Abstract
Background: Mucostatic impressions have been always indicated in thin, sharp, or flabby ridges, and have been addressed for their beneficial effect on long-term residual ridge stability. Nonetheless, a purely mucostatic impression was not possible until intraoral scans became available. This provides an option for digital removable denture which is biologically sensible but might reduce retention in comparison with a mucocompressive impression with border molding. On the other hand, pressure applied to the mucosa may have harmful effects on the long-term residual ridge stability, causing higher resorption and ultimately reduced denture retention. Hence, the possibility to merge mucostatics and mucocompressive philosophies would be a clinically and biologically sensible option for oral rehabilitation in aging populations where patients will potentially wear dentures for longer periods. This possibility is demonstrated in this technical report with a cast-free digital workflow. Technique: Baseplates for occlusion rims, closely adapted to the mucosa, were designed on intraoral scans of edentulous arches and, once 3D-printed, used to register maxillomandibular relations and information for tooth arrangement, as well as to perform border molding. Occlusion rims were then scanned and, within the 3Shape Dental System 2024 software program, the intaglio surfaces of their baseplates were segmented and inverted to obtain the digital master casts which incorporated the precise reproduction of the molded borders. Then, denture design was performed and manufactured; no limitations regarding manufacturing options are applicable to the presented technique. Conclusions: The potential benefits (i.e., improved retention in the initial period after denture delivery and the preservation of tissues) of the presented digital cast-free workflow, based on merging mucostatic and mucocompressive philosophies to obtain dentures with a mucostatic intaglio surface and functional borders, are sensible clinical outcomes which recommend the clinical application of the technique, although further validation, especially in the long term, is required.
1. Introduction
The world’s aging population is a significant achievement of science and medicine, but it may present challenges in ensuring health and quality of life for people living longer. It has already been emphasized that maintaining and improving oral health is one of the key factors for active aging [1]. Enhancing accessibility to basic dental treatments, including removable dentures, is essential in achieving this goal.
Digital technologies applied to removable prosthodontics could be the key to providing effective [2] and affordable oral rehabilitations for edentulous patients.
Complete dentures made with digital protocols were reported more than a decade ago [3]. Over time, they have gained popularity among clinicians because improvements in both subtractive and additive technologies have been proved to streamline the fabrication process and reduce time and processes [3]; this is beneficial to add standardization and reduce procedure/operator-related error, thus enhancing the quality of fabricated dentures. Thus, digital denture protocols provide both clinicians and patients with more affordable treatment options [4], contributing to accessibility to treatment and ultimately improving the quality of life of edentulous patients [5].
It has been noted that digital dentures encompass a wide range of combinations of clinical and laboratory techniques with related technologies and materials [6]. Whether they are part of manufacturer-dependent systems [7] or open protocols [8], what truly differentiates current digital denture systems/protocols is the type of impression used as a starting point: a digitized conventional impression or an intraoral scan (IOS) of the edentulous arches [9]. This is not merely a different starting method; it involves adopting the mucocompressive or mucostatic impression philosophy and their respective conceptual frameworks. A detailed discussion on this topic is beyond the scope of this report; what is of interest here is the different physics behind denture retention. Respectively, for the mucocompressive or mucostatic philosophy, this involves the suction effect obtained through functional border molding and the creation of a post-palatal seal area by applying pressure, or the surface tension forces occurring between two precisely congruent wet surfaces (i.e., the edentulous mucosa and the intaglio surface of the denture base). In other words, assuming that the denture base is congruent with the impression and net of manufacturing tolerances, the type of impression becomes a practical tool to incorporate specific features or differences into the denture base, which may affect denture retention and have various clinical implications. Dentures created using a mucocompressive impression may offer enhanced initial retention, positively impacting patient acceptance and comfort. This is particularly beneficial for patients with neuromuscular disorders, cognitive impairments [10], or age-related neuroplasticity reduction [11], which may hinder their ability to adapt to dentures [12,13]. However, the pressure applied to tissues has been shown to increase residual ridge resorption [14], leading to the misfit of the denture base [15] and potentially causing tissue impingement, pressure spots, or traumatic ulcers. Conversely, dentures made from a mucostatic impression, such as an IOS, might be less retentive, but the even distribution of loads on underlying tissues can better preserve the residual ridge [14]. This makes them the preferred choice when thin, sharp, or flabby ridges are present [16].
