Abstract
Background/Objectives: Family caregivers of individuals with dementia frequently experience substantial psychological distress, yet their emotional responses are heterogeneous. Depression, anxiety and psychological well-being may co-occur in distinct patterns, and socio-economic resources such as education and income are often hypothesized to buffer caregiver distress. This study aimed to identify latent psychological profiles among dementia caregivers and to examine whether education and income moderate the association between affective symptoms and well-being. Methods: A cross-sectional study was conducted with 73 family caregivers of dementia patients attending the Neurology–Psychiatry Department of C.F.2 Clinical Hospital, Bucharest (November 2023–April 2024). Participants completed the PHQ-9 (depression), the COVI Anxiety Scale and Ryff’s Psychological Well-Being Scales. Care recipients’ cognitive status was extracted from medical records using the MMSE. Gaussian Mixture Modeling was used for latent profile analysis (LPA). Between-profile differences were examined using one-way ANOVAs and Tukey post-hoc tests and Pearson correlations were used to assess associations between affective symptoms and psychological well-being, and examined whether education and income were associated with profile membership and psychological well-being. Results: LPA supported a three-profile solution: (1) lower depressive symptoms with moderate anxiety (33%), (2) severe combined depression and anxiety (18%) and (3) moderately severe depression with severe anxiety (49%). Profiles differed significantly in depressive symptom severity, whereas anxiety severity did not differ significantly across profiles. Caregivers in Profile 3 (moderately severe depression–severe anxiety) reported significantly higher overall psychological well-being than those in Profile 1 (moderate depression–moderate anxiety). In contrast, caregivers in Profile 2 (severe depression–severe anxiety), who exhibited the highest affective symptom burden, showed intermediate levels of overall well-being, with comparatively lower scores on specific dimensions such as purpose in life. Depressive symptoms were weakly but significantly associated with autonomy and self-acceptance, whereas anxiety symptoms showed no significant associations with psychological well-being. Education level and household income were not significantly associated with profile membership or psychological well-being. Conclusions: Family caregivers of individuals with dementia can be meaningfully described as forming three exploratory psychological profiles characterized by different configurations of depressive and anxiety symptoms. These findings indicate that caregiver distress does not follow a simple severity gradient and that psychological well-being is not solely determined by symptom burden. Socio-economic characteristics did not account for differences in caregiver adjustment, underscoring the importance of individualized psychological assessment and tailored interventions to support caregiver mental health.
1. Introduction
The global demographic shift toward population aging has profound implications for public health. One of the most pressing concerns is the growing prevalence of dementia and the associated psychological burden experienced by both patients and caregivers. Depression and anxiety are projected to increase alongside the demographic transition, with dementia representing a major driver of disability and dependency in later life. In 2019, it was estimated that the number of people living with dementia could reach 152.8 million by 2050, primarily due to increased life expectancy and demographic aging. More recent studies, however, have challenged these projections, noting potential underestimation of prevalence in minority populations such as Black and Hispanic groups [1,2], while others argue that lifestyle interventions may contribute to a decline in incidence over time [3,4]. According to the World Health Organization (WHO), approximately 57 million people were living with dementia in 2021, with 10 million new cases diagnosed each year, reflecting a constantly rising global burden [5].
Dementia prevalence increases exponentially with age, doubling every five years after age 65 [6]. The condition is particularly prevalent in aging societies such as Japan, Italy and Germany [7], with Alzheimer’s disease ranked as the most common neurodegenerative disorder worldwide, followed by Parkinson’s disease [6,8,9]. Between 2021 and 2023, WHO reports identified Alzheimer’s disease and other dementias among the top three causes of death in Great Britain [10]. Pathophysiologically, dementia involves progressive neuronal degeneration, hippocampal and cortical atrophy, synaptic loss and the accumulation of neurotoxic proteins including amyloid-β plaques and tau neurofibrillary tangles [11,12,13,14]. These changes lead to cognitive decline, behavioral alterations and loss of independence, making dementia the leading cause of disability and death among neurological conditions [15].
Dementia caregiving entails profound emotional, physical and social challenges. A large European survey in 2006 reported that one-third of caregivers provided more than 10 h of daily care, regardless of dementia severity [16]. More recently, a study of over 1400 caregivers across five European countries revealed that nearly 20% received no information at diagnosis, 58% expressed persistent worry about the future, 34% reported depressive symptoms and many described loneliness as a major consequence of their role [17].
Consistently, caregivers of individuals with dementia experience greater psychological distress than caregivers of other chronic conditions [18,19]. A meta-analysis demonstrated that dementia family caregivers are significantly more stressed and report more depressive symptoms and physical problems compared to other caregivers [20]. Risk factors for heightened distress include demographic variables (female gender, older age, spouse or child relationship to the care recipient), lower socioeconomic status and limited social support [21,22,23,24]. The severity of the care recipient’s cognitive impairment, often measured by the Mini-Mental State Examination (MMSE), has also been shown to correlate directly with caregiver burden [25].
Beyond distress, research has increasingly focused on the psychological well-being of caregivers, assessed across multiple domains such as autonomy, self-acceptance, personal growth and purpose in life using Ryff’s Psychological Well-Being Scale [26,27,28]. Evidence suggests that well-being often declines as caregiving responsibilities intensify. For example, Wister et al. (2022) found that caregivers with lower well-being scores were more likely to develop depressive and anxiety symptoms, highlighting the importance of multidimensional assessments [29]. Coping strategies are equally critical; caregivers who adopt adaptive strategies such as seeking social support or maintaining personal control exhibit better mental health outcomes, whereas reliance on maladaptive coping predicts poorer outcomes [30,31].
Depression and anxiety are the two most prevalent mental health concerns among caregivers. According to Pinquart and Sörensen (2007), caregivers consistently report higher levels of depression than non-caregivers, with the gap being most pronounced among those caring for dementia patients [32]. Depression in caregivers is exacerbated by lack of social support, physical exhaustion and isolation [33], while anxiety often stems from uncertainty about the future, financial strain and the overwhelming nature of caregiving responsibilities.
Existing research demonstrates that dementia caregiving is associated with profound psychological challenges, but also that individual, relational and socio-economic resources can shape outcomes. However, most studies treat caregivers as a homogeneous group, overlooking the possibility of latent subgroups that differ in their levels of depression, anxiety and well-being. Identifying such profiles is essential for developing tailored interventions. Moreover, socio-economic resources such as education and income may function as resilience factors that buffer against psychological burden, though evidence remains limited.
However, despite substantial variability in caregiver experiences, few studies have empirically tested whether distinct subgroups (profiles) of caregivers can be identified based on co-occurring depressive and anxiety symptoms. Moreover, prior work rarely integrates psychological well-being into such subgroup analyses, and virtually no studies have examined whether socioeconomic factors moderate these associations. Addressing these gaps requires analytic approaches capable of detecting latent heterogeneity, such as Latent Profile Analysis (LPA), while also acknowledging that the number of identifiable profiles is constrained by sample size and may be limited to a small number of broad caregiver groups.
