Abstract
T-cell acute lymphoblastic leukemia (T-ALL) is an aggressive hematologic malignancy, typically presenting with systemic symptoms and mediastinal involvement. Leukemia cutis (LC) and renal infiltration are rare, especially at disease onset. A 27-year-old man presented with a solitary scalp lesion without systemic symptoms or hematologic abnormalities. Histopathology revealed a blastoid lymphoid infiltrate with a T-ALL immunophenotype. Two weeks later, laboratory tests showed leukocytosis, lymphocytosis, and renal dysfunction. Imaging revealed a large mediastinal mass, scalp soft tissue involvement, and bilateral renal infiltration. Bone marrow biopsy confirmed T-ALL with a mature phenotype. FISH identified TRAD:NKX2 rearrangement and CDKN2AB deletion. The patient received three cycles of pediatric-inspired chemotherapy, achieving complete molecular remission and resolution of extramedullary disease. He subsequently underwent allogeneic hematopoietic stem cell transplantation (HSCT) from an HLA-matched sibling. Post-transplant complications included febrile neutropenia and mucositis. On day +100, he remained in minimal residual disease (MRD)-negative remission. This case illustrates a rare presentation of T-ALL with isolated skin involvement and renal infiltration at diagnosis, highlighting the importance of early biopsy and immunophenotyping of atypical skin lesions. Intensive chemotherapy followed by HSCT represents a viable strategy for young adults with high-risk T-ALL and extramedullary disease.
1. Introduction
Acute lymphoblastic leukemia (ALL) is a rare and aggressive hematologic malignancy characterized by the malignant proliferation of lymphoid cells arrested at an early stage of differentiation, capable of invading the bone marrow, blood, and extramedullary sites [1]. ALL affects individuals across the lifespan, from neonates to the very elderly, with peak incidence in children aged two to five years. Acquired or somatic mutations of some genes may contribute to the clonal transformation of precursor blood cells. Advances in next-generation sequencing have enhanced our understanding of the genetic alterations underlying lymphoblastic leukemia and their association with the disease prognosis [2,3]. The most commonly reported symptoms include fatigue, fever, weight loss, and hemorrhagic manifestations, all consequences of bone marrow failure due to leukemic cell proliferation. Nausea and headaches are less common (5–10% at diagnosis), resulting from the involvement of the central nervous system. Even rarer are localizations in the bones and joints, skin, kidneys, and lungs. Of particular interest, cutaneous involvement in ALL—leukemia cutis (LC)—is a rare but clinically significant finding. LC represents the infiltration of neoplastic lymphoid cells into the skin and may manifest with solitary or multiple papules, nodules, or plaques of variable size and color, often red or violaceous. In most cases, LC occurs in advanced stages of the disease, but in rare instances, it may precede systemic involvement or serve as the initial presentation, as in aleukemic leukemia cutis. All subtypes of leukemia may infiltrate the skin, and several studies in the literature have reported LC [3]. Clinical suspicion should be raised by new-onset skin lesions in patients with established or suspected leukemia, and a skin biopsy is mandatory for diagnosis, allowing immunohistochemical confirmation and distinction from other dermatological or hematologic disorders. The highest incidence of LC is observed in acute myeloid leukemia (AML), chronic myelomonocytic leukemia (cMML), and T-ALL, with poor prognosis [3]. Similarly, kidney infiltration by ALL is an exceptionally rare event, with most cases reported in children or young adults [4,5,6]. Here, we report an unusual case of ALL that initially presented only with skin involvement, underscoring the importance of recognizing cutaneous manifestations as a potential first sign of underlying hematologic malignancy.
2. Case Presentation
A 27-year-old man presented with a progressively enlarging scalp swelling (Figure 1 and Figure 2) persisting for a month in the absence of other symptoms.