This aspect is crucial, especially considering increased life expectancy, which means that patients may need to wear dentures for longer periods. Therefore, preserving tissues as much as possible is both biologically and practically sensible. Clinically, it would be beneficial to combine mucostatic and mucocompressive philosophies to leverage the advantages of both. Because there is no option with a conventional technique to actually obtain mucostatics, digital technologies are needed to accomplish such a task. This means not only exploiting the whole potential and benefit of intraoral scanning technology, together with the reliability of CAM technologies, but also taking advantage of an additional aspect which only digital technologies can offer: the opportunity to merge different sets of data acquired under the two different philosophies. Although this is theoretically feasible in a CAD software environment, practically there is no option to realize it in a streamlined process. A technique has been reported that uses a dedicated CAD software program to achieve this [6].
While effective, this method is system-dependent, requires some workarounds, and cannot be applied in other common clinical/laboratory settings based on different CAD environments, limiting access to this beneficial treatment option (i.e., digital dentures combining advantages from both mucostatic and mucocompressive philosophies). Thus, extending the feasibility of this option to other common CAD environments would make its use more accessible and widespread.
In this technical report, a new technique is presented to merge the concepts and advantages of mucostatic and mucocompressive philosophies; this is obtained with a digital denture cast-free workflow, based on intraoral scans of edentulous arches, capable of creating a denture with a mucostatic base on which functional borders are incorporated. In order to favor its inclusion in a standard production environment, a leading industry CAD environment was used for the technique demonstration.
2. Technique Description
The basic steps used in the current workflow are those reported to incorporate open technologies into a digital denture protocol [8], subsequently modified in order to use intraoral scans [9], and here adapted to obtain the above-mentioned results, as follows:
- Use an intraoral scanner (TRIOS 4; 3Shape A/S, Copenhagen, Denmark) to capture the IOS of the edentulous arches. Utilize instruments for the proper retraction and stabilization of tissues (Lo Russo Retractors; ELDO srl). Process and export the scans (Figure 1).
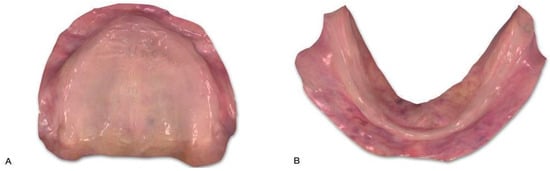 Figure 1. Intraoral scans. (A) Maxilla. (B) Mandible.
Figure 1. Intraoral scans. (A) Maxilla. (B) Mandible. - Design and 3D print baseplates for the fabrication of occlusion rims (ORs). Use the workflow for individual impression trays in the 3Shape Dental System 2024 software program (3Shape A/S, Copenhagen, Denmark) and set the material space to zero so that the baseplates are the negative of the mucosa. The standard tessellation language (STL) files of the designed baseplates can be printed with 0.2 mm thick layers using a 1.75 mm diameter PLA filament (Prusament PLA; Prusa Research, Prague, Czech Republic) in a desktop 3D printer (Prusa i3 MK3; Prusa Research, Prague, Czech Republic) with a 0.4 mm diameter nozzle, according to manufacturer recommendations for infilling, temperature, and printing speed.
- Complete the fabrication of the ORs by manually adding wax (Bite Wax Rims; Henry Schein Inc., Melville, NY, USA) to the baseplates printed in step 2.
- Check the ORs for adaptation and accuracy before proceeding with the border molding procedure. A thermoplastic material (Iso Functional; GC Corporation, Tokyo, Japan) can be used for this task.
- Use the ORs to register and record all parameters for tooth arrangement (occlusal plane, lip support, maxillary incisor length, midline, and smile line), as well as the vertical dimension and maxillo-mandibular relationships. Once a centric relation record is developed and evaluated as a repeatable position, a suitable recording material (Registrado X-tra; VOCO GmbH, Cuxhaven, Germany) may be used to record it in the ORs.
- The ORs, incorporating all the information described in step 5, can be scanned extraorally as a single object using an intraoral scanner (TRIOS 4; 3Shape A/S, Copenhagen, Denmark) to obtain the corresponding STL file (Figure 2).