In this context, the present study proposes three exploratory hypotheses: (H1) caregivers will cluster into a small number of latent psychological profiles defined by different combinations of depression and anxiety; (H2) these profiles will show meaningful differences in psychological well-being; and (H3) higher education and income were explored as potential moderators of the relationship between affective symptoms and psychological well-being.
To fill these gaps, the study applies Latent Profile Analysis (LPA) to depressive and anxiety symptoms among family caregivers of dementia patients, following three objectives: identifying distinct psychological profiles of caregivers, examining their associations with dimensions of psychological well-being and exploring whether education and income act as protective moderators.
Although the concept of resilience is frequently invoked in the caregiving literature, the present study does not directly measure resilience as a distinct psychological construct. Instead, psychological well-being, as assessed by Ryff’s multidimensional model, is conceptualized as a complementary indicator of positive psychological functioning that may reflect resilience-related processes indirectly. Accordingly, references to resilience throughout the manuscript should be understood as descriptive and hypothesis-generating rather than as evidence of resilience per se.
2. Materials and Methods
This was a single-center, observational, analytical cross-sectional study conducted in the Neurology–Psychiatry Department of the C.F.2 Clinical Hospital (Bucharest, Romania). During the six-month recruitment period (November 2023–April 2024), 120 informal caregivers sought dementia-related services and were screened for eligibility; 73 caregivers met inclusion criteria and were enrolled. Eligibility required participants to be ≥30 years old, a family member of a person with dementia, to have provided care for at least six months and to be actively involved in caregiving at the time of recruitment. Non-family caregivers and individuals with incomplete questionnaire data were excluded. No financial incentives were provided.
Because the sample includes all caregivers who met criteria during this interval rather than a probabilistic sample, the study does not aim for population representativeness and is interpreted as exploratory.
Data collection employed a battery of instruments, chosen to capture both psychological outcomes and relevant contextual factors. These included Ryff’s Psychological Well-Being Scales (54 items), the Patient Health Questionnaire-9 (PHQ-9), the COVI Anxiety Scale, the Mini-Mental State Examination (MMSE; extracted from medical records) and an Anthropological Questionnaire (AQ) specifically developed for this study to gather socio-demographic information. All data were collected in person at the physician’s office. Caregivers completed the self-administered questionnaires on-site, with a researcher available for clarification. The assessment required approximately 45 min. Participants were informed that participation was voluntary and would not affect their or their relatives’ access to medical care.
Ryff’s Psychological Well-Being Scales (Romanian adaptation) [26,27,34] were used to evaluate caregivers’ positive psychological functioning. The instrument consists of six conceptually established dimensions: autonomy, personal growth, positive relations, self-acceptance, purpose in life and environmental mastery. Each dimension is assessed using nine distinct items. Responses are rated on a 6-point Likert scale ranging from strongly disagree to strongly agree, with 28 items reverse-coded to control for acquiescence bias. Subscales can be analyzed separately, but they can also be aggregated into a higher-order well-being index. Previous studies have demonstrated the reliability, factorial validity and cross-cultural robustness of this measure, including in Romanian populations [35,36,37,38]. Internal consistency coefficients (Cronbach’s α) for the present sample were calculated and are reported in the Section 3.
Depressive symptoms were assessed using the Patient Health Questionnaire-9 (PHQ-9). This widely used self-report measure is aligned with DSM-IV and DSM-5 diagnostic criteria for major depression. Scores are interpreted according to established clinical cut-offs: 5–9 = mild, 10–14 = moderate, 15–19 = moderately severe and 20–27 = severe depression. The PHQ-9 has been extensively validated in both clinical and community samples, consistently demonstrating strong psychometric properties [39,40,41,42,43]. In Romania, several validation studies have confirmed its reliability and screening utility across diverse patient groups [44].
Anxiety was evaluated using the COVI Anxiety Scale, a clinician-rated instrument designed to quantify the severity of anxiety symptoms. The scale categorizes scores into four severity levels: 3–5 = minimal or no anxiety, 6–8 = mild anxiety, 9–11 = moderate anxiety and 12–15 = severe anxiety. The COVI scale is recognized in both research and practice as a brief yet sensitive tool for the assessment of anxiety and it is frequently employed to guide treatment planning and targeted interventions [45].
Cognitive functioning of the care recipients was assessed using the Mini-Mental State Examination (MMSE). This 30-item screening tool evaluates orientation, attention, memory and language abilities, yielding a total score between 0 and 30, with lower scores indicating greater cognitive impairment. A threshold of 24 or below is commonly used to suggest the presence of clinically significant impairment. In this study, MMSE scores were extracted directly from patients’ medical records under institutional ethics approval. Because the data were de-identified, separate patient consent was not required. The MMSE is one of the most extensively validated instruments in geriatric and neurocognitive assessment and remains a gold standard in the field [46,47,48]. Because MMSE scores were recorded at diagnosis rather than concurrently with caregiver data collection, this temporal mismatch is acknowledged as a methodological limitation.
The Ryff scales, PHQ-9 and AQ were self-administered by participants in a private setting within the physician’s office at C.F.2 Clinical Hospital. In contrast, the COVI Anxiety Scale was clinician-rated by the attending psychiatrist. On average, the full assessment procedure required approximately 45 min per participant. To ensure clarity and appropriateness of the socio-demographic instrument (AQ), a pilot test was conducted with 15 formal caregivers; their feedback was carefully reviewed and integrated into the final version of the questionnaire. Given the multidomain structure of the Anthropological Questionnaire (AQ), internal consistency was assessed only for conceptually coherent subsets representing behavioral and functional characteristics of the care recipients. For these subsets, Cronbach’s α values generally exceeded thresholds considered acceptable for exploratory research (α ≥ 0.60) (e.g., Appetite/Eating domain showed α = 0.69, Current Activity α = 0.73 and Alternative Beliefs α = 0.75.
In contrast, AQ components referring to caregiver sociodemographic information (e.g., age, education, income, living arrangements) were not evaluated using internal consistency metrics because such variables do not represent latent constructs and are not expected to correlate. Accordingly, internal consistency analysis was limited to those AQ domains that conceptually functioned as scales rather than categorical descriptors. All AQ-derived indices were used descriptively, consistent with the instrument’s qualitative–anthropological grounding and the exploratory aims of the study.
All procedures adhered to established ethical standards for research involving human participants. Written informed consent was obtained from all caregivers prior to their participation in the study. Only caregivers were required to sign consent forms, as data regarding the cognitive status of care recipients (MMSE scores) were retrieved exclusively from medical records. These data were used in a fully de-identified format, thereby ensuring participant confidentiality and eliminating the need for separate patient consent.
The overall study protocol was reviewed and approved by the Ethics Committee of C.F.2 Clinical Hospital (No. 1781/06.02.2023) and data collection commenced only after ethics approval had been granted.
To further safeguard ethical compliance, participants were informed about the purpose, procedures, potential risks and benefits of the study and were assured that their participation was entirely voluntary and could be withdrawn at any point without affecting their or their relatives’ access to medical care. Data was stored and analyzed in aggregate form only, thereby preventing the identification of individual participants.
Statistical analyses were performed to explore latent heterogeneity in caregivers’ affective symptomatology and to examine its associations with psychological well-being. Prior to modeling, all continuous variables were standardized (z-scores) to place them on a comparable metric and reduce scale-related biases.
