Abstract
Beyond being painful, fat stigma might facilitate pernicious consequences; over and above one’s weight, fat stigma is associated with lesser wellbeing, poorer health, greater all-cause mortality, and weight gains that perpetuate the weight-stigma cycle. To combat fat stigma effectively requires an understanding of the perceptual calculus underlying it. Here, we seized upon new work asserting that importance of a previously overlooked variable in this calculus—fat deposition location (body shape)—and we examine basic but fundamental open questions about the role of body shape in fat stigma via two experiments (one pre-registered). We replicate and extend work investigating how body shape—over and above body size—drives stigma toward women, using a figure set created specifically to test predictions about the role of body shape as well as size. We asked: (1) Are findings of greater explicit stigma toward adult women with abdominal (gut) versus gluteofemoral fat depositions (hips, thighs, buttocks) replicated—and (2) does this same finding hold for implicit stigma?; (3) Are male targets similarly stigmatized as a function of shape? (4) Do individual difference factors known to predict anti-fat stigma, e.g., Protestant Work Ethic, play a role here? We examined these questions by presenting American participants with women and men targets varying in both body size and shape—assessing participants’ explicit stigma (via self-report) and implicit stigma (via the Attitude Misattribution Procedure; AMP). We replicated the pattern that explicit fat stigma toward women is shape-sensitive and extend that to implicit stigma—finding, for example, that, of two women with the same exact heights and higher weights, the woman with abdominal fat deposition is more stigmatized than the woman with gluteofemoral fat deposition. We found no consistent results regarding the role of body shape in driving fat stigma toward men. We also found that some individual difference factors predicting anti-fat stigma were also attuned to body shape as well as body size. The results underscore the importance of integrating body shape into future work on fat stigma (toward women).
1. The Role of Women’s and Men’s Body Shapes in Explicit and Implicit Fat Stigma
Fat stigma is pervasive, painful, yet remains comparatively more socially acceptable than most other stigmas. Related, in this work, we endeavor to use language that fosters scientific clarity and is also compassionate, but we also note that what is considered compassionate is both currently debated among researchers and activists, e.g., using “with obesity” may be considered best practice or considered medicalizing; see and may change in the future. Worldwide, approximately half a billion people with what we will often call “higher weights” are likely to face its negative effects. For example, heavier daughters receive less support for school from their parents, heavier patients receive poorer treatment from their doctors, and heavier people receive diminished economic opportunities from their employers [1,2,3,4,5,6,7,8,9]. Moreover, regardless of one’s weight, fat stigma itself is linked to negative outcomes, including lowered psychological wellbeing, greater all-cause mortality, and, insidiously, weight gain, e.g., via increased eating, production of obesenogenic hormones, that perpetuate the weight-stigma cycle [8,10,11,12,13,14,15]. These myriad harms have motivated researchers to create an international consensus statement that calls for the end of fat stigma [16].
To combat fat stigma, however, we must understand the perceptual calculus that produces it. Here, we seize upon new work that asserts that importance of a previously overlooked variable critical to this calculus—fat deposition location—and address basic, fundamental but open questions about the role of body shape in fat stigma [17].
2. What We Know about the Role of Shape in Fat Stigma
For decades, most social psychological work on fat stigma has focused, understandably, on the role of fat amount (body size) in driving fat stigma. Across target gender, ethnicity, age, and society, social perceivers stigmatize heavier targets more [14]. These robust findings seem to have given rise to some implicit theoretical assumptions—that, in the eyes of social perceivers, all fat is equally “bad”, and more fat is always “worse” (for reviews, see [18]. Nevertheless, new work reveals that, at least for women, body shape is an important driver of fat stigma.
Integrating research in evolutionary anthropology and biomedicine, Krems and Neuberg [17] made and supported straightforward predictions about the role of body size and shape in fat stigma toward women. In brief, fat located on the gut is associated with the negative outcomes people commonly think about when they think about “obesity”, e.g., Type 2 diabetes, cardiovascular issues [19], and thus social perceivers view this fat deposition pattern particularly negatively. By contrast, across cultures, women with lower waist-to-hip ratios (i.e., less abdominal and more gluteofemoral fat) are viewed as more sexually and romantically attractive [20,21], suggesting that even higher-weight women with fat deposition might be somewhat buffered from fat stigma and possibly even preferred to “healthy-weight” or “underweight” women in some instances. Krems and Neuberg [17] found that, across nations, people tended to stigmatize women with “overweight” or “obesity” and fat primarily in their hips and thighs (gluteofemoral fat) less than same-weight women with their fat primarily in the gut area (abdominal fat). Further, people also tended to stigmatize women less when they had obesity and gluteofemoral fat than when they had overweight with abdominal fat. Taken together, those findings not only pointed out the critical importance of integrating body shape for understanding fat stigma, but also challenged some implicit theoretical assumptions in existing work—that social perceivers view all fat as equally bad and always view more fat as worse.
3. What Remains Unknown about the Role of Shape in Fat Stigma
Because body shape has been largely overlooked in existing research, several fundamental questions about its role in fat stigma remain open. Here, in addition to attempting to replicate the findings described above, we test several of these questions in two well-powered studies with U.S. participants (one preregistered).
Fat Stigma, Body Shape, and Men
Predictions about the role of fat deposition location in fat stigma toward men are less straightforward than those for women. On one hand, there is no reason to suspect that negative views of abdominal fat would be unique to women targets, implying that people might strongly stigmatize higher-weight men with abdominal fat. On the other hand, some work has found that men with “extra” abdominal fat are sometimes viewed favorably—specifically, as better parents [22]. Additionally, when men gain weight, they are unlikely to distribute it gluteofemorally; such a fat deposition pattern is associated with women and female hormones. Thus, the sex/gender-atypicality of being a higher-weight man with gluteofemoral fat might evoke greater stigmatization. We investigate (1) the role of men’s body size in explicit and implicit stigma directed toward them.
We also (2) explore the role of body shape in implicit fat stigma. Work exploring this has tended to focus on explicit fat stigma. But especially in the last decades, a growing number of researchers have used paradigms such as the Implicit Association Test (IAT, [23]) or the Attitude Misattribution Procedure (AMP; [24]) to explore implicit fat stigma [25,26,27,28,29,30,31].
Explicit and implicit stigma are conceptually distinct [32,33]. Most notably, explicit stigma is considered consciously acknowledged, and it is thus aptly measured via self-report. (We use self-report measures here.) By contrast, implicit stigma is thought to reflect evaluations that people are unable or unwilling to explicitly report, e.g., that participants are not conscious of, and it thus requires performance-based measures to assess, such as the IAT or AMP. We use the AMP here and describe that procedure in detail below.
Additionally, explicit attitudes may reflect internalization of wider sociocultural attitudes, whereas implicit attitudes may reflect exposure to those attitudes [34]. For example, both dieters and non-dieters implicitly stigmatized fatness, but dieters, who presumably more strongly internalized anti-fat attitudes, engaged in more explicit stigmatization [33]. Notably, researchers sometimes find little or no association among explicit and implicit measures of stigma [35,36,37]. For example, Teachman and Brownell (2001) [32] found that health professionals specializing in the treatment of people with heavy weight did not report explicit fat stigma, but nevertheless revealed their biases via implicit measures [30]. Yet other researchers have found significant associations between explicit and implicit stigma [38]. Furthermore, some work has specifically found positive relationships between explicit and implicit fat stigma [25,26,27,28,29], such that people more strongly stigmatized targets with higher weights or Body Mass Indices (BMIs)—both explicitly and implicitly.
To the best of our knowledge, however, no work has yet explored whether implicit fat stigma is sensitive to women’s (or men’s) body shapes as well as sizes. Here, we use the AMP to investigate whether implicit stigma follows the same shape-sensitive pattern of explicit fat stigma in previous work—that, for example, two women targets that are overweight are differently stigmatized when one has fat primarily in her abdomen and the other in her hips and thighs.
