Abstract
Background: Liver biopsy performed after less invasive workup, including imaging, for evaluation of abnormal liver function studies occasionally reveals large bile duct obstruction on histology without evidence of biliary obstruction on prior imaging. The utility of ERCP in this setting has not been studied in pediatrics. In the present study, we address this important clinical issue. Methods: A retrospective review of pediatric pathology and clinical records from 2010 to 2019 identified 123 pediatric patients with large duct obstruction on liver biopsy performed after imaging revealed no evidence of biliary obstruction. The absolute standardized difference (ASD) was used to compare baseline covariates between patients who underwent ERCP vs. all others. Covariates included age, gender, race, ethnicity, BMI, and labs (total bilirubin, GGT, alkaline phosphatase, AST, ALT, platelets, and INR). Results: Of 85 unique patients who met inclusion/exclusion criteria, 15 (17.6%) underwent ERCP. The majority of these patients who underwent ERCP (80%) had a therapeutic endoscopic intervention with a favorable impact on clinical trajectory. The mean age of patients with large duct obstruction was 7 years old. Most patients were white (47%), followed by Asian (17%). Only 25% of patients identified as Hispanic. The mean laboratory values were as follows: total bilirubin 4.61 mg/dL, GGT 353 U/L, alkaline phosphatase 403 U/L, AST 343 U/L, ALT 251 U/L, platelets 289 K/uL, and INR 1.19. Absolute standardized differences comparing baseline covariates between the ERCP and non-ERCP groups are included in Table 1. The largest absolute standardized difference between the two groups was for race (1.17), ethnicity (0.553), and GGT (0.463). Age, alkaline phosphatase, and INR were not significantly different between the two groups (ASD <0.2 for both). Conclusions: Only 17.6% of pediatric patients with large ducts undergo ERCP. Pediatric patients who underwent ERCP were more likely to be white, non-Hispanic, and have elevated GGT. Of interest, age did not differ significantly between the two groups, which may reflect enhanced uniformity of utilization of ERCP across age groups in pediatrics. Additional multi-center studies, including more patients and focused on understanding the utility of ERCP and the range of outcomes following the diagnosis of large duct obstruction in pediatrics, would be informative to guide pediatric hepatology and endoscopic practices.
1. Introduction
Abnormal liver function tests (LFTs) are commonly encountered in pediatric clinical practice. Detection of LFT abnormalities typically prompts further laboratory and imaging studies to determine the underlying etiology leading to these abnormalities. Algorithms often recommend liver biopsy for patients with persistent, unexplained liver enzyme abnormalities, even if clinically asymptomatic [1]. In this context, liver histology has been found to be of high utility in both the diagnosis and management of patients with abnormal LFTs [2]. This practice extends to patients who have undergone liver transplantation, where cholestasis can result from allograft rejection or disruptions in bile flow, most commonly at the level of the biliary anastomosis, which may not be evident on imaging [3,4].
Large duct obstruction is diagnosed on liver biopsy in a substantial subset of patients in this clinical context. When large duct obstruction is identified on liver biopsy, the utility of additional invasive and high-risk procedures, such as endoscopic retrograde cholangiopancreatography (ERCP), has not been well studied, especially in the pediatric population. In both Europe and the United States, ERCP has been shown to be an effective and safe modality to treat biliary obstruction in all comers and biliary strictures after pediatric liver transplantation [5,6]. ERCP enables radiographic and direct visualization of the stricture, balloon dilatation, and stent placement. Still, ERCP is not without risk, and an established indication for ERCP is necessary given its associated adverse events, which include post-ERCP pancreatitis, cholangitis, pancreatitis, bleeding, perforation, and stent migration [7].
In this single-center retrospective study, we assess the clinical characteristics of pediatric patients who undergo ERCP when imaging reveals no evidence of biliary obstruction and a liver biopsy reveals large bile duct obstruction. Our clinical impression has been that ERCPs performed in this context have a positive impact on clinical trajectory, and this impression informs the hypothesis of this study. The hypothesis of this study is that, when performed, ERCP often reveals previously undetected biliary obstruction, which is amenable to endoscopic therapy. The goal of this initial study on the topic is to characterize tertiary care practice patterns when this clinical conundrum arises.
