Abstract
Background/Objectives: Pedicled anterolateral thigh (ALT) flaps have proven their versatility through various applications including in different tissue compositions in locoregional reconstructions. However, they are underutilized compared to their free counterparts. Our aim is to systematically review the studies published on the utilization of pedicled ALT flaps in various anatomical regions. Methods: A search was conducted using the PubMed and Embase databases including the terms: (“pedicled” OR “island”) AND (“ALT” OR “anterolateral thigh flap” OR “lateral circumflex femoral” OR “vastus lateralis” OR “rectus femoris”). Outcomes regarding etiology, location, number and composition of flaps, flap and defect size, tunnel of the pedicle, flap viability and complications were collected. Results: A total number of 133 studies met the inclusion criteria, of which the majority were case series. After excluding the case reports (n = 49), studies included in the review were grouped based on anatomical locations such as abdominal (n = 12), groin (n = 12), perineal–vaginal–vulvar (n = 11), penile (n = 15), trochanteric–ischial–sacrogluteal (n = 8) and multiple (n = 19). Among a total of 1227 flaps, there were 46 partial (3.7%) and 16 total losses (1.3%). Conclusions: The pedicled ALT flap has been gaining popularity in the past decade. The overall flap loss rate is relatively low. However, the level of therapeutic evidence of published studies is not high, and there is a large heterogeneity among methods. There is a need in the literature for comparative studies with larger cohorts. Further studies will help to establish guidelines and possible algorithms that could include pedicled ALT flaps as first-line management options in different anatomical locations.
1. Introduction
Advancements in our understanding of cutaneous perforators opened a new chapter in the use of pedicled and free flaps. The lateral circumflex femoral artery (LCFA) system, with its rich perforators, is one of the most versatile donor sites in the body. After its introduction in 1984, the anterolateral thigh (ALT) perforator flap became an extremely valuable asset in the armamentarium of the reconstructive surgeon [1]. With the advantages of reliable anatomy, reduced donor site morbidity and the possibility to include multiple types of tissues, the ALT flap is often referred to as the ideal soft tissue flap for reconstruction of challenging defects in various regions [2].
A true ALT flap is classically described as a cutaneous or fasciocutaneous flap based on the perforators from the descending branch of the LCFA (LCFA-db). In addition to the “classical” flap, many modifications of size, shape, composition and orientation have been tailored according to the individual patients. The rich anatomical variety of this region (including skin, subcutaneous tissues, fascia, muscle, bone and nerve) allows composition of the flap to be adjusted depending on the reconstructive needs of the defects. For example, a part of the vastus lateralis (VL) muscle can be included in the musculocutaneous flap for a cavitary defect that requires coverage with the bulk of the muscle [3,4], or a part of the fascia lata (FL) can be included to reconstruct the abdominal wall integrity [5], or even a part of the femur can be included to form an osteocutaneous flap for a bony defect [6]. This freedom in design requires great understanding of the lateral thigh anatomy to clearly delineate different structures. In addition to the vascular and muscular anatomy, identifying and protecting nerves allow for the possibility of sensate flaps, or less donor site morbidity [7].
Although the free use of the ALT flap has been the subject of numerous publications with high patient numbers, the pedicled counterpart has not been in the spotlight as much. The number of applications of the pedicled use has been increasing over the past decade in reconstruction of the defects around the abdomen, pelvis and perineum [8,9]. The descending branch of the LCFA (LCFA-db) itself not only provides a long pedicle with a wide arc of rotation but also allows both proximal and distal flow. This allows the flap to be used for defects as superior as the supraumbilical region [10] and as inferior as the knee [11]. Tunneling is necessary for most of the locoregional reconstructions, and incorporating anatomical knowledge of the lateral thigh region is key for a successful flap transfer. Different tunneling options and important considerations to take into account while preparing the pedicles have been described in order to maximize the reach of the flap [12].
Limited reviews exist to summarize the outcomes of current literature on the use of the pedicled ALT flaps for reconstruction of locoregional defects. Therefore, this review aims to systematically review studies published on the utilization of pedicled ALT flaps in various anatomical regions, indications, compositions and outcomes.
2. Materials and Methods
A literature review was performed to review studies using pedicled ALT flaps for reconstruction of different anatomical regions between January 1999 and January 2024. PRISMA guidelines were utilized, and the study was approached as a systematic scoping review within the limitations discussed below. Study types included randomized trials, non-randomized trials, prospective studies, case-controlled studies, retrospective cohorts, case series and case reports. Meta-analyses, reviews, pre-clinical studies and cadaveric studies were excluded.
The search was conducted using the Cochrane, PubMed and Embase databases. Search terms included were: (“pedicled” OR “island”) AND (“ALT” OR “anterolateral thigh flap” OR “lateral circumflex femoral” OR “vastus lateralis” OR “rectus femoris”). References of the eligible studies were also reviewed to include any additional articles. The review was conducted by two independent reviewers. The review was not registered.
After removal of duplicate and non-English articles through the initial exclusion criteria, titles and abstracts of the remaining articles in human subjects were reviewed. Articles only including free flaps or muscle-only flaps from the LCFA system (i.e., vastus lateralis muscle flaps) were excluded. Articles only including reconstructions of the lower extremity or the knee with both distally based retrograde-flow and proximal-based pedicled flaps were also excluded. The inclusion criteria were limited to articles that explicitly studied or involved the use of pedicled ALT flaps with anterograde flow. For studies that involve other techniques in addition to the pedicled ALT flaps, only the cases of reconstruction with the pedicled ALT flaps were included.
Screened articles were discussed among the authors, and eligible studies were identified. Data from the eligible studies were extracted into a predesigned spreadsheet. Outcomes regarding etiology, location, number and composition of flaps, flap and defect size, tunnel of the pedicle, flap viability and complications were collected. Owing to the heterogeneity of the studies and the limited number of reported cases, data were not able to be pooled, and statistical meta-analysis was not possible. Similarly, study bias risk assessment was not completed. A qualitative descriptive analysis of all the data was conducted with a systematic narrative synthesis for each anatomical region. The primary outcome consisted of the flap viability rates, and a pooled percent ratio was utilized as the effect measurement for presentation of the results. Determination of the year of publication was based on the issue date of the “published articles” and the date of first online publication of the “online-only articles”.
Included articles were grouped based on the anatomical locations, such as abdominal, groin, perineal–vaginal–vulvar, penile, trochanteric–ischial–sacrogluteal and multiple. The anatomical descriptions included in the articles were accepted as the criteria for grouping. Studies including reconstructions of more than one of the classified anatomical regions were considered as “multiple locations”. Later, in each group, case reports presenting only 1 patient were excluded from the final analysis and included in a supplementary table (see Table S1, Supplementary Digital Content 1).
3. Results
The initial search identified a total of 1568 studies (Figure 1). After the initial exclusion, full texts of 181 articles were reviewed. The studies that did not fulfil the further exclusion criteria were removed, with a total number of 133 studies meeting the inclusion criteria. After excluding case reports (n = 56), articles included in the review comprised 12 abdominal, 12 groin, 11 perineal–vaginal–vulvar, 15 penile, 8 trochanteric–ischial–sacrogluteal and 19 multiple-location reconstructions. When the number of publications was analyzed based on the years that they were published, a trend appeared of increased publications over the past decade (Figure 2).
