Abstract
The integration of smart medical devices (SMDs) driven by artificial intelligence (AI) and the internet of medical things (IoMT) is revolutionizing healthcare through improved diagnostics and continuous monitoring. However, their deployment raises significant ethical concerns, including patient safety, data privacy, informed consent, fairness, bias, and regulatory compliance. This paper presents a structured prioritization framework that assesses these ethical considerations according to their severity, contextual impact, and relevance to clinical practice. The usefulness of this prioritization lies in its ability to guide stakeholders to focus on high-impact areas, ensuring that resources and interventions address the most critical ethical risks first. Targeted mitigation strategies support the application of this framework in practice. By aligning innovation with ethical responsibility, this approach promotes safer, fairer, and more reliable healthcare solutions. This ultimately enables the sustainable and socially responsible integration of SMDs into modern medical systems.
1. Introduction
Today, smart medical devices (SMDs) play a crucial role in the progress of digitalization and automation of healthcare ecosystem, further contributing to improved diagnosis and alleviate the burden on medical professionals. More importantly, these smart devices support patient benefit and well-being by providing better access to health information, as well as through continuous monitoring of symptoms and facilitating real-time surveillance [1]. SMDs incorporate up-and-coming technologies, such as the internet of medical things (IoMT) and artificial intelligence (AI) [2]. The World Health Organization (WHO) emphasizes the pivotal role of SMDs in seamlessly integrating long-term healthcare into patients’ everyday routines [3]. Furthermore, the WHO underscores how technology-assisted solutions reduce healthcare costs by preventing hospital readmissions, decreasing emergency room visits, and minimizing unnecessary testing and treatments [4]. In recent years, the field of SMDs has witnessed remarkable progress, largely driven by the growing number of devices that are computerized and connected. Notably, the IoMT market was valued at over 44 USD billion in 2023 and is projected to grow at a compound annual growth rate (CAGR) of 21.2% over the next six years [5].
Various SMDs categorized by their applications, including wearable health monitors, remote patient monitoring, and health diagnosis systems, have been developed to gather data and process information for assessing health and tracking individualized therapy progress [6]. Additionally, social and physical assistance systems are being deployed to aid individuals in receiving timely help and support when needed. In the context of decision support systems, AI-driven tools have shown significant promise in enhancing clinical workflows and improving healthcare delivery [7]. For instance, the work in [8] presents a CNN-LSTM-based healthcare system integrating Apache Kafka, TensorFlow Serving, and federated learning for secure, real-time anomaly detection. It efficiently processes multimodal data, guaranteeing high accuracy, low latency, and strong privacy protection in distributed medical environments. Moreover, the exponential growth of real-time artificial intelligence aids a real-time AI system developed from EUS images effectively differentiates gastrointestinal stromal tumors from leiomyomas, with high accuracy and superior performance to endoscopists. Validated in multiple cohorts, it demonstrates a strong diagnostic performance, particularly for small lesions, improving clinical decision-making in gastrointestinal care [9]. In Ref. [10], this study presents an IoT-based knee-monitoring system using wearable IMUs and edge-cloud computing for telerehabilitation. Validated by hardware and exercise tests, it demonstrates accurate, efficient, and low-power performance, enabling remote and home rehabilitation with real-time feedback.
However, while their integration represents a transformative step forward, it also introduces significant risks, particularly concerning data accuracy and the potential for breaches of sensitive health information. Moreover, in the high-risk area of healthcare, mistakes can have severe consequences for the patient who is the victim of this error. As such, the deployment of SMDs demands thorough ethical considerations. Indeed, integrating AI and IoMT into healthcare in a responsible way depends on proactively addressing complex ethical challenges, including protecting patient privacy, ensuring robust data protection, clarifying liability frameworks, maintaining transparency in algorithmic decision-making, promoting equitable access and outcomes, and maintaining human agency in care decisions. Finding a compromise between innovation and ethical responsibility is essential, as these smart devices only have transformative potential if their deployment prioritizes patient safety, cultivates equity, and fosters trust between individuals, medical practitioners, and communities. Thoughtfully addressing these challenges will not only mitigate risks but also pave the way for sustainable advances that combine technological progress with societal values and human dignity.
This study examines the complex ethical challenges associated with the integration of SMDs into healthcare through a discussion of their dual roles as transformative tools and sources of risk. It highlights the critical need for dynamic ethical guidelines to govern their deployment, balancing innovation and accountability. By proposing practical strategies at the institutional level, the research attempts to guide the ethical adoption of SMDs in an era of rapid technological progress. The following sections examine the ethical implications of AI and IoMT, assessing their respective relative relevance in healthcare systems. The main contribution of this study lies in the systematic prioritization of ethical concerns, such as privacy, fairness, responsibility, and human agency, according to their societal, clinical, and systemic implications. This approach aims to enable stakeholders to address high-impact issues first, fostering trust and ensuring that technological advances are consistent with the core values of safe, equitable, and patient-centered care.