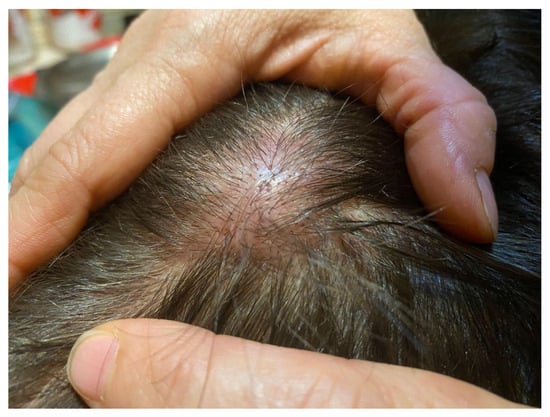
Figure 1.
Cutaneous lesions on the scalp were observed in the patient for approximately two months prior to diagnosis. Skin biopsy was performed on these lesions and subsequently led to the diagnosis.

Figure 2.
Cutaneous lesions on the scalp.
Two weeks prior, on the advice of his general practitioner, he underwent a dermatological evaluation and scalp biopsy accompanied by blood tests, including complete blood count and biochemistry. While the latter were unremarkable, histological examination of the scalp revealed infiltration by a lymphoproliferative disorder with a blastoid phenotype, characterized as TdT+, CD34-, CD1a-, LMO2-, CD10+, CD3+, CD7+, CD5+, CD8+, CD4-, TIA1-, granzyme B-, CD79a+/- (weak), CD20-, PAX5-, CD56-, and CD123-, with a high proliferative index (Ki67 >98%). Therefore, the patient was admitted to the emergency department and, two weeks after the biopsy, laboratory tests revealed leukocytosis with lymphocytosis, hyperuricemia, and renal dysfunction (hemoglobin 14.9 g/dL, MCV 90.7 fl, white blood cells 56.300/mmc, neutrophils 14.970/mmc, lymphocytes 37.400/mmc, platelets 133.000/mmc, creatinine 1.61 mg/dL, lactic dehydrogenase 1309 U/L, uric acid 13 mg/dL). Peripheral blood smear examination showed 52% atypical cells with variable size with a high nucleus/cytoplasm ratio, round nuclei with occasional indentations, some nucleoli, and fine-to-coarse chromatin, consistent with blasts. The chest X-ray showed the presence of massive mediastinal mass. The day after the patient’s admission to our hematology unit, his bone marrow aspiration showed 83% of the blasts with a T phenotype expressing TDT-, cyCD1a-, CD99+, CD34-, cyCD3+, sCD3-, CD7+, CD2+, CD5+, CD8+, CD10+, TCRgd-, TCRab-, HLA-DR+, confirming T-ALL. Bone marrow biopsy demonstrated hypercellular marrow (>95%) with diffuse acute lymphoblastic leukemia infiltration by TdT+ CD99+, CD3+, CD7+, CD4-, CD10+, LMO2-, CD79a+/-, weak, CD20-, PAX5-, CD34-, CD117-, and MPO- blast cells (Figure 3).
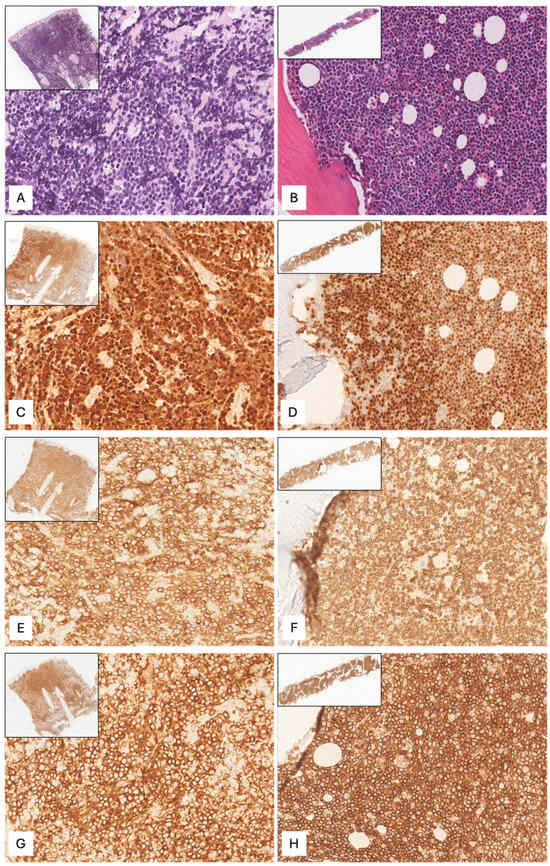
Figure 3.