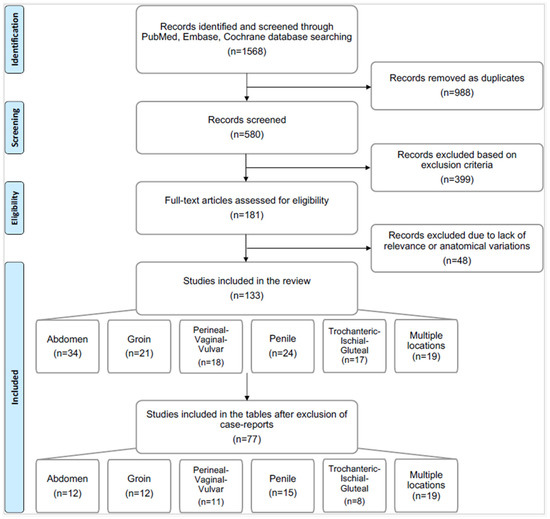
Figure 1.
Flow chart of studies included in the review.
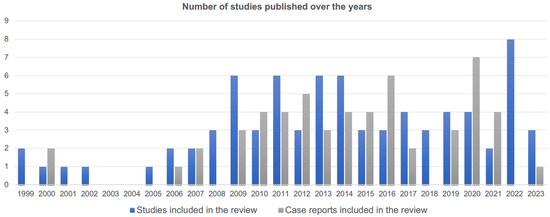
Figure 2.
Number of studies and case reports published on the use of pedicled anterolateral thigh flaps over the years.
The majority of the included articles were case series, in which levels of evidence were not usually beyond level IV. In each anatomical region, the largest series included under 40 patients undergoing reconstructions with pedicled ALT flaps, except for penile and multiple-location groups.
When the number of patients and flaps were pooled within each anatomical region, there were 88 flaps in 86 abdominal patients; 118 flaps in 116 groin patients; 211 flaps in 199 perineal–vaginal–vulvar patients; 321 flaps in 321 penile patients; 110 flaps in 105 trochanteric–ischial–sacrogluteal patients; and 379 flaps in 379 multiple-location patients. Although the complication reporting style was not consistent among the studies, flap viability was able to be assessed. There were six abdominal patients with partial flap loss (6.8%); two groin patients with partial loss (1.7%); two perineal–vaginal–vulvar patients with venous congestion requiring revision (0.9%) as well as two with total (0.9%) and eight with partial loss (3.7%); five penile patients with total (1.6%) and nine with partial loss (2.8%); four trochanteric–ischial–sacrogluteal patients with total loss (3.6%); and two multiple-location patients with venous congestion requiring revision (0.5%) as well as five with total (1.3%) and twenty-one with partial loss (5.5%). Among a total of 1227 flaps included in this review, there were 46 with partial loss (3.7%), 16 with total loss (1.3%) and 4 with venous congestion requiring revision (0.3%). The largest flap size harvested was a 31 × 40 cm musculocutaneous ALT flap with VL [13] for a perineal defect, followed by a 37 × 32 cm fasciocutaneous ALT flap [14] for an abdominal defect.
4. Discussion
Pedicled flaps from the LCFA system have proven their versatility through various applications in locoregional reconstructions. However, they are underutilized compared to their free counterparts. The main reason for this could be the fact that there are almost always other classical options to consider within each anatomical region. Therefore, the pedicled ALT flap has remained as an option only when the defects were deemed unmanageable with other local or simpler alternatives. Even in these complex cases, the pedicled ALT flap was safe, with 3.7% partial and 1.3% total flap loss. These rates are comparable with large series using a free flap counterpart [2,15]. Each anatomical region is discussed separately in the following sections.
4.1. Abdomen
The pedicled ALT flap in the context of reconstruction of complex abdominal wall defects was first reported by Kimata et al. in 1999 [16]. It was stated that this was a superior technique to the conventional tensor fascia lata (TFL) flap, as the distal skin paddle blood supply was more reliable, and the pedicle was longer with a greater reach. Luo et al. in 1999 also described 16 pedicled cases in their series of 168 ALT flaps, where one presented case was reconstruction of an abdominal defect with a pedicled ALT flap [17].
The etiologies mainly consisted of defects after oncological resections or after gastrointestinal surgeries (Table 1). Different components were included in the flap to reconstruct full-thickness abdominal wall defects. Vascularized FL was included in order to prevent hernia formation, especially in cases with failed prosthetic meshes, prior infection, fistula or radiation [5,9,18,19]. When the abdominal wall defect was massive and FL was not enough, composite pedicled flaps including rectus femoris (RF) and VL muscles were used on top of bioprosthetic meshes even in contaminated wounds [20,21,22,23]. Inclusion of muscle within the flap was also used to cover exposed organs such as the intestines or bladder [24,25,26]. A subtotal thigh flap including more than one muscle (RF, VL and FL) has been described for massive, composite abdominal wall defects [27]. Vranckx et al. used innervated VL to restore the continuity of the abdominal wall and create a dynamic reconstruction to improve the functional outcome [28].

Table 1.
Summary of included studies on reconstruction of the abdomen. IBD: inflammatory bowel disease, Fc: fasciocutaneous, TFL: tensor fascia lata, Mc: musculocutaneous, VL: vastus lateralis, RF: rectus femoris, NR: not reported.
In addition to the muscular tissues that can be included in the flap, reconstruction of large surface-only defects in the abdomen is possible with pedicled ALT flaps. In particular, the benefit of a relatively distant donor site might make an ALT flap a primary option for extensive injuries or in donor-area-depleted patients (such as those with burns or trauma). For massive defects, the use of tissue expansion [14,32] or delay methods [14] prior to flap harvest might aid in increasing the surface area of the flap. Additionally, tunneling the flap under RF and sartorius muscles is an important technical modification to increase the flap’s reach up to the contralateral abdomen or supraumbilical regions [10,12,33].
When the pedicled use was compared with the free ALT flap for the abdominal reconstructions, no difference was identified in the outcomes and complications [29,31]. However, Kayano et al. identified that the pedicled ALT flap is superior in decreasing the operative time by two hours [29]. The pedicled flap also has a lower risk of complete flap necrosis compared to the free flap, which is especially important in patients with complex wounds [34].
4.2. Groin
In 1999, Cunha-Gomes et al. introduced the pedicled ALT flap for inguinal defects as a versatile and durable local option with the possibility to harvest large, bulky flaps with reliable vessels [35,36]. In the majority of the articles studying the groin, this region consisted of the inguinal and pelvic areas, with extensions to the lower extremity and hypogastric and perineal regions (Table 2). Considering the anatomy of that area, several articles published reconstructions over exposed vascular structures (femoral artery and vein) or reconstructed vessels with grafts [37,38,39]. The pedicled ALT flap may be a useful alternative in these cases due to the possibility of a lack of recipient vessels around the defect. Other etiologies in the groin included reconstruction of the defects after lymph node dissection due to metastasis from a primary tumor [40,41] and postburn contractures [42].

Table 2.
Summary of included studies on reconstruction of the groin. Fc: fasciocutaneous, TFL: tensor fascia lata, Mc: musculocutaneous, VL: vastus lateralis, RF: rectus femoris, NR: not reported, DVT: deep vein thrombosis.