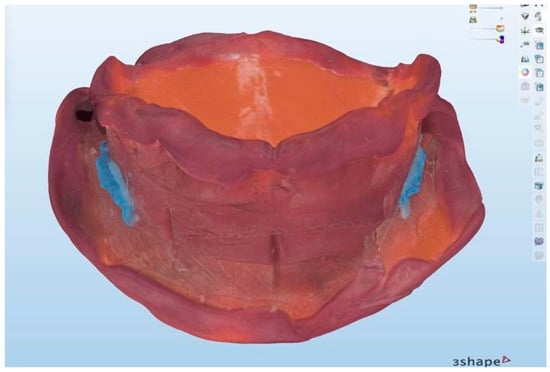 Figure 2. Registered occlusion rims with border molding.
Figure 2. Registered occlusion rims with border molding. - Create the order (referred to as “order” in the 3Shape Dental System 2024 software program) for the maxillary and mandibular complete dentures. Import the scan obtained in step 6 into the created order. The same scan will be used for the maxillary arch, mandibular arch, and wax rim.
- Begin the denture design workflow. At the “refine scan” step, select “impression” as the type of scan. Set the occlusal plane according to the information recorded in the ORs. In the subsequent steps, trim the scans by selecting the intaglio surface of the OR baseplate, including the molded border. Trim the corresponding intaglio surface of the OR baseplate for the maxillary (Figure 3A) and mandibular (Figure 3B) arches. The goal is to create digital master casts (Figure 4A,B) from the trimmed surfaces. Since the intaglio surfaces of the baseplates are the negative images of the IOS of the edentulous arches, selecting “impression”, as described earlier, allows the use of their positive side for creating digital master casts. These digital master casts will also include the precise reproduction of the molded borders.
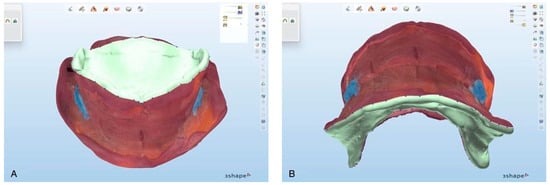 Figure 3. Trimming intaglio surface (light green area) of occlusion rims. (A) Maxilla. (B) Mandible.
Figure 3. Trimming intaglio surface (light green area) of occlusion rims. (A) Maxilla. (B) Mandible.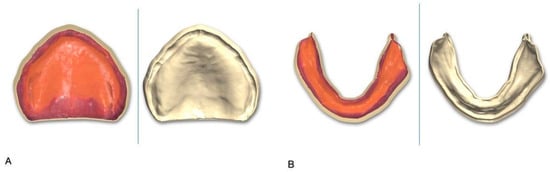 Figure 4. Digital master casts obtained by occlusion rim trimming. Color view (left) and textured view (right). (A) Maxilla. (B) Mandible.
Figure 4. Digital master casts obtained by occlusion rim trimming. Color view (left) and textured view (right). (A) Maxilla. (B) Mandible.
In this step, within the order, you have three copies of the same object (the scan obtained in step 6). From two of these copies, trimming the intaglio surface of the maxillary and mandibular baseplates of the ORs allowed the creation of the digital master casts. The third copy (wax rim) is left untrimmed (Figure 5) to retain all the information registered on the patient for tooth arrangement.
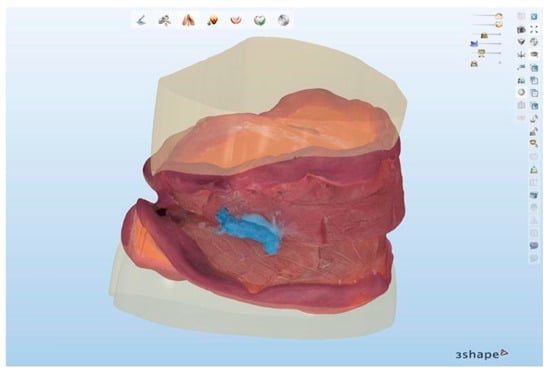
Figure 5.
The occlusion rims will provide both digital master casts and information for tooth arrangement.