Cutaneous ((A), hematoxylin–eosin (H&E), original magnification (o.m.) x300, upper insert o.m.x23) and bone marrow biopsy ((B), H&E, o.m.x200, upper insert o.m.x10) showing diffuse infiltration by medium-sized cells with scant cytoplasm and round nuclei with condensed chromatin and indistinct nucleoli. The neoplastic cells were positive for TdT ((C), o.m.x300, upper insert o.m.x23) ((D), o.m.x200, upper insert o.m.x10), CD3 ((E), o.m.x300, upper insert o.m.x23) ((F), o.m.x200, upper insert o.m.x10), and CD8 ((G), o.m.x300, upper insert o.m.x23) ((H), o.m.x200, upper insert o.m.x10).
A diagnosis of acute lymphoblastic T-cell leukemia with a mature phenotype and skin localization was therefore made. Fluorescence in situ hybridization (FISH) analysis revealed TRAD:NKX2 rearrangement and LEF1/4q21 and CDKN2AB/9p21 deletions in about 25% of the cells analyzed. CT confirmed a voluminous mediastinal disease (13 × 9 × 10 cm) with inhomogeneous post-contrast enhancement of the subcutaneous soft tissues in the left parietal frontalis and right occipital sites and also showed kidney infiltration. Brain MRI was negative. The patient underwent three cycles of intensive chemotherapy. Two diagnostic and prophylactic lumbar punctures with cytarabine and methotrexate were performed at the beginning of the first and second cycles. The first cycle included cyclophosphamide, idarubicin, vincristine, and Peg-asparaginase. The second cycle included cyclophosphamide, idarubicin, cytarabine, and Peg-asparaginase. The third cycle included high-dose methotrexate and cytarabine. At the end of first cycle, bone marrow aspiration and flow cytometry for minimal residual disease (MRD) demonstrated the absence of blastic elements. FISH analyses no longer detected the presence of the genetic rearrangement highlighted at onset. The patient maintained molecular remission until the end of the third cycle. CT scan performed at the end of first and third cycle, revealed significant mediastinal mass reduction and resolution of renal disease. 18F-fluorodeoxyglucose positron emission tomography and CT scan (FDG-PET/TC), at the end of induction, confirmed the absence of hypermetabolic disease.
Upon achieving complete remission, as a high-risk T-ALL, the patient received pre-transplant conditioning chemotherapy (including fludarabine, busulfan, and thiotepa), followed by allogeneic hematopoietic stem cell transplantation (HSCT) from an HLA-matched sibling donor (younger sister). Post-transplant-graft-versus-host disease (GvHD) prophylaxis consisted of methotrexate on post-transplant days 1, 3, 6, and 11, and cyclosporine A. The post-transplant course was complicated by febrile neutropenia, managed with vancomycin and piperacillin–tazobactam, later switched to meropenem due to persistent fever, and grade 3 mucositis treated with analgesics. Bone marrow aspiration on day +15 demonstrated trilinear hematopoietic recovery. On day +100, the patient was in good clinical condition and in MRD (FISH and cytofluorimetric) remission.
3. Discussion
T-cell ALL accounts for 15% of all lymphoblastic leukemia in pediatric patients and 25% in adult patients. Historically, the prognosis for T-cell ALL has been worse than that for B-cell ALL; however, thanks to new therapeutic approaches, outcomes for T-cell ALL have improved significantly and are now approaching those seen in B-cell disease, although relapse rates for these patients are 30% during therapy or within two years [7,8].
Common presentations include nonspecific symptoms such as fatigue, fever, and bleeding. Mediastinal masses and extramedullary involvement in the liver, lymph nodes, spleen, and testes are frequently observed.
