Abstract
Background: The COVID-19 pandemic significantly disrupted forensic science, exposing vulnerabilities and introducing unprecedented challenges. Five years later, its impact persists, necessitating ongoing adaptations in forensic practice. This study examines key transformations, persistent issues, and emerging challenges in forensic science post-pandemic. Methods: A critical analysis of forensic science’s response to the pandemic was conducted, focusing on operational disruptions, methodological advancements, educational shifts, and technological integration. Results: Forensic operations faced delays due to case backlogs, restricted in-person work, and postponed court proceedings. Forensic pathology evolved with increased reliance on molecular autopsy techniques to clarify COVID-19-related deaths. Educational methods shifted toward virtual learning, prompting discussions on standardized digital training. Additionally, artificial intelligence and automation gained prominence in forensic investigations, enhancing crime scene analysis and predictive modeling. Discussion: While forensic science demonstrated adaptability, challenges remain in international collaboration, resource distribution, and professional training. The pandemic accelerated technological integration but also raised ethical and procedural concerns, particularly regarding AI applications in legal contexts. Virtual learning innovations necessitate further development to ensure competency in forensic training. Conclusions: Forensic science continues to evolve in response to post-pandemic realities. Addressing gaps in cooperation, technology implementation, and training will be crucial to strengthening the field. By assessing these changes, this study underscores forensic science’s resilience and adaptability, offering insights into its future trajectory amid ongoing challenges.
1. Introduction
The COVID-19 pandemic significantly impacted various aspects of human life, including forensic sciences, necessitating rapid adaptations to ensure both safety and procedural integrity [1,2,3]. Given the nature of SARS-CoV-2 transmission—primarily through airborne droplets but also via body fluids, tissues, and contaminated surfaces—stringent countermeasures were implemented to reduce infection risks [4]. The inherently multidisciplinary nature of forensic science, which encompasses crime scene investigations, external examinations, autopsies, and genetic and toxicological analyses, placed forensic professionals at particular risk. Furthermore, their frequent interaction with living individuals—such as victims of abuse, suspects, and individuals undergoing medicolegal examinations—further amplified exposure concerns [5,6,7,8,9].
Despite the next generation EU plan, five years after the peak of the pandemic, the urgency surrounding biosafety protocols has diminished, and financial constraints have pushed many healthcare systems, including Italy’s, back to pre-pandemic operational levels [10]. This regression raises concerns regarding the sustainability of protective measures introduced during the crisis. The reduction in funding for forensic investigations, the de-escalation of laboratory biosafety levels, and the discontinuation of advanced personal protective equipment (PPE) usage risk undoing the progress made in forensic biosecurity. Moreover, the lessons learned from COVID-19 highlight the necessity of maintaining a resilient and adaptable forensic framework capable of responding to future public health threats [11].
This narrative review aims to analyze the organizational, adaptational, and continuous changes within forensic sciences due to the COVID-19 pandemic, with a particular focus on how financial constraints have led to a rollback of critical countermeasures. It also underscores the urgent need to balance economic sustainability with preparedness for emerging infectious diseases, ensuring that forensic practices remain both safe and effective in the long term.
2. Forensic Science and SARS-CoV-2: Transmission Risks and Biosecurity Measures
The COVID-19 pandemic presented unprecedented challenges to forensic science, requiring significant adaptations to ensure both biosecurity and the continuity of essential forensic operations. The nature of forensic investigations places professionals at an increased risk of exposure to infectious agents, particularly in postmortem examinations, crime scene investigations, and laboratory analyses. Given the multiple routes through which SARS-CoV-2 can be transmitted, forensic institutions worldwide were compelled to reassess and reinforce safety protocols to minimize risks to personnel while maintaining the integrity of forensic procedures [12,13,14].
2.1. Routes of Transmission in Forensic Settings
Forensic professionals encounter various potential routes of SARS-CoV-2 transmission due to their interactions with both living individuals and contaminated materials. Conversely, studies have demonstrated that the risk of infection from deceased individuals significantly decreases, becoming almost negligible after 12 h post-mortem [4,15]. Understanding these pathways is crucial to developing appropriate protective measures.
2.1.1. Airborne Transmission
One of the primary concerns in forensic settings has been the airborne transmission of SARS-CoV-2. The virus spreads through respiratory droplets and aerosols expelled by infected individuals, which can remain suspended in the air for extended periods, especially in enclosed spaces with inadequate ventilation. This posed significant risks during forensic interviews, medicolegal examinations of living individuals, and autopsies [16,17].
Autopsy procedures, particularly those involving aerosol-generating techniques such as the use of oscillating saws for craniotomy or lung tissue sampling, created additional risks of airborne dissemination of viral particles [18,19]. These risks necessitated modifications in the forensic workflow, including limiting unnecessary procedures and improving ventilation systems in postmortem examination rooms.
2.1.2. Contact Transmission Through Biological Fluids and Tissues
Forensic practitioners frequently handle biological fluids and tissues, making contact transmission another significant risk. SARS-CoV-2 has been detected in various bodily fluids, including saliva, blood, and respiratory secretions, increasing the potential for direct exposure during sample collection, autopsies, and laboratory analyses [20,21]. Forensic pathologists and technicians performing autopsies on suspected or confirmed COVID-19 cases were particularly vulnerable due to their close contact with highly infectious materials.
Furthermore, forensic professionals involved in the collection of biological samples from living individuals, such as buccal swabs for DNA profiling or post-assault medical examinations, also faced an elevated risk of exposure [22]. This routine but high-risk procedures required the adoption of additional precautions, including increased use of personal protective equipment (PPE) and enhanced sanitization protocols [23].
2.1.3. Surface Contamination and Persistence of the Virus
The demonstrated persistence of SARS-CoV-2 on different surfaces added another layer of risk in forensic environments. Studies showed that the virus could remain viable for hours to days on materials commonly encountered in forensic settings, such as plastic, stainless steel, and paper [24,25,26,27]. This raised concerns regarding contamination of forensic laboratories, crime scene evidence, and autopsy tables.
Handling forensic evidence—ranging from documents and clothing to weapons and biological samples—required strict adherence to decontamination procedures to prevent cross-contamination and reduce infection risks. Proper disposal and sterilization of tools, equipment, and work surfaces became an essential part of forensic workflows to ensure biosafety [8,28].
2.2. Implementation of Biosafety Measures
Given the high-risk nature of forensic examinations during the pandemic, various forensic and public health organizations issued guidelines aimed at minimizing infection risks while maintaining forensic services. These measures encompassed the use of advanced PPE, modifications to laboratory biosafety protocols, strict decontamination procedures, and significant adjustments to autopsy practices [29,30].
2.2.1. Personal Protective Equipment (PPE)
The mandatory use of PPE became a cornerstone of forensic biosecurity measures. Forensic personnel were required to wear the following equipment:
N95 or FFP2/FFP3 respirators to filter airborne viral particles.
Face shields or goggles to protect against splashes from biological fluids.
Full-body protective suits to minimize direct skin contact.
Double-layered gloves to prevent contamination during handling of biological samples.
Shoe covers to reduce the risk of environmental contamination.
These PPE requirements extended to all forensic professionals involved in autopsies, sample collection, and crime scene investigations [30,31,32]. However, the increased demand for protective equipment also presented logistical challenges, including supply shortages and additional financial burdens on forensic institutions, particularly in underfunded systems like Italy’s.
2.2.2. Biosecurity Levels in Forensic Laboratories
Forensic laboratories dealing with biological specimens had to comply with heightened biosecurity requirements. International guidelines recommend that forensic laboratories handling SARS-CoV-2-infected samples be upgraded to Biosafety Level 3 (BSL-3), which includes the following:
Dedicated laboratory spaces with controlled access.
Use of biological safety cabinets (BSCs) for handling infectious samples.
Proper waste disposal systems for contaminated materials.
Regular biosafety training for forensic staff.
Upgrading forensic laboratories to meet BSL-3 standards required additional financial investments, which have since been difficult to maintain due to budget constraints [30,33]. As the pandemic subsided, many institutions reverted to pre-pandemic safety levels, raising concerns about preparedness for future outbreaks [34].
2.2.3. Decontamination Protocols
Enhanced disinfection procedures were crucial in reducing the risk of surface contamination in forensic settings. Key protocols included the following:
- Frequent cleaning of forensic workspaces with hospital-grade disinfectants.
- Sterilization of autopsy instruments, laboratory equipment, and protective gear.
- Safe handling and disposal of biological waste from forensic examinations.