To identify distinct caregiver subgroups, a Latent Profile Analysis (LPA) was conducted using depressive symptoms (PHQ-9) and anxiety severity (COVI) as indicators. Competing models specifying one to five latent profiles were estimated. Model adequacy was evaluated primarily using the Bayesian Information Criterion (BIC), with the Akaike Information Criterion (AIC) considered secondarily. Model selection additionally considered conceptual interpretability, profile distinctiveness, adequacy of class sizes, and convergence stability.
After establishing the optimal latent profile solution, group differences across profiles were examined using one-way analyses of variance (ANOVAs) for PHQ-9 and COVI scores, followed by Tukey’s Honest Significant Difference (HSD) tests for pairwise comparisons. Effect sizes (η2) were calculated to quantify the magnitude of the observed differences. This approach allowed for a direct comparison of symptom severity across the emergent caregiver subgroups.
Associations between affective symptomatology (PHQ-9, COVI) and Ryff’s six psychological well-being dimensions were examined using Pearson correlation coefficients. These analyses assessed whether higher depressive or anxiety symptoms were systematically related to lower well-being across specific domains. Correlation analyses were selected to reflect the exploratory nature of the study and to capture broad relational patterns among variables.
Descriptive statistics for each latent profile are presented in tabular form, alongside graphical summaries illustrating profile-specific mean scores and score distributions. These visual and numerical summaries provided a comprehensive overview of within- and between-profile variability. Given the relatively small sample size, latent profile analyses were initially estimated using a parsimonious covariance structure (EII). To evaluate the robustness of the solution, sensitivity analyses were conducted by estimating alternative covariance structures with increasing flexibility, including EEI (allowing correlated indicators within classes) and VVI (allowing class-specific variances). Model fit indices and class structures were compared across specifications. This modeling strategy was selected to reduce the risk of overfitting and unstable parameter estimates, which are known concerns in mixture modeling with limited sample sizes. By constraining variances and excluding within-class covariances, the analysis emphasized robustness and replicability rather than fine-grained class differentiation. Finally, to evaluate the potential protective role of socio-economic resources, moderation analyses were conducted with caregivers’ education level and household income. These analyses tested whether higher education or income buffered the negative associations between depressive or anxiety symptoms and psychological well-being. Moderation was examined to determine whether socio-economic resources influence the strength of the relationship between psychological distress and well-being.
3. Results
A total of 73 family caregivers met the inclusion criteria and completed the study protocol. Most participants were women (75.3%), a distribution consistent with the well-documented gendered patterns of caregiving in dementia. Caregivers’ ages ranged from 34 to 78 years, with a mean age of 57.1 years (SD = 10.4), indicating that most participants were middle-aged or older adults, a demographic commonly involved in long-term family caregiving. Educational backgrounds were heterogeneous, spanning secondary to higher education, while household income varied considerably, suggesting substantial diversity in socio-economic resources within the sample. Most caregivers resided in urban areas, although a notable proportion came from rural settings, thereby reflecting the mixed socio-demographic composition of the catchment area of the C.F.2 Clinical Hospital.
Regarding their caregiving role, all participants were close family relatives of the care recipients, most frequently adult children or spouses. The minimum caregiving duration was six months; however, many caregivers had been providing support for several years, underscoring the chronic and demanding nature of dementia care in this population.
With respect to the cognitive functioning of the patients, as measured by the Mini-Mental State Examination (MMSE), most were documented as presenting moderate to severe impairment, a pattern aligned with the advanced clinical stages at which families typically seek specialized neurological and psychiatric services. These contextual characteristics—marked by high caregiving intensity, prolonged duration, and substantial cognitive decline in care recipients—underscore the significant emotional, cognitive and practical demands placed upon family caregivers in the present study.
To identify subgroups of caregivers based on affective symptomatology, a latent profile analysis (LPA) was conducted on standardized PHQ-9 (depression) and COVI (anxiety) scores. Models specifying one to five latent profiles were estimated using Gaussian finite mixture modeling with an EII covariance structure. Model fit indices (AIC, BIC, SABIC) are presented in Table 1.

Table 1.
Model fit indices for latent profile models.
Model fit indices provided mixed support regarding the optimal number of profiles (Table 1). The Bayesian Information Criterion (BIC) reached its minimum for the two-profile solution, whereas both the Akaike Information Criterion (AIC) and the sample-size-adjusted BIC (SABIC) favored the three-profile model. Given the small sample size, the minimal difference in BIC values between the two- and three-profile solutions, and the greater interpretability and clinical relevance of the three-profile solution, the three-profile model was retained as the most informative and parsimonious representation of latent heterogeneity in caregivers’ affective symptoms. Importantly, this solution should not be interpreted as identifying a definitive or exhaustive taxonomy of caregiver types, but rather as illustrating a limited set of broad patterns observable in this sample. Solutions with four and five profiles showed higher information criteria and smaller, less stable classes, and were therefore not retained. Sensitivity analyses were conducted to examine the robustness of the three-profile solution across different covariance structures. The VVI model did not converge, indicating that a highly flexible variance structure was not supported by the data. The EEI model yielded a slightly improved Bayesian Information Criterion compared to the EII model (ΔBIC = −4.15); however, this difference was small and did not indicate a substantial improvement in model fit. Importantly, the class structure was highly consistent across the EII and EEI specifications, with nearly identical class sizes and only minimal reclassification of individuals. Profile means for depressive symptoms and anxiety were also highly similar across models, and within-class correlations between indicators were small. Taken together, these findings suggest that the EII model provides a stable and parsimonious representation of the data and was therefore retained for all subsequent analyses.
The first profile (Profile 1; n = 24; 32.9%) was characterized by moderate depressive symptoms and moderate anxiety (PHQ-9: M = 11.50, SD = 2.27; COVI: M = 11.46, SD = 2.11), representing the subgroup with the lowest overall level of affective distress, although mean scores remained above standard clinical thresholds (Table 2). The second profile (Profile 2; n = 13; 17.8%) exhibited the highest symptom severity, marked by severe depressive symptoms and severe anxiety (PHQ-9: M = 26.85, SD = 0.38; COVI: M = 12.92, SD = 1.50), and thus represents the most psychologically vulnerable subgroup. The third profile (Profile 3; n = 36; 49.3%) comprised caregivers with moderately severe depressive symptoms accompanied by severe anxiety (PHQ-9: M = 19.72, SD = 1.88; COVI: M = 12.31, SD = 2.44) and constituted nearly half of the sample (SD = severe depression; MD = moderately severe depression; SA = severe anxiety; MA = moderate anxiety).

Table 2.
Latent profile characteristics for depressive symptoms (PHQ-9) and anxiety (COVI).
Group differences across the latent profiles were examined using one-way ANOVAs. For depressive symptoms (PHQ-9), the omnibus test indicated a highly significant effect of large magnitude, F(2, 70) = 307.20, p < 0.001, η2 = 0.90, suggesting that profile membership accounts for a very large proportion of variance in depressive severity. Post hoc Tukey comparisons showed that all three profiles differed significantly from one another, with Profile 2 (SD + SA) exhibiting the highest depressive symptoms, Profile 3 (MD + SA) showing intermediate levels, and Profile 1 (MD + MA) the lowest.