In a level III evidence study, LoGiudice et al. compared the pedicled ALT flap with the workhorse flap in this region, the rectus abdominis flap [43]. They identified lower rates of delayed postoperative complications and favorable donor site morbidity and suggested that the pedicled ALT flap should be considered as a first-line choice for wounds in this area. On the other hand, Arvanitakis et al. suggested that the posteromedial thigh perforator flap should be considered as a primary option, followed by the pedicled ALT flap and the deep inferior epigastric artery perforator flap in the absence of the former options [44]. The study also highlighted the versatility of the pedicled ALT flap and the possibility to use multiple components for complex defects.
4.3. Perineum
The use of a pedicled ALT flap in the reconstruction of a skin and subcutaneous tissue defect of the perineum was described by Luo et al. for a defect where previous gracilis flaps had failed [48]. Later, Huang et al. also described the use of a musculocutaneous ALT flap with VL for reconstruction of a vulvar defect after oncological resection [49].
Perineal defects, mainly due to extirpation of cancer in the rectum, perianal tissues or vagina, are complicated by the possibility of pre-operative or postoperative radiation, exposure of the abdominal contents and the risk of contamination (Table 3) [50,51,52,53,54,55,56]. Rectus abdominis, gracilis, gluteus maximus muscle or gluteal fasciocutaneous flaps have been traditionally used for the reconstruction; however, these options may be limited in certain scenarios. When these options are limited, the pedicled ALT flap has been described as an option with wide capabilities in design. Zeng et al. proposed an algorithm for tailoring the flap to manage different unilateral and bilateral defects with minimal donor site morbidity [52]. Their study identified different modifications of the flap shapes depending on the location of the defects around the vulva, including fusiform, fenestrated or split uses. Zelken et al. proposed an individually tailored algorithm to identify flap composition based on the complexity and requirements of the defects [21].

Table 3.
Summary of included studies on reconstruction of the perineum. IBD: inflammatory bowel disease, HS: hidradenitis suppurativa, Fc: fasciocutaneous, TFL: tensor fascia lata, Mc: musculocutaneous, VL: vastus lateralis, RF: rectus femoris, NR: not reported, DVT: deep vein thrombosis.
Musculocutaneous flaps (mainly ALT with VL) to fill deep cavities in this region were described in the cases of prior radiation, inflammation, infection and exposed foreign materials [4,13,21,38,53,54,56,60]. Wong et al. described the use of pedicled VL as a muscle or a musculocutaneous flap in the reconstruction of large perineal defects resulting from abdominoperineal reconstruction and suggested that this flap can be an option to consider when the rectus abdominis flap is unavailable [51]. di Summa et al. presented their series of reconstructions of large defects that require bulk and are associated with radiotherapy with durable outcomes [4]. In more recent studies, Gentileschi et al. [53] and Perrault et al. [59] suggested that given the already complicated nature (i.e., radiotherapy) of perineal defects after oncological resections, the pedicled ALT flap should be considered as a first-line option given its proven versatility and reliability.
Reconstruction of the defects due to Fournier’s gangrene is another application of the pedicled ALT flap given that there are limited options to provide the soft tissue coverage required for the extensive defects [3,57,58,60,61,62,63].
4.4. Penile
Reconstruction of the penis can be summarized in two groups based on the type of reconstruction, complete or partial. The latter includes reconstruction of part of a damaged penis after infections, burns or trauma [64,65,66]. Complete reconstruction, on the other hand, includes creating a non-existent penis, such as in patients with congenital problems, penile amputation or undergoing gender affirmation surgery (Table 4) [66,67,68].

Table 4.
Summary of included studies on reconstruction of penis. Fc: fasciocutaneous, TFL: tensor fascia lata, RF: rectus femoris, NR: not reported.
The radial forearm free flap (RFFF) and pedicled ALT flap are the main options for complete reconstruction of the penis. Lumen et al. compared these two options in patients with severe penile insufficiency and suggested that the pedicled ALT flap is an option when a free flap is contraindicated [69]. Ascha et al. compared 149 RFFFs with pedicled ALT flap phalloplasty and revealed that the pedicled ALT flap was associated with greater rates of urethral fistula and dehiscence [76]. In general, when an appropriate donor site and vascular anatomy is available, the main advantages of the pedicled ALT flap are (1) an inconspicuous donor site concealable under clothing and (2) surgery without the need for microsurgical anastomosis [65,70,79,80]. The disadvantages of the ALT flap are higher incidence of both flap and urethral complications when compared with a radial forearm phalloplasty [80]. Although the first choice for penile reconstruction varies among surgeons, careful patient selection and discussion regarding the potential of revision surgeries is important for each method.
The vascular anatomy of the flap can be planned preoperatively with CT to allow for adequate perforator selection and to design the flap according to the needs of the patient [72]. Different modifications to the flap design have been described, including tube-in-tube [70], mushroom [81], pre-expansion of the donor site (to allow for primary donor site closure) [74] and combination with other free flaps [77]. van der Sluis et al. combined the pedicled ALT flap with the RFFF, where a smaller RFFF was able to be harvested solely for the purposes of urethral reconstruction, thus resulting in less scar tissue in the forearm and durable urethral reconstruction [75]. In a recent series, D’Arpa et al. presented their 13 years of experience in 93 patients with different methods of pedicled ALT flaps, proposed an algorithm for the challenging topic of urethral reconstruction and highlighted that there is no single best technique because the method should be adjusted based on each patient’s features [77]. Wu et al. also presented their 10-year experience with 49 patients undergoing the pedicled ALT flap; their outcomes and proposed algorithm highlight the importance of adjusting technique based on patient features [66].
4.5. Trochanteric, Ischial and Sacrogluteal
Muscle transposition flaps from the LFCA system have been used for many years for ischial and trochanteric defects. TFL musculocutaneous flaps are the traditional reconstructive option for trochanteric defects [82,83]. The use of musculocutaneous VL flaps was then introduced in 1982 [84], with multiple applications in the years following [85,86]. These applications, however, do not involve perforator identification and follow the concepts of transposition flaps.
Pedicled musculocutaneous ALT flaps are important options for trochanteric defects, with an increased number of applications after the identification of perforator flaps (Table 5) [87,88]. In addition to small defects, the musculocutaneous ALT flap can be suitable for more complex cavitary defects [62,89]. Li et al. compared hatchet-shaped TFL transposition flaps with pedicled ALT flaps and identified that although the operative time with the ALT flap was longer, the recurrence rate was significantly lower [90]. Their study suggested that the musculocutaneous ALT flap should be considered as the first choice in reconstruction of trochanteric defects.

Table 5.
Summary of included studies on reconstruction of trochanteric, ischial and sacrogluteal regions. Fc: fasciocutaneous, TFL: tensor fascia lata, Mc: musculocutaneous, VL: vastus lateralis, RF: rectus femoris, VI: vastus intermedius, VM: vastus medialis, NR: not reported.