Although these measures were essential during the peak of the pandemic, financial constraints and a perceived decline in urgency have led to a reduction in the rigor of decontamination practices. The lack of sustained funding and resources threatens to undermine the progress made in forensic biosafety [35,36].
2.2.4. Autopsy Adjustments and Safety Modifications
Forensic autopsies posed one of the highest risks for SARS-CoV-2 exposure, particularly due to aerosol-generating procedures [4,31,32,37]. To mitigate these risks, forensic institutions implemented several changes:
- Performing autopsies only when deemed essential, with non-invasive imaging (such as computer tomography (CT) scans) used as an alternative where possible.
- Restricting the number of personnel present in the autopsy room to minimize exposure.
- Utilizing closed-circuit ventilation systems to prevent aerosol dispersion.
- Encouraging the use of powered air-purifying respirators (PAPRs) in high-risk settings.
While these modifications effectively reduced infection risks, many forensic institutions have since relaxed these measures due to financial and logistical constraints. The return to pre-pandemic practices raises concerns about preparedness for future public health crises.
3. Modifications in Forensic Practices
The COVID-19 pandemic necessitated significant modifications in forensic practices to ensure the safety of professionals while maintaining the integrity of forensic investigations. Various forensic activities, including crime scene investigations, autopsies, and forensic genetics, required extensive procedural adjustments to mitigate the risks of viral transmission (Table 1).

Table 1.
Changes in forensic practices due to COVID-19.
These modifications not only shaped forensic protocols during the pandemic but also highlighted the need for long-term resilience in forensic science against future biosecurity threats [8,29,38,39,40].
3.1. Crime Scene Investigations
Crime scene investigations, which require meticulous handling of physical evidence and often involve close interactions among forensic personnel, law enforcement, and witnesses, were significantly altered due to infection control measures [5,41]. As summarized in Figure 1, the need to minimize direct human contact and potential viral exposure led to several procedural adaptations:
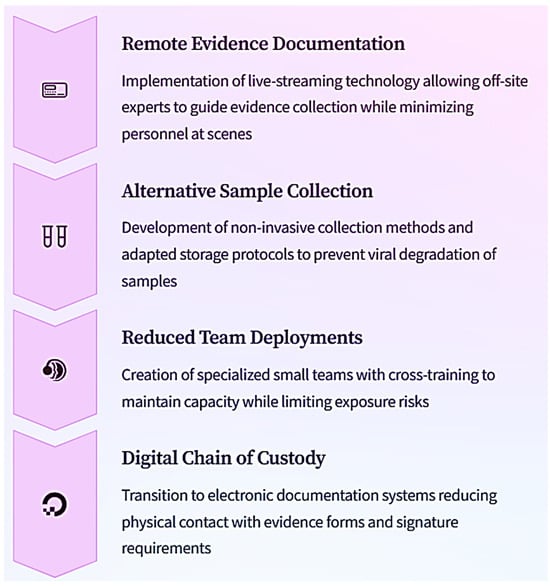
Figure 1.
Adapting crime scene investigation methodologies to pandemic period: These adaptations not only addressed immediate safety concerns but also accelerated the integration of technology into traditional crime scene processing methods, creating efficiencies that outlasted the pandemic itself. These adaptations underscored the necessity of integrating technology into forensic crime scene investigations, a trend that continues to evolve even beyond the pandemic period.
- Limited On-Site Personnel: A fundamental change was the reduction in the number of forensic investigators allowed at crime scenes. Typically, crime scene processing involves multiple professionals working in coordination, but during the pandemic, forensic teams were streamlined to include only essential personnel. This measure aimed to limit potential exposure while ensuring that critical investigative processes remained uninterrupted [22,42,43].
- Remote Consultation and Digital Forensic Tools: Advances in digital forensics and virtual collaboration became essential to overcoming the constraints imposed by the pandemic. Investigators increasingly relied on digital documentation, including high-resolution photography, 3D scanning, and video conferencing, to consult with colleagues and forensic experts remotely. This approach not only reduced the need for physical presence but also improved efficiency by allowing specialists to analyze crime scenes from a safe distance [44,45].
- Protective Equipment and Sanitization Measures: Given the possibility of surface contamination, forensic teams adopted additional protective layers, such as double-gloving techniques and enhanced decontamination procedures for tools and evidence bags. Evidence collection protocols were modified to ensure that items potentially exposed to SARS-CoV-2 were stored and transported safely to minimize contamination risks [23].
3.2. Autopsy and Postmortem Examinations
Among forensic disciplines, autopsy and postmortem examinations posed the highest risk of SARS-CoV-2 transmission. Handling cadavers infected with the virus required stringent biosecurity measures to protect forensic pathologists, technicians, and mortuary staff while maintaining the ability to perform necessary investigations.
- Selective Autopsy Criteria: Given the high transmission risk associated with postmortem examinations, many forensic institutions implemented selective autopsy policies, prioritizing cases with high forensic relevance. In some cases, external examinations and imaging techniques, such as postmortem CT or magnetic resonance imaging scans, were used as alternatives to full autopsies to reduce direct exposure to biological materials [46]. In our opinion, autopsy is the gold standard method to establish the cause of death, particularly in the unknown diseases [12,47,48,49].
- Closed-Chamber Autopsies and Airflow Control: To limit aerosol dispersion, many forensic facilities adopted closed-chamber autopsy rooms with controlled airflow and advanced ventilation systems. Negative pressure rooms, typically used in infectious disease control, became crucial in minimizing the spread of airborne particles during dissections [50,51].
- Avoidance of High-Risk Procedures: Procedures known to generate aerosols, such as the use of oscillating bone saws for cranial autopsies, were either avoided or modified. In some cases, manual dissection techniques replaced power tools to reduce the risk of airborne transmission. When high-risk procedures were unavoidable, additional protective barriers, such as plastic shields and vacuum suction devices, were used to contain aerosolized particles [52,53,54].
These modifications, though necessary for pandemic conditions, raised important discussions about long-term forensic autopsy safety protocols and the need for permanent infrastructure improvements in forensic pathology facilities.
3.3. Forensic Genetics and DNA Analysis
Forensic genetics and DNA analysis were also significantly impacted by the pandemic, particularly due to the need to handle biological samples with heightened infection control measures. The collection, transportation, and processing of genetic material required stricter biosafety protocols to prevent potential viral contamination while preserving sample integrity [22,55].
- Enhanced Biosafety Measures for Buccal Swabs: Buccal swabs, one of the primary sources for DNA profiling, presented a high risk of viral transmission due to their direct association with respiratory secretions. As a result, forensic laboratories implemented stricter guidelines for handling these samples, including additional layers of PPE, increased use of biosafety cabinets, and extended decontamination protocols for laboratory surfaces and equipment [56,57].
- Alternative Sample Collection Techniques: The pandemic accelerated the development and adoption of non-invasive or remote DNA collection methods. Instead of traditional buccal swabs, alternative biological sources such as hair, nails, and dried blood spots were explored for forensic DNA analysis. Additionally, self-collection kits for DNA samples were introduced in some jurisdictions to minimize direct interactions between forensic personnel and sample donors [58,59,60].
- Decontamination and Storage Protocols: Forensic laboratories introduced additional decontamination steps for incoming biological evidence, including UV irradiation and chemical disinfectants to ensure the safety of laboratory personnel. Moreover, modified storage protocols were implemented to balance biosecurity measures with the need to preserve DNA quality for forensic analysis [61,62].
These advancements in forensic genetics demonstrated the importance of biosafety measures in forensic laboratories and highlighted the need for sustained investments in biosecurity infrastructure, particularly as financial constraints threaten to revert forensic practices to pre-pandemic levels.
4. Legal and Judicial Implications
4.1. Impact on Criminal Case Processing
The COVID-19 pandemic had profound effects on the legal and judicial systems, particularly in the realm of forensic casework. As lockdowns and mobility restrictions were enforced worldwide, forensic science had to adapt to an evolving landscape of criminal activity and judicial procedures [63].
One of the most notable changes was the overall decline in certain types of crime. With people confined to their homes and public spaces heavily monitored or closed, crimes such as homicides, burglaries, and street thefts saw a temporary reduction [64]. However, this decline in traditional crime was counterbalanced by a sharp rise in other types of offenses, particularly cybercrime, domestic violence, and fraud. The increased reliance on digital communication, e-commerce, and online transactions created new opportunities for cybercriminals, leading to a surge in hacking incidents, online scams, and identity theft. Many of these crimes targeted vulnerable individuals seeking financial aid, healthcare services, or information about COVID-19 [65,66,67].