2. Ethical Considerations in AI and IoMT
As the healthcare sector harnesses the revolutionary potential of AI and IoMT, it must navigate an intricate ethical landscape shaped by rapid technological advancement. These innovations promise to redefine patient care through enhanced diagnostics, personalized treatments, and real-time health monitoring, while optimizing operational efficiency across hospitals and clinics. Yet, their integration into healthcare systems introduces profound ethical dilemmas that demand rigorous scrutiny, proactive governance, and multidisciplinary collaboration. Hereby, we explore the ethical dimensions to ensuring that AI and IoMT serve as forces for good, balancing their transformative potential with societal values, patient rights, and long-term sustainability.
Figure 1 encapsulates the multifaceted ethical landscape surrounding the integration of AI and the IoMT in healthcare. These technologies promise transformative advancements, yet their deployment demands rigorous ethical scrutiny to ensure they align with societal values, patient rights, and global sustainability goals. Below is a comprehensive interpretation of the interconnected ethical domains and their implication. The radar chart visualizes ethical considerations for AI-based and IoMT-based systems in healthcare, comparing how each aligns with key ethical dimensions.
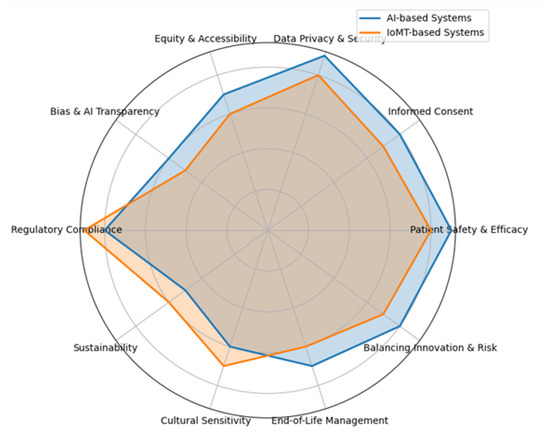
Figure 1.
Ethical considerations for AI and IoMT in Healthcare.
AI and IoMT technologies present distinct ethical considerations across key domains. AI scores higher in areas such as patient safety and efficacy due to its central role in diagnosis, decision-making, and predictive modeling, which have direct impacts on patient outcomes. It also raises heightened concerns around informed consent and bias, as patients must understand complex algorithmic decisions, and underrepresented groups risk unfair treatment if training data lacks diversity. In contrast, IoMT excels in regulatory compliance and sustainability, as it involves numerous hardware components subject to strict approval processes and environmental concerns. Both technologies share high stakes in data privacy and security, particularly due to the sensitive nature of health data and widespread connectivity. Equity and accessibility remain pressing for both, though AI may pose greater challenges if algorithmic deployment fails to account for marginalized groups.
Cultural sensitivity, end-of-life management, and innovation risk are also crucial, with AI typically facing greater scrutiny due to its autonomy, while IoMT raises concerns about device access and lifecycle ethics.
3. Prioritizing Ethical Considerations in the Integration of AI and IoMT-Based SMDs
The utility of this prioritization framework lies in its ability to guide healthcare stakeholders, such as developers, clinicians, policymakers, and regulatory bodies, in making informed, ethical decisions throughout the lifecycle of SMDs. Categorizing ethical concerns based on severity, real-world risks, and potential mitigation strategies helps identify which issues demand immediate attention and resource allocation. For example, prioritizing patient safety, data privacy, and informed consent ensures that foundational principles of medical ethics are upheld, thereby reducing harm and fostering trust. Additionally, it enables proactive planning for moderate or context-dependent issues like cultural sensitivity or sustainability by integrating ethical foresight into design and deployment. This structured approach enhances transparency, accountability, and inclusivity in digital health innovation, ultimately supporting safer, fairer, and more socially responsible technology adoption in healthcare systems.
The Table 1 provides a comprehensive overview of the ethical challenges associated with SMDs powered by AI and IoMT, systematically evaluating each consideration based on its application, severity, risks, and mitigation strategies. High-priority concerns such as patient safety, informed consent, and data privacy highlight the urgent need for secure design, transparent communication, and robust Cybersecurity, as failures in these areas can result in life-threatening outcomes. Moderate to high risks include bias, equity, and regulatory compliance, where algorithmic discrimination and unequal access can undermine fairness and effectiveness, necessitating inclusive datasets, explainable AI, and regulatory alignment. Context-dependent issues like sustainability, cultural sensitivity, and end-of-life management reflect the importance of adaptability and local engagement to ensure ethical alignment with societal values and environmental responsibility. The table ultimately serves as a strategic guide for healthcare stakeholders, enabling them to prioritize high-impact ethical domains while fostering responsible and equitable innovation.