Proceed with the denture design workflow. If the baseplates of the ORs are precisely trimmed, the extension of the denture base will match the trimmed surfaces (Figure 6A,B) and will accurately reproduce the molded borders (Figure 7 and Figure 8).
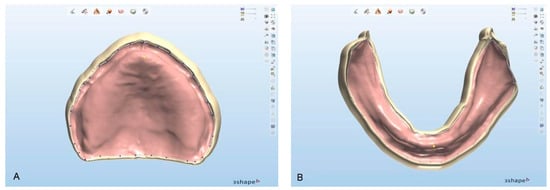
Figure 6.
Denture borders as defined by trimmed surfaces from occlusion rims. (A) Maxilla. (B) Mandible.
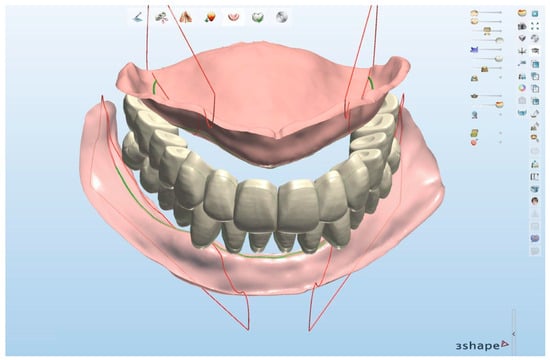
Figure 7.
Tooth setup: Detail of intaglio surfaces obtained from trimming of occlusion rims.
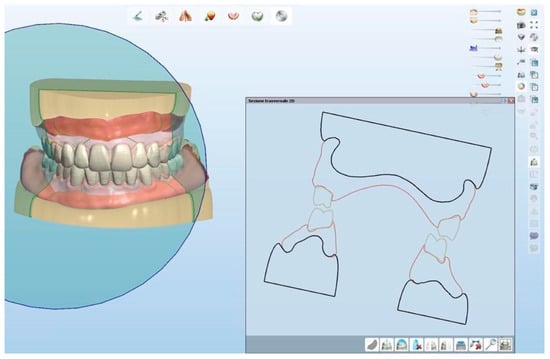
Figure 8.
Cross section of designed denture and digital casts. Denture borders are actually negative of molded borders of occlusion rims.
- 9.
- Create a rapid prototype of the trial dentures [17] and clinically assess it with the patient. Then, proceed with your preferred fabrication technology (milling or 3D printing) and materials of choice for denture manufacturing and finalization. Discussing the rationale behind such aspects is beyond the scope of this paper. For the example case shown in this report, milling was chosen for both denture bases and teeth. Pictures of the definitive dentures and the patient wearing them are shown in Figure 9 and Figure 10.
 Figure 9. Definitive dentures fabricated by using milling: intraoral picture.
Figure 9. Definitive dentures fabricated by using milling: intraoral picture.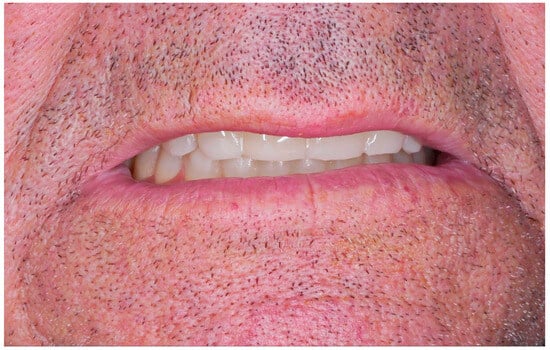 Figure 10. Patient with definitive dentures.
Figure 10. Patient with definitive dentures.
A summary of the specifications of the materials and equipment used, together with an estimate of the time required for each step, is reported in Table 1.

Table 1.
Specifications of the materials and equipment used.