Simultaneously, the rise in domestic violence cases became a critical concern. The enforced confinement of individuals within their households, combined with economic stress and mental health challenges, led to a significant uptick in reported cases of intimate partner violence and child abuse. Forensic professionals specializing in trauma analysis, injury documentation, and DNA evidence collection played a crucial role in assisting legal proceedings related to these offenses. However, restrictions on in-person forensic examinations and court hearings led to delays in justice delivery [65,66].
Another major challenge was the disruption of judicial processes. Court closures and reduced staffing levels led to significant backlogs in criminal cases. Forensic laboratories faced delays due to limitations on personnel capacity, difficulties in procuring necessary equipment, and stringent biosecurity measures that slowed down processing times. The postponement of trials and evidentiary hearings meant that forensic evidence, particularly biological samples, had to be preserved for longer durations, raising concerns about sample degradation and chain-of-custody issues [68,69].
The transition to virtual court proceedings became an essential adaptation, allowing some legal processes to continue despite physical distancing requirements. Digital forensic evidence, including phone records, emails, and surveillance footage, became increasingly central to case resolutions. However, the reliance on virtual hearings also introduced new legal complexities, such as ensuring the authenticity and security of digital evidence, as well as maintaining the integrity of witness testimonies conducted remotely [70,71,72,73].
4.2. Rise in Medicolegal Disputes
The COVID-19 pandemic led to an unprecedented rise in medicolegal disputes, driven by concerns over medical care, institutional accountability, and death certification challenges. One of the primary areas of contention involved allegations of medical negligence in the treatment of COVID-19 patients. Lawsuits were filed against healthcare professionals and institutions, questioning the adequacy of clinical management, resource allocation, and adherence to evolving treatment protocols. In many cases, the legal system had to navigate complex issues of liability, considering the rapidly changing understanding of the virus and the extreme pressures on healthcare facilities [74,75,76].
Another major source of medicolegal disputes stemmed from the high mortality rates in nursing homes and long-term care facilities. Families of deceased patients sought legal action against institutions, citing concerns over insufficient protective measures, inadequate staffing, and failures in early detection and treatment of COVID-19 cases. These disputes often required forensic investigations to determine whether deaths were directly attributable to COVID-19 or exacerbated by pre-existing conditions, raising challenges in establishing causation and responsibility [77,78].
Additionally, the pandemic created significant difficulties in death certification and forensic pathology. Many cases required thorough postmortem examinations to distinguish between COVID-19 as a primary cause of death and deaths resulting from comorbidities or secondary complications. The legal system faced an influx of disputes over the accuracy of death certificates, particularly in cases where families contested official determinations, sometimes seeking alternative forensic assessments to challenge initial findings. These disputes had broader implications, influencing insurance claims, inheritance matters, and government compensation programs for COVID-19 victims [79,80,81].
Overall, the rise in medicolegal disputes during the pandemic underscored the need for clear forensic protocols, standardized death certification processes, and legal frameworks that account for the complexities of pandemic-related fatalities. The experience highlighted the importance of interdisciplinary collaboration between forensic experts, legal professionals, and healthcare providers to ensure transparency, accuracy, and justice in pandemic-related cases [82,83].
5. Psychological and Occupational Effects on Forensic Personnel
The COVID-19 pandemic placed unprecedented demands on forensic professionals, significantly impacting their workload, mental health, and overall well-being. As essential workers, forensic scientists, pathologists, and crime scene investigators had to navigate a rapidly evolving crisis while ensuring that justice processes remained functional. The heightened stress, prolonged working hours, and continuous exposure to pandemic-related fatalities took a severe toll on their psychological resilience and occupational stability [84].
5.1. Increased Workload and Stress
As previously described, since the COVID-19 pandemic, there has been no significant increase in the overall crime rate; indeed, due to the restriction measures, several crimes have resulted in a reduction. On the contrary, other activities are increasing, such as the post-mortem investigation and the infection monitoring procedures. Moreover, due to the stringent requirements imposed by accreditation guidelines, which mandate meticulous adherence to standardized procedures for documentation, examination, result verification, and reporting, there was an increase in healthcare stress conditions.
On the one hand, these measures are essential to ensure the quality, reliability, and consistency of forensic services. On the other hand, they are extremely demanding in terms of both time and resources. Nevertheless, it is evident that one of the most immediate consequences of the pandemic for forensic personnel was a dramatic increase in workload. Several factors contributed to this escalation, including:
- Extended procedural time due to safety measures: The implementation of enhanced biosecurity protocols, such as mandatory use of personal protective equipment (PPE), stringent decontamination procedures, and modified forensic workflows, significantly lengthened standard investigative and laboratory processes. Tasks that previously took hours now required additional time to ensure infection control, further straining already overburdened forensic teams [85].
- Surge in postmortem examinations: The pandemic resulted in an overwhelming rise in postmortem examinations, particularly in the early waves when cause-of-death determination became a contentious issue. Many jurisdictions require forensic pathologists to conduct autopsies on suspected COVID-19 victims to confirm diagnoses, ascertain possible medical negligence, and address legal disputes related to hospital or nursing home care. The increased caseload placed forensic teams under extraordinary pressure, leading to physical and emotional exhaustion [8].
- Impact on forensic genetics and DNA analysis: Laboratories specializing in forensic genetics faced unique challenges. Routine DNA profiling was complicated by the heightened risk of viral contamination, requiring additional biosafety precautions and delaying the analysis of critical evidence. The backlog of forensic casework, combined with reduced staffing due to quarantine measures, created significant delays in criminal investigations, exacerbating stress among forensic professionals [86].
- Emotional burden of handling COVID-19-related fatalities: Beyond the technical challenges, forensic personnel were constantly exposed to the grim realities of pandemic-related deaths. Investigating cases involving victims of COVID-19, often in distressing conditions such as overwhelmed hospital wards or makeshift morgues, took an emotional toll. Unlike other natural causes of death, COVID-19 deaths carried an added layer of anxiety, as forensic personnel not only documented the fatalities but also worried about their own safety and that of their families [40,87].
5.2. Burnout and Mental Health Considerations
The prolonged exposure to high-risk environments led to increased rates of burnout, anxiety, and psychological distress among forensic personnel. Burnout—a state of physical, emotional, and mental exhaustion caused by prolonged stress—became particularly prevalent during the pandemic due to the combination of excessive workloads, moral dilemmas, and lack of institutional support [88,89].
- Mental health struggles and post-traumatic stress: Forensic professionals often encountered harrowing scenes, such as mass casualties in hospitals or the remains of individuals who had died alone and gone undiscovered for days. These experiences, combined with the pressures of maintaining forensic accuracy under crisis conditions, contributed to symptoms of post-traumatic stress disorder (PTSD), depression, and anxiety. The sense of helplessness in witnessing large-scale mortality further intensified emotional distress [90,91,92].
- Limited access to psychological support: Despite the rising mental health concerns, forensic personnel often lacked access to adequate psychological support systems. Many departments operated under severe financial and logistical constraints, leaving forensic scientists and pathologists to cope with their stress in isolation. In some cases, informal peer support networks emerged, but these were insufficient in addressing the long-term mental health consequences of working through a global crisis [93,94].
- Structured debriefing and counseling programs: Some forensic institutions recognized the need for psychological intervention and implemented structured debriefing sessions after particularly distressing cases. These sessions allowed forensic personnel to process their experiences in a controlled environment, reducing the risk of cumulative stress. However, the effectiveness of these programs varied, depending on the resources available and the willingness of professionals to seek support [95,96].
- Rotational shift policies and workload distribution: To mitigate the psychological strain of continuous exposure to pandemic-related deaths, some forensic units adopted rotational shift policies. By ensuring that personnel alternated between high-risk and lower-risk forensic duties, institutions aimed to prevent burnout and provide professionals with periods of relative respite. However, due to staffing shortages, many forensic teams were unable to fully implement these policies, leaving employees overworked and exhausted [97,98].
- Moral injury and ethical dilemmas: Beyond physical and mental exhaustion, forensic professionals also faced moral and ethical dilemmas throughout the pandemic. Many were required to make difficult decisions regarding resource allocation, prioritization of forensic cases, and interactions with grieving families. The inability to provide families with clear answers regarding the deaths of their loved ones, particularly when pandemic-related restrictions limited forensic investigations, contributed to a sense of moral injury—an emotional burden resulting from ethical conflicts in professional duties [99].
The long-term psychological impact of the pandemic on forensic professionals remains an area of concern. While forensic institutions have gradually returned to pre-pandemic operational levels, the residual effects of burnout, PTSD, and emotional fatigue persist. The lessons learned from this crisis highlight the urgent need for comprehensive mental health support, improved occupational policies, and better preparedness for future global health emergencies.
