Abstract
Background: Skeleton involvement is one of the most significant aspects of Gaucher disease (GD). However, the treatment for spinal involvement in GD among patients undergoing enzyme replacement therapy (ERT) is poorly characterized. We present a case of progressive kyphotic spinal deformity in a young child caused by vertebral involvement, which was managed by posterior spinal fusion without anterior spinal release under ERT. Case presentation: This is a retrospective study. A 10-year-old boy presenting with progression kyphosis (thoracic kyphotic angle of 113°) associated with type-IIIb GD had undergone posterior spinal fusion with segmental pedicle screw fixation (from T6-L3) and Ponte osteotomy. The patient went back to school without further brace protection. Proximal junctional kyphosis (PJK) was observed at 4 months postoperatively. Revision surgery was performed to prevent neurological impairment. Additional posterior spinal fusion from T2–T6 and decompressive laminectomy were performed during the revision surgery. A 2-year follow-up showed no recurrence of PJK and solid fusion was achieved in the patient under ERT and brace protection. Conclusions: Posterior spinal fusion without anterior spinal release is a good treatment option for severe spinal deformity in patients with GD. However, the fusion level and reinforced fixation require careful consideration. Revision surgery and brace protection is needed as long as PJK is observed.
1. Introduction
Gaucher disease (GD) was first reported in 1882 by a French dermatologist, Philippe Gaucher, in a patient with massive splenomegaly without leukemia. It is characterized by massive splenomegaly and thrombocytopenia due to the deficiency of the glucosidase enzyme [1]. In the human glucocerebrosidase gene (chromosome 1q22) [2], 250 mutations responsible for this enzymatic deficiency have been identified. Previous reports show that the four most common mutations observed in 90% of the disease alleles are N370S, 84GG, L444P, and IVS2+1 [3]. GD is divided into three types: chronic (type I, non-neurological), acute (type II, acute neuronopathic), and subacute (type III, chronic neuronopathic). Meanwhile, according to clinical manifestations of the subacute type, type III GD is classified as IIIa (progressive myoclonus and dementia), IIIb (horizontal gaze paralysis, short stature, suboptimal bodyweight, and prone to cardiopulmonary, liver, and bone complications), and IIIc (cardiac valve calcification) [4,5].
Involvement of the skeleton is common in GD, which primarily causes pain, disability, and a reduced quality of life. In particular, spinal involvement in GD among patients undergoing enzyme replacement therapy (ERT) is poorly characterized. We present a case of progressive kyphotic spinal deformity in a young child (type IIIb) caused by vertebral involvement, which was managed only by posterior spinal fusion under ERT. To date, few studies have described the surgical correction of spinal deformities in patients with GD under ERT.
2. Case Presentation
A 10-year-old boy (weight, 23 kg; height, 123 cm; and body mass index, 13.33 kg/m2) was referred to us in 2019 with a diagnosis of type-III GD. Thrombocytopenia was detected in the patient and a β-glucocerebrosidase (GCase) level of 1.54 nmol/h.mg was detected. He had undergone splenectomy in 2012 and had been administered 1200 units of imiglucerase once every 2 weeks since 2015. He had no history of bone crisis, pathologic fractures, or osteomyelitis. Deterioration of the thoracic kyphosis (TK) was noted in July 2017, but no rigid bracing was used. Thereafter, the deformity increased rapidly, leading to a kyphosis of 113° in 2019 (Figure 1A). Pain developed over the apex of his deformity, and he started to have difficulty walking, with lower extremity weakness (3+/5–4/5). Moreover, the boy suffered from moderate horizontal gaze palsy and sternum deformity. Genetic testing indicated heterogeneity for the gene mutations c.1448T>C and c.1205A>G. There were no signs of pulmonary dysfunction or myelopathy. The patient had mild anemia with normal platelet counts and blood clotting. Radiographs were obtained, which revealed a Cobb angle of TK as 113° (Figure 1A). Computed tomography (CT) and magnetic resonance imaging (MRI) revealed inflammation of the mesenteric lymph nodes and anterior wedging of the vertebrae from T7 to T10. The patient was diagnosed as having spinal kyphosis deformity, type IIIb GD, and sternal lordosis.