2. Methods
2.1. Study Design and Data Source
We performed a retrospective evaluation of pediatric patients with large duct obstruction on liver biopsy from 2010 to 2019 at our center, a major referral and transplant center in the Western United States. The study was approved by the Stanford IRB (Protocol # 45179, 52588). Inclusion criteria were all patients 18 years of age and under who underwent liver biopsy with pathology diagnosis of large duct obstruction from that liver biopsy and who had undergone pre-biopsy imaging, which did not reveal evidence of biliary obstruction. Patients whose liver biopsy was performed at the time of native liver explant were excluded from the analysis. For patients who had more than one liver biopsy, only the first liver biopsy demonstrating large duct obstruction was included in the analysis. Histologic diagnoses were rendered by subspecialized hepatobiliary pathologists using hematoxylin and eosin, trichrome, rhodanine, and diastase-predigested periodic acid–Schiff stains to assess for standard morphologic features of large duct obstruction, including portal edema, ductular proliferation, neutrophilic peri-cholangitis, canalicular/ductal cholestasis, reactive epithelial changes of the interlobular bile ducts, and acute cholangitis. Features of prolonged obstruction, such as fibrosis, feathery degeneration, and periportal copper accumulation, were also examined. Each patient record was thoroughly reviewed by two reviewers, and the following covariates were collected for each patient: age, gender (female/male), race (white, Asian, etc.), ethnicity (Hispanic/non-Hispanic), insurance status (private insurance, government insurance, unknown), body mass index (BMI), andlabs (total bilirubin, Gamma-glutamyl transferase (GGT), alkaline phosphatase (ALP), aspartate aminotransferase (AST), alanine aminotransferase (ALT), platelets, and international normalized ratio (INR)). Hospital length of stay was analyzed in both groups, as was hospital re-admission in the 6 months following liver biopsy demonstrating large duct obstruction. ERCPs were categorized as positive or negative, depending on whether there was an intervenable finding at the time of ERCP. ERCPs with intervenable findings were categorized as ‘positive’, and findings classified as ‘intervenable’ included biliary stricture or intrinsic/extrinsic obstructing lesion, biliary stone, papillary stenosis or ampullary obstruction, and anatomical irregularity of the bile duct for which stent placement was necessary. See Figure 1 for conceptual depiction of study flow.
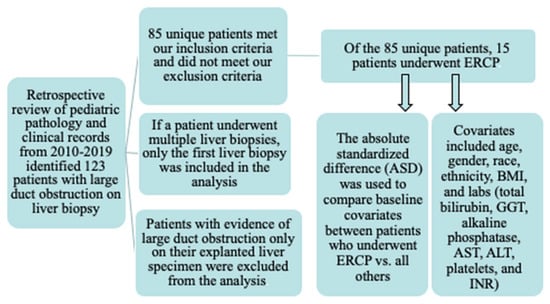
Figure 1.
Study flow diagram.
2.2. Study Outcomes
The primary study outcome was the presence of intervenable ERCP findings in patients who had evidence of large duct obstruction on liver biopsy without evidence of biliary obstruction on imaging and who subsequently underwent ERCP. The covariates listed above were included in the analysis to determine whether there were clinical differences in patients who had intervenable ERCP findings vs. those who did not.
We further characterize the population of pediatric patients in whom large duct obstruction was diagnosed on liver biopsy to identify comorbidities and demographics of this population.
2.3. Statistical Analysis
Descriptive statistics with proportions, means, and standard deviations were presented for the entire cohort in regard to demographics and clinical variables, including prior medical history, labs, and imaging.
The study population was stratified into those who underwent ERCP post-liver biopsy and those who did not. We evaluated each variable using the absolute standardized difference (ASD). The ASD is defined as the difference in means or proportions divided by the pooled standard deviation. An ASD of 0.2, 0.5, and 0.8 represents small, median, and large differences. ASD values <0.2 represent no discernible difference between the two groups. The larger the ASD, the more different the two groups are from each other. The ASD is increasingly utilized for analysis of descriptive data and quantification of differences between groups, while p-values are largely reserved for hypothesis testing [8]. P-values indicate whether a difference exists, but they do not describe the difference in the effect size [9]. The ASD is a measure of covariate balance [10].
