Abstract
Simultaneous recording of breathing and heart rate signals was carried out on a healthy volunteer with a fully knitted, non-sports-type garment. Breathing was recorded using two knitted respiratory inductive plethysmography (RIP) sensors. Electrocardiogram (ECG) recordings were obtained from three knitted electrodes. The knitted garment design was customised for the specific requirements of RIP and ECG by adapting the needle size and/or introducing knit-in-elastic in the sensor areas. RIP was read out using an in-house-developed cross-coupled complementary oscillator circuit. The ECG was recorded using the commercial OpenBCI board. The sensors produced excellent signal quality that allowed for simple signal processing to extract information on heart and breathing rates, showing good correlation between the two.
1. Introduction
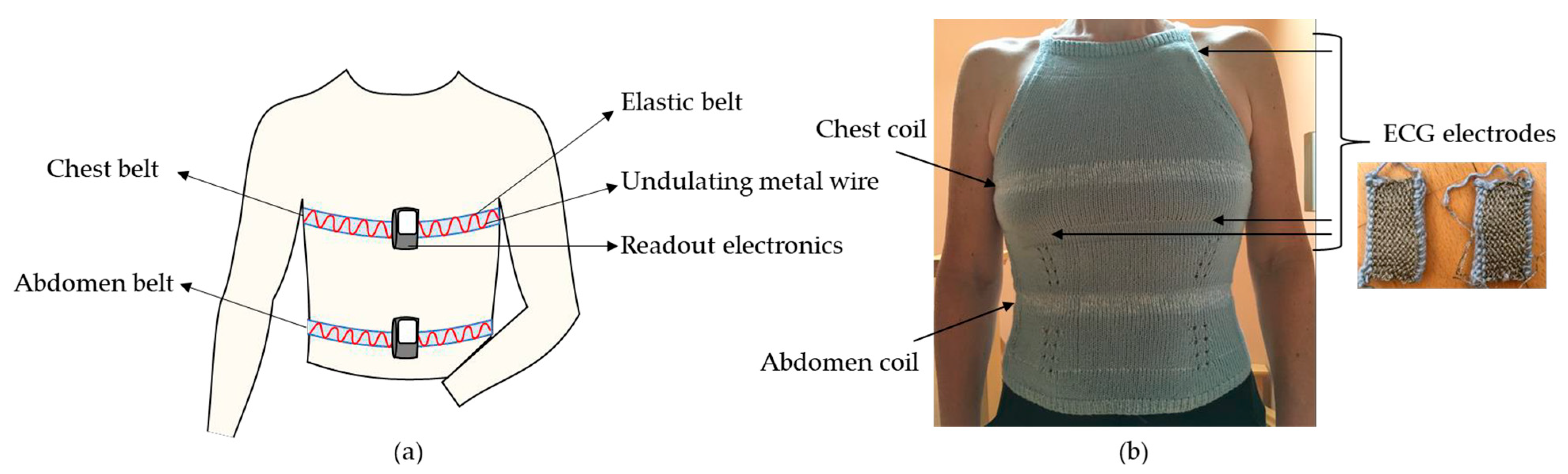
Among service prices, population growth and aging, chronic conditions play a major role in substantially increasing healthcare costs. Wearable technology is attractive for continuous health monitoring and thus reduces the costs associated with doctor–patient interactions. Knitting offers the possibility to integrate different sensors for non-invasive and real-time breathing and heart rate monitoring in wearable garments. This can be achieved by tracking changes in chest/abdomen circumference using transduction methods such as resistance changes [1,2] or inductance changes of a coil wound around the body [3]. In most cases, RIP (respiratory inductive plethysmography) is implemented in elastic belts that are strapped around the chest and/or the abdomen, shown in Figure 1a. For ECG, gelled electrodes are normally taped on the body. A more wearable implementation comes in the form of dry knitted electrodes [4]. In our implementation, knitted RIP and ECG were optimised in conjunction with the garment to increase sensitivity and reduce motion artifacts, illustrated in Figure 1b.
Figure 1.
(a) Classical RIP implementation using elastic belts with one metal winding strapped around the chest and abdomen. (b) Knitted implementation of RIP in a halter top, on the chest and on the abdomen. The ECG electrodes and their positions on the inside of the garment are shown with arrows. Inset show the knitted electrodes.
2. Materials and Methods
2.1. Knitted Breathing Sensors
In our previous work, RIP sensors were integrated into a garment by a thin, circular knitted, insulated metal wire with yarn [5], achieving ultra-wearability and higher sensitivity proportional to the number of knitted rows with metal [6]. Figure 1b shows the implementation of two knitted coils, at the chest and the abdomen level. The RIP sensors were knitted using a needle size appropriate for the yarn, allowing the knit’s natural elasticity to accommodate the stretch when inhaling. Knit-in-elastic is added to force the knit to return to its minimum circumference when exhaling.