The use of the pedicled musculocutaneous ALT flap for reconstruction of ischial pressure sores was also reported, mostly in challenging cases with wide surface or depth area and depleted local flap options [3,63,91,94,95]. Tunneling the flap from the anterior muscle compartment to the posterior muscle compartment of the thigh through a medially based tunnel can also extend the reach of the flap towards the posterior thigh and ischium [12]. The flap can also be extended towards the sacrum and higher gluteal areas [39]. Often, in patients with longstanding paraplegia, the individual quadriceps muscles can be atrophic, and any single one of them may not be enough to provide adequate bulk to fill a deep and wide cavitary defect. This may necessitate the use of the “tri-muscle” flap to include VL, vastus intermedius and RF muscles [92].
4.6. Multiple Locations
Studies grouped under multiple locations have been discussed previously based on the most common anatomical region reconstructed in them. The majority of published studies on the use of pedicled ALT flaps report reconstructions involving multiple anatomical locations and indications (Table 6). This shows that the surgeons who are familiar with the anatomy of this region and comfortable using this flap are capable of using it as a primary go-to option for multiple locations. The demonstrated versatility of this donor site is unmatched by any other donor site in the body, where in addition to its free flap counterpart, pedicled uses can reach the supraumbilical region, gluteal area, perineum, trochanteric region and contralateral groin. We believe that, as more surgeons become comfortable with its use, indications of this flap as a primary option will increase.

Table 6.
Summary of included studies on reconstruction of multiple locations. IBD: inflammatory bowel disease, Fc: fasciocutaneous, TFL: tensor fascia lata, Mc: musculocutaneous, VL: vastus lateralis, RF: rectus femoris, VI: vastus intermedius, VM: vastus medialis, NR: not reported.
4.7. Limitations
This review is limited by the availability of publications and associated biases. Almost all the studies included in the review presented a low level of therapeutic evidence and mainly consisted of case series. This largely suggests that the groups were not randomized and there were no control groups used for comparison. Another major limitation is the heterogeneity among studies. Although we grouped studies based on the anatomical regions to minimize this limitation, there were still heterogeneities among the etiologies, flap compositions, tunneling methods, surgical techniques and reporting of the complications. This made pooling of the studies and interpretation of the results difficult and prone to bias [101]. In order to partially address this limitation, we used flap viability as a primary outcome of the review, as this was generally consistent among a majority of the studies. However, the reader should take into consideration that surgical technique variability may still be a crucial factor. These major limitations further prevented completion of certain stages in the PRISMA guidelines, including assessment for bias, meta-analysis and additional syntheses and analysis.
The value of case reports cannot be ignored in a topic a with low level of reported patient numbers. We therefore have included all case reports that fit the inclusion criteria in a separate Supplementary File, although these studies were not included in the analysis.
5. Conclusions
The pedicled ALT flap has been gaining popularity in the past decade, with an increased rate of indications. In addition to its versatility with respect to the arc of rotation, various tissue compositions can also be adjusted depending on the needs of the defect. We identified that the overall flap loss rate was relatively low, although the level of therapeutic evidence of published studies is not high, and there is significant heterogeneity among methods. We hope that this review demonstrates how versatile the pedicled ALT flap is, and that there is a need in the literature for comparative studies with larger cohorts. It is still unclear which factors are associated with which complications in each method and anatomical location. Further studies will help establish guidelines and possible algorithms that could include the pedicled ALT flap as a first-line management option in different anatomical locations.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/surgeries6010013/s1, Table S1, Supplementary Digital Content 1. Summary of case reports that met the inclusion criteria and their references. All case reports include presentation of a single patient where the reconstruction was performed with a pedicled anterolateral thigh flap. AVM: arteriovenous malformation, Fc: Fasciocutaneous, TFL: Tensor fascia lata, Mc: Musculocutaneous, VL: vastus lateralis, RF: rectus femoris, NR: not reported, DVT: deep vein thrombosis, PE: pulmonary embolism.
Author Contributions
Conceptualization, F.B.B. and T.O.A.; methodology, F.B.B. and E.D.; software, F.B.B. and E.D.; validation, F.B.B., E.D. and T.O.A.; formal analysis, F.B.B. and E.D.; investigation, F.B.B. and E.D.; data curation, F.B.B. and E.D.; writing—original draft preparation, F.B.B. and E.D.; writing—review and editing, F.B.B., E.D. and T.O.A.; visualization, F.B.B. and E.D.; supervision, T.O.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Published with the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Song, Y.G.; Chen, G.Z.; Song, Y.L. The free thigh flap: A new free flap concept based on the septocutaneous artery. Br. J. Plast. Surg. 1984, 37, 149. [Google Scholar] [CrossRef]
- Wei, F.C.; Jain, V.; Celik, N.; Chen, H.C.; Chuang, D.C.C.; Lin, C.H. Have we found an ideal soft-tissue flap? An experience with 672 anterolateral thigh flaps. Plast. Reconstr. Surg. 2002, 109, 2219–2230. [Google Scholar] [CrossRef] [PubMed]