We also explore (3) several individual difference measures known to be associated with anti-fat attitudes: (a) Perceived Vulnerability to Disease (PVD [39]), which is positively associated with fat stigma, and (b) the Three Domain Disgust Scale (TDDS [40,41]), which tracks sensitivity to pathogen, sexual, and moral disgust, with pathogen disgust linked to increased weight bias. In past work, people scoring more highly on these dimensions also reported greater fat stigma toward targets with increasing weights or BMIs. However, figural targets used in past work have not varied in body shape as well as size. To the extent that, in the eyes of social perceivers, abdominal fat is more strongly associatedwith pathogens or poor-health [19,42]—whether consciously or not—then people higher in PVD and pathogen disgust should hold greater fat stigma toward targets with abdominal fat. We also assess (c) the Protestant Work Ethic (PWE), captured by the notion that ‘anyone who works hard can succeed,’ and which is positively associated with fat stigma [3,42]; and (d) participant Body Mass Index (BMI). With respect to the BMI, some evidence suggests that, unlike members of some other stigmatized groups, higher BMI people can also hold strong anti-fat attitudes [3,43,44,45,46]. However, robust research—which also included more people representing a higher range of BMIs—found that, whereas people of all BMIs held significant anti-fat bias, anti-fat bias was attenuated among participants with increasing BMIs [29]. We tested the extent to which these measures were correlated with stigma toward targets varying in body size and shape.
4. Open Practices
The data and the preregistration plan are available on the Open Science Framework (OSF) [47]. The BODSS Figure set is also available on the OSF [48].
5. Studies 1 and 2
5.1. Method
5.1.1. Study 1 Participants
One hundred and ninety-five participants were recruited to the study “Person Perception” on Amazon Mechanical Turk (MTurk) via TurkPrime in exchange for a small monetary compensation. Exclusion criteria primarily consisted of AMP-related concerns [24,49,50,51,52,53]: participants (n = 23) with an average reaction time (RT) less than 200 milliseconds (ms) were immediately excluded. Additionally, because the AMP requires that participants evaluate Chinese characters (as part of a distractor task), participants (n = 10) who indicated an ability to read Chinese were excluded, as were those reporting that they did not follow instructions. Lastly, we excluded two participants because they had an average RT +/− 3 SDs above the sample mean (M = 902.18, SD = 407.87).
This resulted in a final sample of 160 participants (81 females, 77 males, 2 non-binary/other; Mage = 36.61, SD = 10.59) completing focal outcome measures. This yields 0.80 power to detect small focal effects (f = 0.07) with 0.5 correlation among repeated measures and 0.95 non-sphericity correction. No additional data were collected after analyses, and all measures are reported. All Study 1 and Study 2 data were collected in 2018 and 2019.
5.1.2. Study 2 Participants
Two hundred and twenty undergraduates from a large Southern university participated for a partial course credit. As in Study 1, participants were excluded if they had an average RT +/− 3 SDs above the sample mean (n = 3; M = 1102.33, SD = 327.37), indicated an ability to read Chinese (n = 4), and/or if they indicated that they did not follow instructions (n = 38). This resulted in a final sample of 169 participants (98 females, 77 males; Mage = 19.42, SD = 2.48) completing focal outcomes measures. This final sample size slightly exceeded the 156 participants recommended by an a priori power analysis (G*Power) to detect our interactions of interest, based on 0.80 power to detect small effects (η2p = 0.02) assuming 0.2 correlation between measures. A sensitivity analysis conducted yielded 0.80 power (a = 0.05) to detect small focal effects (f = 0.09) with a 0.95 non-sphericity correction. No additional data were collected after analyses, and all measures are reported.
5.2. Procedure
Informed consent was obtained from all subjects involved in the study. Similar procedures were used in both Studies 1 and 2.
For Study 1, all procedures were conducted using the web-version of Inquisit 5.0 software (Millisecond Software, 2017). After consenting to the study, participants completed the AMP to assess implicit fat stigma toward female targets. The AMP is described in detail below. Immediately following the AMP, participants were given an initial demographics questionnaire asking about their age, sex, sexual orientation, relationship status, and AMP-related manipulation checks. Next, participants completed an explicit measure of fat stigma. Participants then completed individual difference measures, supplied their weights (in pounds) and heights (in feet and inches) to calculate BMI, and were then asked to select the target that best resembled their own body shape from a range of male or female targets from the BODy Size and Shape (BODSS) figure set [48], described in detail below.
Study 2 differed in that the AMP was conducted using the lab-based version of Inquisit 5.0 and used both female and male targets. After the AMP was completed, a research assistant opened a Qualtrics survey link for the participant to complete the remainder of the study, following Study 1.
5.3. Materials
Stimuli. To assess how both body fat amount (body size) and fat deposition location (body shape) affect stigma, we used the BODy Size and Shape (BODSS) figure set [17]. The BODSS is a newer figure set containing male and female targets varying in life stage (i.e., age). These line-drawn, forward-facing figures depict, for example, men and women roughly at the peaks of their reproductive careers (who look to be ~18–28) as well as men and women likely to be engaged in parenting (who look to be ~30–40). For each sex-age tranche, e.g., reproductively- or parenting-aged men or women, there are several figures that vary not only in body size—underweight, “healthy”- or “average”-weight, overweight, and obese—but, importantly, that vary in body shape as well. That is, the higher-weight figures have systematically varying fat deposition location. Specifically, each sex-age tranche of the BODSS contains two “overweight” targets depicted as being the same BMIs but that have fat concentrated in either abdominal (gut) region or the gluteofemoral (hips and thighs) region. Three obese figures again have the same BMIs but have variously abdominal, gluteofemoral, and global (fat in both places) depositions. See Figure 1 for an example. Following past work, we used the reproductively-aged (~18-year-old) female and male figures. However, following best practices related to the AMP, we additionally used the parenting-aged (~35-year-old) female and male targets to increase the number of targets. The use of reproductively- and parenting-aged targets was simply to increase the number of trials.
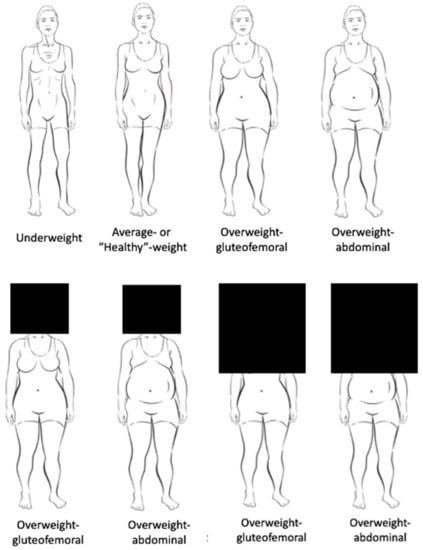
Figure 1.
Example stimuli from the BODSS figure set, with the top row depicting four adult (“reproductively-aged”) women targets: underweight, average-weight, overweight-gluteofemoral, overweight-abdominal. In the present studies, figure faces and/or faces-and-chests were blacked out (i.e., covered by square black boxes) to focus participants on the bodies. Respective examples are given in the bottom row.
Explicit Fat Stigma. In Study 1, participants viewed and responded to five female targets (healthy-weight, overweight targets with gluteofemoral and abdominal fat, and obese targets with gluteofemoral and abdominal fat) with the face and chest obscured, and the same targets with only the face obscured. In work assessing fat stigma as a function of target size and shape, Krems and Neuberg [17] used the BODSS figures with the faces blacked out to focus participants on the bodies. Thus, other features of the target’s body, e.g., the presence/absence and type of breasts, may have influenced fat stigma ratings. Here, we extend this work by examining explicit stigma toward targets that either had only the face obscured (as in previous work) or targets with both the face and chest obscured. If we found the same patterns of results with either depiction mode, this would suggest that fat stigma ratings were not strongly calibrated to the targets’ chests, but rather to their abdominal versus gluteofemoral fat, as expected. We largely found this expected pattern, and report this in detail in the Supplementary Material available online, and we discuss these results briefly in the Discussion. Within each type (chest and face obscured, face obscured), the presentation order of the individual targets was randomized.
In Study 2, participants viewed all seven reproductively-aged female targets—the previous five, and (a) an “underweight” female target and (b) a globally “obese” female target—and all seven reproductively-aged male targets. As in Study 1, participants rated targets with both the face and chest obscured, followed by the targets with only the face obscured. Whether the participants first saw female or male targets was randomized.