6. Long-Term Implications and Future Directions
The long-term implications of the COVID-19 pandemic have reshaped forensic science, necessitating lasting adaptations in biosafety, technology, workforce management, and legal frameworks. While many of the measures adopted during the pandemic addressed immediate concerns, they also paved the way for a more resilient forensic system capable of responding to future public health crises. However, financial constraints and a return to pre-pandemic operational standards threaten to reverse some of these advancements (Figure 2).
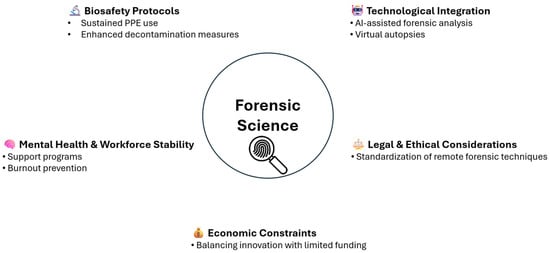
Figure 2.
This figure illustrates the key areas of forensic science that have undergone transformation due to the pandemic and highlights the necessary adaptations to ensure sustained progress. As forensic institutions navigate this new landscape, two critical aspects emerge: the need for integrating new safety standards to protect forensic personnel and maintain biosecurity (Section 6.1) and the continued technological advancements in forensic investigations that enhance efficiency and accuracy in forensic casework (Section 6.2).
6.1. Integration of New Safety Standards
The COVID-19 pandemic has had a lasting impact on forensic science, leading to the institutionalization of enhanced biosafety protocols. These changes are not only necessary for dealing with current biohazards but also serve as a precautionary framework for future pandemics or emerging infectious diseases. The integration of new safety standards has become a priority, ensuring that forensic professionals are better prepared for similar crises in the future [30,100].
One of the key adaptations has been the implementation of standardized biosafety protocols across forensic institutions. The pandemic highlighted vulnerabilities in forensic workflows, leading to a reassessment of occupational safety measures. PPE usage, routine decontamination procedures, and controlled work environments have now become a staple in forensic settings. Even as the immediate threat of COVID-19 diminishes, these protocols are likely to persist in safeguarding forensic personnel against other potential biological threats [7].
Additionally, forensic science has embraced remote methodologies to minimize physical presence at crime scenes and laboratories. The increased reliance on digital forensic tools allows experts to analyze evidence remotely, reducing the need for direct contact with potentially contaminated materials. While in-person forensic examinations remain crucial, virtual consultations and teleforensics are becoming valuable supplementary tools, enhancing efficiency while mitigating risks [101,102].
Another crucial shift has been the emphasis on continuous training for forensic personnel. The pandemic underscored the necessity for biohazard risk management skills, prompting forensic institutions to develop specialized training programs. These programs focus on safe handling of biological specimens, infection control measures, and emergency preparedness. Ensuring that forensic professionals are well-versed in biosecurity protocols is now a standard requirement, reinforcing a proactive rather than reactive approach to health crises [103].
6.2. Technological Advancements in Forensic Investigations
The challenges posed by the pandemic accelerated the adoption of cutting-edge technologies in forensic science. With the need to limit physical contact, forensic professionals turned into advanced technological solutions to facilitate investigations while maintaining safety [104,105].
One significant advancement has been the integration of artificial intelligence (AI) into forensic analysis. AI-assisted forensic tools can efficiently process vast amounts of evidence, identifying patterns and generating insights at a speed unattainable through manual analysis. Machine learning algorithms are increasingly being utilized to enhance crime scene reconstruction, DNA profiling, and digital forensic investigations. These AI-driven advancements not only improve accuracy but also expedite forensic workflows, addressing case backlogs that accumulated due to pandemic-related disruptions [106].
Another transformative development is the growing reliance on digital forensic techniques. The surge in cybercrime during the pandemic, including fraud, identity theft, and digital harassment, highlighted the need for forensic professionals to specialize in analyzing electronic evidence. Digital forensics now plays a crucial role in criminal investigations, with experts extracting, preserving, and interpreting data from electronic devices. The ability to conduct remote digital investigations has proven invaluable, reducing the need for in-person evidence collection while ensuring forensic integrity [107].
Additionally, contactless autopsy techniques have gained significant traction in forensic pathology. The use of virtual autopsies, employing advanced imaging technologies such as CT and magnetic resonance imaging, allows forensic pathologists to conduct postmortem examinations without direct contact with cadavers. These imaging techniques provide detailed insights into causes of death, offering a safer alternative to traditional autopsy methods, particularly in cases involving infectious diseases [108].
Beyond safety, virtual autopsies also present logistical and ethical advantages. In regions where autopsy procedures face cultural or religious objections, postmortem imaging provides a non-invasive alternative, facilitating forensic investigations without compromising sensitivities. Moreover, the ability to digitally store and revisit autopsy data enhances long-term forensic case management, allowing for secondary reviews and multidisciplinary consultations [109,110].
As forensic science continues to evolve, the integration of these technological advancements will play a pivotal role in shaping future investigative methodologies.
However, it also raises ethical and procedural issues which require critical and shared reflection. Therefore, these recent developments in forensic technology make it essential to promote international cooperation, adequate allocation of resources, preparedness of operators for exposure to traumatic events in operational, laboratory and judicial contexts, as well as support in stress management.
The pandemic has demonstrated that adaptability and innovation are essential in forensic practice, and the lessons learned will continue to influence forensic strategies in the years to come.
7. Conclusions
The COVID-19 pandemic reshaped forensic science, necessitating substantial modifications to ensure the safety of personnel while maintaining forensic integrity. Adaptations included enhanced biosecurity measures, revised forensic protocols, and the integration of new technologies. The crisis forced forensic professionals to develop more resilient practices, which have led to lasting improvements in the field.
While the immediate threat of COVID-19 has diminished, the lessons learned during the pandemic continue to shape forensic methodologies. Permanent biosafety protocols, technological advancements, and revised investigative approaches have strengthened forensic science, ensuring greater preparedness for future public health crises. However, financial constraints have threatened the sustainability of these improvements, particularly in countries where healthcare systems have reverted to pre-pandemic funding levels. Moving forward, it is crucial to secure long-term investments in forensic infrastructure, research, and training to maintain the progress achieved during the pandemic.
Future forensic practices must continue to prioritize biosafety while integrating innovations that emerged during this unprecedented global crisis. By leveraging the advancements made in biosecurity, digital forensics, and AI-driven investigations, forensic science can evolve into a more efficient, resilient, and adaptive discipline capable of responding to both present and future challenges.
Author Contributions
Conceptualization, M.C. and L.D.M.; methodology, M.C., M.F., S.F., G.V., R.R., N.D.F. and L.D.M.; validation, M.C. and L.D.M.; data curation, M.C., M.F., S.F., G.V., R.R., N.D.F. and L.D.M.; writing—original draft preparation, M.C., M.F., S.F. and G.V.; writing—review and editing, R.R., N.D.F. and L.D.M. All authors have read and agreed to the published version of the manuscript.
Funding
This work was partially supported by Department of Medical, Surgical and Advanced Technologies “G.F. Ingrassia”, University of Catania, 95121 Catania.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| PPE | personal protective equipment |
| BSL-3 | Biosafety Level 3 |
| BSCs | biological safety cabinets |
| CT | computed tomography |
| PTSD | post-traumatic stress disorder |
| AI | artificial intelligence |
References
- Pomara, C.; Li Volti, G.; Cappello, F. The Post-Lockdown Era: What Is next in Italy? Front. Pharmacol. 2020, 11, 1074. [Google Scholar] [CrossRef]
- Valenzano, A.; Scarinci, A.; Monda, V.; Sessa, F.; Messina, A.; Monda, M.; Precenzano, F.; Mollica, M.P.; Carotenuto, M.; Messina, G.; et al. The Social Brain and Emotional Contagion: COVID-19 Effects. Medicina 2020, 56, 640. [Google Scholar] [CrossRef] [PubMed]
- Pomara, C.; Sessa, F.; Galante, D.; Pace, L.; Fasanella, A.; Di Nunno, N.; Esposito, M.; Salerno, M. Do We Really Need Hazard Prevention at the Expense of Safeguarding Death Dignity in COVID-19? Diagnostics 2021, 11, 1913. [Google Scholar] [CrossRef]
- Pomara, C.; Salerno, M.; Sessa, F.; Esposito, M.; Barchitta, M.; Ledda, C.; Grassi, P.; Liberto, A.; Mattaliano, A.R.; Rapisarda, V.; et al. Safe Management Strategies in Clinical Forensic Autopsies of Confirmed COVID-19 Cases. Diagnostics 2021, 11, 457. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Sessa, F.; Cocimano, G.; Zuccarello, P.; Roccuzzo, S.; Salerno, M. Advances in Technologies in Crime Scene Investigation. Diagnostics 2023, 13, 3169. [Google Scholar] [CrossRef] [PubMed]
- OECD Policy Responses to Coronavirus (COVID-19). The Territorial Impact of COVID-19: Managing the Crisis Across Levels of Government. Available online: https://www.oecd.org/en/publications/the-territorial-impact-of-covid-19-managing-the-crisis-and-recovery-across-levels-of-government_a2c6abaf-en.html/ (accessed on 31 March 2023).