Classification quality was high. Average posterior probabilities for Profile 1, Profile 2 and Profile 3 were 0.92, 0.99, and 0.96, respectively, exceeding the recommended threshold of 0.85 and indicating excellent classification accuracy across profiles.
In contrast, anxiety severity (COVI) showed no statistically significant differences across profiles, F(2, 70) = 2.09, p = 0.131, η2 = 0.06, indicating only a small and non-significant effect. Although descriptive means suggested a trend toward elevated anxiety in Profile 3 (MD + SA) and lower anxiety in Profile 1 (MD + MA), these differences did not reach statistical significance.
Boxplots illustrating the distribution of PHQ-9 and COVI scores across profiles are presented in Figure 1 and Figure 2, respectively, and standardized mean symptom patterns for each latent profile are shown in Figure 3, providing a visual summary of the magnitude and direction of between-profile differences.
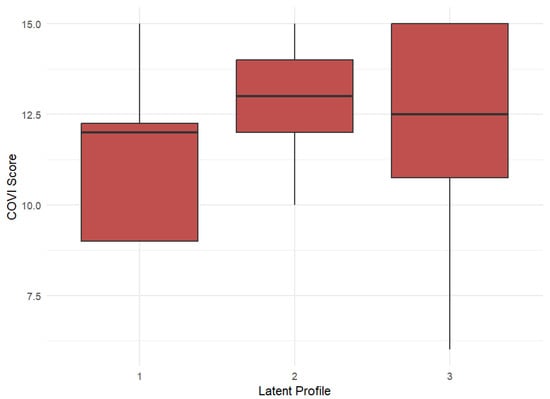
Figure 1.
Distribution of COVI scores by latent profile (median and interquartile ranges shown).
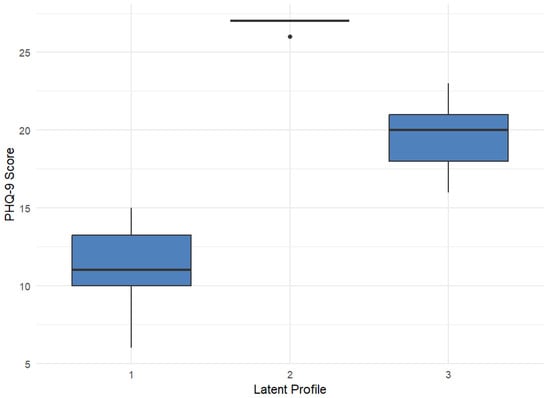
Figure 2.
Distribution of PHQ-9 scores by latent profile (median and interquartile ranges shown, points indicate outliers).
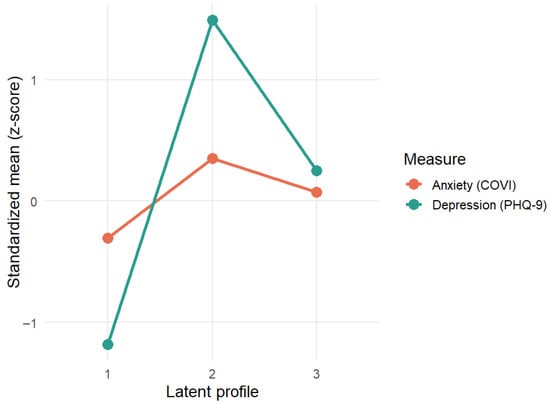
Figure 3.
Latent profile characteristics—PHQ-9 and COVI means.
Between-profile comparisons for the six Ryff psychological well-being dimensions indicated that several aspects of well-being differed significantly across the three latent profiles identified through LPA. The most pronounced difference was observed for purpose in life, where the omnibus ANOVA was significant, F(2, 70) = 4.53, p = 0.014, η2 = 0.115, showing that caregivers belonging to different latent profiles reported significantly different levels of purpose in life. A similar pattern emerged for self-acceptance, F(2, 70) = 3.90, p = 0.025, η2 = 0.100, again indicating systematic variation across profiles. Differences in personal growth approached significance, F(2, 70) = 2.93, p = 0.060, η2 = 0.077, suggesting a possible but not statistically confirmed profile-related effect. In contrast, positive relations, environmental mastery, and autonomy did not vary significantly across the three profiles (all p > 0.15), indicating that these dimensions were comparatively stable regardless of caregivers’ latent class membership.
Pearson correlations further clarified the associations between affective symptomatology and well-being (Table 3). Depressive symptoms (PHQ-9) were weakly but significantly positively correlated with self-acceptance (r = 0.25, p = 0.033) and autonomy (r = 0.24, p = 0.044). No other correlations between depressive symptoms and well-being dimensions were significant (all p > 0.16). The positive direction of these correlations should be interpreted with caution. Given the scoring structure of the Ryff scales and the cross-sectional nature of the data, these associations do not imply that higher depressive symptoms are beneficial for psychological well-being. Rather, they indicate that depressive symptom severity covaried with specific dimensions of self-evaluation and perceived autonomy in this sample, without establishing directionality or causality. Anxiety severity (COVI) showed no significant associations with any of the well-being dimensions (all p > 0.21), suggesting that variation in psychological well-being was more closely related to depressive symptoms than to anxiety levels in this sample.

Table 3.
Pearson correlations between PHQ-9, COVI and Ryff well-being dimensions.
To visualize the multivariate pattern of psychological well-being across profiles, a standardized (z-score) heatmap was generated for the six Ryff dimensions (Figure 4). The heatmap revealed a clear gradient of well-being across latent profiles. Values represent within-sample standardized z-scores.
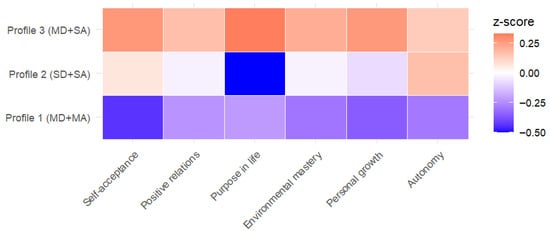
Figure 4.
Standardized Ryff Profiles (Z-scores).
Profile 1 (MD + MA) showed consistently negative z-scores across all Ryff domains, indicating levels below the sample mean. Profile 2 (SD + SA) showed scores largely centered around the sample mean, except for purpose in life, which exhibited a notable negative deviation, whereas Profile 3 (MD + SA) exhibited standardized scores above the sample mean across all Ryff dimensions.
This pattern indicates that Profile 3 (MD + SA) exhibited the highest relative scores across the Ryff dimensions despite presenting moderately severe affective symptoms, whereas Profile 1 (MD + MA) showed the lowest relative scores despite having the mildest affective symptomatology. Profile 2 (SD + SA) occupied an intermediate position, characterized by comparatively lower purpose in life. Overall, the heatmap corroborates the ANOVA findings by highlighting that psychological well-being, as indexed by standardized Ryff scores, does not follow a strictly linear relationship with affective symptom severity. This pattern underscores the multidimensional nature of psychological well-being and suggests that affective symptom severity alone may not fully capture caregivers’ subjective well-being profiles.