The study population that underwent ERCP was then stratified into those who had a positive ERCP and those who had a negative ERCP. A positive ERCP was defined as an ERCP in which there was an intervenable finding.
3. Results
3.1. Demographic and Clinical Characteristics of All Patients
During the study period from 2010 to 2019, 123 liver biopsies performed in patients without evidence of biliary obstruction on prior imaging with abdominal ultrasound, magnetic resonance cholangiopancreatography, or computed tomography scan and with evidence of large duct obstruction on biopsy were analyzed. After inclusion and exclusion criteria were applied, 85 unique patients were identified as having large duct obstruction on liver biopsy.
Table 1 depicts demographic and clinical characteristics of the study population. The mean patient age was 7 years (SD 6.66). Females accounted for the majority of patients (60%). Racial composition was notable, and there were 47.1% white and 20% Asian patients. The study population was predominantly non-Hispanic (74.1%). The mean GGT and total bilirubin were 353 U/L and 4.6 mg/dL, respectively.

Table 1.
Demographics and clinical characteristics of pediatric patients with large duct obstruction on liver biopsy.
3.2. Demographic and Clinical Characteristics of Patients Who Underwent ERCP
3.2.1. Demographics
During the study period, 15 patients without evidence of biliary obstruction on imaging and with evidence of large duct obstruction on liver biopsy underwent ERCP, and 70 did not (Table 1). Among patients who underwent ERCP, 53% were white, 0% were Asian, and 40% identified as other, as compared to 46% white, 24% Asian, and 14% other in the non-ERCP group (ASD = 1.177). The two groups were less different in regard to ethnicity (ASD 0.553).
3.2.2. Clinical Characteristics
Among patients who underwent ERCP, four (36.7%) had previously undergone liver transplantation (26.7%). Among patients who did not undergo ERCP, 15 (21.4%) had previously undergone liver transplantation. The GGT was noted to be significantly higher in the ERCP group, with an ASD of 0.46. The mean GGT for the ERCP group was 497 U/L (SD 347.70) compared to 320 U/L (SD 413.45) for the non-ERCP group. Interestingly, ALT showed a reverse trend with a mean of 147 U/L (SD 4146.25) for the ERCP group and a mean of 275 U/L (SD 425.59) for the non-ERCP group. INR, alkaline phosphatase, and total bilirubin had ASD values of <0.2.
Among patients who underwent ERCP following liver biopsy demonstrating large duct obstruction, all underwent ERCP within 72 h of the biopsy diagnosis of large duct obstruction. None of the patients in this study (ERCP group or non-ERCP group) had a firm contraindication to performing ERCP.
3.3. ERCP Findings
Of the fifteen patients who underwent ERCP, 80% had an intervenable finding at ERCP, including biliary stricture (six patients, 50%) and choledocholithiasis (five patients, 41.6%). Intervention was successfully performed at ERCP for all patients in whom an intervenable finding was evident during cholangiography. Improvement in GGT (>20% improvement) was noted for 11 (91.7%) patients in the laboratory study following ERCP (within 36 h of ERCP). Among patients who underwent ERCP, non-intervenable findings were not evident in any patients (e.g., findings that would suggest the need for hepatobiliary surgery or interventional radiology intervention).
3.4. Clinical Trajectory
Among patients who underwent ERCP and had an intervenable lesion, 11/12 (91.67%) were noted to be clinically improved upon evaluation of the medical record one week after ERCP. One-week follow-up data documenting the clinical trajectory were not available for four patients in the medical record following ERCP.
Among patients who did not undergo ERCP, none had an interventional radiology or surgical intervention within one week of the liver biopsy diagnosis of large duct obstruction. One week following liver biopsy diagnosis of large duct obstruction, 42 (60%) patients who did not undergo ERCP were noted to be without change in clinical status based on medical record documentation, and 12 (17.1%) had documented deterioration in clinical status. One week follow-up clinical documentation was not available in the medical record in this time frame for the remaining 16 patients.