- Puzzo, I.; Aldridge-Waddon, L.; Stokes, N.; Rainbird, J.; Kumari, V. The Impact of the COVID-19 Pandemic on Forensic Mental Health Services and Clinical Outcomes: A Longitudinal Study. Front. Psychiatry 2022, 12, 780236. [Google Scholar] [CrossRef]
- Esposito, M.; Salerno, M.; Scoto, E.; Di Nunno, N.; Sessa, F. The Impact of the COVID-19 Pandemic on the Practice of Forensic Medicine: An Overview. Healthcare 2022, 10, 319. [Google Scholar] [CrossRef]
- Bertozzi, G.; Salerno, M.; Pomara, C.; Sessa, F. Neuropsychiatric and Behavioral Involvement in Aas Abusers. A Literature Review. Medicina 2019, 55, 396. [Google Scholar] [CrossRef]
- Vendramini, E.A.; Lega, F. Revitalizing the Italian NHS: Remarks on the 2021–2026 National Recovery Plan (next Generation EU). J. Hosp. Manag. Health Policy 2022, 6, 30. [Google Scholar] [CrossRef]
- Goniewicz, K.; Khorram-Manesh, A.; Burkle, F.M.; Hertelendy, A.J.; Goniewicz, M. The European Union’s Post-Pandemic Strategies for Public Health, Economic Recovery, and Social Resilience. Glob. Transit. 2023, 5, 201–209. [Google Scholar] [CrossRef]
- Sessa, F.; Salerno, M.; Pomara, C. Autopsy Tool in Unknown Diseases: The Experience with Coronaviruses (SARS-CoV, MERS-CoV, SARS-CoV-2). Medicina 2021, 57, 309. [Google Scholar] [CrossRef] [PubMed]
- Mondello, C.; Roccuzzo, S.; Malfa, O.; Sapienza, D.; Gualniera, P.; Ventura Spagnolo, E.; Di Nunno, N.; Salerno, M.; Pomara, C.; Asmundo, A. Pathological Findings in COVID-19 as a Tool to Define SARS-CoV-2 Pathogenesis. A Systematic Review. Front. Pharmacol. 2021, 12, 614586. [Google Scholar] [CrossRef] [PubMed]
- Pomara, C.; Volti, G.L.; Cappello, F.; Li Volti, G.; Cappello, F. COVID-19 Deaths: Are We Sure It Is Pneumonia? Please, Autopsy, Autopsy, Autopsy! J. Clin. Med. 2020, 9, 1259. [Google Scholar] [CrossRef]
- Salerno, M.; Sessa, F.; Piscopo, A.; Montana, A.; Torrisi, M.; Patanè, F.; Murabito, P.; Li Volti, G.; Pomara, C.; Volti, G.L.; et al. No Autopsies on COVID-19 Deaths: A Missed Opportunity and the Lockdown of Science. J. Clin. Med. 2020, 9, 1472. [Google Scholar] [CrossRef]
- Handiso, T.B.; Jifar, M.S.; Nuriye Hagisso, S. Coronavirus’s (SARS-CoV-2) Airborne Transmission. SAGE Open Med. 2022, 10, 20503121221094185. [Google Scholar] [CrossRef]
- Tang, S.; Mao, Y.; Jones, R.M.; Tan, Q.; Ji, J.S.; Li, N.; Shen, J.; Lv, Y.; Pan, L.; Ding, P.; et al. Aerosol Transmission of SARS-CoV-2? Evidence, Prevention and Control. Environ. Int. 2020, 144, 106039. [Google Scholar] [CrossRef]
- Sah, P.; Fitzpatrick, M.C.; Zimmer, C.F.; Abdollahi, E.; Juden-Kelly, L.; Moghadas, S.M.; Singer, B.H.; Galvani, A.P. Asymptomatic SARS-CoV-2 Infection: A Systematic Review and Meta-Analysis. Proc. Natl. Acad. Sci. USA 2021, 118, e2109229118. [Google Scholar] [CrossRef] [PubMed]
- Satturwar, S.; Fowkes, M.; Farver, C.; Wilson, A.M.; Eccher, A.; Girolami, I.; Pujadas, E.; Bryce, C.; Salem, F.; El Jamal, S.M.; et al. Postmortem Findings Associated with SARS-CoV-2: Systematic Review and Meta-Analysis. Am. J. Surg. Pathol. 2021, 45, 587–603. [Google Scholar] [CrossRef]
- Cox, J.; Christensen, B.; Burton, N.; Dunn, K.H.; Finnegan, M.; Ruess, A.; Estill, C. Transmission of SARS-CoV-2 in the Workplace: Key Findings from a Rapid Review of the Literature. Aerosol Sci. Technol. 2023, 57, 233–254. [Google Scholar] [CrossRef]
- Kutti-Sridharan, G.; Vegunta, R.; Vegunta, R.; Mohan, B.P.; Rokkam, V.R.P. SARS-CoV2 in Different Body Fluids, Risks of Transmission, and Preventing COVID-19: A Comprehensive Evidence-Based Review. Int. J. Prev. Med. 2020, 11, 97. [Google Scholar] [CrossRef]
- De Ungria, M.C.A. Forensic DNA Testing during the SARS-CoV-2 Pandemic. Forensic Sci. Int. Genet. 2020, 48, 102346. [Google Scholar] [CrossRef]
- Griswold, D.P.; Gempeler, A.; Kolias, A.; Hutchinson, P.J.; Rubiano, A.M. Personal Protective Equipment for Reducing the Risk of COVID-19 Infection among Health Care Workers Involved in Emergency Trauma Surgery during the Pandemic: An Umbrella Review. J. Trauma Acute Care Surg. 2021, 90, e72–e80. [Google Scholar] [CrossRef]
- Marquès, M.; Domingo, J.L. Contamination of Inert Surfaces by SARS-CoV-2: Persistence, Stability and Infectivity. A Review. Environ. Res. 2021, 193, 110559. [Google Scholar] [CrossRef]
- Ashokkumar, S.; Kaushik, N.K.; Han, I.; Uhm, H.S.; Park, J.S.; Cho, G.S.; Oh, Y.J.; Shin, Y.O.; Choi, E.H. Persistence of Coronavirus on Surface Materials and Its Control Measures Using Nonthermal Plasma and Other Agents. Int. J. Mol. Sci. 2023, 24, 14106. [Google Scholar] [CrossRef] [PubMed]
- Gidari, A.; Sabbatini, S.; Bastianelli, S.; Pierucci, S.; Busti, C.; Bartolini, D.; Stabile, A.M.; Monari, C.; Galli, F.; Rende, M.; et al. SARS-CoV-2 Survival on Surfaces and the Effect of Uv-c Light. Viruses 2021, 13, 408. [Google Scholar] [CrossRef] [PubMed]
- Musso, N.; Falzone, L.; Stracquadanio, S.; Bongiorno, D.; Salerno, M.; Esposito, M.; Sessa, F.; Libra, M.; Stefani, S.; Pomara, C. Post-Mortem Detection of SARS-CoV-2 RNA in Long-Buried Lung Samples. Diagnostics 2021, 11, 1158. [Google Scholar] [CrossRef] [PubMed]
- Sessa, F.; Esposito, M.; Cocimano, G.; Sablone, S.; Karaboue, M.A.A.; Chisari, M.; Albano, D.G.; Salerno, M. Artificial Intelligence and Forensic Genetics: Current Applications and Future Perspectives. Appl. Sci. 2024, 14, 2113. [Google Scholar] [CrossRef]
- Di Luise, E.; Magni, P.A. Interim Recommendations for the Management of Forensic Investigation during the COVID-19 Pandemic: An Italian Perspective. Sci. Justice 2021, 61, 735–742. [Google Scholar] [CrossRef]
- Prajapati, S.; Kaur, S. Safety Recommendations for Forensic Laboratory Staff During COVID-19 Pandemic. Acad. Forensic Pathol. 2021, 11, 94–102. [Google Scholar] [CrossRef]
- Cheung, J.C.H.; Ho, L.T.; Cheng, J.V.; Cham, E.Y.K.; Lam, K.N. Staff Safety during Emergency Airway Management for COVID-19 in Hong Kong. Lancet Respir. Med. 2020, 11, 94–102. [Google Scholar] [CrossRef]
- Baj, J.; Ciesielka, M.; Buszewicz, G.; Maciejewski, R.; Budzyńska, B.; Listos, P.; Teresiński, G. COVID-19 in the Autopsy Room-Requirements, Safety, Recommendations and Pathological Findings. Forensic Sci. Med. Pathol. 2021, 17, 101–113. [Google Scholar] [CrossRef] [PubMed]