To evaluate whether global psychological well-being differed between the three latent profiles, an ANOVA was conducted using the composite Ryff total score. The omnibus test approached but did not reach statistical significance, F(2, 70) = 3.06, p = 0.053, η2 = 0.08, indicating a trend toward differences in overall psychological well-being across profiles.
Mean well-being scores increased progressively across the three profiles (Table 4). However, post hoc Tukey comparisons did not reveal statistically significant differences between profiles after correction for multiple comparisons (all p > 0.05) (Table 5).

Table 4.
Mean Ryff total scores vs. LPA profile.

Table 5.
Post-hoc Tukey Pairwise Comparisons.
Based on mean symptom scores, Profile 1 (MD + MA) represented the group with the lowest affective symptom burden, whereas Profiles 2 (SD + SA) and 3 (MD + SA) reflected progressively higher levels of depression and anxiety. Despite this pattern, caregivers in Profile 3 (MD + SA) showed descriptively higher overall psychological well-being compared with those in Profile 1 (MD + MA). Although this difference did not reach conventional statistical significance at the omnibus level, the observed pattern suggests that psychological well-being in this sample does not vary strictly as a linear function of affective symptom severity.
In contrast, Profile 2 (SD + SA), which was characterized by the most severe affective symptomatology, displayed intermediate levels of overall psychological well-being. This profile was not consistently associated with either particularly low or high well-being, but rather showed a more heterogeneous pattern, including comparatively lower scores on specific dimensions such as purpose in life. This pattern may reflect a subgroup of caregivers experiencing high emotional distress without corresponding compensatory psychological resources. No other pairwise differences between profiles were observed.
To examine whether the three latent profiles differed in socio-economic characteristics, caregivers’ education level and monthly household income were compared across profiles (Table 6). Education levels were relatively evenly distributed among the three groups: Profile 1 (MD + MA) included comparable proportions of caregivers with high school and higher education, Profile 2 (SD + SA) showed a similar pattern with a slightly higher proportion of caregivers in the secondary education category, and Profile 3 (MD + SA) presented the highest proportion of caregivers with high school education. Fisher’s exact test indicated that these distributions did not differ significantly across profiles.

Table 6.
Distribution of education level and household income across the three latent profiles (%).
A similar pattern emerged for household income. Profile 1 (MD + MA) and Profile 2 (SD + SA) were comparable in their concentration of caregivers within the middle-income range (400–1000 EUR), whereas Profile 3 (MD + SA) showed a somewhat higher proportion of caregivers with lower income (up to 400 EUR) and a moderately higher proportion reporting incomes above 1000 EUR. Despite these descriptive contrasts, the association between income and profile membership did not reach statistical significance.
Taken together, the results indicate that the three latent profiles identified through LPA reflect meaningful variation in caregivers’ affective symptomatology, with implications for their psychological well-being but not for their socio-economic positioning. While education and household income did not differ significantly across profiles—indicating that depressive and anxiety symptom patterns cut across demographic and economic strata—clear differences emerged in psychological functioning. Caregivers in Profile 3 (MD + SA), characterized by the moderately severe affective symptom levels, reported significantly higher overall well-being than those in Profile 1 (MD + MA), which exhibited the lowest symptom severity, whereas other pairwise contrasts were nonsignificant.
These findings suggest that emotional distress represents an important dimension of caregiver functioning in this sample; however, the relationship between affective symptom severity and psychological well-being is not strictly linear and appears to operate independently of socio-economic resources.
4. Discussion
The present study identified three distinct affective symptom profiles among family caregivers of individuals with dementia, reflecting meaningful heterogeneity in depressive and anxiety symptomatology rather than differences driven primarily by demographic or socio-economic characteristics. This pattern is consistent with previous research documenting substantial variability in caregivers’ emotional adjustment, even within broadly similar caregiving contexts [18,25].
The three profiles captured qualitatively different configurations of affective distress. Profile 1 (moderate depression–moderate anxiety) was characterized by the lowest levels of depressive symptoms combined with moderate anxiety. Profile 3 (moderately severe depression–severe anxiety) displayed elevated depressive and anxiety symptoms, whereas Profile 2 (severe depression–severe anxiety) exhibited extremely high levels of affective distress, with mean PHQ-9 scores approaching the upper limit of the scale. These findings indicate that depressive and anxiety symptoms do not simply increase along a single continuum, but tend to co-occur in distinct patterns with different clinical implications [29,49,50].
Although the three profiles can be broadly conceptualized along a severity gradient of affective distress, the clinical relevance of this gradient was not uniform across groups. In particular, Profile 2 (severe depression–severe anxiety) warrants special attention. Caregivers in this subgroup reported pervasive depressive symptomatology, likely reflecting near-daily endorsement of most PHQ-9 items, including suicidality-related symptoms. This level of distress suggests profound psychological suffering and potentially heightened clinical risk. Notably, this profile also showed particularly low scores on purpose in life, pointing to a marked erosion of meaning-related psychological resources. From a clinical perspective, Profile 2 represents the most vulnerable subgroup identified in the present study and underscores the importance of proactive screening, risk assessment, and targeted psychological interventions.
Differences in affective symptomatology were mirrored, though not perfectly, in caregivers’ psychological well-being. At the dimensional level, purpose in life and self-acceptance showed the clearest variation across profiles, whereas the composite well-being index (Ryff total) demonstrated only a trend-level omnibus effect. Despite this, post-hoc comparisons revealed that caregivers in Profile 3 reported higher overall psychological well-being than those in Profile 1, even though Profile 3 exhibited more pronounced depressive and anxiety symptoms. This counterintuitive pattern challenges simple linear models linking symptom severity directly to psychological well-being and suggests that affective symptoms and psychological well-being are not merely opposite ends of a single dimension. This contrast refers specifically to relative differences within the sample, reflecting the coexistence of elevated affective symptom severity and comparatively preserved psychological well-being, rather than the absence of psychological distress.
One possible interpretation is that caregivers in Profile 3 may rely on compensatory or resilience-related processes—such as stronger meaning-making, emotional engagement, or perceived competence in the caregiving role—that help sustain well-being despite elevated affective symptoms [29,32]. In contrast, caregivers in Profile 1 may experience diminished well-being due to factors not captured directly by depressive and anxiety symptoms, such as caregiver fatigue, role overload, or unresolved interpersonal stressors.
The heatmap of standardized Ryff scores reinforced this interpretation by showing that caregivers in Profile 3 (MD + SA)—though moderately symptomatic—displayed the highest psychological well-being across all Ryff dimensions, whereas Profile 1 (MD + MA) consistently scored lower. Profile 2 (SD + SA) showed an intermediate pattern of well-being, with values closer to the sample mean but with notably lower scores on specific dimensions, particularly purpose in life. This overall configuration suggests the presence of compensatory or resilience-related processes (e.g., meaning in caregiving, perceived competence, or social support) that may buffer the impact of affective symptoms on psychological well-being in some caregivers. In contrast, the comparatively low well-being observed in Profile 1 (MD + MA), despite the lowest levels of depressive and anxiety symptoms, indicates that reduced affective symptoms alone do not guarantee psychological flourishing. Taken together, these findings support a multidimensional view in which caregiver well-being is shaped by the interplay between emotional distress and protective psychological resources rather than by symptom severity in isolation [49,50,51,52,53,54,55,56,57,58].