The involvement of the skin as the first clinical manifestation, in the absence of additional symptoms or signs, is extremely rare. Only a few cases of acute lymphoblastic leukemia with skin involvement are reported in the literature, mostly concerning children or young adults. It typically occurs after the diagnosis of leukemia and is usually associated with other lymphadenopathies or mediastinal involvement, as reported in the few cases described in the literature. The cases described often involved skin associated with lymphadenopathy and/or systemic symptoms. Table 1 reports cases described in the literature on T- and B-lymphoblastic leukemias and/or lymphoma with skin involvement, either at onset or relapse (n = 16), and renal involvement (n = 3) (Table 1; [4,5,6,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24]).

Table 1.
Reported cases of T- and B-lymphoblastic leukemia and lymphoma with skin and renal involvement.
Additionally, two case reports provide reviews of 12 and 31 cases of pre-B-ALL and B-LBL, respectively. Among the 16 cases with skin involvement, 10 presented with cutaneous manifestations either at disease onset or even as the initial sign preceding the diagnosis. Of these cases, ten were B-ALL/LBL and six were T-ALL. In the latter group, the median age at diagnosis was 14 years (range 6 months–50 years), and four out of six cases presented skin localization on the face or scalp. All cases reported with renal involvement were T-ALL, including one relapse, with a median age of 10 years (range 18 months–43 years).
The cases differed in their therapeutic protocols. Three cases achieved complete remission (CR), including one case of T-ALL with renal involvement, one case of B-LBL, and one case of T-ALL with skin involvement, who was treated with chemotherapy and allogenic transplantation. Two cases relapsed, and two resulted in fatal outcomes. The uniqueness of the present case lies in its isolated skin manifestation without hematologic abnormalities at onset. Additionally, the patient’s renal involvement is an unusual feature, suggesting a marked extramedullary tropism of the disease.
Considering genetic findings, the NKX2 rearrangement was first described by Homminga et al. [25] in 2011 and is associated with NKX2-1 dysregulation [25]. In particular, 117 cases of pediatric ALL were studied, and four clusters of cytogenetic and molecular alterations were distinguished. One of these clusters, called “proliferative”, has been most prominently highlighted in the pediatric population and was characterized by the rearrangement of the NKX2-1 gene. This cluster was also associated with the cortical arrest of thymocytes and CD1 expression, and it is extremely rare (<5%) [26].
Unlike the cases described by Homminga et al. [25], which reported T-ALL with NKX2 rearrangement associated with strong CD1a expression, our case presents a CD1a-negative immunophenotype despite harboring the TRAD:NKX2 rearrangement. This finding emphasizes the biological and immunophenotypic heterogeneity of NKX2-rearranged T-ALL, suggesting that not all cases within this molecular cluster exhibit the cortical phenotype typically marked by CD1a positivity. The absence of CD1a in our patient expands the immunophenotypic spectrum of NKX2-rearranged T-ALL and highlights the importance of thorough immunophenotypic characterization in clinical practice, as outcomes and therapeutic implications may differ from those described in previous literature.
Several studies in the literature have shown an association between intensive chemotherapy and improved outcome in patients with T-ALL. The adolescent and young adult (AYA) patient population may represent a unique age-based subgroup, distinct from children and older adults, that is underrepresented in the literature. It is variably defined in different studies as an age range between 15 and 18 years and between 25 and 39 years. Many studies in the literature involving young patients with ALL have aimed at evaluating the use of a pediatric treatment approach [27,28]. They have shown to achieve higher complete response rates and improved overall survival (OS) without excessive toxicity, even if they have worse prognosis than children [29]. The correct approach to the management of AYA ALL includes risk stratification (genetics and MRD) and the use of an institutional/national pediatric-based protocol containing Peg-ASP [30].
However, the overall 5-year survival in these patients is 5%, and outcomes in patients who relapse are very poor. Allogeneic SCT is recommended for adult patients in second or later complete remission, but also in first CR in those with high-risk features [31,32,33]. Due to the presence of the rearrangement identified by FISH and extramedullary involvement, we strongly considered the patient eligible for allogeneic SCT. At the end of the first chemotherapy cycle, our patient had a complete resolution of the skin and renal involvement, which no longer detectable on total-body CT scan, as well as complete medullary remission. The patient also maintained complete response even at the end of the third cycle before starting allogeneic transplantation.