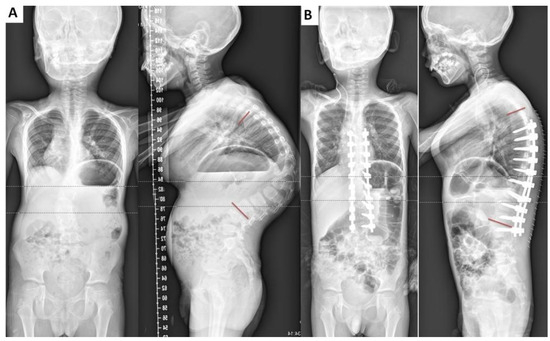
Figure 1.
Case: A 10-year-old boy. (A) Preoperative Cobb angle of thoracic kyphosis (TK): 113°, anterior wedging is observed in the T7-T10 vertebrae (TK: 113°, LL: 67°, PI: 45°, PI-LL: −22°, sagittal vertical axis [SVA]: 58 mm). (B) We performed posterior spinal fusion with a pedicle screw construct from T6 to L3. Postoperative Cobb angle of TK angle improved to 43° (TK: 43°, LL: 38°, PI: 45°, PI-LL: 7°, SVA: 39 mm).
After anesthesia was induced, the child was placed in the prone position without compression of the sternum. After the pedicle screws had been implanted from T6 to L3, Smith–Peterson osteotomies were performed at five levels (T8–L1). The surgical time was 180 min, and blood loss was 300 mL. Intraoperative monitoring with neurogenic or transcranial motor-evoked potentials were used during every procedure. Correction of the segmental kyphotic angle was achieved (70°) after the first surgery, yielding a 61% correction rate (TK, 43°; lumbar lordosis [LL], 38°; pelvic incidence [PI], 45°; PI-LL: −7°, sagittal vertical axis [SVA], 39 mm).
The patient went back to school without further brace protection. He was administered 1200 units of imiglucerase once every 2 weeks as before. However, proximal junctional kyphosis (PJK) was observed 4 months postoperatively (PJA, 55°). Revision surgery was performed to prevent neurological impairment. During the revision surgery, we initially placed the screws in T2–T5 and then removed the screws of T6, after which laminectomy was performed, and a domino linkage system was used to link the internal fixation (Figure 2D; TK: 60°, LL: 45°, PI: 45°, PI-LL: 0°, SVA:67 mm). The surgical time was 195 min, and blood loss was 200 mL. We tried to mobilize the boy on the following day and discharged him on the fourth day after the revision surgery. He used brace protection for 5 months and was followed up at 3 months, 5 months, and 2 years. X-rays were repeated at the 2-year follow-up, which showed no obvious recurrence of PJK and solid fusion was achieved (Figure 3; PJA, 19°, TK: 60°, LL: 50°, PI: 45°, PI-LL: −5°, SVA: −30 mm).
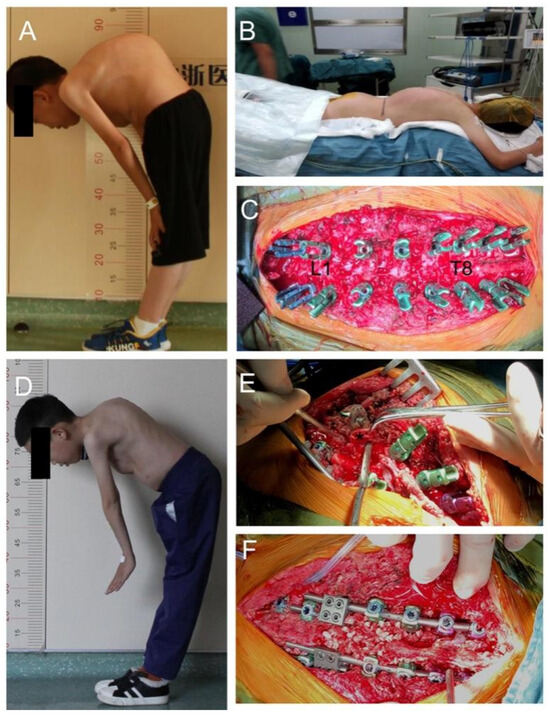
Figure 2.