4. Discussion
In contrast to adult patients, in whom we have found that 48.1% of patients with large duct obstruction on liver biopsy undergo ERCP [11], only 17.6% of pediatric patients with no evidence of biliary obstruction on imaging and large duct obstruction on liver biopsy undergo ERCP. This suggests substantial differences in practice patterns between adult and pediatric hepatologists, as well as the likely relative under-utilization of ERCP in the pediatric population. Practice pattern differences between pediatric and adult hepatologists may be historical and could reflect the traditionally less mainstream role of ERCP in the evaluation and management of pediatric hepatobiliary disorders.
Large duct obstruction on liver biopsy arises particularly frequently in the setting of patients who have previously undergone liver transplantation—a substantial subset of patients included in this study. For example, one study from China found that out of 254 cases with liver allograft biopsies showing cholestasis, in 83 cases, the cholestasis was secondary to large duct obstruction, stricture, or stone [12]. Within the first month of liver transplantation, large duct obstruction/stricture was the third most common cause (13 cases) of cholestasis, with acute cellular rejection and sepsis being the two most common causes. However, large duct obstruction due to anastomotic or non-anastomotic biliary stricture was the most common cause of cholestasis at 6 months or more post-transplant. Thus, in addition to acute cellular rejection, large duct obstruction is one of the most common liver transplant complications [13,14].
The under-utilization of ERCP in children and adolescents is attributable to several factors. These factors contributing to less utilization of ERCP in children include lower rates of hepatobiliary disease addressable by ERCP in children, lack of adequate training in therapeutic endoscopy for pediatric gastroenterologists, and less availability of appropriately sized equipment for performing ERCP in children. Of interest, patient age did not differ significantly between children who underwent ERCP and those who did not. This may reflect enhanced uniformity of utilization of ERCP across age groups in pediatrics. Recent studies have attested to the safety and utility of ERCP in children. These studies underscore the importance of the present study in shaping practice patterns and indications for pediatric ERCP [15].
In the present study, ERCP was performed within 72 h of liver biopsy diagnosis of large duct obstruction for all patients who ultimately underwent ERCP in this clinical context; however, we recognize that variation in the time course from biopsy to ERCP may be present. This is relevant because some etiologies leading to large duct obstruction may require more time-sensitive intervention. Additionally, the utility of ERCP, as well as the capacity to intervene during ERCP, may wane as the interval from liver biopsy diagnosis of large duct obstruction to ERCP is prolonged.
Clinical decision making surrounding the decision to perform ERCP is influenced by a multitude of factors, including imaging findings, laboratory studies, and specifics of the patient’s overall medical comorbidities and clinical status. Pediatric patients who underwent ERCP were notable for having more pronounced elevation in GGT, and ALT was noted to be higher in the non-ERCP group. Elevated GGT level is a strong indicator of a biliary obstruction, because GGT is highly sensitive to impaired bile flow and rises quickly when the ducts are blocked. The GGT levels were overall higher (497 U/L) for patients who underwent ERCP in this study compared with those who did not undergo ERCP (320 U/L). This suggests a potential threshold of elevation in the mid-300 to mid-400 range that may have supported or prompted the decision to perform ERCP in these patients. Bilirubin levels, however, did not differ significantly between patients who underwent and did not undergo ERCP in this study. Given our limited sample size, the significance of these laboratory study differences cannot be fully determined. In addition to these laboratory findings of differences, demographic factors differed between pediatric patients who underwent ERCP and those who did not. Pediatric patients who underwent ERCP were more likely to be white and non-Hispanic—a finding that warrants further demographic study of pediatric patients who undergo ERCP.
