RECURRENT SKIN INFECTIONS | Skin/Soft Tissue Infection |
| RESPIRATORY DISTRESS | General Medical/Other |
| RIB INJURY | General Medical/Other |
| RING REMOVAL | General Medical/Other |
| RULE OUT STROKE | General Medical/Other |
| SEIZURES | General Medical/Other |
| SEPSIS OUTREACH | General Medical/Other |
| SEXUAL ASSAULT | Trauma |
| SHORTNESS OF BREATH | General Medical/Other |
| SHOULDER PAIN | General Medical/Other |
| SINUSITIS | General Medical/Other |
| SKIN PROBLEM | Skin/Soft Tissue Infection |
| SOCIAL DETERMINANTS SCREENING | Psychiatric, Behavioral, and Social Needs |
| SORE THROAT | General Medical/Other |
| SPASMS | General Medical/Other |
| STAB WOUND | Trauma |
| STROKE ALERT | General Medical/Other |
| SUICIDAL | Psychiatric, Behavioral, and Social Needs |
| SUICIDE ATTEMPT | Psychiatric, Behavioral, and Social Needs |
| SWELLING | General Medical/Other |
| SWELLING HEAD/NECK | General Medical/Other |
| SYNCOPE | General Medical/Other |
| TRAUMA | Trauma |
| URI | General Medical/Other |
| URINARY PROBLEM | General Medical/Other |
| VAGINAL BLEEDING | General Medical/Other |
| VAGINAL BLEEDING—PREGNANT | General Medical/Other |
| VASCULAR ACCESS PROBLEM | General Medical/Other |
| VENOUS THROMBOSIS | General Medical/Other |
| VOMITING | General Medical/Other |
| VOMITING BLOOD | General Medical/Other |
| WEAKNESS—GENERALIZED | General Medical/Other |
| WELLNESS VISIT | Psychiatric, Behavioral, and Social Needs |
| WITHDRAWAL | Opioid Withdrawal |
| WOUND CARE | Skin/Soft Tissue Infection |
| WOUND CHECK | Skin/Soft Tissue Infection |
| WOUND DEHISCENCE | Skin/Soft Tissue Infection |
| WOUND INFECTION | Skin/Soft Tissue Infection |
| WRIST PAIN | General Medical/Other |
References
- Quijano, T.; Crowell, J.; Eggert, K.; Clark, K.; Alexander, M.; Grau, L.; Heimer, R. Xylazine in the drug supply: Emerging threats and lessons learned in areas with high levels of adulteration. Int. J. Drug Policy 2023, 120, 104154. [Google Scholar] [CrossRef] [PubMed]
- DeBord, J.S.; Shinefeld, J.; Russell, R.; Denn, M.; Quinter, A.; Logan, B.K.; Teixeira da Silva, D.; Krotulski, A.J. Drug Checking—Quarterly Report; Center for Forensic Science Research and Education: Philadelphia, PA, USA, 2023; Available online: https://www.cfsre.org/images/content/reports/drug_checking/2023_Q1_and_Q2_Drug_Checking_Quarterly_Report_CFSRE_NPS_Discovery.pdf (accessed on 9 April 2025).
- Varshneya, N.B.; Thakrar, A.P.; Hobelmann, J.G.; Dunn, K.E.; Huhn, A.S. Evidence of buprenorphine-precipitated withdrawal in persons who use fentanyl. J. Addict. Med. 2022, 16, e265–e268. [Google Scholar] [CrossRef] [PubMed]
- London, K.; Li, Y.; Kahoud, J.L.; Cho, D.; Mulholland, J.; Roque, S.; Stugart, L.; Gillingham, J.; Borne, E.; Slovis, B. Tranq dope: Characterization of an ED cohort treated with a novel opioid withdrawal protocol in the era of fentanyl/xylazine. Am. J. Emerg. Med. 2024, 85, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Teixeira da Silva, D.; LaBoy, C.; Franklin, F. Hospitals and Behavioral Health Providers Are Reporting Severe and Worsening Presentations of Withdrawal Among People Who Use Drugs (PWUD) in Philadelphia; Philadelphia Department of Public Health, Health Alert: Philadelphia, PA, USA, 2024. Available online: https://hip.phila.gov/document/4874/PDPH-HAN-00444A-12-10-2024.pdf/ (accessed on 9 April 2025).