In both Studies 1 and 2, consistent with previous work [17], participants indicated how positive and negative they felt toward each target using a 1 (not at all) to 7 (very) Likert-type scale, one for positive, one for negative feelings, respectively. Participants were instructed: “Below, you will see a 26-year-old (female/male). Please rate how (positively/negatively) you feel about this person”. We used 26-year-old” as a description because (a) that is consistent with past work [17], which we attempted to replicate here, and (b) the AMP calls for use of more figures than exist in any one sex-age tranche, thus, we were forced to use both those figures seemingly 18–28 years old and those 30–40 years old. Luckily, the ages of these particular targets might be especially cued by their facial rather than body features, which means that participants can plausibly view all such targets as being about 26 years of age. We calculated an explicit stigma rating toward each target by subtracting the negative rating from the positive rating, such that ratings of zero indicate neutrality toward targets, higher scores indicate more favorable feelings toward targets, and lower scores indicate greater stigmatization of targets.
Implicit Fat Stigma. We used the AMP to measure implicit fat stigma toward targets. In general, the AMP is an indirect measure of affect, which capitalizes on principles of misattribution [54]. In a standard AMP task, participants are presented a prime image, e.g., a target of experimental interest, and then that prime image is immediately followed by a Chinese pictograph. Participants are instructed to ignore the prime image and to then rate the pleasantness of the pictograph. Although the pictographs should be relatively ambiguous and non-valenced to American participants, past work has found that the affect towards the prime image tends to be misattributed to that Chinese pictograph. Thus, it measures implicit stigma by capturing affect toward a prime image that is misattributed to a neutral target image.
In Study 1, participants rated the same five reproductively-aged female targets as from the explicit task (with only faces obscured), as well as parenting-aged (~35 years-old) versions of the same five figure types (with only faces obscured). Again, these additional targets were included in the AMP to increase the number of stimuli, following best practices [50,51]. Each target was presented four times and was randomly paired with a unique Chinese pictograph, resulting in 40 experimental trials.
In Study 2, we used all seven female and all seven male targets—both seven reproductively-aged and seven parenting-aged—all with only faces obscured. As in Study 1, each target image was presented four times and was randomly paired with a unique Chinese pictograph, resulting in 112 experimental trials. The AMP trials for female and male trials were done separately, and the order was counterbalanced.
Prior to completing the experimental trials, participants were given instructions that explained the AMP procedure and completed 10 practice trials. Participants were then shown the instructions for the task once again before proceeding. Participants were instructed to make their responses as quickly and accurately as possible. The entire procedure was displayed on a black screen with white text. Following common AMP procedures [24], for a single trial, a cue (+) was presented at the center of the screen for 150 ms, followed by a randomly selected target (prime) image for 75 ms, followed by blank screen for 125 ms, followed by a Chinese pictograph for 100 ms, followed by a visual mask (i.e., black and white “static”) with instructions to rate the Chinese pictograph as “unpleasant” or “pleasant” using the “E” and “I” keys, respectively. The visual mask remained on the screen until a response was made, and following a response, the next trial began.
For each AMP trial, a response of “unpleasant” was scored as 0, and a response of “pleasant” was scored as 1 [24]. A proportion score for the number of “pleasant” responses was then calculated separately for each type of target, e.g., healthy-weight reproductive-aged female, overweight-gluteofemoral reproductive-aged female, with lower scores indicating greater implicit fat stigma.
Individual Differences Linked to Fat Stigma. Participants completed three individual difference scales, each positively correlated with anti-fat attitudes [3,41,55,56,57]: (1) the 15-item Perceived Vulnerability to Disease scale (PVD) assessed chronic concerns about the acquisition and transmission of pathogens [55]. It contains two subscales that measure one’s perceived infectability (α = 0.87; e.g., “In general, I am very susceptible to colds, flu and other infectious diseases”) and aversion to germs (α = 0.69; e.g., “It really bothers me when people sneeze without covering their mouths”). Responses were made using a 1 (Strongly disagree) to 5 (Strongly agree) Likert-type scale.
(2) The 21-item Three Domain Disgust Scale (TDDS) measured sensitivity to three types of disgust (each containing seven items) [57]. The domains of disgust were pathogen (α = 0.76; e.g., “Sitting next to someone who has red sores on their arm”), sexual (α = 0.85; e.g., “Watching a pornographic video”), and moral (α = 0.85; e.g., “Deceiving a friend”), and were all rated using a 0 (Not at all disgusting) to 6 (Extremely disgusting) Likert-type scale.
Lastly, (3) the 19-item Protestant Work Ethic scale (α = 0.74; PWE) measured the extent to which participants value hard work and self-determination, e.g., “A distaste for hard work usually reflects a weakness of character” [3]. Responses were made using a −3 (I disagree strongly) to +3 (I agree strongly) scale.
In both studies, we also asked participants to provide their weight (in pounds) and height (in both feet and inches) to calculate their BMI.
Additional variables. We additionally assessed a number of exploratory individual difference variables (participant ecological circumstances, sociosexuality, age at puberty) not germane to focal hypotheses and not examined here. Additionally, participants identified one of the seven (male or female) target images that best resembled their own body size and shape; because we did not use these categorical responses in analyses, we do not describe this novel body/size shape scale further here.
6. Results
6.1. Does Shape Influence Fat Stigma toward Women?
Explicit Stigma. Yes; we largely replicated the pattern of work found in previous research [17]. Table 1 displays the means, standard deviations, and 95% confidence intervals for all explicit stigma analyses in Studies 1 and 2. Table 2 displays the omnibus effects the research questions focusing on how target shape and depiction affects explicit and implicit stigma in Studies 1 and 2.

Table 1.
Means (SDs) and 95% Confidence Intervals (CI) for Explicit Stigma Toward Female and Male Targets by Target View (Studies 1 and 2).

Table 2.
F-statistics for all analyses.
Women with Gluteofemoral Fat Are Buffered from Fat Stigma (Versus Same-BMI Women with Other Shapes). First, regardless of whether the target face or face and chest were obscured, both overweight and obese targets with gluteofemoral fat were buffered from stigma compared to the same-BMI females with abdominal (or global) fat depositions, replicating and extending past work [17]. See Figure 2 and Figure 3.
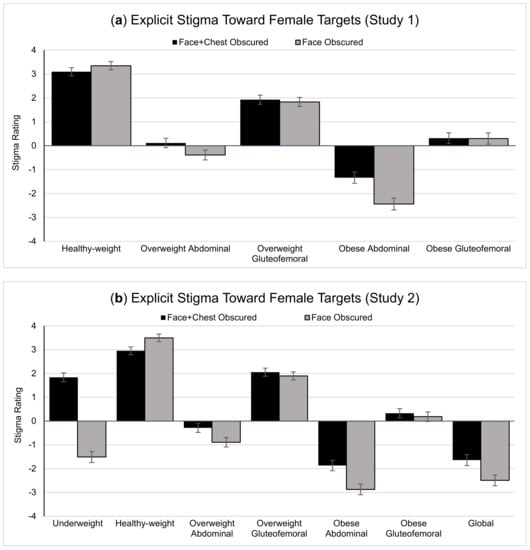
Figure 2.
Explicit fat stigma ratings toward female targets in (a) Study 1 and (b) Study 2. Error bars represent standard error. Note that lower numbers indicate more negative attitudes—or greater stigma—toward targets.
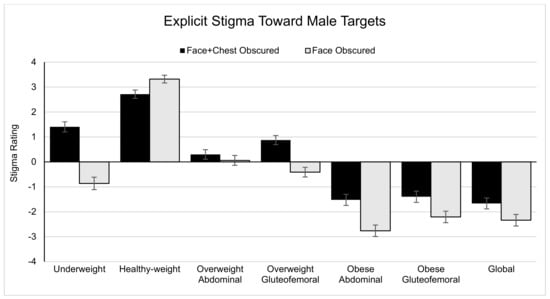
Figure 3.
Explicit fat stigma ratings toward male targets in Study 2. Error bars represent standard error. Note that lower numbers indicate more negative attitudes—or greater stigma—toward targets.
In Study 1, when the targets had faces and chests obscured, overweight targets with gluteofemoral fat were less stigmatized than overweight targets with abdominal fat (p < 0.001, d = 0.75), and when the targets had only the faces obscured, overweight targets with gluteofemoral fat were less stigmatized than overweight targets with abdominal fat (p < 0.001, d = 0.82). When obese targets had both faces and chests obscured, those with gluteofemoral fat were more stigmatized than those with abdominal fat (p < 0.001, d = 0.80). When obese targets had only the faces obscured, those with gluteofemoral fat were also less stigmatized than those with abdominal fat (p < 0.001, d = 1.04).