3. Discussion
The retention and stability of removable dentures are crucial for successful rehabilitation in removable prosthodontics. It has already been demonstrated that digital dentures are characterized by higher retention and fit in comparison with dentures fabricated using conventional techniques [2]. Similarly, digital manufacturing technologies have been shown to provide a high trueness of denture bases, assuming CAD designs as reference [18], and less, if any, distortion [7]. Besides accuracy in manufacturing, denture retention and stability can be influenced by specific denture features (e.g., the accuracy of the denture base, flange extension, and peripheral seal) that adhere to different physical principles based on specific conceptual frameworks (i.e., mucostatics or mucocompression). Additionally, they depend on the active participation of the patient’s muscles, which can enhance both retention and stability. Initially, after a new or replacement denture is inserted, retention is primarily achieved through the physical characteristics of the denture and relies less on motor skills [12]. Over time, however, neuromuscular adaptation to the denture may become more significant, provided that the ability to learn new motor skills or adapt existing motor patterns is not impaired by reduced neuroplasticity [11,19]. This adaptation process requires time; therefore, a denture with higher retention immediately after insertion is preferable as it may offer greater comfort to the patient and facilitate the adaptation process. Since a better initial retention has been described [20] as a result of using the conventional mucocompressive impression to fabricate a denture, if the primary aim is favoring the adaptation process, starting from a conventional impression may be sensible from a clinical point of view. However, when retention is achieved by applying continuous pressure on the mucosal tissues, as with mucocompressive impressions, it can lead to long-term tissue damage [14]. This pressure accelerates the resorption of the residual ridge [14], resulting in a worsening fit of the denture over time. If the denture base is repeatedly adapted with additional mucocompressive impressions, a harmful cycle may begin, impairing both the stability of the denture and the health and preservation of the residual ridge [6].
For these reasons, combining the benefits of both mucostatics (tissue preservation) and mucocompression (improved initial retention) is sensible and relevant, especially for older adults or patients with neurological issues affecting motor skills. To achieve this goal, the denture should have a mucostatic intaglio surface for tissue preservation, which is possible using IOS, combined with functionally molded borders and a post-palatal seal area for improved retention [6]. This is the rationale behind the technique presented in this report. To date, there is no conventional technique capable of creating a mucostatic denture base because of issues related to impression and manufacturing. All impression materials exert, to some extent, compression of tissues; hence, a mucostatic base cannot be made on an impression which, by definition, captures a “compressed” representation of the anatomy of the edentulous arches and tissues. In addition, there is no agreement on the most effective material or compression technique [21]. On the other hand, using conventional manufacturing processes and techniques inevitably results in a significant distortion or deformation in different dimensions of the denture base [22,23,24], which is clearly a major limitation to achieve a passive, mucostatic fit of the base on the edentulous arches. As a consequence, the only option to obtain a mucostatic denture base is through the use of digital technologies which make it possible to obtain a pure mucostatic impression of the edentulous arches [25] using intraoral scans and manufacture CAD/CAM materials in their final state with almost no processing distortion [26] and manufacturing tolerances close to zero [7]. Besides the manufacturing and material technologies, there is an additional relevant task that digital technologies may handle: the design process within a CAD software environment, which offers the unique opportunity to merge and use different sets of data. This is not only cost-effective [3] and beneficial to decrease the clinical steps and laboratory procedures [27] but, in the particular case of the proposed technique, also makes it possible to merge data from the intraoral scans with those from the border molding procedure, which is the key to obtaining the desired goal of merging benefits from mucostatic and mucocompressive philosophies. Using the described digital workflow, the present technique makes this possible and straightforward within a single integrated system of equipment and software, which are leading industry options in the field of digital dentures and commonly used in the routine design and manufacture of clinical and dental laboratory environments, thus potentially promoting its widespread application in routine clinical practice.
A potential limitation of the proposed technique is that the intaglio surface of the denture base mirrors the digital casts obtained by the segmentation and inversion of the intaglio surface from the baseplates of the occlusion rims which were derived from IOS. This means that the denture’s intaglio surface is essentially the negative of the IOS, with accuracy dependent on the precision of the equipment and the manufacturing technology used to fabricate the baseplates of the occlusion rims. The chosen 3D-printing technology has demonstrated excellent accuracy [17], supporting the assumption that the denture base closely mirrors the IOS. Additional limitations may be related to the fact that the present technique does not provide quantitative and qualitative data related to its performance but just describes how to obtain a specific and sensible goal in a common clinical setup.
4. Conclusions
In conclusion, the potential benefits (i.e., improved retention in the initial period after denture delivery and the preservation of tissues) of the presented digital cast-free workflow, made possible by merging mucostatic and mucocompressive philosophies to obtain dentures with a mucostatic intaglio surface and functional borders, are sensible clinical outcomes which recommend the clinical application of the technique, although further validation, especially in the long term, is required.