- Virtanen, R.; Savola, J.M.; Saano, V.; Nyman, L. Characterization of the selectivity, specificity and potency of medetomidine as an α2-adrenoceptor agonist. Eur. J. Pharmacol. 1988, 150, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Yaygıngül, R.; Belge, A. The comparison of clinical and cardiopulmonary effects of xylazine, medetomidine and detomidine in dogs. Ankara Univ. Vet. Fak. Derg. 2018, 65, 313–322. [Google Scholar] [CrossRef]
- Sugarman, O.K.; Shah, H.; Whaley, S.; McCourt, A.; Saloner, B.; Bandara, S. A content analysis of legal policy responses to xylazine in the illicit drug supply in the United States. Int. J. Drug Policy 2024, 129, 104472. [Google Scholar] [CrossRef] [PubMed]
- Huo, S.; London, K.; Murphy, L.; Casey, E.; Durney, P.; Arora, M.; McKeever, R.; Tasillo, A.; Goodstein, D.; Hart, B.; et al. Notes from the field: Suspected medetomidine withdrawal syndrome among fentanyl-exposed patients—Philadelphia, Pennsylvania, September 2024–January 2025. MMWR Morb. Mortal. Wkly. Rep. 2025, 74, 266–268. [Google Scholar] [CrossRef] [PubMed]
- Kukoyi, A.T.; Coker, S.A.; Lewis, L.D.; Nierenberg, D.W. Two cases of acute dexmedetomidine withdrawal syndrome following prolonged infusion in the intensive care unit: Report of cases and review of the literature. Hum. Exp. Toxicol. 2013, 32, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Wesson, D.R.; Ling, W. The clinical opiate withdrawal scale (COWS). J. Psychoact. Drugs 2003, 35, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Alexander, R.; Agwuncha, C.; Wilson, C.; Schrecker, J.; Holt, A.; Heltsley, R. Withdrawal signs and symptoms among patients positive for fentanyl with and without xylazine. J. Addict. Med. 2025, 19, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Kariisa, M.; O’Donnell, J.; Kumar, S.; Mattson, C.L.; Goldberger, B.A. Illicitly Manufactured Fentanyl–Involved Overdose Deaths with Detected Xylazine—United States, January 2019–June 2022. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, E.S.; Buchanan, J.; Aldy, K.; Shulman, J.; Krotulski, A.J.; Walton, S.E.; Logan, B.K.; Wax, P.M.; Campleman, S.; Brent, J.A.; et al. Notes from the Field: Detection of Medetomidine Among Patients Evaluated in Emergency Departments for Suspected Opioid Overdoses—Missouri, Colorado, and Pennsylvania, September 2020–December 2023. CDC MMWR Morb. Mortal. Wkly. Rep. 2024, 73, 672–674. [Google Scholar] [CrossRef] [PubMed]
- Philadelphia Department of Public Health. Health Alert: Medetomidine Detected in Philadelphia’s Illicit Drug Supply. 13 May 2024. Available online: https://hip.phila.gov/document/4421/PDPH-HAN-0441A-05-13-24.pdf (accessed on 6 October 2024).
- New York State Office of Addiction Services and Supports. Another Potent Sedative, Medetomidine, Now Appearing in Illicit Drug Supply. 31 May 2024. Available online: https://oasas.ny.gov/advisory-may-31-2024 (accessed on 6 October 2024).
- Krotulski, A.J.; Shinefeld, J.; Moraff, C.; Wood, T.; Walton, S.E.; DeBord, J.S.; Denn, M.T.; Quinter, A.D.; Logan, B.K. Medetomidine Rapidly Proliferating Across USA—Implicated in Recreational Opioid Drug Supply & Causing Overdose Outbreaks. CFSRE NPS Discovery Public Alert. 20 May 2024. Available online: https://www.cfsre.org/nps-discovery/public-alerts/medetomidine-rapidly-proliferating-across-usa-implicated-in-recreational-opioid-drug-supply-causing-overdose-outbreaks (accessed on 6 October 2024).
- Sood, N.; Dhillon, G. Illicit Medetomidine Use with Fentanyl. The Hospitalist. 1 January 2025. Available online: https://www.the-hospitalist.org/hospitalist/article/38385/addiction-medicine/illicit-medetomidine-use-with-fentanyl/ (accessed on 30 March 2025).
- Sood, N. Rise of illicit medetomidine use: A worrisome trend. Am. J. Addict. 2025, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Scheinin, H.; Virtanen, R.; MacDonald, E.; Lammintausta, R.; Scheinin, M. Medetomidine—A Novel Alpha2-Adrenoceptor Agonist: A Review of Its Pharmacodynamic Effects. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 1989, 13, 635–651. [Google Scholar] [CrossRef] [PubMed]
- Papich, M.G. Medetomidine Hydrochloride. In Saunders Handbook of Veterinary Drugs, 4th ed.; Papich, M.G., Ed.; W.B. Saunders: Philadelphia, PA, USA, 2016; pp. 481–483. [Google Scholar]
- New York City Department of Health and Mental Hygiene. What Is Xylazine? (Frequently Asked Questions). May 2023. Available online: https://www.nyc.gov/assets/doh/downloads/pdf/basas/xylazine-faq.pdf (accessed on 30 March 2025).
- Suárez-Lledó, A.; Padullés, A.; Lozano, T.; Cobo-Sacristán, S.; Colls, M.; Jódar, R. Management of Tizanidine Withdrawal Syndrome: A Case Report. Clin. Med. Insights Case Rep. 2018, 11, 1179547618758022. [Google Scholar] [CrossRef] [PubMed]
- Knapp, T.; DiLeonardo, O.; Maul, T.; Hochwald, A.; Li, Z.; Hossain, J.; Lowry, A.; Parker, J.; Baker, K.; Wearden, P.; et al. Dexmedetomidine Withdrawal Syndrome in Children in the PICU: Systematic Review and Meta-Analysis. Pediatr. Crit. Care Med. 2024, 25, 62–71. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.S.; McLaughlin, K.C.; Romero, N.; Crowley, K.E. Evaluation of Dexmedetomidine Withdrawal and Management After Prolonged Infusion. Clin. Ther. 2024, 46, 1034–1040. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).