This was replicated in Study 2. When the targets had faces and chests obscured, overweight targets with gluteofemoral fat were less stigmatized than overweight targets with abdominal fat (p < 0.001, d = 0.97), and with only faces obscured, overweight targets with gluteofemoral fat were less stigmatized than overweight targets with abdominal fat (p < 0.001, d = 1.05). When obese targets had faces and chests obscured, targets with gluteofemoral fat were less stigmatized than both globally obese targets and targets with abdominal fat (pglobal < 0.001, d = 0.74; pabdominal < 0.001, d = 0.89). There was not a significant difference in stigma toward obese targets with global or abdominal fat (p = 0.154, d = 0.11). Similarly, when targets had only the faces obscured, targets with gluteofemoral fat were less stigmatized than globally obese targets (p < 0.001, d = 1.01), or obese targets with abdominal fat (p < 0.001, d = 1.18). Targets with abdominal fat were also more stigmatized than obese targets with global fat (p < 0.001, d = 0.29). This suggests that the presentation mode of figures (face-only v. face and chests obscured) may not be a hugely important factor in shaping fat stigma, and that fat deposition location is a robust, significant factor in the perceptual calculus of fat stigma.
Women Are Sometimes Stigmatized Less at Objectively Higher Weights. A second finding in previous work on fat stigma underscoring the importance of body shape is that people tended to stigmatize women less when they were obese with gluteofemoral fat than overweight with abdominal fat [17]. In Study 1, stigma did not significantly differ for this comparison when targets had faces and chests obscured (p = 0.274, d = 0.09), but did when targets had only the faces obscured; overweight targets with abdominal fat were more stigmatized than obese targets with gluteofemoral fat (p < 0.001, d = 0.30). In Study 2, we found this same pattern whether targets had faces and chests obscured (p < 0.001, d = 0.28) or only the faces obscured (p < 0.001, d = 0.50).
In Study 2, we replicated a third finding from previous work—that people tend to stigmatize the underweight figure more relative to the healthy-weight figure, again countering the notion that more fat is always more stigmatized [17]. When the targets had faces and chests obscured, underweight (versus healthy-weight) targets were more stigmatized (p < 0.001, d = 0.43), and this was replicated when targets had only the faces obscured (p < 0.001, d = 1.39).
Implicit stigma. We largely replicated the pattern of findings for explicit stigma toward women. Recall that all figures used in the implicit stigma task had only faces obscured. Table 3 displays the means, standard deviations, and 95% confidence intervals for all implicit stigma analyses in Studies 1 and 2. First, we replicated the finding that women are stigmatized less when carrying gluteofemoral versus abdominal fat, underscoring the importance of shape in understanding fat stigma, see Figure 4.

Table 3.
Means (SDs) and 95% Confidence Intervals (CI) for Implicit Stigma Toward Female and Male Targets by Target View (Studies 1 and 2).
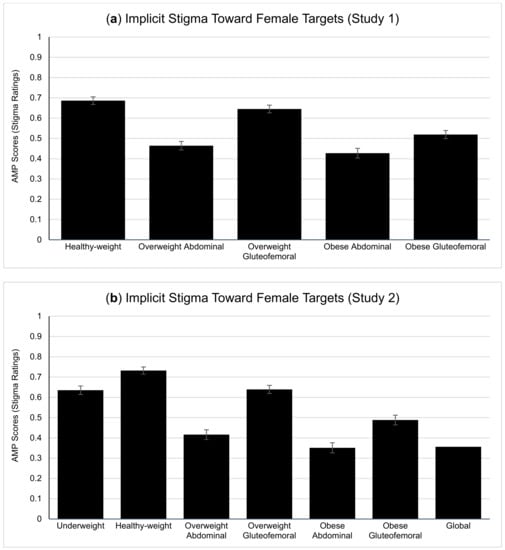
Figure 4.
Implicit fat stigma ratings toward female targets in (a) Study 1 and (b) Study 2. Error bars represent standard error. Note that lower numbers indicate more negative attitudes—or greater stigma—toward targets.
Women with Gluteofemoral Fat Are Buffered from Fat Stigma (Versus Same-BMI Women with Other Shapes). In Study 1, overweight targets with gluteofemoral fat were less stigmatized than overweight targets with abdominal fat (p < 0.001, d = 0.61), and obese targets with gluteofemoral fat were less stigmatized than obese targets with abdominal fat (p < 0.001, d = 0.36).
Similarly, in Study 2, overweight targets with gluteofemoral fat were less stigmatized than overweight targets with abdominal fat (p < 0.001, d = 0.60), and obese targets with gluteofemoral fat were less stigmatized than obese targets with abdominal fat (p < 0.001, d = 0.44) or global obesity (p < 0.001, d = 0.38). Globally obese targets did not differ from obese targets with abdominal fat (p = 0.771 d = 0.02).
Women Are Sometimes Stigmatized Less at Objectively Higher Weights. We again found that people tend to stigmatize women less—but here, implicitly—when they are obese with gluteofemoral fat then overweight with abdominal fat than, both in Study 1 (p = 0.046, d = 0.23) and in Study 2 (p = 0.001, d = 0.25).
In Study 2, we included an underweight figure and found that people tend to stigmatize the underweight figure relative to the healthy-weight figure (p < 0.001, d = 0.35), replicating our findings with explicit stigma.
6.2. Does Shape Influence Explicit Fat Stigma toward Men?
Explicit Stigma. Yes, but not in a manner as consistent as that for female targets (see Table 1 and Table 2, Figure 3).
When overweight targets had faces and chests obscured, those with abdominal fat were more stigmatized than those with gluteofemoral fat (p = 0.004, d = 0.22), a similar pattern to female targets; however, when targets had only the faces obscured, overweight targets with abdominal fat were less stigmatized than overweight targets with gluteofemoral fat (p = 0.025, d = 0.17), the reverse pattern. When obese targets had faces and chests obscured, stigma did not differ between those with abdominal or gluteofemoral fat (p = 0.431, d = 0.06), or between those with global versus gluteofemoral fat (p = 0.104, d = 0.13) or abdominal fat (p = 0.295, d = 0.08). When only faces were obscured, those with obesity and abdominal fat were more stigmatized than targets with gluteofemoral fat (p < 0.001, d = 0.31) or global fat (p = 0.010, d = 0.20). Ratings for targets did not differ when comparing gluteofemoral versus global fat (p = 0.409, d = 0.06). Whereas findings for female targets were straightforward and in line with a priori predictions—specifically, that women who were overweight or obese with gluteofemoral (versus abdominal) fat were buffered from stigma—we found that men with abdominal fat tended be more stigmatized, but the pattern of results was relatively inconsistent.
However, and supporting the proposition that more fat is not always more stigmatized and replicating findings for female targets, male targets were more stigmatized when underweight than healthy-weight, whether faces and chests were obscured (p < 0.001, d = 0.50) or only faces were obscured (p < 0.001, d = 1.15).
Implicit stigma. Overweight male targets were more stigmatized when carrying abdominal fat versus gluteofemoral fat (p < 0.001, d = 0.26). However, stigma did not significantly differ between obese targets with depositions (p = 0.202), although globally obese targets were more stigmatized than obese targets with gluteofemoral fat (p = 0.049, d = 0.15), but did not differ from obese targets with abdominal fat (p = 0.590, d = 0.04). Again, no single clear pattern emerged for male targets (see Table 3, Figure 5). Although implicit stigma ratings of female targets did not differ between the reproductively and parenting-aged targets, we found that these two groups differed in minor ways for male targets. See Supplemental Materials for complete information on these analyses.
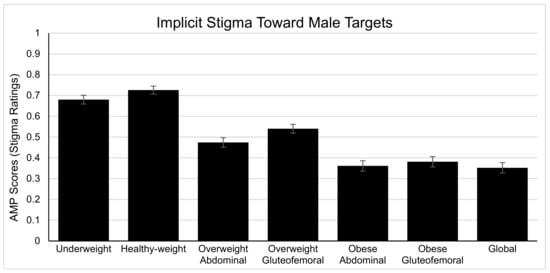
Figure 5.