- Hsu, H.; Chien, S.H.; Wang, C.H.; Hsu, H.M.; Chien, S.-H.; Wang, C.-H.; Cheng, L.-F.; Lin, C.-M.; Wu, M.-S.; Huang, C.-C.; et al. Expanding the Applications of the Pedicled Anterolateral Thigh and Vastus Lateralis Myocutaneous Flaps. Ann. Plast. Surg. 2012, 69, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Di Summa, P.G.; Tremp, M.; Meyer zu Schwabedissen, M.; Schaefer, D.J.; Kalbermatten, D.F.; Raffoul, W. The Combined Pedicled Anterolateral Thigh and Vastus Lateralis Flap as Filler for Complex Perineal Defects. Ann. Plast. Surg. 2015, 75, 66–73. [Google Scholar] [CrossRef]
- Shih, P.K. Feasibility of pedicled anterolateral thigh flap with tensor fascia lata and vastus lateralis for difficult abdominal wall closure. Hernia 2019, 23, 749–755. [Google Scholar] [CrossRef]
- Acartürk, T. Femur-Vastus Intermedius-Anterolateral Thigh Osteomyocutaneous Composite Chimeric Free Flap: A New Free Flap for the Reconstruction of Complex Wounds. J. Reconstr. Microsurg. 2011, 27, 187–194. [Google Scholar] [CrossRef]
- Toia, F.; D’Arpa, S.; Brenner, E.; Melloni, C.; Moschella, F.; Cordova, A. Segmental anatomy of the vastus lateralis: Guidelines for muscle-sparing flap harvest. Plast. Reconstr. Surg. 2015, 135, 185e–198e. [Google Scholar] [CrossRef] [PubMed]
- Neligan, P.C.; Lannon, D.A. Versatility of the Pedicled Anterolateral Thigh Flap. Clin. Plast. Surg. 2010, 37, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Lannon, D.A.; Ross, G.L.; Addison, P.D.; Novak, C.B.; Lipa, J.E.; Neligan, P.C. Versatility of the Proximally Pedicled Anterolateral Thigh Flap and Its Use in Complex Abdominal and Pelvic Reconstruction. Plast. Reconstr. Surg. 2011, 127, 677–688. [Google Scholar] [CrossRef]
- Fernandez-Alvarez, J.A.; Barrera-Pulido, F.; Lagares-Borrego, A.; Narros-Gimenez, R.; Gacto-Sanchez, P.; Gomez-Cia, T. Coverage of supraumbilical abdominal wall defects: The tunnelled-pedicled ALT technique. Microsurgery 2017, 37, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Gravvanis, A.I.; Tsoutsos, D.A.; Karakitsos, D.; Panayotou, P.; Iconomou, T.; Zografos, G.; Karabinis, A.; Papadopoulos, O. Application of the pedicled anterolateral thigh flap to defects from the pelvis to the knee. Microsurgery 2006, 26, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Vijayasekaran, A.; Gibreel, W.; Carlsen, B.T.; Moran, S.L.; Saint-Cyr, M.; Bakri, K.; Sharaf, B. Maximizing the Utility of the Pedicled Anterolateral Thigh Flap for Locoregional Reconstruction: Technical Pearls and Pitfalls. Clin. Plast. Surg. 2017, 44, 371–384. [Google Scholar] [CrossRef] [PubMed]
- Kosutic, D.; Tsapralis, N.; Gubbala, P.; Smith, M. Reconstruction of critically-sized perineal defect with perforator flap puzzle technique: A case report. Case Rep. Plast. Surg. Hand Surg. 2019, 6, 38–42. [Google Scholar] [CrossRef]
- Frey, J.D.; Jacoby, A.; Cohen, S.M.; Saadeh, P.B.; Levine, J.P. Massive, Extended Pedicled Anterolateral Thigh Flap for Abdominal Wall Reconstruction. Plast. Reconstr. Surg. 2020, 147, 181e–182e. [Google Scholar] [CrossRef]
- Yang, Q.; Ren, Z.H.; Chickooree, D.; Wu, H.; Tan, H.; Wang, K.; He, Z.; Gong, C.; Ram, V.; Zhang, S. The effect of early detection of anterolateral thigh free flap crisis on the salvage success rate, based on 10 years of experience and 1072 flaps. Int. J. Oral Maxillofac. Surg. 2014, 43, 1059–1063. [Google Scholar] [CrossRef]
- Kimata, Y.; Uchiyama, K.; Sekido, M.; Sakuraba, M.; Iida, H.; Nakatsuka, T.; Harii, K. Anterolateral thigh flap for abdominal wall reconstruction. Plast. Reconstr. Surg. 1999, 103, 1191–1197. [Google Scholar] [CrossRef] [PubMed]
- Luo, S.; Raffoul, W.; Luo, J.; Luo, L.; Gao, J.; Chen, L.; Egloff, D.V. Anterolateral thigh flap: A review of 168 cases. Microsurgery 1999, 19, 232–238. [Google Scholar] [CrossRef]
- Nthumba, P.; Barasa, J.; Cavadas, P.C.; Landin, L. Pedicled Fasciocutaneous Anterolateral Thigh Flap for the Reconstruction of a Large Postoncologic Abdominal Wall Resection Defect. Ann. Plast. Surg. 2012, 68, 188–189. [Google Scholar] [CrossRef]
- Di Summa, P.G.; Watfa, W.; Giordano, S.; Elahi-Rausis, L.; Bauquis, O.; Hahnloser, D.; Raffoul, W. Composite ALT flap for structured reconstruction of the abdominal wall: New insights from long-term outcomes in 14 patients. J. Plast. Reconstr. Aesthet. Surg. 2019, 72, 1700–1738. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Zhou, X.; Li, Z.; Chen, J.-Y.; Peng, X.-W.; Yang, L.-C.; Lv, C.-L. Reconstruction of the Lower Abdominal Region Using Bilateral Pedicled Anterolateral Thigh Flaps Combined with Poly-Surgical Mesh. Medicine (Baltimore) 2015, 94, e2375. [Google Scholar] [CrossRef] [PubMed]
- Zelken, J.A.; AlDeek, N.F.; Hsu, C.C.; Chang, N.J.; Lin, C.H.; Lin, C.H. Algorithmic approach to lower abdominal, perineal, and groin reconstruction using anterolateral thigh flaps. Microsurgery 2016, 36, 104–114. [Google Scholar] [CrossRef]
- Fukui, K.; Fujioka, M.; Ishiyama, S. Reconstruction of Abdominal Wall Defects Using a Pedicled Anterolateral Thigh Flap Including the Vastus Lateralis Muscle: A Report of Two Cases. Case Rep. Surg. 2016, 2016, 8753479. [Google Scholar] [CrossRef]
- Gao, Z.; Zhang, D.; Lei, F.; Zeng, Q.; Huang, W.; Wang, Y.; Gao, Q.; Niu, P.; Hong, Y.; He, X.; et al. Surgical treatment of massive stoma site tumors after a curative operation for rectal cancer. Eur. J. Surg. Oncol. 2020, 46, e40–e46. [Google Scholar] [CrossRef]
- Lambe, G.; Russell, C.; West, C.; Kalaiselvan, R.; Slade, D.A.J.; Anderson, I.D.; Watson, J.S.; Carlson, G.L. Autologous reconstruction of massive enteroatmospheric fistulation with a pedicled subtotal lateral thigh flap. Br. J. Surg. 2012, 99, 964–972. [Google Scholar] [CrossRef]
- Wu, C.W.; Lin, C.H.; Lin, C.H. One-stage posttraumatic bladder reconstruction and soft-tissue coverage of the lower abdomen or perineum. Ann. Plast. Surg. 2010, 64, 65–68. [Google Scholar] [CrossRef]
- Ete, G.; Mj, F.C.; Kingsly, P.M.; Akamanchi, A.K.; Agarwal, S. Abdominal Wall Reconstruction in Adults with Exstrophy of the Bladder. Ann. Plast. Surg. 2022, 89, 675–678. [Google Scholar] [CrossRef]