Perioperative images of the patient: (A) lateral photograph before the first surgery; (B) protection from sternum compression intraoperatively because of the deformity; (C) Smith–Peterson osteotomies are performed at five levels (T8–T9, T9–T10, T11–T12, T12–L1, L1–L2); (D) lateral photograph showing the proximal junctional kyphosis (PJK) at 4 months postoperatively; (E) removal of T6 screws and laminectomy (* indicates the lamina of T6); (F) additional posterior spinal fusion from T2–T6 to correct the PJK during the revision surgery.
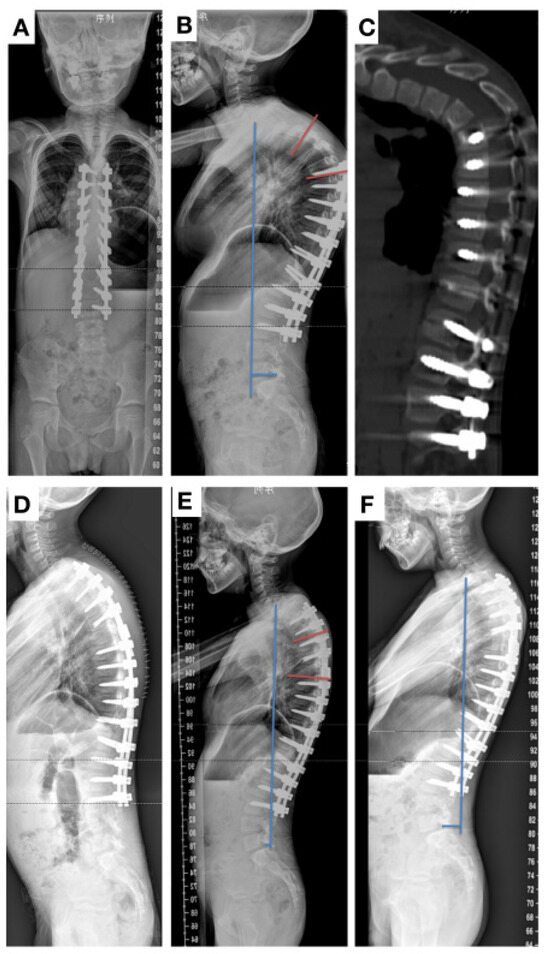
Figure 3.
(A,B) Radiographs obtained 4 months after surgery showing a proximal junctional kyphosis (PJK) angle of 55°. (C) Postoperative computed tomography demonstrated severe PJK. (D) Additional posterior fusion from T2 to T6 was performed; postoperative radiographs showed PJK angle reduced to 12° after the second surgery (TK: 60°, LL: 45°, PI: 45°, PI-LL: 0°, SVA: 67 mm). (E,F) Plain radiographs showing that no PJK occurred after 5 and 24 months of follow up (TK: 60°, LL: 62°, PI: 45°, PI-LL: −17°, SVA: 16 mm).
Hematoxylin–eosin staining and immunohistochemistry analysis were performed for CD68 (M1-type macrophages) and CD206 (M2-type macrophages) in the resected lamina of the patient and compared with those of a 14 year-old healthy boy (control). An increased expression of CD68 but lower expression of CD206 was observed in the cancellous bone of the patient (Figure 4).