Implicit fat stigma ratings toward male targets in Study 2. Error bars represent standard error. Note that lower numbers indicate more negative attitudes—or greater stigma—toward targets.
6.3. Links between Explicit and Implicit Stigma?
We examined the relationship between explicit and implicit stigma, as these may be conceptually distinct [32,58,59,60,61,62,63]. See Table 4 for all relationships in Studies 1 and 2.

Table 4.
Bivariate Correlations Between Implicit and Explicit Stigma Ratings (Studies 1 and 2).
Results from Study 1 indicated that explicit and implicit stigma ratings of female targets were significantly and positively correlated for targets that were overweight (p = 0.013) and obese with abdominal fat (p = 0.019). The correlation was marginally significant for targets that were obese gluteofemoral fat (p = 0.085). No other relationships were statistically significant (ps > 0.132). In Study 2, all the explicit and implicit stigma ratings of female targets were significantly and positively correlated (ps < 0.020), except for ratings of the healthy-weight target (p = 0.210).
For male targets, the results indicate that all of the explicit and implicit stigma ratings of male targets were significantly and positively correlated (ps < 0.035), except for the ratings of the healthy-weight (p = 0.263) and overweight with abdominal fat targets (p = 0.127); the correlation was marginally significant for underweight targets (p = 0.071).
Across both studies, and for both female and male targets, the correlations were small to medium in size—effect sizes consistent with what is typically observed for implicit-explicit associations [58,59,60,61,62], especially for the AMP [60].
6.4. Does Target Gender Influence Stigma?
Explicit Stigma. Yes. A 2 (Target gender: female, male) × 2 (Target view: faces and chests obscured, only faces obscured) × 7 (Target shape) ANOVA on data from Study 2 (wherein male targets were included) revealed a significant three-way interaction (see Table 5 for omnibus effects for these analyses). When the targets had faces and chests obscured, male targets were more stigmatized than female targets that were overweight with gluteofemoral fat (p < 0.001, d = 0.43) or obese with gluteofemoral fat (p < 0.001, d = 0.62), possibly underscoring the role of such fat in social perceptions of female (but not male) attractiveness [20,21]. Conversely, female targets were more stigmatized than male targets when they were overweight with abdominal fat (p < 0.001, d = 0.31) or obese with abdominal fat (p = 0.039, d = 0.13), perhaps indicating greater fat stigma toward women in general and/or some buffering toward men with this fat deposition [8,22]. Ratings of globally obese targets did not differ by target gender (p = 0.921, d = 0.01).

Table 5.
F-statistics for Analyses Testing Whether Target Gender Influences Stigma (Study 2).
This same general pattern was observed when only faces were obscured. Male targets were more stigmatized than female targets when overweight with gluteofemoral fat (p < 0.001, d = 0.89) or obese with gluteofemoral fat (p < 0.001, d = 0.90). Conversely, female targets were more stigmatized than male targets when they were overweight with abdominal fat (p < 0.001, d = 0.39) but not obese with abdominal fat (p = 0.288, d = 0.09). Ratings of globally obese targets again did not differ by target gender (p = 0.317, d = 0.07).
Implicit Stigma. A 2 (Target gender: female, male) × 7 (Target shape) ANOVA revealed a significant two-way interaction (see Table 5). Recall that all figures used for implicit stigma had only faces obscured. Consistent with patterns for explicit stigma, male targets were more stigmatized than female targets when overweight with gluteofemoral fat (p < 0.001, d = 0.31) or obese with gluteofemoral fat (p < 0.001, d = 0.33). Conversely, female targets were more implicitly stigmatized than male targets when they were overweight with abdominal fat (p = 0.007, d = 0.21) but not obese with abdominal fat (p = 0.516, d = 0.05). Ratings of globally obese targets did not differ by target gender (p = 0.829, d = 0.02).
6.5. Individual Differences in Explicit and/or Implicit Stigma?
We also examined whether individual differences in factors associated with fat stigma in previously work were correlated with our measures of explicit or implicit fat stigma. We included participant BMI, two sub-scales of Perceived Vulnerability to Disease (PVD; perceived infectability, germ aversion), each of the three sub-scales of the Three Domain Disgust Scale (TDDS; pathogen disgust, sexual disgust, moral disgust), and Protestant Work Ethic (PWE). See Table 6.

Table 6.
Bivariate Correlations Between BMI, PVD, TDDS, PWE, and Explicit and Implicit Stigma Toward Female and Male Targets (Studies 1 and 2).
To briefly summarize the major findings, it seems that participants with higher BMI were less stigmatizing (explicitly and implicitly) of higher-weight female or male targets, consistent with past findings [29].
We also observed that participants who perceived themselves to be less infectable to disease (a subscale of PVD) were less explicitly stigmatizing of female or male targets with overweight, replicating past work [39], though these effects were quite small. Participants with higher levels of germ aversion (a subscale of PVD) were more implicitly (but not explicitly) stigmatizing of higher-weight male targets, though findings were inconsistent for female targets.
However, the most consistent correlate of fat stigma outcomes was the pathogen disgust subscale of the TDDS [41]. Participants who reported they were less pathogenic disgusted were less explicitly stigmatizing of overweight and obese targets but more implicitly stigmatizing of these same targets. This held for both female and male targets.
Correlations between stigma toward female of male targets and the TDDS sexual and moral disgust subscales as well as the PWE were inconsistent.
7. Discussion
Decades of research in social psychology have revealed that higher-weight people routinely and consistently face pernicious, painful fat stigma [16,18], but recent work suggests that fat stigma is not merely a function of target fat amount; that is, the perceptual calculus of fat stigma is highly attuned to fat deposition locations or body shape, as well [17]. Here, we replicated and extended this initial work on body shape work in several novel ways.
First, we replicated findings from previous work [17] showing that (a) women who were overweight or obese with gluteofemoral (versus abdominal) fat are relatively buffered from explicit fat stigma, (b) women who were overweight with abdominal fat were more stigmatized than objectively higher-weight women who were obese with gluteofemoral fat, and (c) women were stigmatized more when underweight versus healthy-weight. As with the original work, these replications suggest the importance of taking shape into account to understand fat stigma and challenge assumptions perhaps implicit in traditional work on fat stigma—that social perceivers always view all fat as equally bad and more fat as worse.
Second, we extended this work on the importance of shape in fat stigma toward men. Whereas predictions and findings were straightforward for female targets, this was not the case for male targets. There was no consistent pattern of shape affecting fat stigma toward men. However, we did again see that males were more stigmatized when underweight than healthy-weight, a pattern also seen for women here and elsewhere [17], which again suggests that more mass is not always viewed as worse.
Ancillary to this, we addressed a possible limitation of previous work by exploring explicit stigma toward targets that had only faces obscured, to focus participants on bodies (as in previous work), or had faces and chests obscured, given that the breasts on targets with gluteofemoral versus abdominal fat are depicted somewhat differently. Most notably, we found the predicted pattern of stigma toward female targets for both depiction modes (with faces and chests versus only faces obscured), suggesting that the depiction of the chest area alone is not driving the past or present results dealing with fat stigma toward women. There were no straightforward results for male targets. For detailed analyses, see the Supplementary Materials.
Third, we conducted one of the first tests of the role of body shape in implicit fat stigma and were thus able to explore the extent to which such explicit and implicit fat stigma are related. For stigma toward women, implicit stigma followed the same pattern as explicit stigma—higher-weight women with gluteofemoral versus abdominal fat were less stigmatized, women were more stigmatized when overweight and carrying abdominal fat than when obese and carrying gluteofemoral fat, and when underweight versus healthy-weight. Again, no single clear pattern emerged for the role of shape driving implicit stigma toward men.