- Lin, S.J.; Butler, C.E. Subtotal Thigh Flap and Bioprosthetic Mesh Reconstruction for Large, Composite Abdominal Wall Defects. Plast. Reconstr. Surg. 2010, 125, 1146–1156. [Google Scholar] [CrossRef] [PubMed]
- Vranckx, J.J.; Stoel, A.M.; Segers, K.; Nanhekhan, L. Dynamic reconstruction of complex abdominal wall defects with the pedicled innervated vastus lateralis and anterolateral thigh PIVA flap. J. Plast. Reconstr. Aesthet. Surg. 2015, 68, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Kayano, S.; Sakuraba, M.; Miyamoto, S.; Nagamatsu, S.; Taji, M.; Umezawa, H.; Kimata, Y. Comparison of pedicled and free anterolateral thigh flaps for reconstruction of complex defects of the abdominal wall: Review of 20 consecutive cases. J. Plast. Reconstr. Aesthet. Surg. 2012, 65, 1525–1529. [Google Scholar] [CrossRef]
- Srinivas, J.S.; Panagatla, P.; Damalacheru, M.R. Reconstruction of Type II abdominal wall defects: Anterolateral thigh or tensor fascia lata myocutaneous flaps? Indian J. Plast. Surg. 2018, 51, 33–39. [Google Scholar] [CrossRef]
- Di Summa, P.G.; Watfa, W.; Campisi, C.; Giordano, S.; Oranges, C.M.; Elahi-Rausis, L.; Bauquis, O.; Hahnloser, D.; Demartines, N.; Raffoul, W. Free versus pedicled anterolateral thigh flap for abdominal wall reconstruction. Anticancer Res. 2019, 39, 6759–6768. [Google Scholar] [CrossRef] [PubMed]
- Acarturk, T.O.; Bengur, F.B. Total aesthetic subunit reconstruction of the burned anterior abdomen using pre-expanded pedicled anterolateral thigh flap—A case report. Microsurgery 2019, 39, 753–757. [Google Scholar] [CrossRef]
- Tamai, M.; Nagasao, T.; Miki, T.; Hamamoto, Y.; Kogure, T.; Tanaka, Y. Rotation arc of pedicled anterolateral thigh flap for abdominal wall reconstruction: How far can it reach? J. Plast. Reconstr. Aesthet. Surg. 2015, 68, 1417–1424. [Google Scholar] [CrossRef] [PubMed]
- Maxhimer, J.B.; Hui-Chou, H.G.; Rodriguez, E.D. Clinical Applications of the Pedicled Anterolateral Thigh Flap in Complex Abdominal–Pelvic Reconstruction. Ann. Plast. Surg. 2011, 66, 285–291. [Google Scholar] [CrossRef]
- Cunha-Gomes, D.; Bembde, R.; Bhathena, H.; Kavarana, N.M. The pedicled anterolateral thigh island flap for inguinal defects. Eur. J. Plast. Surg. 2000, 23, 97–100. [Google Scholar] [CrossRef]
- Cunha-Gomes, D.; Bhathena, H.M.; Kavarana, N.M. The anterolateral thigh flap: A versatile pedicled and free flap transfer. Eur. J. Plast. Surg. 2001, 24, 80–84. [Google Scholar] [CrossRef]
- Shih, P.K.; Cheng, H.T.; Wu, C.I.; Chang, S.C.N.; Chen, H.C.; Chen, H.H. Management of infected groin wounds after vascular surgery. Surg. Infect. 2013, 14, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Aslim, E.J.; Rasheed, M.Z.; Lin, F.; Ong, Y.S.; Tan, B.K. Use of the Anterolateral Thigh and Vertical Rectus Abdominis Musculocutaneous Flaps as Utility Flaps in Reconstructing Large Groin Defects. Arch. Plast. Surg. 2014, 41, 556. [Google Scholar] [CrossRef] [PubMed]
- Friji, M.T.; Suri, M.P.; Shankhdhar, V.K.; Ahmad, Q.G.; Yadav, P.S. Pedicled Anterolateral Thigh Flap. Ann. Plast. Surg. 2010, 64, 458–461. [Google Scholar] [CrossRef] [PubMed]
- Evriviades, D.; Raurell, A.; Perks, A.G.B. Pedicled Anterolateral Thigh Flap for Reconstruction After Radical Groin Dissection. Urology 2007, 70, 996–999. [Google Scholar] [CrossRef] [PubMed]
- Gravvanis, A.; Caulfield, R.H.; Mathur, B.; Ramakrishnan, V. Management of Inguinal Lymphadenopathy. Ann. Plast. Surg. 2009, 63, 307–310. [Google Scholar] [CrossRef]
- Uygur, F.; Sever, C.; Kulahci, Y.; Gideroğlu, K. Reconstruction of postburn inguinal contractures using the pedicled anterolateral thigh Flap. Burns 2009, 35, e3–e7. [Google Scholar] [CrossRef] [PubMed]
- Logiudice, J.A.; Haberman, K.; Sanger, J.R. The anterolateral thigh flap for groin and lower abdominal defects: A better alternative to the rectus abdominis flap. Plast. Reconstr. Surg. 2014, 133, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Arvanitakis, M.; Schlagnitweit, P.; Franchi, A.; Fritsche, E.; Chen, Y.C.; Scaglioni, M.F. Groin defect reconstruction with perforator flaps: Considerations after a retrospective single-center analysis of 54 consecutive cases. J. Plast. Reconstr. Aesthet. Surg. 2019, 72, 1795–1804. [Google Scholar] [CrossRef] [PubMed]
- Fuzzard, S.K.; Mah, E.; Choong, P.F.M.; Grinsell, D. Lymphoedema rates in pedicled anterolateral thigh flaps for coverage of irradiated groin defects. ANZ J. Surg. 2020, 90, 135–138. [Google Scholar] [CrossRef] [PubMed]
- Hernekamp, J.F.; Lauer, H.; Goertz, O.; Weigang, E.; Kneser, U.; Kremer, T. Soft Tissue Reconstruction of Complex Infrainguinal Wounds Following Revisionary Vascular Surgery. Ann. Vasc. Surg. 2023, 88, 108–117. [Google Scholar] [CrossRef] [PubMed]
- Scaglioni, M.F.; Meroni, M.; Fritsche, E. Soft Tissue Defect Reconstruction and Lymphatic Complications Prevention: The Lymphatic Flow-Through (LyFT) Concept. Medicina 2022, 58, 509. [Google Scholar] [CrossRef]
- Luo, S.; Raffoul, W.; Piaget, F.; Egloff, D.V. Anterolateral thigh fasciocutaneous flap in the difficult perineogenital reconstruction. Plast. Reconstr. Surg. 2000, 105, 171–173. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.Y.; Lin, H.; Liu, Y.T.; ChangChien, C.C.; Chang, S.Y. Anterolateral thigh vastus lateralis myocutaneous flap for vulvar reconstruction after radical vulvectomy: A preliminary experience. Gynecol. Oncol. 2000, 78, 391–393. [Google Scholar] [CrossRef]
- Wang, X.; Qiao, Q.; Burd, A.; Liu, Z.; Zhao, R.; Wang, C.; Zeng, A. Perineum reconstruction with pedicled anterolateral thigh fasciocutaneous flap. Ann. Plast. Surg. 2006, 56, 151–155. [Google Scholar] [CrossRef]
- Wong, S.; Garvey, P.; Skibber, J.; Yu, P. Reconstruction of Pelvic Exenteration Defects with Anterolateral Thigh–Vastus Lateralis Muscle Flaps. Plast. Reconstr. Surg. 2009, 124, 1177–1185. [Google Scholar] [CrossRef]
- Zeng, A.; Qiao, Q.; Zhao, R.; Song, K.; Long, X. Anterolateral thigh flap-based reconstruction for oncologic vulvar defects. Plast. Reconstr. Surg. 2011, 127, 1939–1945. [Google Scholar] [CrossRef] [PubMed]