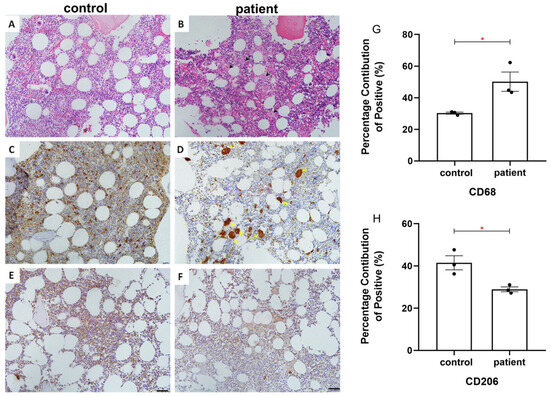
Figure 4.
Hematoxylin–eosin staining and immunohistochemistry of CD68 and CD206 in the lamina of a 14-year-old boy (control, (A,C,E)) and the patient (B,D,F). (A,B) H&E staining; black arrows indicate Gaucher cells. (C,D) Immunohistochemistry of CD68; higher intensity of CD68 is observed in Gaucher cells (yellow arrows). (E,F) Immunohistochemistry of CD206. Fewer CD206-positive cells are found in the vertebral lamina of the patient than in the normal child. (G,H) The percentage of CD68- and CD206-positive cells was statistically assessed in both groups. p-values were indicated (* p ≤ 0.05; scale bar = 50 μm).
3. Discussion
TK may develop in any patient with GD from previous vertebral fragility fractures due to low bone mass and the infiltration of Gaucher cells [6,7]. Such cases generally deteriorate progressively, and orthodontic treatment is often ineffective [8,9]. We found only nine cases in five reports from 1983 to 2021; the details of these nine cases are summarized in Table 1. There were six males and three females, with a mean age of 14.3 years (range, 10–31 years). Most patients presenting with back pain and lower extremity weakness, except two patients, had definite signs of neurological deficit, which could be explained by spinal cord compression. The combined strategy with anterior discectomy and posterior spinal fusion were used for most cases (7/9). Ruff et al. treated a 12-year-old girl with GD who had progressive kyphosis (Cobb angle, 65°) by staged anterior discectomy and T11 vertebrectomy with rib grafting, followed by posterior spinal fusion with segmental instrumentation of T8-L3 [10], and reported good outcomes. Katz et al. reported a case of a 31-year-old man with kyphotic deformity at T12 with myelopathy and complete myelopgraphic block. Decompressive laminectomies over the apex of the deformity were performed [11]. Wiesner et al. treated a 12-year-old boy with a collapse of three consecutive vertebral bodies (T7−T9) and created a global kyphosis of 90°. Ventral decompression was performed and the spine was stabilized by a TSRH-System from T5–L2 [12]. Mininder et al. reported four children and adolescents with GD who developed a TK angle of 70–120°; two of them were associated with neurologic compromise, which were managed by anterior spinal release in cases of spinal cord compromise at the apex of the kyphotic deformity [7].
Posterior fusion without anterior spinal release was used for the correction of severe kyphosis with Ponte osteotomy. We performed posterior fusion from T6 to L3 and achieved adequate correction after the first operation (TK angle decreased from 113° to 43°; Figure 1B). The child returned to school 1 month postoperatively without further bracing. However, the child experienced difficulties while lifting his head at 4 months post operation and proximal junctional kyphosis (PJK angle [PJA], 55°) was detected without neurological impairment (Figure 2D and Figure 3A–C).
The overall incidence of PJK in pediatric and adolescent patients is estimated to be 11%, with a range of 0–55% [13,14], while in children with early-onset scoliosis, the prevalence of PJK is much higher (48.9%) [15]. No standards on the selection of fusion levels and instrumentation by posterior fusion in previous studies have been suggested for patients with GD [16,17]. We initially sought to preserve the T2–T6 interspinous ligament during the first surgery, although PJK developed soon after. According to the classification of PJK [18], the type of PJK in this case was 1CN. Therefore, additional posterior spinal fusion from T2–T6 and decompressive laminectomy were performed during the revision surgery.