Author Contributions
Conceptualization, L.L.R. and L.G.; methodology, L.L.R.; software, L.L.R.; validation, L.G.; formal analysis, D.C.; investigation, F.E.; data curation, L.L.R.; writing—original draft preparation, L.G.; writing—review and editing, F.E., M.L. and A.D.L.; visualization, D.C.; supervision, L.L.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- WHO. Active Ageing: A Policy Framework; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Srinivasan, M.; Kamnoedboon, P.; McKenna, G.; Angst, L.; Schimmel, M.; Özcan, M.; Müller, F. CAD-CAM Removable Complete Dentures: A Systematic Review and Meta-Analysis of Trueness of Fit, Biocompatibility, Mechanical Properties, Surface Characteristics, Color Stability, Time-Cost Analysis, Clinical and Patient-Reported Outcomes. J. Dent. 2021, 113, 103777. [Google Scholar] [CrossRef]
- El Osta, N.; Bessadet, M.; Drancourt, N.; Batisse, C. Time Efficiency and Cost of Fabricating Removable Complete Dentures Using Digital, Hybrid, and Conventional Workflows: A Systematic Review. J. Prosthet. Dent. 2024. [Google Scholar] [CrossRef]
- Jurado, C.A.; Tsujimoto, A.; Alhotan, A.; Villalobos-Tinoco, J.; AlShabib, A. Digitally Fabricated Immediate Complete Dentures: Case Reports of Milled and Printed Dentures. Int. J. Prosthodont. 2020, 33, 232–241. [Google Scholar] [CrossRef]
- Jafarpour, D.; Haricharan, P.B.; de Souza, R.F. CAD/CAM versus Traditional Complete Dentures: A Systematic Review and Meta-Analysis of Patient- and Clinician-Reported Outcomes and Costs. J. Oral Rehabil. 2024, 51, 1911–1924. [Google Scholar] [CrossRef] [PubMed]
- Lo Russo, L.; Guida, L.; Ronsivalle, V.; Ercoli, C. Digital Denture with Mucostatic Base and Functional Borders: A Cast-Free Digital Technique. J. Prosthodont. 2024. [Google Scholar] [CrossRef]
- Steinmassl, O.; Dumfahrt, H.; Grunert, I.; Steinmassl, P.A. CAD/CAM Produces Dentures with Improved Fit. Clin. Oral Investig. 2018, 22, 2829–2835. [Google Scholar] [CrossRef] [PubMed]
- Lo Russo, L.; Salamini, A. Removable Complete Digital Dentures: A Workflow That Integrates Open Technologies. J. Prosthet. Dent. 2018, 119, 727–732. [Google Scholar] [CrossRef]
- Lo Russo, L.; Salamini, A.; Troiano, G.; Guida, L. Digital Dentures: A Protocol Based on Intraoral Scans. J. Prosthet. Dent. 2021, 125, 597–602. [Google Scholar] [CrossRef]
- Taji, T.; Yoshida, M.; Hiasa, K.; Abe, Y.; Tsuga, K.; Akagawa, Y. Influence of Mental Status on Removable Prosthesis Compliance in Institutionalized Elderly Persons. Int. J. Prosthodont. 2005, 18, 146–149. [Google Scholar]
- Luraschi, J.; Korgaonkar, M.S.; Whittle, T.; Schimmel, M.; Müller, F.; Klineberg, I. Neuroplasticity in the Adaptation to Prosthodontic Treatment. J. Orofac. Pain. 2013, 27, 206–216. [Google Scholar] [CrossRef]
- Müller, F.; Heath, M.R.; Ferman, A.M.; Davis, G.R. Modulation of Mastication during Experimental Loosening of Complete Dentures. Int. J. Prosthodont. 2002, 15, 553–558. [Google Scholar] [PubMed]
- Inamochi, Y.; Fueki, K.; Usui, N.; Taira, M.; Wakabayashi, N. Adaptive Change in Chewing-Related Brain Activity While Wearing a Palatal Plate: An Functional Magnetic Resonance Imaging Study. J. Oral Rehabil. 2017, 44, 770–778. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, A.; Singh, S.V.; Aggarwal, H.; Gupta, A. Effect of Mucostatic and Selective Pressure Impression Techniques on Residual Ridge Resorption in Individuals with Different Bone Mineral Densities: A Prospective Clinical Pilot Study. J. Prosthet. Dent. 2019, 121, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Tallgren, A. The Continuing Reduction of the Residual Alveolar Ridges in Complete Denture Wearers: A Mixed-Longitudinal Study Covering 25 Years. J. Prosthet. Dent. 1972, 27, 120–132. [Google Scholar] [CrossRef]