2.2. RIP Read-Out Electronics
A complementary cross-coupled pair oscillator translates the coil’s inductance to frequency [7]. For a wide range of coil dimensions to be recorded, the oscillator is followed by a rail-to-rail comparator that converts the sine-wave oscillations to a rectangular waveform. An esp32 microcontroller counts the frequency and logs the data to a micro-SD card [8].
2.3. Knitted ECG Electrodes
The ECG electrodes were knitted using Ag-coated polyester thread with a size equivalent to commercial pads. The different implementations are given in Table 1.

Table 1.
Five different types of knitted electrodes. The four on the right were knitted by hand.
By knitting different yarn thicknesses and adapting the needles’ size, the roughness of the rib side of the electrodes can be controlled while maintaining a similar stitch density, unlike in the previous work [10]. The rib side of the knit is placed against the skin to reduce movement artifacts and improve signal quality. To decrease the movement artifacts in the ECG signals further, the regions in the knitted garment where the electrodes are sewn in, are knitted with a smaller needle size. This reduces the elasticity of the knit in those areas, reducing movement against the body. The ECG signals were recorded using the OpenBCI board [11]. The quality of the electrodes was defined by comparing the mean and median signal and signal frequency histogram that must be non-Gaussian. The electrode with 3 Shieldex threads and 2 mm needles gave the best performance.
3. Results
3.1. Breathing of the Volunteer
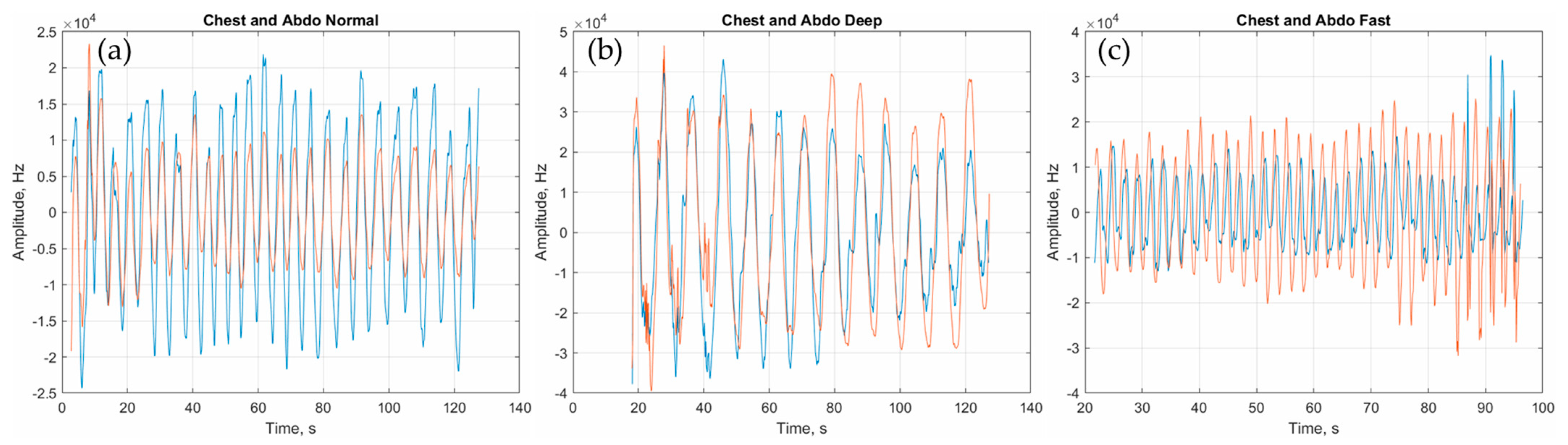
The performance parameters for a range of coils are given in Table 2. A larger number of windings N results in larger sensitivity s and smaller current icoil. Thus, although Q is low for high N, a reduced icoil is better for user safety. Using coils with N = 8 in the knit of Figure 1, different breathing patterns, normal, slow and fast, were recorded from a healthy volunteer and are given in Figure 2.

Table 2.
Characteristics of the knitted coil: c circumference, N number of windings, s sensitivity, fosc oscillator frequency, Q quality factor and icoil the RMS current through the coil at fosc.
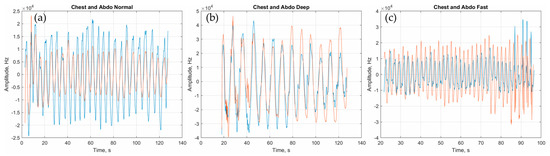
Figure 2.
Frequency variations of the chest (blue) and abdomen (orange) (colour available online) coils due to breathing. (a) Normal breathing, (b) deep and slow breathing and (c) fast breathing.