4. Conclusions
T-ALL with skin and kidney infiltration is exceptionally rare, particularly in the absence of systemic symptoms or hematologic abnormalities. The use of complementary laboratory investigations such as immunophenotyping, cytogenetics, and FISH analysis is crucial not only for risk stratification but also for MRD monitoring and treatment planning [34]. Despite the poor prognosis associated with extramedullary disease, intensive chemotherapy protocols including Peg-asparaginase, followed by allogeneic SCT as soon as possible, remains a viable therapeutic opportunity for this class of patients.
Author Contributions
V.D.S. conceptualized and wrote the manuscript; S.M., G.P., M.P., A.D.N., G.M., E.C., C.T., V.D.S., F.L.L., E.R. and S.P. researched the data; V.D.S. and S.M. edited the manuscript; S.M. and A.T. reviewed the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Territorial Ethics Committee Lazio Area 1 (Protocol No. 937/2025 dated 9 October 2025).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study and written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
Due to patient privacy, all data pertaining to the patient in this case report cannot be shared or distributed.
Acknowledgments
The authors would like to thank all those who contributed to the treatment of the patient. We would also like to thank the patient for giving us consent to write this case report.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Malard, F.; Mohty, M. Acute lymphoblastic leukaemia. Lancet 2020, 395, 1146–1162. [Google Scholar] [CrossRef]
- Inaba, H.; Greaves, M.; Mullighan, C.G. Acute lymphoblastic leukaemia. Lancet 2013, 381, 1943–1955. [Google Scholar] [CrossRef] [PubMed]
- Robak, E.; Braun, M.; Robak, T. Leukemia Cutis-The Current View on Pathogenesis, Diagnosis, and Treatment. Cancers 2023, 15, 5393. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vijayasekharan, K.; Bhat, K.V.; Venkatagiri, A.M.; Godkhindi, V.M.; Laxminarayana, S.L.K.; Belurkar, S. Bilateral massive nephromegaly—A rare presentation of t-cell acute lymphoblastic leukemia. Leuk. Res. Rep. 2021, 15, 100246, Erratum in: Leuk. Res. Rep. 2022, 17, 100307. https://doi.org/10.1016/j.lrr.2022.100307. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bednarkiewicz, J.; Grzejszczak, P.; Szmigielska-Kapłon, A.; Stefańczyk, L.; Wągrowska-Danilewicz, M.; Kurnatowska, I. Acute kidney injury in a patient with T-cell acute lymphoblastic leukemia. Pol. Arch. Intern. Med. 2023, 133, 16346. [Google Scholar] [CrossRef] [PubMed]
- Asdahl, P.H.; Warner, L.F.; Bendix, K.; Hasle, H. Acute renal failure and normal blood count: A rare presentation of T-cell acute lymphoblastic leukemia. Leuk. Res. Rep. 2013, 3, 14–16. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vadillo, E.; Dorantes-Acosta, E.; Pelayo, R.; Schnoor, M. T-cell acute lymphoblastic leukemia (T-ALL): New insights into the cellular origins and infiltration mechanisms common and unique among hematologic malignancies. Blood Rev. 2018, 32, 36–51. [Google Scholar] [CrossRef]
- Raetz, E.A.; Teachey, D.T. T-cell acute lymphoblastic leukemia. Hematol. Am. Soc. Hematol. Educ. Program. 2016, 2016, 580–588. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Konik, A.; Dührsen, U.; Röth, A. Nodular lesions of the scalp and a mediastinal mass in T cell acute lymphoblastic leukemia. Int. J. Hematol. 2010, 92, 3–4. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kanoje, P.K.; Khullar, G.; Yadav, A.K.; Saxena, A.K.; Gupta, D.K. Generalized leukemia cutis as the initial manifestation of precursor B-cell acute lymphoblastic leukemia in a young male. Dermatol. Ther. 2021, 34, e14594. [Google Scholar] [CrossRef] [PubMed]