- Cornish, N.E.; Anderson, N.L.; Arambula, D.G.; Arduino, M.J.; Bryan, A.; Burton, N.C.; Chen, B.; Dickson, B.A.; Giri, J.G.; Griffith, N.K.; et al. Clinical Laboratory Biosafety Gaps: Lessons Learned from Past Outbreaks Reveal a Path to a Safer Future. Clin. Microbiol. Rev. 2021, 34, e0012618. [Google Scholar] [CrossRef]
- Williams, B.A.; Jones, C.H.; Welch, V.; True, J.M. Outlook of Pandemic Preparedness in a Post-COVID-19 World. NPJ Vaccines 2023, 8, 178. [Google Scholar] [CrossRef] [PubMed]
- Weaver, D.T.; McElvany, B.D.; Gopalakrishnan, V.; Card, K.J.; Crozier, D.; Dhawan, A.; Dinh, M.N.; Dolson, E.; Farrokhian, N.; Hitomi, M.; et al. UV Decontamination of Personal Protective Equipment with Idle Laboratory Biosafety Cabinets during the COVID-19 Pandemic. PLoS ONE 2021, 16, e0241734. [Google Scholar] [CrossRef]
- Escandón, K.; Rasmussen, A.L.; Bogoch, I.I.; Murray, E.J.; Escandón, K.; Popescu, S.V.; Kindrachuk, J. COVID-19 False Dichotomies and a Comprehensive Review of the Evidence Regarding Public Health, COVID-19 Symptomatology, SARS-CoV-2 Transmission, Mask Wearing, and Reinfection. BMC Infect. Dis. 2021, 21, 710. [Google Scholar] [CrossRef] [PubMed]
- Yaacoub, S.; Schünemann, H.J.; Khabsa, J.; El-Harakeh, A.; Khamis, A.M.; Chamseddine, F.; El Khoury, R.; Saad, Z.; Hneiny, L.; Cuello Garcia, C.; et al. Safe Management of Bodies of Deceased Persons with Suspected or Confirmed COVID-19: A Rapid Systematic Review. BMJ Glob. Health 2020, 5, e002650. [Google Scholar] [CrossRef]
- Carretero-Barrio, I.; Lop-Gros, J.; Iglesias, M.; Martínez, C.; Matias-Guiu, X.; Pérez-Mies, B.; Palacios, J. Impact of the COVID-19 Pandemic on Pathology Training: A Survey among Spanish Residents. Virchows Arch. 2022, 481, 505–509. [Google Scholar] [CrossRef]
- Sacco, M.A.; Caputo, F.; Ricci, P.; Sicilia, F.; De Aloe, L.; Bonetta, C.F.; Cordasco, F.; Scalise, C.; Cacciatore, G.; Zibetti, A.; et al. The Impact of the COVID-19 Pandemic on Domestic Violence: The Dark Side of Home Isolation during Quarantine. Med.-Leg. J. 2020, 88, 71–73. [Google Scholar] [CrossRef]
- Manchia, M.; Gathier, A.W.; Yapici-Eser, H.; Schmidt, M.V.; de Quervain, D.; van Amelsvoort, T.; Bisson, J.I.; Cryan, J.F.; Howes, O.D.; Pinto, L.; et al. The Impact of the Prolonged COVID-19 Pandemic on Stress Resilience and Mental Health: A Critical Review across Waves. Eur. Neuropsychopharmacol. 2022, 55, 22–83. [Google Scholar] [CrossRef]
- Miller, M.T.; Jones, P. Crime Scene Investigation. In Forensic Science: An Introduction to Scientific and Investigative Techniques, 4th ed.; CRC Press: Boca Raton, FL, USA, 2014; ISBN 9781439853863. [Google Scholar]
- Lidén, M. The Impact of COVID-19 on Criminal Investigations and Proceedings in Sweden—A Snapshot of Practitioners’ Realities. Forensic Sci. Int. 2020, 2, 325–332. [Google Scholar] [CrossRef]
- Wüllenweber, S.; Giles, S. The Effectiveness of Forensic Evidence in the Investigation of Volume Crime Scenes. Sci. Justice 2021, 61, 542–554. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Shaikh, A.A.; Laghari, A.A.; Rind, M.M. Cloud Forensics and Digital Ledger Investigation: A New Era of Forensics Investigation. Int. J. Electron. Secur. Digit. Forensics 2023, 15, 1–23. [Google Scholar] [CrossRef]
- Nhamu, I.; Rita, M.N.; Katanga, J.; Hoff, A.A. Conducting Effective Digital Forensics Investigations in the COVID-19 Era. In Proceedings of the 2021 3rd International Multidisciplinary Information Technology and Engineering Conference, IMITEC 2021, Windhoek, Namibia, 23–25 November 2021. [Google Scholar]
- Fryer, E.P.; Traill, Z.C.; Benamore, R.E.; Roberts, I.S.D. High Risk Medicolegal Autopsies: Is a Full Postmortem Examination Necessary? J. Clin. Pathol. 2013, 66, 1–7. [Google Scholar] [CrossRef] [PubMed]
- D’Errico, S.D.; Zanon, M.; Montanaro, M.; Radaelli, D.; Sessa, F.; Di Mizio, G.; Montana, A.; Corrao, S.; Salerno, M.; Pomara, C.; et al. More than Pneumonia: Distinctive Features of SARS-CoV-2 Infection. from Autopsy Findings to Clinical Implications: A Systematic Review. Microorganisms 2020, 8, 1642. [Google Scholar] [CrossRef] [PubMed]
- Sessa, F.; Bertozzi, G.; Cipolloni, L.; Baldari, B.; Cantatore, S.; D’Errico, S.; Di Mizio, G.; Asmundo, A.; Castorina, S.; Salerno, M.; et al. Clinical-Forensic Autopsy Findings to Defeat COVID-19 Disease: A Literature Review. J. Clin. Med. 2020, 8, 2026. [Google Scholar] [CrossRef]
- Sessa, F.; Salerno, M.; Esposito, M.; Di Nunno, N.; Zamboni, P.; Pomara, C. Autopsy Findings and Causality Relationship between Death and COVID-19 Vaccination: A Systematic Review. J. Clin. Med. 2021, 10, 5876. [Google Scholar] [CrossRef]
- Keten, D.; Okdemir, E.; Keten, A. Precautions in Postmortem Examinations in COVID-19—Related Deaths: Recommendations from Germany. J. Forensic Leg. Med. 2020, 73, 102000. [Google Scholar] [CrossRef]
- Kyada, H.C.; Bhalara, R.V.; Vadgama, D.K.; Varu, P.K.; Trangadia, M.M.; Manvar, P.J.; Bhuva, S.D. Pathological Findings in COVID-19: A Conventional Autopsy-Based Study from India. Indian J. Med. Res. 2022, 155, 178–188. [Google Scholar] [CrossRef]
- Das, S.; Roy, A.; Das, R. New Autopsy Technique in COVID-19 Positive Dead Bodies: Opening the Thoracic Cavity with an Outlook to Reduce Aerosol Spread. J. Clin. Pathol. 2023, 76, 664–670. [Google Scholar] [CrossRef]
- Daniel, D.; Lin, M.; Luhung, I.; Lui, T.; Sadovoy, A.; Koh, X.; Sng, A.; Tran, T.; Schuster, S.C.; Jun Loh, X.; et al. Effective Design of Barrier Enclosure to Contain Aerosol Emissions from COVID-19 Patients. Indoor Air 2021, 31, 1639–1644. [Google Scholar] [CrossRef]
- Price, C.; Ben-Yakov, M.; Choi, J.; Orchanian-Cheff, A.; Tawadrous, D. Barrier Enclosure Use during Aerosol-Generating Medical Procedures: A Scoping Review. Am. J. Emerg. Med. 2021, 41, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Karthik, K.; Aravindh Babu, R.P.; Dhama, K.; Chitra, M.A.; Kalaiselvi, G.; Alagesan Senthilkumar, T.M.; Raj, G.D. Biosafety Concerns During the Collection, Transportation, and Processing of COVID-19 Samples for Diagnosis. Arch. Med. Res. 2020, 51, 623–630. [Google Scholar] [CrossRef]
- Yang, X.; Xu, Q.; Liu, H.; Xu, J.; Yang, D.; Xiao, C.; Hu, H.; Liu, Y.; Liu, C. Collection and Disinfection of Forensic Biological Specimens in Five Cases Concerning COVID-19 in Guangzhou, China. Forensic Sci. Int. 2020, 2, 210–214. [Google Scholar] [CrossRef] [PubMed]
- Bruijns, B. What Are the Limitations and Challenges of Swab-Based DNA Sampling? Forensic Sci. 2024, 4, 76–95. [Google Scholar] [CrossRef]