Table 1.
Structured application of ethical considerations to SMDs mapped to their severity.
4. Conclusions
In conclusion, AI and IoMT in healthcare have immense potential to revolutionize patient care and healthcare delivery. However, their responsible and ethical use depends on considering the multifaceted considerations described in this manuscript, particularly through the conscious prioritization of competing values and goals. By focusing on patient well-being, transparency, fairness, and equitable resource allocation, stakeholders can find complex trade-offs, such as balancing innovation and safety, efficiency and privacy, or scalability and personalization of care. Healthcare systems, technologists, policymakers and professionals must work together to establish clear ethical hierarchies, ensuring that key priorities such as patient safety and efficacy, societal benefit, and harm mitigation guide decision-making.
As we move forward, the ethical pathway for AI and IoMT must remain dynamic. Continuous reflection, adaptation, and strategic prioritization will be essential to harness the full potential of these technologies while preserving well-being and trust. In the ever-changing healthcare landscape, ethics and intentional prioritization must remain central, so that AI and IoMT serve as tools for empowerment and healing. Only by rigorously prioritizing ethical imperatives can we ensure that these advances equitably benefit individuals and society now and in the future.
Author Contributions
Conceptualization, M.E.A. and A.A.; methodology, M.E.A.; validation, A.E.F., I.Y.M. and S.E.M.; formal analysis, A.A.; investigation, M.E.A.; resources, I.Y.M.; writing—original draft preparation, M.E.A.; writing—review and editing, A.E.F., I.Y.M. and S.E.M.; visualization, A.A.; supervision, S.E.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing is not applicable to this paper, as no datasets were generated or analyzed during the current study.
Acknowledgments
The authors gratefully acknowledge the support and collaboration of all institutions and laboratories involved in this research. We extend our sincere thanks to colleagues, technical staff, and administrative personnel who contributed their expertise and assistance throughout the course of this study.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| SMD | Integration of Smart Medical Device |
| AI | Artificial Intelligence |
| IoMT | Internet of Medical Thing |
| WHO | World Health Organization |
| CAGR | Compound Annual Growth rate |
| CNN | Convolutional Neural Network |
| LSTM | Long Short-Term Memory |
| IMU | Inertial Measurement Unit |
| FDA | Food and Drug Administration. |
| MDR | Medical Device Regulation. |
References
- Fernández-Alemán, J.L.; Señor, I.C.; Lozoya, P.Á.O.; Toval, A. Security and privacy in electronic health records: A systematic literature review. J. Biomed. Inform. 2013, 46, 541–562. [Google Scholar] [CrossRef] [PubMed]
- Obermeyer, Z.; Powers, B.; Vogeli, C.; Mullainathan, S. Dissecting racial bias in an algorithm used to manage the health of populations. Science 2019, 366, 447–453. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Integrated Care for Older People: Guidelines on Community-Level Interventions to Manage Declines in Intrinsic Capacity; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- World Health Organization. Ageism in Artificial Intelligence for Health; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Internet of Medical Things (IoMT) Market–Size, Share & Trends Analysis Report. Available online: https://www.grandviewresearch.com/industry-analysis/internet-of-medical-things-iomt-market-report (accessed on 16 October 2025).
- Zarif, A. The ethical challenges facing the widespread adoption of digital healthcare technology. Health Technol. 2022, 12, 175–179. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kumar, Y.; Koul, A.; Singla, R.; Ijaz, M.F. Artificial intelligence in disease diagnosis: A systematic literature review, synthesizing framework and future research agenda. J. Ambient Intell. Humaniz. Comput. 2023, 14, 8459–8486. [Google Scholar] [CrossRef] [PubMed]
- Nagamani, G.M.; Kumar, C.K. Design of an improved graph-based model for real-time anomaly detection in healthcare using hybrid CNN-LSTM and federated learning. Heliyon 2024, 10, e41071. [Google Scholar] [CrossRef] [PubMed]
- Dong, Z.; Zhao, X.; Zheng, H.; Zheng, H.; Chen, D.; Cao, J.; Xiao, Z.; Sun, Y.; Zhuang, Q.; Wu, S.; et al. Efficacy of real-time artificial intelligence-aid endoscopic ultrasonography diagnostic system in discriminating gastrointestinal stromal tumors and leiomyomas: A multicenter diagnostic study. EClinicalMedicine 2024, 73, 102656. [Google Scholar] [CrossRef] [PubMed]
- El Fezazi, M.; Achmamad, A.; Jbari, A.; Jilbab, A. IoT-based System using IMU Sensor Fusion for Knee Telerehabilitation. Monit. IEEE Sens. J. 2025, 25, 11906–11914. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).