- Arora, P.; Sinha, N.; Malhotra, P.; Kumar, V.; Shastri, A.; Yadav, K. T-cell acute lymphoblastic leukemia with a rare chromosomal translocation presenting as leukemia cutis. Int. J. Dermatol. 2022, 61, e120–e123. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Wang, T. Leukemia cutis in T-cell acute lymphoblastic leukemia: A 3-year follow-up case report. Ann. Palliat. Med. 2023, 12, 200–204. [Google Scholar] [CrossRef]
- Taljanovic, M.S.; Hulett, R.L.; Graham, A.R.; Graham, M.L.; Hunter, T.B. Acute lymphoblastic leukemia of the skin and subcutaneous tissues; the first manifestation of disease in a 6-month-old infant: A case report with literature review. Emerg. Radiol. 2004, 11, 60–64. [Google Scholar] [CrossRef] [PubMed]
- Tsetnov, I.; Haiduk, I.; Lyapichev, K.A. CD3/cd20/CD45 negative leukemia cutis. J. Hematop. 2025, 18, 4, Erratum in: J. Hematop. 2025, 18, 5. https://doi.org/10.1007/s12308-025-00622-0. [Google Scholar] [CrossRef] [PubMed]
- Kaur, D.; Arneja, J.S.; Senger, C.; Chipperfield, K.; Lam, J.; Cheng, S. Cutaneous precursor T-lymphoclastic lymphoma in a child. Pediatr. Blood Cancer 2002, 69, e29635. [Google Scholar] [CrossRef] [PubMed]
- Montes-Torres, A.; Llamas-Velasco, M.; Capusan, T.M.; Aguado, B.; Adrados, M. Cutaneous involvement as the first manifestation of T- lymphoblastic lymphoma and review of the literature. J. Cutan. Pathol. 2019, 46, 372–375. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.Y.; Liu, M.; Ruth, J.S.; Potensiani, S.; Hsu, S. precursor-Bcell-ALL cutis resembling lipomas: An atypical presentation of a rare entity and review of the literature. Dermatol. Online J. 2017, 15, 23. [Google Scholar] [PubMed]
- Najem, N.; Zadeh, V.B.; Badawi, M.; Kumar, R.; Al-Otaibi, S.; Al-Abdulrazzaq, A. Aleukemic leukemia cutis in a child preceding T-call acute lymphoblastic leukemia. Pediatr. Dermatol. 2011, 28, 535–537. [Google Scholar] [CrossRef] [PubMed]
- Song, H.; Todd, P.; Chiarle, R.; Billett, A.L.; Gellis, S. Primary Cutaneous B-Cell Lymphoblatic Lymphoma Arising from a Long-Standing Lesion in a Child and Review of the literature. Pediatr. Dermatol. 2017, 34, e182–e186. [Google Scholar] [CrossRef] [PubMed]
- Kawamaki, T.; kimura, S.; Kinoshita, A.; Kondo, K.; Soma, Y. Precursor-cell lymphoblastic lymphoma with only cutaneous involvement. Acta Derm. Venereol. 2009, 89, 540–541. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, S.; Prabhu, S.; Prabhu, M.; Parampalli Srinivas, S.; Kudva, R.; Belurkar, S. Leukemia cutis unveiling underlying pre-B-cell acute lymphoblastic leukemia. Australas. J. Dermatol. 2020, 61, e111–e113. [Google Scholar] [CrossRef] [PubMed]
- Jouini, R.; Chabchoub, I.; Khanchel, F.; Helal, I.; Badri, T.; Ben Brahim, E.; Hammami, H.; chadli-Debbiche, A. Primary and isolated cutaneous precursor B-lymphoblastic lymphoma in an infant. Pediatr. Dermatol. 2021, 38, 707–708. [Google Scholar] [CrossRef] [PubMed]