Table 1.
Summary of Gaucher disease-associated spinal deformity cases corrected by surgery in the English literature.
Table 1.
Summary of Gaucher disease-associated spinal deformity cases corrected by surgery in the English literature.
| Report | Age (Years)/Sex | Disease Type | Presentation | Vertebrate Collapse (Site) | Complications | Treatment | Follow-Up | Outcome |
|---|---|---|---|---|---|---|---|---|
| Ruff et al., 1984 [10] | 12/F | Not available | Back pain | T11 | Progressive kyphosis of 64° | Anterior discectomies and T11 vertebrectomy, posterior spinal fusion of T8–L3 | Not available | Not available |
| Katz et al., 1993 [11] | 31/M | Not available | Back pain and lower extremity weakness | T12, L4 | Cord compression, hemorrhage | Laminectomy | 7 weeks | Died of gastric hemorrhage and bronchopneumonia |
| 17/M | Not available | Back pain | T5, T7, T12, L1–L5 | Kyphoscoliosis, cord compression | Brace, laminectomy, spinal fusion | Not available | Not available | |
| Kocher et al., 2000 [7] | 18/M | Type I | Lower extremity weakness and stumbling gait | T8–T12 | Cord compression and edema at the apex of the kyphosis | Anterior decompression and posterior fusion | 5 years | Good outcome |
| 11/M | Type 3 | Back pain and lower extremity weakness | Midthoracic spine | A thoracic kyphosis of ~120° and flattening of the cord | Anterior discectomies and fusion of T2–T11, posterior spinal fusion of T1–L3 | 19 months | Solid fusion with normal strength and sensation | |
| 13/M | Type 3 | Back pain | T6 and T10 | A thoracic kyphosis of 94° | Anterior discectomies and fusion of T8–L2, posterior spinal fusion of T5–L3 | 18 months | Maintenance of correction and solid fusion | |
| 15/F | Type 3 | Back pain | T5 and T10 | A thoracic kyphosis of 70° and slight cord impingement | Anterior discectomies and fusion of T8–T11, posterior spinal fusion of T2–L2 | 1 year | Good outcome and solid fusion | |
| Wiesner et al., 2003 [12] | 12/M | Type I | Back pain | T7–T9 | No complications | Ventral decompression with bone graft and fusion with TSRH(T5–L2) | 5 years | Good outcome |
| Ito et al., 2017 [17] | 10/F | Not available | Lower extremity weakness | No collapse | Kyphosis of 84° between T6 and L3 | T3–L3 posterior fusion with T12 osteotomy and anterior fusion from T12–L3 with bone grafts | 6 years | No progression of kyphosis, but suffered from fracture of limbs |
The histological and immunohistochemical evaluation of the resected vertebral lamina showed osseous manifestation of GD, with a positive reaction of histiocytes to CD68 and CD206 (Figure 4). Our immunohistological staining analysis revealed a higher expression of CD68 (M1-type macrophages) but lower expression of CD206 (M2-type macrophages) in the cancellous bone of the patient than those of the healthy young 14-year-old boy. These results indicated that the infiltration of Gaucher cells may impair the M2 phenotype formation and promote the proinflammatory capacity of macrophages in these patients [19,20].
Our choice of a single-stage posterior fusion approach was based on the patient’s acceptable spinal flexibility, advancements in posterior osteotomy and fusion techniques, and the significant trauma associated with anterior surgery. We conducted posterior fusion from T6 to L3 and achieved satisfactory correction after the initial operation. The occurrence of PJK may be attributed to improper UIV selection and the extensive correction of kyphosis; however, we still consider this a meaningful attempt. After all, for patients with type-IIIb Gaucher disease kyphosis who have been treated with ERT, how to better correct the lateral and posterior convex deformities remains unknown.