Breathing parameters (Table 3) were extracted using signal processing in MATLAB. The signal amplitude is related to the effort from the chest and abdomen. The phase difference during fast breathing mirrors minor hyperventilation and is the result of the increased work of breathing and the use of accessory muscles.

Table 3.
Breathing parameters. BPM: breaths per minute, Ti/Ttot the ratio of the inhalation time to the total time of one breath, |A| the mean amplitude of one breath and Δϕ the phase difference between the signal from the chest and the abdomen.
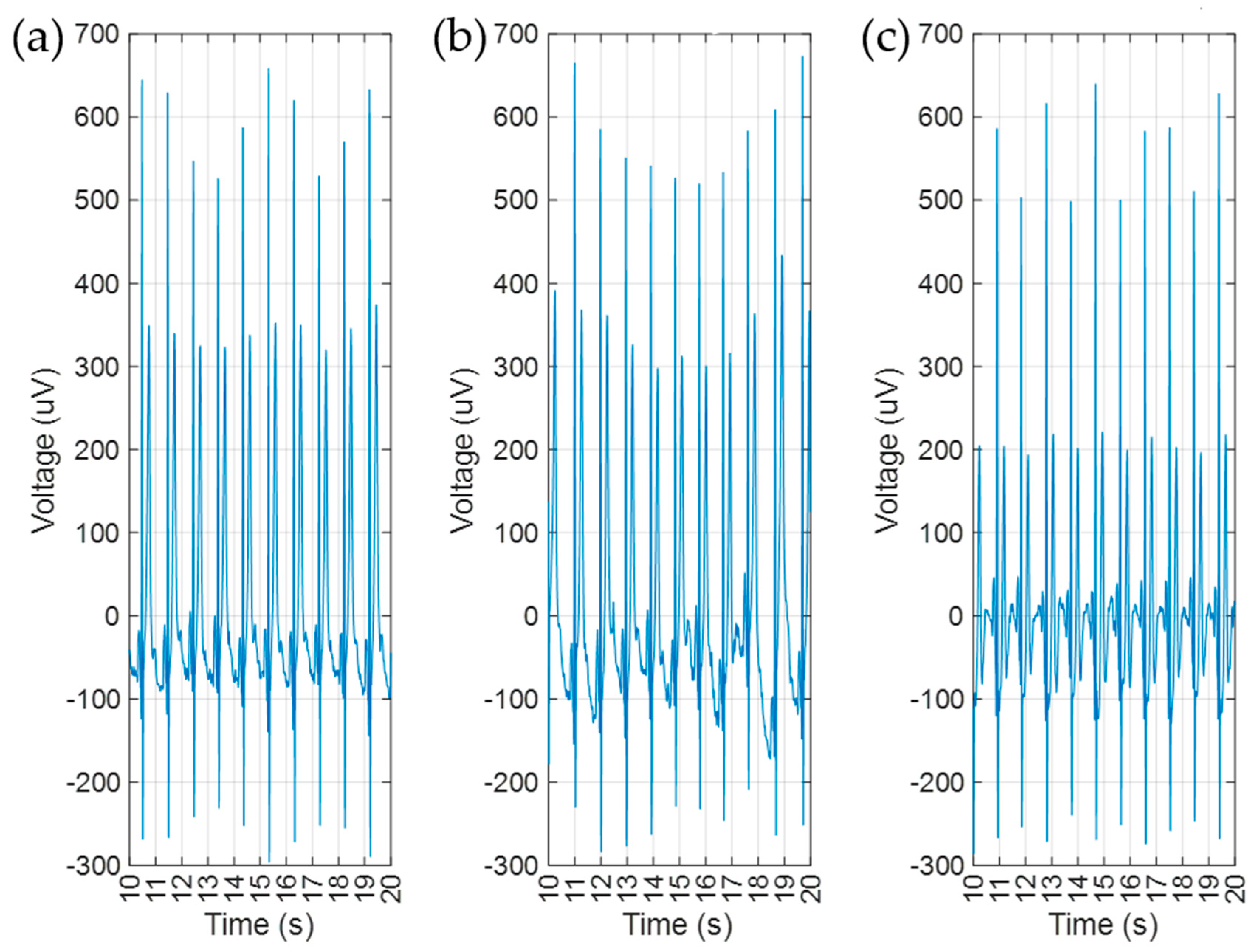
3.2. ECG on the Volunteer
Figure 3 shows 10 s ECG snapshots of 1 min measurements using the dry knitted contacts as implemented in Figure 1b during normal, fast and slow breathing. Typical signal parameters were extracted in MATLAB, as given in Table 4. In Figure 3, we observe that the amplitude of the R-peaks (the peaks with the largest amplitude) is modulated by the breathing signal. Breathing in, increases the resistance of the chest and breathing out decreases it. The breathing rate associated to this modulation is similar to that reported in Table 3.