Endoscopic ultrasound (EUS) is a modality commonly used prior to ERCP for biliary evaluation in adult patients and is emerging as a cornerstone modality for biliary evaluation in pediatric patients, for whom it has been found to be safe and effective. There is a potential role for EUS for these patients who have evidence of large duct obstruction on liver biopsy. EUS could help evaluate bile duct diameter and identify potential obstructing stones or lesions while also assessing liver and pancreatic morphology. It would be reasonable to consider the use of pre-ERCP EUS in this context for pediatric patients with evidence of large duct obstruction on liver biopsy.
Among patients who underwent ERCP for large duct obstruction in this series, the vast majority (80%) had intervenable findings, allowing for interventions to address biliary obstruction, including sphincterotomy, balloon dilatation, stone removal, and stent placement at the time of the procedure. Thus, the pediatric population may benefit substantially from ERCP in this clinical context. This is the first study to highlight the utility of ERCP in pediatric patients who have evidence of large duct obstruction on ERCP. These findings have been impactful in guiding decision making at our institution when a patient presents with liver biopsy demonstrating large duct obstruction. We have a lower threshold for performing ERCPs in these patients, given the high rate of intervenable findings addressed during ERCP. This has also been a point of training for our fellows, which shapes their practice during training and beyond.
Our study has several limitations. First, the sample size for the ERCP-negative group was small, and for that reason, ASD values may not have reflected significant differences between the ERCP and non-ERCP groups. A second limitation is that all patients included in this study were from one tertiary care center. Thus, it may be the case that different centers across the nation may have different results. Additionally, our patient population was primarily white and non-Hispanic, thus not reflecting the overall diversity of the U.S. population. Furthermore, clinical trajectory analysis was limited by data available in the medical record, the retrospective nature of the study, the lack of a robust electronic medical record for much of the study period, and the fact that patients may have sought care outside of our institution, which would prevent capture and analysis of that care. We also cannot rule out the possibility that some patients who did not undergo ERCP had a contraindication to the procedure that was not documented or captured in the medical record. Lack of follow-up data at one week and beyond for a subset of patients in this study who underwent ERCP also limits the conclusions that can be drawn from our analysis. Of note, small sample sizes were present for pediatric patients who underwent ERCP, which limited our ability to report granular clinical data and necessitated presentation of findings in aggregate to prevent linkage of data with a single individual, per our IRB regulations.
Although hepatobiliary disease and the finding of large duct obstruction on liver biopsy are much less common in children compared to adults, their life-year impact is high in the pediatric population. Furthermore, childhood hepatobiliary disorders are often precursors to adult liver disease [16], underscoring the importance of studying the role of endoscopic intervention in children when large duct obstruction is diagnosed on liver biopsy—a potential opportunity for intervention to prevent progressive biliary obstruction and hepatic function sequelae. Additional multi-center studies, including more patients and focused on understanding the utility of ERCP and the range of outcomes following the diagnosis of large duct obstruction in pediatrics, would be informative to guide pediatric hepatology and endoscopic practices.
In conclusion, the present study is the first study to highlight that the vast majority of ERCPs performed for pediatric patients who have evidence of large duct obstruction on liver biopsy have findings amenable to intervention to address the cause of biliary obstruction and improve the clinical trajectory of these patients. These data have had an impact on practice patterns at our institution, where there is now a lower threshold to perform ERCP for patients who have evidence of large duct obstruction on liver biopsy. These findings may also help guide practice patterns at other institutions to facilitate management of endoscopically intervenable obstruction in this population whenever possible.
Author Contributions
Conceptualization, M.M., M.T.B., R.G., G.C. and J.L.; methodology, M.M., M.T.B., R.G., G.C. and J.L.; formal analysis, J.L.; data curation, M.M.; writing—original draft preparation, M.M. and M.T.B.; writing—review and editing, M.M., M.T.B., R.G., G.C. and J.L. All authors have read and agreed to the published version of the manuscript.
Funding
NIH 5T32DK007056-43 supported MTB during initial phases of this study. This research received no additional external funding.
Institutional Review Board Statement
This study was approved by the Stanford University Institutional Review Board Protocol #s 45179, 52588.
Informed Consent Statement
Patient consent was not required by our IRB due to the retrospective nature of the study and the nature of data collected.