- Kemps, P.G.; Cleven, A.H.G.; van Wezel, T.; van Eijk, R.; Bot, F.J.; Veelken, H.; van Balen, P.; Kerkhoffs, J.H. B-cell lymphoblastic lymphoma with cutaneous involvement and a KMT2A gene rearrangement. Am. J. Hematol. 2020, 95, 1427–1429. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bandyopadhyay, R.; Bandyopadhyay, S.K.; Dhua, D.; Roy, S. Primary cutaneous precursor B-cell lymphoblastic lymphoma with late dissemination. Singap. Med. J. 2011, 52, e258–e261. [Google Scholar] [PubMed]
- Homminga, I.; Pieters, R.; Langerak, A.W.; de Rooi, J.J.; Stubbs, A.; Verstegen, M.; Vuerhard, M.; Buijs-Gladdines, J.; Kooi, C.; Klous, P.; et al. Integrated transcript and genome analyses reveal NKX2-1 and MEF2C as potential oncogenes in T cell acute lymphoblastic leukemia. Cancer Cell 2011, 19, 484–497. [Google Scholar] [CrossRef] [PubMed]
- Duffield, A.S.; Mullighan, C.G.; Borowitz, M.J. International Consensus Classification of acute lymphoblastic leukemia/lymphoma. Virchows Arch. 2023, 482, 11–26. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rijneveld, A.W.; van der Holt, B.; Daenen, S.M.; Biemond, B.J.; de Weerdt, O.; Muus, P.; Maertens, J.; Mattijssen, V.; Demuynck, H.; Legdeur, M.C.; et al. Intensified chemotherapy inspired by a pediatric regimen combined with allogeneic transplantation in adult patients with acute lymphoblastic leukemia up to the age of 40. Leukemia 2011, 25, 1697–1703. [Google Scholar] [CrossRef] [PubMed]
- Muffly, L.; Alvarez, E.; Lichtensztajn, D.; Abrahão, R.; Gomez, S.L.; Keegan, T. Patterns of care and outcomes in adolescent and young adult acute lymphoblastic leukemia: A population-based study. Blood Adv. 2018, 2, 895–903. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, J.W. Optimal therapy for adolescents and young adults with acute lymphoblastic leukemia-current perspectives. Blood Res. 2020, 55, S27–S31. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Curran, E.; Stock, W. How I treat acute lymphoblastic leukemia in older adolescents and young adults. Blood J. Am. Soc. Hematol. 2015, 125, 3702–3710. [Google Scholar] [CrossRef] [PubMed]
- Bakr, M.; Rasheed, W.; Mohamed, S.Y.; Al-Mohareb, F.; Chaudhri, N.; Al-Sharif, F.; Al-Zahrani, H.; Al-Dawsari, G.; Saleh, A.J.; Nassar, A.; et al. Allogeneic hematopoietic stem cell transplantation in adolescent and adult patients with high-risk T cell acute lymphoblastic leukemia. Biol. Blood Marrow Transplant. 2012, 18, 1897–1904. [Google Scholar] [CrossRef] [PubMed]
- Hahn, T.; Wall, D.; Camitta, B.; Davies, S.; Dillon, H.; Gaynon, P.; Larson, R.A.; Parsons, S.; Seidenfeld, J.; Weisdorf, D.; et al. The role of cytotoxic therapy with hematopoietic stem cell transplantation in the therapy of acute lymphoblastic leukemia in adults: An evidence-based review. Biol. Blood Marrow Transplant. 2006, 12, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Rowe, J.M.; Buck, G.; Burnett, A.K.; Chopra, R.; Wiernik, P.H.; Richards, S.M.; Lazarus, H.M.; Franklin, I.M.; Litzow, M.R.; Ciobanu, N.; et al. Induction therapy for adults with acute lymphoblastic leukemia: Results of more than 1500 patients from the international ALL trial: MRC UKALL XII/ECOG E2993. Blood 2005, 106, 3760–3767. [Google Scholar] [CrossRef] [PubMed]
- La Starza, R.; Pierini, V.; Pierini, T.; Nofrini, V.; Matteucci, C.; Arniani, S.; Moretti, M.; Lema Fernandez, A.G.; Pellanera, F.; Di Giacomo, D.; et al. Design of a Comprehensive Fluorescence in Situ Hybridization Assay for Genetic Classification of T-Cell Acute Lymphoblastic Leukemia. J. Mol. Diagn. 2020, 22, 629–639. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).