Related, we also found that, for both female and male targets, explicit and implicit stigma were correlated with small-to-medium effect sizes. This is consistent with effect sizes observed for explicit-implicit associations [41,58,59,60,61], especially for the AMP [59]. Our use of the same target images for explicit and implicit measurement conferred the benefit of structural fit in that the attitude-object (i.e., stimulus) was held constant. However, the different ways in which we measured explicit (i.e., Likert-type scale) and implicit stigma (i.e., forced-choice) may have also attenuated the size of a true relationship [62]. That there is some significant and positive relationship between these forms of stigma makes some sense; implicit stigma might reflect sociocultural attitudes and explicit stigma might reflect internalization of these attitudes, and there is no reason to suspect that sociocultural attitudes or their internalization are not equally attuned to body shape. Thus, these observed relationships may reflect true differences in the two forms of fat stigma, as explicit and implicit stigma may be conceptually distinct, arise from distinct processes, and predict different behavioral outcomes [33,34,63,64,65,66]. Although it remains to be seen if these two stigma instantiations lead to different behavioral outcomes.
Because we included both female and male targets, we were also able to examine differences in fat stigma as a function not only of target body size and shape, but also of target gender. Whereas existing work suggests that, in general, heavier targets are more stigmatized, regardless of target gender [38], we found that this pattern is shape sensitive. Here, we tended to see that higher-weight women with abdominal fat tended to be more stigmatized than same-BMI women with gluteofemoral fat, but the reverse for men. This (a) underscores the role of gluteofemoral fat depositions in buffering fat stigma toward women and (b) might also suggest that fat stigma may be driven, in part, by the gender-typicality of fat depositions, with more female-typical gluteofemoral fat evoking greater stigma for men and what might be somewhat more male-typical abdominal fat evoking greater stigma for women.
8. Limitations and Future Directions
Whereas this work is among the first to explore several basic open questions about the role of body fat amount and deposition location in driving fat stigma, there remain a number of limitations and questions ripe for future work. First, one might ask why we failed to find consistent effects of body shape for men. In line with others [17,67,68], we would not assert that shape is irrelevant for men. However, compared to women, men have greater muscle mass, and women have greater fat mass than men do. Thus, fat stigma toward men might be especially attendant to the amount of men’s muscle mass, a variable we did not manipulate here.
Additionally, predictions about the role of body shape in fat stigma toward women benefitted from understanding the functionality and social perceptions of different fat on different parts of women’s bodies, drawing on the anthropological literature [20,69]. Taking a similar tack for men also seems to imply that muscle mass plays a role in the social perceptions of men [67,70,71]. For example, higher-weight men with some muscle mass, e.g., Tony Soprano, might be deemed more masculine and desirable than higher-weight men with little muscle mass, e.g., George Costanza [67], and thus buffered from fat stigma. Future work on the role of male shape in fat stigma might do well take into account muscle as well as fat mass and deposition [67]. Whereas previous figural sets have manipulated body size and muscularity [68], and the BODSS figure set is among the first to systematically vary fat amount and deposition, none have integrated fat amount, fat deposition, and muscularity. However, male figures recently added to the BODSS now additionally vary muscle mass, making them useful for future research in this vein.
Our samples consisted of Americans; thus, one might wonder whether findings here are specific to this population [72,73,74]. For fat stigma toward women, at least, this is unlikely; the pattern of results found here for explicit stigma replicate findings among White and Black Americans and Indian participants [17], and the novel findings for implicit stigma follow the same predicted pattern as those for explicit stigma. However, given that explicit and implicit stigma are conceptually distinct, it remains an open question whether implicit fat stigma toward women might vary across cultures. To the extent that implicit stigma happens outside of awareness and/or because individuals are motivated to deny these responses, e.g., to appear fair-minded, we might expect that implicit fat stigma might vary as a function of the cultural value of appearing non-prejudiced toward higher-weight individuals.
There is also reason to suspect some cultural variation in fat stigma toward men. Some “extra” abdominal fat on male bodies might perhaps cue a man’s ability to access resources—a primary feature that women desire in prospective male partners across cultures [75,76]. (To the extent that males’ fat amount, deposition, and muscle mass might all have similar cue-value for social perceivers aiming to infer a man’s ability to acquire resources, it is possible that each of these features are components driving fat stigma.) For example, rural Gambian men with higher BMIs had more wives and surviving children than did lower-BMI men [71]. The value of this ability, cued by more abdominal fat—might be greater in societies where resources are scarcer and/or contested, further suggesting that men with greater fat would be less stigmatized in such societies.
Finally, we focused on big, open questions about fat stigma here, showing that fat stigma—at least toward women—is highly sensitive not only to body size but also to body shape. Whereas these questions are of basic theoretical interest, they also have practical implications for future work and intervention. In particular, we suggest that future research should reexamine patterns of explicit and implicit fat stigma—and their respective consequences, e.g., discrimination—among consequential populations, such as medical professionals, teachers, parents, and others whose routine interactions with and prejudice toward higher-weight people can have real, lasting effects [29,76,77,78,79,80]. For example, higher-weight individuals might forgo routine medical care to avoid the stigma of medical professionals, and parents might withhold support for higher-weight children’s education [2,4,7]. If the stigma underlying these negative outcomes is also sensitive to target shape, then interventions might do well to take target shape into account when assessing and/or implementing these prejudice reduction tactics [75].
Supplementary Materials
The following supporting information can be accessed at https://osf.io/3zd7a/.
Author Contributions
Conceptualization, methodology, writing—original draft preparation; writing—review and editing: J.A.K. and J.E.B. Supervision; project administration: J.A.K. Formal analysis; investigation; data curation; visualization: J.E.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank OCEAN RA Jade House for her help with references.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Brewis, A.A.; Wutich, A. Explicit versus implicit fat-stigma. Am. J. Hum. Biol. 2012, 24, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Crandall, C.S. Do Parents Discriminate against Their Heavyweight Daughters? Pers. Soc. Psychol. Bull. 1995, 21, 724–735. [Google Scholar] [CrossRef]
- Crandall, C.S. Prejudice against fat people: Ideology and self-interest. J. Pers. Soc. Psychol. 1994, 66, 882–894. [Google Scholar] [CrossRef] [PubMed]
- Foster, G.D.; Wadden, T.A.; Makris, A.P.; Davidson, D.; Sanderson, R.S.; Allison, D.B.; Kessler, A. Primary Care Physicians’ Attitudes about Obesity and Its Treatment. Obes. Res. 2003, 11, 1168–1177. [Google Scholar] [CrossRef]
- Hatzenbuehler, M.L.; Phelan, J.C.; Link, B.G. Stigma as a Fundamental Cause of Population Health Inequalities. Am. J. Public Health 2013, 103, 813–821. [Google Scholar] [CrossRef]
- Janssen, I.; Craig, W.M.; Boyce, W.F.; Pickett, W. Associations Between Overweight and Obesity with Bullying Behaviors in School-Aged Children. Pediatrics 2004, 113, 1187–1194. [Google Scholar] [CrossRef]