- Butler, J.M. Recent Advances in Forensic Biology and Forensic DNA Typing: INTERPOL Review 2019–2022. Forensic Sci. Int. 2023, 6, 100311. [Google Scholar] [CrossRef] [PubMed]
- Sessa, F.; Pomara, C.; Esposito, M.; Grassi, P.; Cocimano, G.; Salerno, M. Indirect DNA Transfer and Forensic Implications: A Literature Review. Genes 2023, 14, 2153. [Google Scholar] [CrossRef]
- Thornbury, D.; Goray, M.; van Oorschot, R.A.H. Indirect DNA Transfer without Contact from Dried Biological Materials on Various Surfaces. Forensic Sci. Int. Genet. 2021, 51, 102457. [Google Scholar] [CrossRef]
- Loibner, M.; Langner, C.; Regitnig, P.; Gorkiewicz, G.; Zatloukal, K. Biosafety Requirements for Autopsies of Patients with COVID-19: Example of a BSL-3 Autopsy Facility Designed for Highly Pathogenic Agents. Pathobiology 2021, 88, 37–45. [Google Scholar] [CrossRef]
- Buhr, T.L.; Borgers-Klonkowski, E.; Gutting, B.W.; Hammer, E.E.; Hamilton, S.M.; Huhman, B.M.; Jackson, S.L.; Kennihan, N.L.; Lilly, S.D.; Little, J.D.; et al. Ultraviolet Dosage and Decontamination Efficacy Were Widely Variable across 14 UV Devices after Testing a Dried Enveloped Ribonucleic Acid Virus Surrogate for SARS-CoV-2. Front. Bioeng. Biotechnol. 2022, 10, 875817. [Google Scholar] [CrossRef]
- Esposito, M.; Salerno, M.; Di Nunno, N.; Ministeri, F.; Liberto, A.; Sessa, F. The Risk of COVID-19 Infection in Prisons and Prevention Strategies: A Systematic Review and a New Strategic Protocol of Prevention. Healthcare 2022, 10, 270. [Google Scholar] [CrossRef]
- Liu, L.; Chang, J.; Long, D.; Liu, H. Analyzing the Impact of COVID-19 Lockdowns on Violent Crime. Int. J. Environ. Res. Public. Health 2022, 19, 15525. [Google Scholar] [CrossRef]
- Piquero, A.R.; Jennings, W.G.; Jemison, E.; Kaukinen, C.; Knaul, F.M. Domestic Violence during the COVID-19 Pandemic—Evidence from a Systematic Review and Meta-Analysis. J. Crim. Justice 2021, 74, 101806. [Google Scholar] [CrossRef]
- Usher, K.; Bhullar, N.; Durkin, J.; Gyamfi, N.; Jackson, D. Family Violence and COVID-19: Increased Vulnerability and Reduced Options for Support. Int. J. Ment. Health Nurs. 2020, 29, 549–552. [Google Scholar] [CrossRef] [PubMed]
- Buil-Gil, D.; Miró-Llinares, F.; Moneva, A.; Kemp, S.; Díaz-Castaño, N. Cybercrime and Shifts in Opportunities during COVID-19: A Preliminary Analysis in the UK. Eur. Soc. 2021, 23, S47–S59. [Google Scholar] [CrossRef]
- Godfrey, B.; Richardson, J.C.; Walklate, S. The Crisis in the Courts: Before and Beyond COVID. Br. J. Criminol. 2022, 62, 1036–1053. [Google Scholar] [CrossRef]
- Baldwin, J.M.; Eassey, J.M.; Brooke, E.J. Court Operations during the COVID-19 Pandemic. Am. J. Crim. Justice 2020, 45, 743–758. [Google Scholar] [CrossRef] [PubMed]
- Sanders, P.A. Video-Hearings in Europe Before, During and After the COVID-19 Pandemic. Int. J. Court. Adm. 2021, 12, 3. [Google Scholar] [CrossRef]
- Harker, L.; Ryan, M. Remote Hearings in Family Courts in England and Wales during COVID-19: Insights and Lessons. Fam. Court. Rev. 2022, 60, 207–219. [Google Scholar] [CrossRef]
- Lea, L.P. New Technologies in the Court: Remote Hearings and Hybrid Interpreting during the Pandemic. Across Lang. Cult. 2023, 24, 257–267. [Google Scholar] [CrossRef]
- Legg, M.; Song, A. The Courts, the Remote Hearing and the Pandemic: From Action to Reflection. Univ. N. S. W. Law J. 2021, 44, 126–166. [Google Scholar] [CrossRef]
- Filograna, L.; Manenti, G.; Arena, V.; Dell’Aquila, M.; Pascali, V.L.; Natale, L.; Colosimo, C.; Grassi, S.; Floris, R.; Oliva, A. Claimed Medical Malpractice in Fatal SARS-CoV-2 Infections: The Importance of Combining Ante- and Post-Mortem Radiological Data and Autopsy Findings for Correct Forensic Analysis. Forensic Imaging 2021, 25, 200454. [Google Scholar] [CrossRef]
- Klemann, D.; Mertens, H.; van Merode, F. Trends and Developments in Medical Liability Claims in The Netherlands. Healthcare 2022, 10, 1929. [Google Scholar] [CrossRef] [PubMed]
- Omboni, S.; Padwal, R.S.; Alessa, T.; Benczúr, B.; Green, B.B.; Hubbard, I.; Kario, K.; Khan, N.A.; Konradi, A.; Logan, A.G.; et al. The Worldwide Impact of Telemedicine during COVID-19: Current Evidence and Recommendations for the Future. Connect. Health 2022, 1, 7–35. [Google Scholar] [CrossRef]
- de Girolamo, G.; Bellelli, G.; Bianchetti, A.; Starace, F.; Zanetti, O.; Zarbo, C.; Micciolo, R. Older People Living in Long-Term Care Facilities and Mortality Rates During the COVID-19 Pandemic in Italy: Preliminary Epidemiological Data and Lessons to Learn. Front. Psychiatry 2020, 11, 586524. [Google Scholar] [CrossRef]
- Levin, A.T.; Jylhävä, J.; Religa, D.; Shallcross, L. COVID-19 Prevalence and Mortality in Longer-Term Care Facilities. Eur. J. Epidemiol. 2022, 37, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Nada, K.M.S.A.; Hsu, E.-S.; Seashore, J.; Zaidan, M.F.; Nishi, S.P.E.; Duarte, A.G.; Sharma, G. Determination of Cause of Death During COVID-19 Pandemic. In Proceedings of the American Thoracic Society 2021 International Conference, San Diego, CA, USA, 14–19 May 2021. [Google Scholar]
- Jacobson, S.H.; Jokela, J.A. Beyond COVID-19 Deaths during the COVID-19 Pandemic in the United States. Health Care Manag. Sci. 2021, 24, 661–665. [Google Scholar] [CrossRef]
- Xue, Y.; Lai, L.; Liu, C.; Niu, Y.; Zhao, J. Perspectives on the Death Investigation during the COVID-19 Pandemic. Forensic Sci. Int. 2020, 2, 126–128. [Google Scholar] [CrossRef]
- Pomara, C.; Salerno, M.; Miani, A.; Piscitelli, P. Autopsies in COVID-Related Deaths: The Need for Following the Model of German COVID-19 Autopsy Registry. Lancet Reg. Health—Eur. 2022, 17, 100392. [Google Scholar] [CrossRef]
- Aljerian, K.; BaHammam, A.S. COVID-19: Lessons in Laboratory Medicine, Pathology, and Autopsy. Ann. Thorac. Med. 2020, 15, 138–145. [Google Scholar] [CrossRef]
- Lombardo, C.; Capasso, E.; Li Rosi, G.; Salerno, M.; Chisari, M.; Esposito, M.; Di Mauro, L.; Sessa, F. Burnout and Stress in Forensic Science Jobs: A Systematic Review. Healthcare 2024, 12, 2032. [Google Scholar] [CrossRef]
- Magnavita, N.; Soave, P.M.; Antonelli, M. Prolonged Stress Causes Depression in Frontline Workers Facing the COVID-19 Pandemic—A Repeated Cross-Sectional Study in a COVID-19 Hub-Hospital in Central Italy. Int. J. Environ. Res. Public Health 2021, 18, 7316. [Google Scholar] [CrossRef] [PubMed]