Correlation analyses provided convergent but more fine-grained evidence regarding the associations between affective symptoms and psychological well-being. Depressive symptoms were weakly and positively associated with self-acceptance and autonomy, two central components of psychological well-being that reflect caregivers’ self-valuation and perceived capacity to manage life demands. Importantly, prior research consistently indicates that depressive symptoms in caregivers are generally associated with poorer self-worth, reduced perceived control, and impaired adaptive functioning [29,32]. The weak positive associations observed between depressive symptoms and the dimensions of self-acceptance and autonomy were unexpected and diverge from the dominant literature linking depression to poorer psychological functioning. These findings should therefore be interpreted as sample-specific and exploratory. One possible explanation is that caregivers with higher symptom awareness may also engage in greater self-reflection or perceive autonomy in the caregiving role despite emotional distress. Alternatively, these associations may reflect measurement or contextual effects rather than substantive psychological advantages. Replication in larger samples is required before drawing substantive conclusions. In contrast, anxiety severity showed no meaningful associations with any of the Ryff dimensions, suggesting that in this sample anxiety may have been more contextually fluctuating and less tightly coupled with global well-being than depressive symptomatology.
Socio-economic characteristics—namely education level and household income—did not differ significantly across profiles and were not significantly associated with profile membership, nor did they moderate the observed relationships between affective symptoms and psychological well-being. Although descriptive analyses indicated that one profile included a somewhat higher proportion of caregivers with lower income, this pattern did not reach statistical significance and should be interpreted with caution. These findings are in line with previous evidence indicating that, while socio-economic factors can shape access to services and long-term care arrangements, emotional strain and psychological distress in dementia caregiving often cut across socio-economic strata [49,50,51,52,53,54,55,56,57,58]. The absence of significant associations between education, income, and either profile membership or psychological well-being should be interpreted considering the study’s exploratory design and limited statistical power. Importantly, these results do not rule out the potential protective role of socio-economic resources but suggest that, in this sample, affective symptom configurations were more salient than structural socio-economic differences. In this context, psychological burden and well-being appeared to be more strongly linked to affective symptom configurations and available psychological resources than to educational attainment or financial status.
Overall, the identification of three distinct profiles underscores the importance of assessing both depression and anxiety simultaneously and of considering their combined expression when evaluating caregiver mental health. The findings point to specific subgroups—particularly caregivers with high co-occurring depressive and anxiety symptoms (Profile 2 (SD + SA)—for whom targeted interventions may be especially warranted. At the same time, the unexpected advantage in well-being observed in Profile 3 (MD + SA) relative to the least symptomatic group highlights the potential role of resilience-related processes and suggests that interventions aiming to strengthen meaning, self-acceptance, and autonomy may be beneficial even in the presence of persistent affective symptoms. In sum, the present study contributes to a more nuanced understanding of caregiver adjustment in dementia, emphasizing that psychological well-being reflects not only the presence or absence of distress but also the capacity to mobilize personal and contextual resources in the face of ongoing caregiving demands.
5. Conclusions
This study shows that family caregivers of individuals with dementia can be meaningfully grouped into three distinct psychological profiles, characterized by different constellations of depressive and anxiety symptoms. These findings demonstrate that caregiver distress does not follow a simple severity gradient, but instead forms qualitatively different profiles, each associated with distinct patterns of psychological well-being. Such heterogeneity underscores the importance of individualized screening approaches that consider both depression and anxiety. Enhancing caregiver mental health is essential not only for improving their own well-being but also for supporting the sustainability and quality of care provided to people living with dementia.
6. Limitations and Future Directions
Several limitations of this study should be acknowledged. First, the single-center, cross-sectional design limits the generalizability of the findings and does not permit conclusions regarding causality or the temporal stability of the identified profiles. Second, although adequate for exploratory latent profile analysis, the sample size was modest (n = 73), which may have reduced statistical power, particularly for detecting small-to-moderate differences in psychological well-being across profiles. Accordingly, the LPA findings should be considered exploratory and in need of replication in larger samples. To reduce the risk of overfitting, we relied on a parsimonious covariance structure and conducted sensitivity analyses across alternative model specifications; nevertheless, solution stability should be re-evaluated in future studies with greater statistical power. Third, the study relied on self-report measures for caregivers and retrospective MMSE scores for patients; despite the strong psychometric properties of these instruments, reporting biases and temporal mismatch cannot be fully excluded. Moreover, the study did not directly assess potentially relevant psychological or contextual variables—such as coping strategies, perceived meaning in caregiving, resilience, or social support—that may help explain why some caregivers maintain higher well-being despite elevated symptoms.
Future research should aim to replicate these findings in larger and more diverse, multi-center samples, enabling more stable estimation of latent profiles. Longitudinal designs are needed to examine transitions between profiles over time and to clarify whether specific symptom configurations predict future changes in well-being or caregiving outcomes. Further work should also incorporate additional psychological and contextual factors to better understand the mechanisms underlying differences in well-being among caregivers and to identify targets for tailored intervention strategies.
Taken together, these limitations underscore that the present findings should be viewed as hypothesis-generating rather than confirmatory. The identified profiles are intended to illustrate potential patterns of caregiver adjustment rather than to define stable or generalizable caregiver typologies.
Author Contributions
Conceptualization, C.S.G., L.F.T. and S.T.; formal analysis, C.S.G., L.F.T. and S.T.; investigation, L.F.T.; methodology, C.S.G., L.F.T. and S.T.; software, C.S.G., L.F.T. and S.T.; supervision, C.S.G., L.F.T. and S.T.; validation, C.S.G., L.F.T. and S.T.; writing—original draft, C.S.G., L.F.T. and S.T.; writing—review and editing, C.S.G., L.F.T. and S.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of C.F.2 Clinical Hospital (approval code: 1781; approval date: 6 February 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding authors. The data are not publicly available due to ethical issues.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Nichols, E.; Steinmetz, J.D.; Vollset, S.E.; Fukutaki, K.; Chalek, J.; Abd-Allah, F.; Abdoli, A.; Abualhasan, A.; Abu-Gharbieh, E.; Akram, T.T.; et al. Estimation of the Global Prevalence of Dementia in 2019 and Forecasted Prevalence in 2050: An Analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022, 7, e105–e125. [Google Scholar] [CrossRef] [PubMed]
- Alzheimer’s Disease Facts and Figures. Alzheimer’s Dement. 2024, 20, 3708–3821. [CrossRef]
- Stallard, P.J.E.; Ukraintseva, S.V.; Doraiswamy, P.M. Changing Story of the Dementia Epidemic. JAMA 2025, 333, 1579. [Google Scholar] [CrossRef] [PubMed]
- Dou, X.; Lenzen, S.; Connelly, L.B.; Lin, R. Generational Differences in Age-Specific Dementia Prevalence Rates. JAMA Netw. Open 2025, 8, e2513384. [Google Scholar] [CrossRef]
- Dementia. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 18 May 2025).