- Kenrick, A.C.; Shapiro, J.R.; Neuberg, S.L. Do Parental Bonds Break Anti-fat Stereotyping?: Parental Work Ethic Ideology and Disease Concerns Predict Bias Against Heavyweight Children. Soc. Psychol. Personal. Sci. 2013, 4, 721–729. [Google Scholar] [CrossRef]
- Puhl, R.M.; Heuer, C.A. The Stigma of Obesity: A Review and Update. Obesity 2009, 17, 941–964. [Google Scholar] [CrossRef]
- Sjöberg, R.L.; Nilsson, K.W.; Leppert, J. Obesity, Shame, and Depression in School-Aged Children: A Population-Based Study. Pediatrics 2005, 116, e389–e392. [Google Scholar] [CrossRef]
- Brewis, A.; Sturtzsreetharan, C.; Wutich, A. Obesity stigma as a globalizing health challenge. Glob. Health 2018, 14, 20. [Google Scholar] [CrossRef]
- Jackson, S.E.; Beeken, R.J.; Wardle, J. Perceived weight discrimination and changes in weight, waist circumference, and weight status. Obesity 2014, 22, 2485–2488. [Google Scholar] [CrossRef] [PubMed]
- Major, B.; Hunger, J.M.; Bunyan, D.P.; Miller, C.T. The ironic effects of weight stigma. J. Exp. Soc. Psychol. 2014, 51, 74–80. [Google Scholar] [CrossRef]
- Major, B.; Tomiyama, A.J.; Hunger, J.M. The negative and bidirectional effects of weight stigma on health. In The Oxford Handbook of Stigma, Discrimination, and Health; Oxford University Press: Oxford, UK, 2018; Volume 556, pp. 499–519. [Google Scholar]
- Puhl, R.M.; Brownell, K.D. Psychosocial origins of obesity stigma: Toward changing a powerful and pervasive bias. Obes. Rev. 2003, 4, 213–227. [Google Scholar] [CrossRef]
- Tomiyama, A.J.; Carr, D.; Granberg, E.M.; Major, B.; Robinson, E.; Sutin, A.R.; Brewis, A. How and why weight stigma drives the obesity “epidemic” and harms health. BMC Med. 2018, 16, 123. [Google Scholar] [CrossRef]
- Rubino, F.; Puhl, R.M.; Cummings, D.E.; Eckel, R.H.; Ryan, D.H.; Mechanick, J.I.; Nadglowski, J.; Ramos Salas, X.; Schauer, P.R.; Twenefour, D.; et al. Joint international consensus statement for ending stigma of obesity. Nat. Med. 2020, 26, 485–497. [Google Scholar] [CrossRef] [PubMed]
- Krems, J.A.; Neuberg, S.L. Updating Long-Held Assumptions About Fat Stigma: For Women, Body Shape Plays a Critical Role. Soc. Psychol. Pers. Sci. 2021, 13, 70–82. [Google Scholar] [CrossRef]
- Diedrichs, P.C.; Puhl, R. Weight bias: Prejudice and discrimination toward overweight and obese people. In The Cambridge Handbook of the Psychology of Prejudice; Sibley, C., Ed.; Cambridge University Press: Cambridge, UK, 2017; Volume 671, pp. 392–412. [Google Scholar]
- Jayedi, A.; Soltani, S.; Zargar, M.S.; Khan, T.A.; Shab-Biidar, S. Central fatness and risk of all cause mortality: Systematic review and doe-response meta-analysis of 72 prospective cohort studies. Br. Med. J. 2020, 370, m3324. [Google Scholar] [CrossRef]
- Lassek, W.D.; Gaulin, S.J.C. Do the Low WHRs and BMIs Judged Most Attractive Indicate Better Health? Evol. Psychol. 2018, 16, 147470491880399. [Google Scholar] [CrossRef] [PubMed]
- Lassek, W.D.; Gaulin, S.J.C. Do the Low WHRs and BMIs Judged Most Attractive Indicate Higher Fertility? J. Evol. Psychol. 2018, 16, 1474704918800063. [Google Scholar] [CrossRef]
- Sacco, D.F.; Holifield, K.; Drea, K.; Brown, M.; Macchione, A. Dad and Mom Bods? Inferences of Parenting Ability from Bodily Cues. Evol. Psychol. Sci. 2020, 6, 207–214. [Google Scholar] [CrossRef]
- Nosek, B.A.; Greenwald, A.G.; Banaji, M.R. The Implicit Association Test at age 7: A methodological and conceptual review. In Social Psychology and the Unconscious: The Automaticity of Higher Mental Processes; Bargh, J.A., Ed.; Psychology Press: London, UK, 2006; pp. 265–292. [Google Scholar]
- Payne, B.K.; Cheng, C.M.; Govorun, O.; Stewart, B.D. An inkblot for attitudes: Affect misattribution as implicit measurement. J. Pers. Soc. Psychol. 2005, 89, 277–293. [Google Scholar] [CrossRef]
- Guedj, R.; Marini, M.; Kossowsky, J.; Berde, C.; Mateo, C.; Fleegler, E.W. Explicit and implicit bias based on race, ethnicity, and weight among pediatric emergency physicians. Acad. Emerg. Med. 2021, 28, 1073–1076. [Google Scholar] [CrossRef] [PubMed]
- Sabin, J.A.; Maddalena, M.; Nosek, B.A. Implicit and explicit anti-fat bias among a large sample of medical doctors by BMI, race/ethnicity and gender. PLoS ONE 2012, 7, e48448. [Google Scholar] [CrossRef]
- Nosek, B.A.; Hawkins, C.B.; Frazier, R.S. Implicit social cognition: From measures to mechanisms. Trends Cogn. Sci. 2011, 15, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Nosek, B.A.; Hawkins, C.; Frazier, R.S. Implicit social cognition. Soc. Cogn. 2012, 31–53. [Google Scholar]
- Fitzgerald, C.; Hurst, S. Implicit bias in healthcare professionals: A systematic review. BMC Med. Ethic 2017, 18, 19. [Google Scholar] [CrossRef]
- Schwartz, M.B.; Vartanian, L.; Nosek, B.; Brownell, K.D. The Influence of One’s Own Body Weight on Implicit and Explicit Anti-fat Bias. Obesity 2006, 14, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, M.B.; Chambliss, H.O.; Brownell, K.D.; Blair, S.N.; Billington, C. Weight Bias among Health Professionals Specializing in Obesity. Obes. Res. 2003, 11, 1033–1039. [Google Scholar] [CrossRef]
- Teachman, B.; Brownell, K. Implicit anti-fat bias among health professionals: Is anyone immune? Int. J. Obes. 2001, 25, 1525–1531. [Google Scholar] [CrossRef]
- Rudman, L.A. Sources of Implicit Attitudes. Curr. Dir. Psychol. Sci. 2004, 13, 79–82. [Google Scholar] [CrossRef]
- Marini, M.; Sriram, N.; Schnabel, K.; Maliszewski, N.; Devos, T.; Ekehammar, B.; Wiers, R.; HuaJian, C.; Somogyi, M.; Shiomura, K.; et al. Overweight People Have Low Levels of Implicit Weight Bias, but Overweight Nations Have High Levels of Implicit Weight Bias. PLoS ONE 2013, 8, e83543. [Google Scholar] [CrossRef] [PubMed]
- Vartanian, L.R.; Herman, C.P.; Polivy, J. Implicit and explicit attitudes toward fatness and thinness: The role of the internalization of societal standards. Body Image 2005, 2, 373–381. [Google Scholar] [CrossRef]
- Greenwald, A.G.; Banaji, M.R. Implicit social cognition: Attitudes, self-esteem, and stereotypes. Psychol. Rev. 1995, 102, 4. [Google Scholar] [CrossRef]
- Marini, M. Underweight vs. overweight/obese: Which weight category do we prefer? Obes. Sci. Pract. 2017, 3, 390–398. [Google Scholar] [CrossRef]
- Robertson, N.; Vohora, R. Fitness vs. fatness: Implicit bias towards obesity among fitness professionals and regular exercisers. Psychol. Sport Exerc. 2008, 9, 547–557. [Google Scholar] [CrossRef]
- Brochu, P.; Morrison, M.A. Implicit and Explicit Prejudice Toward Overweight and Average-Weight Men and Women: Testing Their Correspondence and Relation to Behavioral Intentions. J. Soc. Psychol. 2007, 147, 681–706. [Google Scholar] [CrossRef]
- Park, J.H.; Schaller, M.; Crandall, C.S. Pathogen-avoidance mechanisms and the stigmatization of obese people. Evol. Hum. Behav. 2007, 28, 410–414. [Google Scholar] [CrossRef]
- Tybur, J.M.; Lieberman, D.; Griskevicius, V. Microbes, mating, and morality: Individual differences in three functional domains of disgust. J. Pers. Soc. Psychol. 2009, 97, 103–122. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, D.L.; Tybur, J.M.; Latner, J.D. Disgust Sensitivity, Obesity Stigma, and Gender: Contamination Psychology Predicts Weight Bias for Women, Not Men. Obesity 2012, 20, 1803–1814. [Google Scholar] [CrossRef]
- Han, S.-J.; Zaretsky, A.G.; Andrade-Oliveira, V.; Collins, N.; Dzutsev, A.; Shaik, J.; da Fonseca, D.M.; Harrison, O.J.; Tamoutounour, S.; Byrd, A.L.; et al. White Adipose Tissue Is a Reservoir for Memory T Cells and Promotes Protective Memory Responses to Infection. Immunity 2017, 47, 1154–1168.e6. [Google Scholar] [CrossRef] [PubMed]
- Katz, I.; Hass, R.G. Racial ambivalence and American value conflict: Correlational and priming studies of dual cognitive structures. J. Pers. Soc. Psychol. 1988, 55, 893. [Google Scholar] [CrossRef]
- Allison, D.B.; Basile, V.C.; Yuker, H.E. The measurement of attitudes toward and beliefs about obese persons. Int. J. Eat. Disord. 1991, 10, 599–607. [Google Scholar] [CrossRef]
- Rudman, L.A.; Feinberg, J.; Fairchild, K. Minority Members’ Implicit Attitudes: Automatic Ingroup Bias as a Function of Group Status. Soc. Cogn. 2002, 20, 294–320. [Google Scholar] [CrossRef]
- Wang, S.S.; Brownell, K.D.; A Wadden, T. The influence of the stigma of obesity on overweight individuals. Int. J. Obes. 2004, 28, 1333–1337. [Google Scholar] [CrossRef] [PubMed]
- Open Science Framework. Available online: https://osf.io/3zd7a/ (accessed on 24 October 2018).