- Bini, C.; Giorgetti, A.; Giovannini, E.; Pelletti, G.; Fais, P.; Pelotti, S. Human DNA Contamination of Postmortem Examination Facilities: Impact of COVID-19 Cleaning Procedure. J. Forensic Sci. 2022, 67, 1867–1875. [Google Scholar] [CrossRef]
- Simon, N.M.; Saxe, G.N.; Marmar, C.R. Mental Health Disorders Related to COVID-19-Related Deaths. JAMA—J. Am. Med. Assoc. 2020, 324, 1493–1494. [Google Scholar] [CrossRef] [PubMed]
- Babamiri, M.; Bashirian, S.; Khazaei, S.; Sohrabi, M.S.; Heidarimoghadam, R.; Mortezapoor, A.; Zareian, S. Burnout and Mental Health of COVID-19 Frontline Healthcare Workers: Results from an Online Survey. Iran. J. Psychiatry 2022, 17, 136–143. [Google Scholar] [CrossRef]
- Burrowes, S.A.B.; Casey, S.M.; Pierre-Joseph, N.; Talbot, S.G.; Hall, T.; Christian-Brathwaite, N.; Del-Carmen, M.; Garofalo, C.; Lundberg, B.; Mehta, P.K.; et al. COVID-19 Pandemic Impacts on Mental Health, Burnout, and Longevity in the Workplace among Healthcare Workers: A Mixed Methods Study. J. Interprof. Educ. Pract. 2023, 32, 100661. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J.; Phelps, A.J.; Ng, C.H.; Forbes, D. Diagnosis and Treatment of Post-Traumatic Stress Disorder during the COVID-19 Pandemic. Aust. J. Gen. Pract. 2020, 49, 785–789. [Google Scholar] [CrossRef]
- Karbasi, Z.; Eslami, P. Prevalence of Post-Traumatic Stress Disorder during the COVID-19 Pandemic in Children: A Review and Suggested Solutions. Middle East Curr. Psychiatry 2022, 29, 74. [Google Scholar] [CrossRef]
- Asim, M.; Van Teijlingen, E.; Sathian, B. Coronavirus Disease (COVID-19) and the Risk of Post-Traumatic Stress Disorder: A Mental Health Concern in Nepal. Nepal. J. Epidemiol. 2020, 10, 841–844. [Google Scholar] [CrossRef]
- Duden, G.S.; Gersdorf, S.; Stengler, K. Global Impact of the COVID-19 Pandemic on Mental Health Services: A Systematic Review. J. Psychiatr. Res. 2022, 154, 354–377. [Google Scholar] [CrossRef]
- Menculini, G.; Tortorella, A.; Albert, U.; Carmassi, C.; Carrà, G.; Cirulli, F.; Dell’osso, B.; Luciano, M.; Nanni, M.G.; Pompili, M.; et al. Access to Mental Health Care during the First Wave of the COVID-19 Pandemic in Italy: Results from the Comet Multicentric Study. Brain Sci. 2021, 11, 1413. [Google Scholar] [CrossRef]
- David, E.; DePierro, J.M.; Marin, D.B.; Sharma, V.; Charney, D.S.; Katz, C.L. COVID-19 Pandemic Support Programs for Healthcare Workers and Implications for Occupational Mental Health: A Narrative Review. Psychiatr. Q. 2022, 93, 227–247. [Google Scholar] [CrossRef] [PubMed]
- De Kock, J.H.; Latham, H.A.; Cowden, R.G. The Mental Health of Healthcare Workers during the COVID-19 Pandemic: A Narrative Review. Curr. Opin. Psychiatry 2022, 35, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Casjens, S.; Tisch, A.; Brenscheidt, F.; Beermann, B.; Brüning, T.; Behrens, T.; Rabstein, S. Investigating the Influence of Shift Work Rosters on Stress Measured as Cortisol in Hair during the SARS-CoV-2 Pandemic. Psychoneuroendocrinology 2022, 143, 105858. [Google Scholar] [CrossRef]
- Babamohamadi, H.; Davari, H.; Safari, A.A.; Alaei, S.; Pordanjani, S.R. The Association between Workload and Quality of Work Life of Nurses Taking Care of Patients with COVID-19. BMC Nurs. 2023, 22, 234. [Google Scholar] [CrossRef]
- Farrell, C.M.; Hayward, B.J. Ethical Dilemmas, Moral Distress, and the Risk of Moral Injury: Experiences of Residents and Fellows during the COVID-19 Pandemic in the United States. Acad. Med. 2022, 97, S55–S60. [Google Scholar] [CrossRef] [PubMed]
- Moretti, M.; Malhotra, A.; Visonà, S.D.; Finley, S.J.; Osculati, A.M.M.; Javan, G.T. The Roles of Medical Examiners in the COVID-19 Era: A Comparison between the United States and Italy. Forensic Sci. Med. Pathol. 2021, 17, 262–270. [Google Scholar] [CrossRef]
- Vermeulen, N.; Ata, B.; Gianaroli, L.; Lundin, K.; Mocanu, E.; Rautakallio-Hokkanen, S.; Tapanainen, J.S.; Veiga, A. A Picture of Medically Assisted Reproduction Activities during the COVID-19 Pandemic in Europe. Hum. Reprod. Open 2020, 2020, hoaa035. [Google Scholar] [CrossRef]
- Marin, L.; Ambrosini, G.; Fantò, F.M.; Della Vella, M.; Massaro, A.; Dessole, F.; Capobianco, G.; Andrisani, A. Telemedicine for Virtual Consultations During COVID-19 Pandemic in a Medically Assisted Reproduction Center: Patients’ Perspective. Telemed. E-Health 2023, 29, 459–465. [Google Scholar] [CrossRef]
- Roux, C.; Weyermann, C. Can Forensic Science Learn from the COVID-19 Crisis? Forensic Sci. Int. 2020, 316, 110503. [Google Scholar] [CrossRef]
- Majeed, A.; Zhang, X. On the Adoption of Modern Technologies to Fight the COVID-19 Pandemic: A Technical Synthesis of Latest Developments. COVID 2023, 3, 90–123. [Google Scholar] [CrossRef]
- Pomara, C.; Zappalà, S.A.; Salerno, M.; Sessa, F.; Esposito, M.; Cocimano, G.; Ippolito, S.; Miani, A.; Missoni, E.; Piscitelli, P. Migrants’ Human Rights and Health Protection during the COVID-19 Pandemic in the Mediterranean Sea: What We Have Learnt from Direct Inspections in Two Italian Hotspots. Front. Public Health 2023, 11, 1129267. [Google Scholar] [CrossRef] [PubMed]
- Dinis-Oliveira, R.J.; Azevedo, R.M.S. ChatGPT in Forensic Sciences: A New Pandora’s Box with Advantages and Challenges to Pay Attention. Forensic Sci. Res. 2023, 8, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Cruz, C. Innovative Learning in a Digital Forensics Laboratory: Tools and Techniques for Data Recovery. Appl. Sci. 2024, 14, 11095. [Google Scholar] [CrossRef]
- Cergan, R.; Taciuc, I.A.; Dumitru, M.; Vrinceanu, D.; Manole, F.; Sanda, N.; Marinescu, A.N. The Current Status of Virtual Autopsy Using Combined Imaging Modalities: A Scoping Review. J. Clin. Med. 2025, 14, 782. [Google Scholar] [CrossRef] [PubMed]
- Sessa, F.; Chisari, M.; Esposito, M.; Karaboue, M.A.A.; Salerno, M.; Cocimano, G. Ethical, Legal and Social Implications (ELSI) Regarding Forensic Genetic Investigations (FGIs). J. Acad. Ethics 2024, 1–21. [Google Scholar] [CrossRef]
- Smith, M.J.; Ahmad, A.; Arawi, T.; Dawson, A.; Emanuel, E.J.; Garani-Papadatos, T.; Ghimire, P.; Iliyasu, Z.; Lei, R.; Mastroleo, I.; et al. Top Five Ethical Lessons of COVID-19 That the World Must Learn. Wellcome Open Res. 2021, 6, 17. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).