- Bindhoo, Y.A.; Thirumurthy, V.R.; Kurien, A. Complete Mucostatic Impression: A New Attempt. J. Prosthodont. 2012, 21, 209–214. [Google Scholar] [CrossRef]
- Lo Russo, L.; Lo Muzio, E.; Troiano, G.; Salamini, A.; Zhurakivska, K.; Guida, L. Accuracy of Trial Complete Dentures Fabricated by Using Fused Deposition Modeling 3-Dimensional Printing: An in Vitro Study. J. Prosthet. Dent. 2023, 129, 908–912. [Google Scholar] [CrossRef]
- Lo Russo, L.; Troiano, G.; Santarelli, A.; Salamini, A.; Gallo, C.; Guida, L. Trueness of Intaglio Surface of Milled Digital Dentures Designed from Intraoral Scans. J. Prosthodont. 2022, 31, 210–214. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Leung, W.K. Functional Neuroplasticity of Adults with Partial or Complete Denture Rehabilitation with or without Implants: Evidence from FMRI Studies. Nutrients 2023, 15, 1577. [Google Scholar] [CrossRef]
- Chebib, N.; Imamura, Y.; El Osta, N.; Srinivasan, M.; Müller, F.; Maniewicz, S. Fit and Retention of Complete Denture Bases: Part II—Conventional Impressions versus Digital Scans: A Clinical Controlled Crossover Study. J. Prosthet. Dent. 2024, 131, 618–625. [Google Scholar] [CrossRef]
- Jayaraman, S.; Singh, B.P.; Ramanathan, B.; Pazhaniappan Pillai, M.; MacDonald, L.; Kirubakaran, R. Final-Impression Techniques and Materials for Making Complete and Removable Partial Dentures. Cochrane Database Syst. Rev. 2018, 4, CD012256. [Google Scholar] [CrossRef]
- Pasam, N.; Hallikerimath, R.B.; Arora, A.; Gilra, S. Effect of Different Curing Temperatures on the Distortion at the Posterior Peripheral Seal: An in Vitro Study. Indian. J. Dent. Res. 2012, 23, 301–304. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, A.; Lindquist, T.; Schneider, R.; Williamson, D.; Boyer, D.; Dawson, D.V. Comparison of the Dimensional Accuracy of Injection-Molded Denture Base Materials to That of Conventional Pressure-Pack Acrylic Resin. J. Prosthodont. 2004, 13, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Ghani, F.; Kikuchi, M.; Lynch, C.D.; Watanabe, M. Effect of Some Curing Methods on Acrylic Maxillary Denture Base Fit. Eur. J. Prosthodont. Restor. Dent. 2010, 18, 132–138. [Google Scholar] [PubMed]
- Lo Russo, L.; Caradonna, G.; Troiano, G.; Salamini, A.; Guida, L.; Ciavarella, D. Three-Dimensional Differences between Intraoral Scans and Conventional Impressions of Edentulous Jaws: A Clinical Study. J. Prosthet. Dent. 2020, 123, 264–268. [Google Scholar] [CrossRef]
- Masri, G.; Mortada, R.; Ounsi, H.; Alharbi, N.; Boulos, P.; Salameh, Z. Adaptation of Complete Denture Base Fabricated by Conventional, Milling, and 3-D Printing Techniques: An In Vitro Study. J. Contemp. Dent. Pract. 2020, 21, 367–371. [Google Scholar]
- Lefrançois, E.; Delanoue, V.; Morice, S.; Ravalec, X.; Desclos-Theveniau, M. A Digital Approach for a Complete Rehabilitation with Fixed and Removable Prostheses: A Technical Procedure. Dent. J. 2024, 13, 7. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).