- Open Science Framework. Available online: https://osf.io/tvrb8/ (accessed on 24 October 2018).
- Payne, B.K.; Brown-Iannuzzi, J.; Burkley, M.; Arbuckle, N.L.; Cooley, E.; Cameron, C.D.; Lundberg, K.B. Intention invention and the affect misattribution procedure: Reply to Bar-Anan and Nosek (2012). Pers. Soc. Psychol. Bull. 2013, 39, 375–386. [Google Scholar] [CrossRef]
- Gawronski, B.; Ye, Y. What drives priming effects in the affect misattribution procedure? Pers. Soc. Psychol. Bull. 2014, 40, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.; Gawronski, B. Validating the semantic misattribution procedure as an implicit measure of gender stereotyping. Eur. J. Soc. Psychol. 2018, 48, 348–364. [Google Scholar] [CrossRef]
- Magallares, A. Predictors of Social Distance Toward People with Obesity: The Role of Allophilia. Int. Rev. Soc. Psychol. 2017, 30, 102–110. [Google Scholar] [CrossRef]
- Millisecond Software 2017, Millisecond: Seattle, WA, USA, 2017.
- Neuberg, S.; Krems, J. The BODy Size and Shape (BODSS) Figure Set. OSF 2016. [Google Scholar] [CrossRef]
- Payne, K.; Lundberg, K. The Affect Misattribution Procedure: Ten Years of Evidence on Reliability, Validity, and Mechanisms. Soc. Pers. Psychol. Compass 2014, 8, 672–686. [Google Scholar] [CrossRef]
- Duncan, L.A.; Schaller, M.; Park, J.H. Perceived vulnerability to disease: Development and validation of a 15-item self-report instrument. Pers. Individ. Differ. 2009, 47, 541–546. [Google Scholar] [CrossRef]
- van Leeuwen, F.; Hunt, D.; Park, J.H. Is Obesity Stigma Based on Perceptions of Appearance or Character? Theory, Evidence, and Directions for Further Study. Evol. Psychol. 2015, 13, 1474704915600565. [Google Scholar] [CrossRef]
- Bar-Anan, Y.; Nosek, B.A. A comparative investigation of seven indirect attitude measures. Behav. Res. Methods 2014, 46, 668–688. [Google Scholar] [CrossRef]
- Bar-Anan, Y.; Vianello, M. A multi-method multi-trait test of the dual-attitude perspective. J. Exp. Psychol. Gen. 2018, 147, 1264–1272. [Google Scholar] [CrossRef] [PubMed]
- Cameron, C.D.; Brown-Iannuzzi, J.L.; Payne, B.K. Sequential priming measures of implicit social cognition: A meta-analysis of associations with behavior and explicit attitudes. Pers. Soc. Psychol. 2012, 16, 330–350. [Google Scholar] [CrossRef]
- Greenwald, A.G.; Poehlman, T.A.; Uhlmann, E.L.; Banaji, M.R. Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. J. Pers. Soc. Psychol. 2009, 97, 17–41. [Google Scholar] [CrossRef]
- Oswald, F.L.; Mitchell, G.; Blanton, H.; Jaccard, J.; Tetlock, P.E. Predicting ethnic and racial discrimination: A meta-analysis of IAT criterion studies. J. Pers. Soc. Psychol. 2013, 105, 171–192. [Google Scholar] [CrossRef]
- Gawronski, B.; Hahn, A. Implicit measures: Procedures, use, and interpretation. In Measurement in Social Psychology; Blanton, H., LaCroix, J., Webster, G., Eds.; Taylor & Francis: Abingdon, UK, 2019; pp. 29–55. [Google Scholar]
- Payne, B.K.; Burkley, M.A.; Stokes, M.B. Why do implicit and explicit attitude tests diverge? The role of structural fit. J. Pers. Soc. Psychol. 2008, 94, 16–31. [Google Scholar] [CrossRef]
- Bessenoff, G.R.; Sherman, J.W. Automatic and Controlled Components of Prejudice toward Fat People: Evaluation versus Stereotype Activation. Soc. Cogn. 2000, 18, 329–353. [Google Scholar] [CrossRef]
- Devine, P.G. Stereotypes and prejudice: Their automatic and controlled components. J. Pers. Soc. Psychol. 1989, 56, 5. [Google Scholar] [CrossRef]
- Karpinski, A.; Hilton, J.L. Attitudes and the implicit association test. J. Pers. Soc. Psychol. 2001, 81, 774. [Google Scholar] [CrossRef]
- Frederick, D.A.; Haselton, M.G. Why Is Muscularity Sexy? Tests of the Fitness Indicator Hypothesis. Pers. Soc. Psychol. Bull. 2007, 33, 1167–1183. [Google Scholar] [CrossRef]
- Gray, P.B.; Frederick, D.A. Body image and body type preferences in St. Kitts, Caribbean: A cross-cultural comparison with US samples regarding attitudes towards muscularity, body fat, and breast size. Evol. Psychol. 2012, 10, 147470491201000319. [Google Scholar] [CrossRef]
- Brown, P.J.; Konner, M. An Anthropological Perspective on Obesity. Ann. N. Y. Acad. Sci. 1987, 499, 29–46. [Google Scholar] [CrossRef] [PubMed]
- Kirchengast, S. Differential reproductive success and body size in! Kung San people from northern Namibia. Coll. Antropol. 2000, 24, 121–132. [Google Scholar]
- Sear, R. Size-dependent reproductive success in Gambian men: Does height or weight matter more? Biodemogr. Soc. Biol. 2006, 53, 172–188. [Google Scholar] [CrossRef]
- Anderson, J.L.; Crawford, C.B.; Nadeau, J.; Lindberg, T. Was the Duchess of windsor right? A cross-cultural review of the socioecology of ideals of female body shape. Ethol. Sociobiol. 1992, 13, 197–227. [Google Scholar] [CrossRef]
- Crandall, C.S.; Schiffhauer, K.L. Anti-Fat Prejudice: Beliefs, Values, and American Culture. Obes. Res. 1998, 6, 458–460. [Google Scholar] [CrossRef]
- Buss, D.M. Toward an evolutionary psychology of human mating. Behav. Brain Sci. 1989, 12, 39–49. [Google Scholar] [CrossRef]
- Walter, K.V.; Conroy-Beam, D.; Buss, D.M.; Asao, K.; Sorokowska, A.; Sorokowski, P.; Zupančič, M. Sex differences in mate preferences across 45 countries: A large-scale replication. Psychol. Sci. 2020, 31, 408–423. [Google Scholar] [CrossRef]
- O'Brien, K.S.; Puhl, R.M.; Latner, J.D.; Mir, A.S.; Hunter, J.A. Reducing Anti-Fat Prejudice in Preservice Health Students: A Randomized Trial. Obesity 2010, 18, 2138–2144. [Google Scholar] [CrossRef] [PubMed]
- Phelan, S.M.; Dovidio, J.F.; Puhl, R.M.; Burgess, D.J.; Nelson, D.B.; Yeazel, M.W.; Hardeman, R.; Perry, S.; Van Ryn, M. Implicit and explicit weight bias in a national sample of 4,732 medical students: The medical student CHANGES study. Obesity 2014, 22, 1201–1208. [Google Scholar] [CrossRef] [PubMed]
- Teachman, B.A.; Gapinski, K.D.; Brownell, K.D.; Rawlins, M.; Jeyaram, S. Demonstrations of implicit anti-fat bias: The impact of providing causal information and evoking empathy. Health Psychol. 2003, 22, 68. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).