Data Availability Statement
Data supporting these results can not be made publicly available, per our IRB guidelines. These data are publicly unavailable due to patient privacy and ethical restrictions.
Conflicts of Interest
None of the authors have any conflicts of interest pertaining to the study to disclose.
References
- Pratt, D.S.; Kaplan, M.M. Evaluation of abnormal liver-enzyme results in asymptomatic patients. N. Engl. J. Med. 2000, 342, 1266–1271. [Google Scholar] [CrossRef] [PubMed]
- Skelly, M.M.; James, P.D.; Ryder, S.D. Findings on liver biopsy to investigate abnormal liver function tests in the absence of diagnostic serology. J. Hepatol. 2001, 35, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Villa, N.A.; Harrison, M.E. Management of biliary strictures after liver transplantation. Gastroenterol. Hepatol. 2015, 11, 316–328. [Google Scholar]
- Ponziani, F.R.; Bhoori, S.; Pompili, M.; Zocco, M.A.; Biolato, M.; Marrone, G.; Gasbarrini, A.; Mazzaferro, V.M.; Grieco, A. Post-liver transplant intrahepatic cholestasis: Etiology, clinical presentation, therapy. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 23–36. [Google Scholar] [PubMed]
- Czubkowski, P.; Pertkiewicz, J.; Markiewicz-Kijewska M Kaliciński, P.; Rurarz, M.; Jankowska, I.; Pawłowska, J. Endoscopic treatment in biliary strictures after pediatric liver transplantation. Pediatr. Transplant. 2018, 22, e13271. [Google Scholar] [CrossRef] [PubMed]
- Girotra, M.; Soota, K.; Klair, J.S.; Dang, S.M.; Aduli, F. Endoscopic management of post-liver transplant biliary complications. World J. Gastrointest. Endosc. 2015, 7, 446–459. [Google Scholar] [CrossRef] [PubMed]
- Szary, N.M.; Al-Kawas, F.H. Complications of endoscopic retrograde cholangiopancreatography: How to avoid and manage them. Gastroenterol. Hepatol. 2013, 9, 496–504. [Google Scholar]
- Thomas, E.; Pencina, M.J. Do Not Over (P) Value Your Research Article. JAMA Cardiol. 2016, 1, 1055. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, G.M.; Feinn, R. Using Effect Size-or Why the P Value Is Not Enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Thomas, L.E.; Li, F. Addressing Extreme Propensity Scores via the Overlap Weights. Am. J. Epidemiol. 2019, 188, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Martin, M.; Lee, J.; Gugig, R.; Ofosu, A.; Charville, G.W.; Barakat, M.T. The Majority of Patients Who Undergo ERCP When Large Duct Obstruction Is Evident on Liver Biopsy Have Biliary Findings Amenable to Endoscopic Intervention. J. Clin. Med. 2023, 12, 482. [Google Scholar] [CrossRef] [PubMed]
- Lo, R.C.; Chan, K.K.; Chok, K.S.; Ng, I.O. Liver allograft biopsies with histological cholestasis: A clinicopathological study of 254 cases from a single centre. J. Clin. Pathol. 2018, 71, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Perkins, J.D. Acute cellular rejection rates in living-donor and deceased-donor liver transplantation. Liver Transpl. 2006, 12, 886–887. [Google Scholar] [PubMed]
- Kochhar, G.; Parungao, J.M.; Hanouneh, I.A.; Parsi, M.A. Biliary complications after liver transplantation. World J. Gastreoenterol. 2013, 19, 2841–2846. [Google Scholar] [CrossRef] [PubMed]
- Barakat, M.T.; Cholankeril, G.; Gugig, R.; Berquist, W.E. Nationwide Evolution of Pediatric Endoscopic Retrograde Cholangiopancreatography Indications, Utilization, and Readmissions over Time. J. Pediatr. 2021, 232, 159–165.e1. [Google Scholar] [CrossRef] [PubMed]
- Arya, G.; Balistreri, W.F. Pediatric liver disease in the United States: Epidemiology and impact. J. Gastroenterol. Hepatol. 2002, 17, 521–525. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).