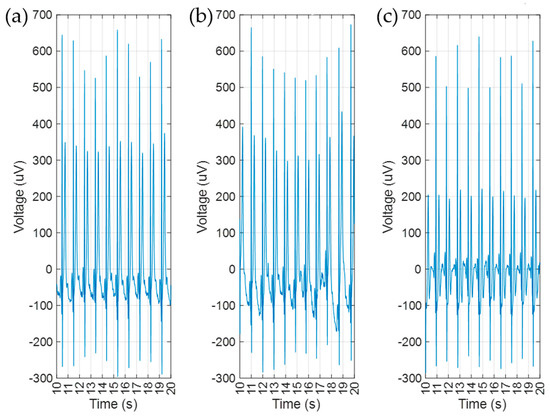
Figure 3.
10 s ECG recordings for (a) normal, (b) deep and (c) fast breathing. All recorded using dry knitted electrodes.

Table 4.
ECG parameters. R: distance between R-peaks, σ: standard variation on the R-peak position and HR: heart rate in beats per second (bps).
4. Conclusions
Knitted RIP sensors and ECG electrodes were implemented in a garment and were used to record breathing and ECG signals simultaneously. This implementation gave good quality recordings and health parameters in a relatively relaxed fitting garment when the wearer sat still.
Author Contributions
Conceptualization, K.F.; methodology, K.F., C.P. and G.H.; software, K.F. and G.H.; validation, K.F.; formal analysis, K.F.; investigation, K.F. and C.P.; resources, K.F.; data curation, K.F. and C.P.; writing—original draft preparation, K.F.; writing—review and editing, C.P.; visualization, K.F.; supervision, K.F.; project administration, K.F.; funding acquisition, K.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study as the dataset is not related to clinical trials.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data can be requested from K.F.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Liang, A.; Stewart, R.; Bryan-Kinns, N. Analysis of Sensitivity, Linearity, Hysteresis, Responsiveness, and Fatigue of Textile Knit Stretch Sensors. Sensors 2019, 19, 3618. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Ali, S.; Wijekoon, J.; Hugh Gong, R.; Fernando, A. A wearable piezo-resistive sensor for capturing cardiorespiratory signals. Sens. Actuators A Phys. 2018, 282, 215–229. [Google Scholar] [CrossRef]
- Ngo, H.T.; Nguyen, C.V.; Nguyen, T.M.H.; Van Vo, T. A Portable Respiratory Monitor Using Respiratory Inductive Plethysmography. In Proceedings of the 4th International Conference on Biomedical Engineering in Vietnam, Ho Chi Minh City, Vietnam, 8–12 January 2012; IFMBE Proceedings. Springer: Berlin/Heidelberg, Germany, 2013; Volume 49. [Google Scholar] [CrossRef]
- Le, K.; Narayana, H.; Servati, A.; Bahi, A.; Soltanian, S.; Servati, P.; Ko, F. Electronic textiles for electrocardiogram monitoring: A review on the structure–property and performance evaluation from fiber to fabric. Text. Res. J. 2022, 1–33. [Google Scholar] [CrossRef]
- Fobelets, K. Knitted coils as breathing sensors. Sens. Actuators A Phys. 2020, 306, 111945. [Google Scholar] [CrossRef]
- Fobelets, K.; Panteli, C.; Hammour, G. E-knits for bio-signal recordings. In Proceedings of the 4th International e-Textiles Conference, Nottingham, UK, 9–10 November 2022. [Google Scholar]
- Kiener, K.; Anand, A.; Fobelets, W.; Fobelets, K. Low Power Respiration Monitoring Using Wearable 3D Knitted Helical Coils. IEEE Sens. J. 2022, 22, 1374–1381. [Google Scholar] [CrossRef]
- Panteli, C.; Fobelets, K. Complementary cross-coupled LC oscillator for Respiratory Inductive Plethysmography readout. In Proceedings of the 4th International e-Textiles Conference, Nottingham, UK, 9–10 November 2022. [Google Scholar]
- Shieldex®. Available online: https://www.shieldex.de/en/products_categories/fibers-yarns/ (accessed on 18 January 2023).
- Euler, L.; Guo, L.; Persson, N.-K. Textile Electrodes: Influence of Knitting Construction and Pressure on the Contact Impedance. Sensors 2021, 21, 1578. [Google Scholar] [CrossRef] [PubMed]
- Low-Cost Biosensing Starter Kit|OpenBCI. Available online: https://openbci.com/ (accessed on 30 November 2022).
- Kniterate|The Digital Knitting Machine. Available online: https://www.kniterate.com/ (accessed on 30 November 2022).
- EcoKnitware. Available online: https://ecoknitware.com/ (accessed on 30 November 2022).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).