- Licher, S.; Darweesh, S.K.L.; Wolters, F.J.; Fani, L.; Heshmatollah, A.; Mutlu, U.; Koudstaal, P.J.; Heeringa, J.; Leening, M.J.G.; Ikram, M.K.; et al. Lifetime Risk of Common Neurological Diseases in the Elderly Population. J. Neurol. Neurosurg. Psychiatry 2019, 90, 148–156. [Google Scholar] [CrossRef]
- OECD. Health at a Glance 2023: OECD Indicators. In Health at a Glance; OECD: Paris, France, 2023; ISBN 978-92-64-95793-0. [Google Scholar]
- Dorsey, E.R.; Sherer, T.; Okun, M.S.; Bloem, B.R. The Emerging Evidence of the Parkinson Pandemic. J. Park. Dis. 2018, 8, S3–S8. [Google Scholar] [CrossRef]
- Furdu-Lunguț, E.; Antal, C.; Turcu, S.; Costea, D.-G.; Mitran, M.; Mitran, L.; Diaconescu, A.-S.; Novac, M.-B.; Gorecki, G.-P. Study on Pharmacological Treatment of Impulse Control Disorders in Parkinson’s Disease. J. Clin. Med. 2024, 13, 6708. [Google Scholar] [CrossRef]
- United Kingdom of Great Britain and Northern Ireland. Available online: https://data.who.int/countries/826 (accessed on 16 May 2025).
- Ye, J.; Wan, H.; Chen, S.; Liu, G.-P. Targeting Tau in Alzheimer’s Disease: From Mechanisms to Clinical Therapy. Neural Regen. Res. 2024, 19, 1489–1498. [Google Scholar] [CrossRef]
- Rapoport, M.; Dawson, H.N.; Binder, L.I.; Vitek, M.P.; Ferreira, A. Tau Is Essential to β-Amyloid-Induced Neurotoxicity. Proc. Natl. Acad. Sci. USA 2002, 99, 6364–6369. [Google Scholar] [CrossRef] [PubMed]
- Hardy, J.; Selkoe, D.J. The Amyloid Hypothesis of Alzheimer’s Disease: Progress and Problems on the Road to Therapeutics. Science 2002, 297, 353–356. [Google Scholar] [CrossRef]
- Jack, C.R.; Bennett, D.A.; Blennow, K.; Carrillo, M.C.; Dunn, B.; Haeberlein, S.B.; Holtzman, D.M.; Jagust, W.; Jessen, F.; Karlawish, J.; et al. NIA-AA Research Framework: Toward a Biological Definition of Alzheimer’s Disease. Alzheimer’s Dement. 2018, 14, 535–562. [Google Scholar] [CrossRef]
- Georges, J.; Jansen, S.; Jackson, J.; Meyrieux, A.; Sadowska, A.; Selmes, M. Alzheimer’s Disease in Real Life—The Dementia Carer’s Survey. Int. J. Geriat. Psychiatry 2008, 23, 546–551. [Google Scholar] [CrossRef]
- Alzheimer Europe. 2006 Alzheimer Europe Survey: Who Cares? The State of Dementia Care in Europe; Alzheimer Europe: Luxembourg, 2006; p. 12. [Google Scholar]
- Alzheimer Europe. European Carers’ Report 2018: Carers’ Experiences of Diagnosis in Five European Countries; Alzheimer Europe: Luxembourg, 2018; ISBN 978-999959-995-2-0. [Google Scholar]
- Pinquart, M.; Sörensen, S. Differences between Caregivers and Noncaregivers in Psychological Health and Physical Health: A Meta-Analysis. Psychol. Aging 2003, 18, 250–267. [Google Scholar] [CrossRef]
- Abdelhalim, D.S.; Ahmed, M.M.; Hussein, H.A.; Khalaf, O.O.; Sarhan, M.D. Burden of Care, Depression and Anxiety Among Family Caregivers of People with Dementia. J. Prim. Care Community Health 2024, 15, 21501319241288029. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.-T. Dementia Caregiver Burden: A Research Update and Critical Analysis. Curr. Psychiatry Rep. 2017, 19, 64. [Google Scholar] [CrossRef]
- Grande, G.; Shield, T.; Bayliss, K.; Rowland, C.; Flynn, J.; Bee, P.; Hodkinson, A.; Panagioti, M.; Farquhar, M.; Harris, D.; et al. Understanding the Potential Factors Affecting Carers’ Mental Health during End-of-Life Home Care: A Meta Synthesis of the Research Literature. Health Soc. Care Deliv. Res. 2025, 13, 165–242. [Google Scholar] [CrossRef]
- Pacheco Barzallo, D.; Schnyder, A.; Zanini, C.; Gemperli, A. Gender Differences in Family Caregiving. Do Female Caregivers Do More or Undertake Different Tasks? BMC Health Serv. Res. 2024, 24, 730. [Google Scholar] [CrossRef] [PubMed]
- Sörensen, S.; Conwell, Y. Issues in Dementia Caregiving: Effects on Mental and Physical Health, Intervention Strategies and Research Needs. Am. J. Geriatr. Psychiatry 2011, 19, 491–496. [Google Scholar] [CrossRef] [PubMed]
- González-Fernández, M.; Davis, C.; Molitoris, J.J.; Newhart, M.; Leigh, R.; Hillis, A.E. Formal Education, Socioeconomic Status and the Severity of Aphasia After Stroke. Arch. Phys. Med. Rehabil. 2011, 92, 1809–1813. [Google Scholar] [CrossRef]
- Brodaty, H.; Donkin, M. Family Caregivers of People with Dementia. Dialogues Clin. Neurosci. 2009, 11, 217–228. [Google Scholar] [CrossRef]
- Ryff, C.D. Happiness Is Everything, or Is It? Explorations on the Meaning of Psychological Well-Being. J. Personal. Soc. Psychol. 1989, 57, 1069–1081. [Google Scholar] [CrossRef]
- Ryff, C.D. Beyond Ponce de Leon and Life Satisfaction: New Directions in Quest of Successful Ageing. Int. J. Behav. Dev. 1989, 12, 35–55. [Google Scholar] [CrossRef]
- Ryff, C.D.; Keyes, C.L.M. The Structure of Psychological Well-Being Revisited. J. Personal. Soc. Psychol. 1995, 69, 719–727. [Google Scholar] [CrossRef]
- Wister, A.; Li, L.; Mitchell, B.; Wolfson, C.; McMillan, J.; Griffith, L.E.; Kirkland, S.; Raina, P.; Canadian Longitudinal Study on Aging (CLSA) Team; Costa, A.; et al. Levels of Depression and Anxiety Among Informal Caregivers During the COVID-19 Pandemic: A Study Based on the Canadian Longitudinal Study on Aging. J. Gerontol. Ser. B 2022, 77, 1740–1757. [Google Scholar] [CrossRef]
- Ashley, N.R.; Kleinpeter, C.H. Gender Differences in Coping Strategies of Spousal Dementia Caregivers. J. Hum. Behav. Soc. Environ. 2002, 6, 29–46. [Google Scholar] [CrossRef]
- Geiger, J.R.; Wilks, S.E.; Lovelace, L.L.; Chen, Z.; Spivey, C.A. Burden Among Male Alzheimer’s Caregivers: Effects of Distinct Coping Strategies. Am. J. Alzheimer’s Dis. Other Dement. 2015, 30, 238–246. [Google Scholar] [CrossRef]