- Gentileschi, S.; Servillo, M.; Garganese, G.; Simona, F.; Scambia, G.; Salgarello, M. Versatility of pedicled anterolateral thigh flap in gynecologic reconstruction after vulvar cancer extirpative surgery. Microsurgery 2017, 37, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Ng, R.W.M.; Chan, J.Y.W.; Mok, V.; Li, G.K.H. Clinical use of a pedicled anterolateral thigh flap. J. Plast. Reconstr. Aesthet. Surg. 2008, 61, 158–164. [Google Scholar] [CrossRef]
- Crosby, M.A.; Hanasono, M.M.; Feng, L.; Butler, C.E. Outcomes of partial vaginal reconstruction with pedicled flaps following oncologic resection. Plast. Reconstr. Surg. 2011, 127, 663–669. [Google Scholar] [CrossRef] [PubMed]
- Rossi, S.A.; Martineau, J.J.C.; Guillier, D.; Hübner, M.; Hahnloser, D.; Raffoul, W.; di Summa, P.G.M. Outcomes of the Composite Anterolateral Thigh Flap for Perineal Reconstruction after Postoncological Abdominoperineal Resection. Colon Rectum 2022, 65, 373–381. [Google Scholar] [CrossRef]
- Spyropoulou, G.A.; Jeng, S.F.; Demiri, E.; Dionyssopoulos, A.; Feng, K.M. Reconstruction of Perineoscrotal and Vaginal Defects with Pedicled Anterolateral Thigh Flap. Urology 2013, 82, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.T.; Chang, S.C.; Chen, S.G.; Tzeng, Y.S. Reconstruction of perineoscrotal defects in Fournier’s gangrene with pedicle anterolateral thigh perforator flap. ANZ J. Surg. 2016, 86, 1052–1055. [Google Scholar] [CrossRef] [PubMed]
- Perrault, D.; Kin, C.; Wan, D.C.; Kirilcuk, N.; Shelton, A.; Momeni, A. Pelvic/Perineal Reconstruction: Time to Consider the Anterolateral Thigh Flap as a First-line Option? Plast. Reconstr. Surg. Glob. Open 2020, 8, e2733. [Google Scholar] [CrossRef]
- Meuli, J.N.; Hubner, M.; Martineau, J.; Oranges, C.M.; Guillier, D.; Raffoul, W.; di Summa, P.G. Impact of etiology leading to abdominoperineal resection with anterolateral thigh flap reconstruction: A retrospective cohort study. J. Surg. Oncol. 2023, 127, 40–47. [Google Scholar] [CrossRef]
- Nthumba, P. Versatility of the Pedicled ALT Flap in Defect Reconstruction: Experience of a Unit in Rural Sub-Saharan African. Ann. Afr. Surg. 2018, 15. [Google Scholar] [CrossRef][Green Version]
- Lin, C.T.; Wang, C.H.; Ou, K.W.; Chang, S.; Dai, N.; Chen, S.; Chen, T.; Tzeng, Y. Clinical applications of the pedicled anterolateral thigh flap in reconstruction. ANZ J. Surg. 2017, 87, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Yu, P.; Sanger, J.R.; Matloub, H.S.; Gosain, A.; Larson, D. Anterolateral Thigh Fasciocutaneous Island Flaps in Perineoscrotal Reconstruction. Plast. Reconstr. Surg. 2002, 109, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Gravvanis, A.I.; Tsoutsos, D.A.; Iconomou, T.G.; Papadopoulos, S.G. Penile Resurfacing with Vascularized Fascia Lata. J. Urol. 2006, 175, 594. [Google Scholar] [CrossRef]
- Rashid, M.; Aslam, A.; Malik, S.; Tamimy, M.S.; Haq, E.U.; Aman, S.; Jamy, O. Clinical applications of the pedicled anterolateral thigh flap in penile reconstruction. J. Plast. Reconstr. Aesthet. Surg. 2011, 64, 1075–1081. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Yang, Z.; Ma, N.; Wang, W.; Li, Y. Urethra Reconstruction and Revision Urethroplasty in Pedicled Anterolateral Thigh Flap Penile Reconstruction. Ann. Plast. Surg. 2022, 89, 201–206. [Google Scholar] [CrossRef]
- Cao, Z.; Liu, L.; Yang, Z.; Li, Y.; Jiao, H.; Zhang, T.; Zhou, L. The pedicled gracilis muscle combined with the fascia lata: A preliminary clinical study of a new biomimetic dynamic phalloplasty method. J. Sex. Med. 2023, 20, 573–579. [Google Scholar] [CrossRef]
- Robinson, I.; Chao, B.W.; Blasdel, G.; Levine, J.P.; Bluebond-Langner, R.; Zhao, L.C. Anterolateral Thigh Phalloplasty with Staged Skin Graft Urethroplasty: Technique and Outcomes. Urology 2023, 177, 204–212. [Google Scholar] [CrossRef]
- Lumen, N.; Monstrey, S.; Ceulemans, P.; van Laecke, E.; Hoebeke, P. Reconstructive Surgery for Severe Penile Inadequacy: Phalloplasty with a Free Radial Forearm Flap or a Pedicled Anterolateral Thigh Flap. Adv. Urol. 2008, 2008, 704343. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.K.; Lim, A.F.; Bird, E.T. A novel single-flap technique for total penile reconstruction: The pedicled anterolateral thigh flap. Plast. Reconstr. Surg. 2009, 124, 163–166. [Google Scholar] [CrossRef] [PubMed]
- Descamps, M.J.L.; Hayes, P.M.; Hudson, D.A. Phalloplasty in complete aphallia: Pedicled anterolateral thigh flap. J. Plast. Reconstr. Aesthet. Surg. 2009, 62, e51–e54. [Google Scholar] [CrossRef]
- Sinove, Y.; Kyriopoulos, E.; Ceulemans, P.; Houtmeyers, P.; Hoebeke, P.; Monstrey, S. Preoperative planning of a Pedicled Anterolateral Thigh (ALT) flap for penile reconstruction with the multidetector CT scan. Handchir. Mikrochir. Plast. Chir. 2013, 45, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.F.; Liu, C.Y.; Qu, C.Y.; Lu, L.-X.; Liu, A.-T.; Zhu, L.; Wang, H.; Lin, Z.-H.; Zhao, Y.-Z.; Zhu, X.-H.; et al. Is vaginal mucosal graft the excellent substitute material for urethral reconstruction in female-to-male transsexuals? World J. Urol. 2015, 33, 2115–2123. [Google Scholar] [CrossRef] [PubMed]
- D’Arpa, S.; Colebunders, B.; Stillaert, F.; Monstrey, S. Pre-expanded Anterolateral Thigh Perforator Flap for Phalloplasty. Clin. Plast. Surg. 2017, 44, 129–141. [Google Scholar] [CrossRef]
- van der Sluis, W.B.; Smit, J.M.; Pigot, G.L.S.; Buncamper, M.E.; Winters, H.A.; Mullender, M.G.; Bouman, M. Double flap phalloplasty in transgender men: Surgical technique and outcome of pedicled anterolateral thigh flap phalloplasty combined with radial forearm free flap urethral reconstruction. Microsurgery 2017, 37, 917–923. [Google Scholar] [CrossRef] [PubMed]
- Ascha, M.; Massie, J.P.; Morrison, S.D.; Crane, C.N.; Chen, M.L. Outcomes of Single Stage Phalloplasty by Pedicled Anterolateral Thigh Flap versus Radial Forearm Free Flap in Gender Confirming Surgery. J. Urol. 2018, 199, 206–214. [Google Scholar] [CrossRef] [PubMed]
- D’Arpa, S.; Claes, K.; Lumen, N.; Oieni, S.; Hoebeke, P.; Monstrey, S. Urethral Reconstruction in Anterolateral Thigh Flap Phalloplasty: A 93-Case Experience. Plast. Reconstr. Surg. 2019, 143, 382e–392e. [Google Scholar] [CrossRef] [PubMed]
- Sinatti, C.; Wolff, D.; Buncamper, M.; Verla, W.; Claes, K.; Lumen, N.; Waterloos, M.; Monstrey, S.; Hoebeke, P.; Spinoit, A.-F. Phalloplasty in biological men with penile insufficiency. J. Pediatr. Urol. 2020, 16, 404–405. [Google Scholar] [CrossRef] [PubMed]
- Terrell, M.; Roberts, W.; Price, C.W.; Slater, M.; Loukas, M.; Schober, J. Anatomy of the pedicled anterolateral thigh flap for phalloplasty in transitioning-males. Clin. Anat. 2018, 31, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Xu, K.Y.; Watt, A.J. The Pedicled Anterolateral Thigh Phalloplasty. Clin. Plast. Surg. 2018, 45, 399–406. [Google Scholar] [CrossRef]
- Morrison, S.D.; Son, J.; Song, J.; Berger, A.; Kirby, J.; Ahdoot, M.; Lee, G.K. Modification of the Tube-in-Tube Pedicled Anterolateral Thigh Flap for Total Phalloplasty. Ann. Plast. Surg. 2014, 72 (Suppl. S1), S22–S26. [Google Scholar] [CrossRef] [PubMed]
- Nahai, F.; Silverton, J.S.; Hill, H.L.; Vasconez, L.O. The tensor fascia lata musculocutaneous flap. Ann. Plast. Surg. 1978, 1, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.T.; Chang, K.P.; Lin, S.D.; Lai, C.S.; Yang, Y.L. Tensor fasciae latae combined with tangentially split vastus lateralis musculocutaneous flap for the reconstruction of pressure sores. Ann. Plast. Surg. 2004, 53, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Bovet, J.L.; Nassif, T.M.; Guimberteau, J.C.; Baudet, J. The Vastus Lateralis Musculocutaneous Flap in the Repair of Trochanteric Pressure Sores. Plast. Reconstr. Surg. 1982, 69, 830–834. [Google Scholar] [CrossRef] [PubMed]
- Drimmer, M.A.; Krasna, M.J. The Vastus Lateralis Myocutaneous Flap. Plast. Reconstr. Surg. 1987, 79, 560–564. [Google Scholar] [CrossRef] [PubMed]
- Waterhouse, N.; Healy, C. Vastus lateralis myocutaneous flap for reconstruction of defects around the groin and pelvis. Br. J. Surg. 1990, 77, 1275–1277. [Google Scholar] [CrossRef]
- Tzeng, Y.S.; Yu, C.C.; Chou, T.D.; Chen, T.M.; Chen, S.G. Proximal Pedicled Anterolateral Thigh Flap for Reconstruction of Trochanteric Defect. Ann. Plast. Surg. 2008, 61, 79–82. [Google Scholar] [CrossRef]
- Tzeng, Y.S.; Chang, S.C.; Dai, N.T.; Deng, S.C.; Wang, C.H.; Chen, T.M.; Chen, S.G. Versatile application of pedicled anterolateral thigh flaps in reconstruction. J. Med. Sci. Taiwan 2013, 33, 177–182. [Google Scholar] [CrossRef]
- Wang, C.H.; Chen, S.Y.; Fu, J.P.; Dai, N.-T.; Chen, S.-L.; Chen, T.-M.; Chen, S.-G. Reconstruction of trochanteric pressure sores with pedicled anterolateral thigh myocutaneous flaps. J. Plast. Reconstr. Aesthet. Surg. 2011, 64, 671–676. [Google Scholar] [CrossRef] [PubMed]
- Li, C.C.; Chang, S.C.; Fu, J.P.; Tzeng, Y.-S.; Wang, C.-H.; Chen, T.-M.; Chen, S.-G. Comparison of Hatchet-Shaped Tensor Fascia Lata Flap and Pedicle Anterior Lateral Thigh Flap for Treatment of Trochanteric Sores. Ann. Plast. Surg. 2013, 71, 659–663. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.T.; Cheng, L.F.; Lin, C.M.; Wang, C.H.; Huang, C.C.; Chien, S.H. A new technique of transferring island pedicled anterolateral thigh and vastus lateralis myocutaneous flaps for reconstruction of recurrent ischial pressure sores. J. Plast. Reconstr. Aesthet. Surg. 2007, 60, 1060–1066. [Google Scholar] [CrossRef]
- Acartürk, T.O. Treatment of large ischial ulcers communicating with the hip joint with proximal femoral resection and reconstruction with a combined vastus lateralis, vastus intermedius and rectus femoris musculocutaneous flap. J. Plast. Reconstr. Aesthet. Surg. 2009, 62, 1497–1502. [Google Scholar] [CrossRef]
- Batdorf, N.J.; Lettieri, S.C.; Saint-Cyr, M. Trans-vastus intermedius transfer of the pedicled anterolateral thigh flap for posterior thigh reconstruction. Plast. Reconstr. Surg. 2013, 1, e81. [Google Scholar] [CrossRef] [PubMed]
- Santanelli di Pompeo, F.; Longo, B.; Pagnoni, M.; Laporta, R. Sensate anterolateral thigh perforator flap for ischiatic sores reconstruction in meningomyelocele patients. Microsurgery 2015, 35, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.A.; Lozano-Calderon, S.A.; Berner, E.A.; Austen, W.G.; Winograd, J.M.; Park, H.Y.; Bernthal, N.M.; Crawford, B.M.; Hornicek, F.J. Pedicled vastus lateralis myocutaneous flap for sacropelvic defects after wide oncologic resection: Wound complications and outcomes. J. Surg. Oncol. 2022, 126, 978–985. [Google Scholar] [CrossRef] [PubMed]
- Madsen, C.B.; Sørensen, J.A. Versatility of the pedicled anterolateral thigh flap for surgical reconstruction, a case series. JPRAS Open 2020, 25, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Jakubietz, R.; Jakubietz, M.; Vater, A.; Kocot, A.; Kübler, H.; Kalogirou, C. Complex Soft Tissue Defects in Operative Urology: Pedicled Perforator Flaps of the Anterior Lateral Thigh for Tissue Reconstruction of the Lower Trunk. Urol. Int. 2021, 105, 477–482. [Google Scholar] [CrossRef] [PubMed]
- Acartürk, T.O.; Bengür, F.B. individually tailored approach to reconstruction of complex defects using versatility of the lateral circumflex femoral artery system-based pedicled flaps. J. Plast. Reconstr. Aesthet. Surg. 2022, 75, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Scaglioni, M.F.; Meroni, M.; Fuchs, B.; Knobe, M.; Fritsche, E. The use of the chimeric conjoint flap technique for complex defects reconstruction throughout the body: Clinical experience with 28 cases. Microsurgery 2023, 43, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Cammarata, E.; Toia, F.; Maltese, M.; Rossi, M.; Tripoli, M.; Cordova, A. Soft tissue reconstruction of the trunk with pedicled perforator and musculocutaneous flaps: A single-center comparative retrospective study. Microsurgery 2024, 44, e31131. [Google Scholar] [CrossRef] [PubMed]
- McGuire, C.; Samargandi, O.A.; Corkum, J.; Retrouvey, H.; Bezuhly, M. Meta-Analyses in Plastic Surgery: Can We Trust Their Results? Plast. Reconstr. Surg. 2019, 144, 519–530. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).