- Pinquart, M.; Sorensen, S. Correlates of Physical Health of Informal Caregivers: A Meta-Analysis. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2007, 62, P126–P137. [Google Scholar] [CrossRef]
- Schulz, R.; Martire, L.M. Family Caregiving of Persons with Dementia: Prevalence, Health Effects and Support Strategies. Am. J. Geriatr. Psychiatry 2004, 12, 240–249. [Google Scholar] [CrossRef]
- Costea-Bărluțiu, C.; Bălaș-Baconschi, C.; Hathazi, A. Romanian Adaptation of the Ryff’s Psychological Well-Being Scale: Brief Report of the Factor Structure and Psychometric Properties. J. Evid.-Based Psychother. 2018, 18, 21–34. [Google Scholar] [CrossRef]
- Luştrea, A.; Ghazi, L.A.; Predescu, M. Adapting and Validating Ryff’s Psychological Well-Being Scale on Romanian Student Population. Educatia 21 2018, 16, 118. [Google Scholar] [CrossRef]
- García, M.J.; Del Valle, M.V.; López Morales, H.; Urquijo, S. Propiedades Psicométricas de La Escala de Bienestar Psicológico de Ryff En Argentina. Cienc. Psicol. 2024, 18, e-3739. [Google Scholar] [CrossRef]
- Ruini, C.; Ottolini, F.; Rafanelli, C.; Ryff, C.; Fava, G.A. La Validazione Italiana Delle Psychological Well-Being Scales (PWB). Riv. Psichiatr. 2003, 38, 117–130. [Google Scholar]
- Van Dierendonck, D. The Construct Validity of Ryff’s Scales of Psychological Well-Being and Its Extension with Spiritual Well-Being. Personal. Individ. Differ. 2004, 36, 629–643. [Google Scholar] [CrossRef]
- Bains, N.; Abdijadid, S. Major Depressive Disorder. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Sawaya, H.; Atoui, M.; Hamadeh, A.; Zeinoun, P.; Nahas, Z. Adaptation and Initial Validation of the Patient Health Ques-tionnaire—9 (PHQ-9) and the Generalized Anxiety Disorder—7 Questionnaire (GAD-7) in an Arabic Speaking Lebanese Psychiatric Outpatient Sample. Psychiatry Res. 2016, 239, 245–252. [Google Scholar] [CrossRef]
- Huang, F.Y.; Chung, H.; Kroenke, K.; Delucchi, K.L.; Spitzer, R.L. Using the Patient Health Questionnaire-9 to Measure De-pression among Racially and Ethnically Diverse Primary Care Patients. J. Gen. Intern. Med. 2006, 21, 547–552. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L. The PHQ-9: A New Depression Diagnostic and Severity Measure. Psychiatr. Ann. 2002, 32, 509–515. [Google Scholar] [CrossRef]
- Lipman, R.S.; Covi, L.; Downing, R.; Fisher, S.; Kahn, R.; McNair, D.; Rickels, K.; Smith, V. Pharmacotherapy of Anxiety and Depression. Psychopharmacol. Bull. 1981, 17, 91–103. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. Mini-Mental State. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Tombaugh, T.N.; McIntyre, N.J. The Mini-Mental State Examination: A Comprehensive Review. J. Am. Geriatr. Soc. 1992, 40, 922–935. [Google Scholar] [CrossRef]
- Monroe, T.; Carter, M. Using the Folstein Mini Mental State Exam (MMSE) to Explore Methodological Issues in Cognitive Aging Research. Eur. J. Ageing 2012, 9, 265–274. [Google Scholar] [CrossRef]
- García-Mochón, L.; Peña-Longobardo, L.M.; Del Río-Lozano, M.; Oliva-Moreno, J.; Larrañaga-Padilla, I.; García-Calvente, M.D.M. Determinants of Burden and Satisfaction in Informal Caregivers: Two Sides of the Same Coin? The CUIDAR-SE Study. Int. J. Environ. Res. Public Health 2019, 16, 4378. [Google Scholar] [CrossRef]
- Vitaliano, P.P.; Echeverria, D.; Yi, J.; Phillips, P.E.M.; Young, H.; Siegler, I.C. Psychophysiological Mediators of Caregiver Stress and Differential Cognitive Decline. Psychol. Aging 2005, 20, 402–411. [Google Scholar] [CrossRef]
- Cejalvo, E.; Martí-Vilar, M.; Merino-Soto, C.; Aguirre-Morales, M.T. Caregiving Role and Psychosocial and Individual Factors: A Systematic Review. Healthcare 2021, 9, 1690. [Google Scholar] [CrossRef]
- Romão, M.E.; Setti, I.; Alfano, G.; Barello, S. Exploring Risk and Protective Factors for Burnout in Professionals Working in Death-Related Settings: A Scoping Review. Public Health 2025, 241, 1–11. [Google Scholar] [CrossRef]
- Haro, J.M.; Kahle-Wrobleski, K.; Bruno, G.; Belger, M.; Dell’Agnello, G.; Dodel, R.; Jones, R.W.; Reed, C.C.; Vellas, B.; Wimo, A.; et al. Analysis of Burden in Caregivers of People with Alzheimer’s Disease Using Self-Report and Supervision Hours. J. Nutr. Health Aging 2014, 18, 677–684. [Google Scholar] [CrossRef]
- Mahoney, R.; Regan, C.; Katona, C.; Livingston, G. Anxiety and Depression in Family Caregivers of People With Alzheimer Disease: The LASER-AD Study. Am. J. Geriatr. Psychiatry 2005, 13, 795–801. [Google Scholar] [CrossRef]
- Chiao, C.-Y.; Wu, H.-S.; Hsiao, C.-Y. Caregiver Burden for Informal Caregivers of Patients with Dementia: A Systematic Review. Int. Nurs. Rev. 2015, 62, 340–350. [Google Scholar] [CrossRef]
- Liang, X.; Guo, Q.; Luo, J.; Li, F.; Ding, D.; Zhao, Q.; Hong, Z. Anxiety and Depression Symptoms among Caregivers of Care-Recipients with Subjective Cognitive Decline and Cognitive Impairment. BMC Neurol. 2016, 16, 191. [Google Scholar] [CrossRef]
- Rada, C. Factors Associated with Depression in Middle-Aged and Elderly People in Romania. Psichologija 2020, 61, 33–50. [Google Scholar] [CrossRef]
- Schulz, R.; Sherwood, P.R. Physical and Mental Health Effects of Family Caregiving. Am. J. Nurs. 2008, 108, 23–27. [Google Scholar] [CrossRef]
- Tatomirescu, L.F.; Glavce, C.S.; Prada, G.I.; Borosanu, A.; Turcu, S. Socio-Demographic Factors Linked to Psychological Well-Being in Dementia Caregivers. Healthcare 2025, 13, 2235. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.