4. Conclusions
Based on the present case, posterior spinal fusion without anterior spinal release is a good corrective option for severe spinal kyphosis in patients with GD undergoing ERT. However, the fusion level should be decided carefully because the infiltration of Gaucher cells in the patient’s vertebrate, and reinforced fixation is recommended to prevent PJK even under ERT. Revision surgery and brace protection were needed to prevent neurological involvement, as long as PJK was observed during follow-up.
Author Contributions
All authors contributed to the treatment of this patient. Data collection was performed by J.L. and L.C. The first draft of the manuscript was written by T.Z. T.Z. and N.Z. were involved in the management of the patient. Q.C. and F.L. revised previous versions of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study was financially supported by the National Natural Science Foundation of China (grant nos. 82072481 and 81972096, Li) and the Natural Science Foundation of Zhejiang, China (grant no. LY20H060009, Zhao) for patient follow-up and data collection costs.
Institutional Review Board Statement
This study was approved by the Institutional Review Board of Second Affiliated Hospital of Zhejiang University, School of Medicine (COA number 2022-0125 and date of approval 14 February 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
GD: Gaucher disease; ERT: enzyme replacement therapy; PJK: proximal junctional kyphosis; TK: thoracic kyphosis; LL: lumbar lordosis; PI: pelvic incidence, SVA: sagittal vertical axis, PJA: PJK angle.
References
- Goldblatt, J.; Sacks, S.; Beighton, P. The orthopedic aspects of Gaucher disease. Clin. Orthop. Relat. Res. 1978, 208–214. [Google Scholar] [CrossRef]
- Grabowski, G.A. Phenotype, diagnosis, and treatment of Gaucher’s disease. Lancet 2008, 372, 1263–1271. [Google Scholar] [CrossRef] [PubMed]
- Erdos, M.; Hodanova, K.; Taskó, S.; Palicz, A.; Stolnaja, L.; Dvorakova, L.; Hrebicek, M.; Maródi, L. Genetic and clinical features of patients with Gaucher disease in Hungary. Blood Cells Mol. Dis. 2007, 39, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Abrahamov, A.; Elstein, D.; Gross-Tsur, V.; Farber, B.; Glaser, Y.; Hadas-Halpern, I.; Ronen, S.; Tafakjdi, M.; Horowitz, M.; Zimran, A. Gaucher’s disease variant characterised by progressive calcification of heart valves and unique genotype. Lancet 1995, 346, 1000–1003. [Google Scholar] [CrossRef] [PubMed]
- Patterson, M.C.; Horowitz, M.; Abel, R.B.; Currie, J.N.; Yu, K.T.; Kaneski, C.; Higgins, J.J.; O’Neill, R.R.; Fedio, P.; Pikus, A.; et al. Isolated horizontal supranuclear gaze palsy as a marker of severe systemic involvement in Gaucher’s disease. Neurology 1993, 43, 1993–1997. [Google Scholar] [CrossRef] [PubMed]
- Hughes, D.; Mikosch, P.; Belmatoug, N.; Carubbi, F.; Cox, T.; Goker-Alpan, O.; Kindmark, A.; Mistry, P.; Poll, L.; Weinreb, N.; et al. Gaucher Disease in Bone: From Pathophysiology to Practice. J. Bone Miner. Res. 2019, 34, 996–1013. [Google Scholar] [CrossRef] [PubMed]
- Kocher, M.S.; Hall, J.E. Surgical management of spinal involvement in children and adolescents with Gaucher’s disease. J. Pediatr. Orthop. 2000, 20, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, P.; Andersson, H.C.; Kacena, K.A.; Yee, J.D. The clinical and demographic characteristics of nonneuronopathic Gaucher disease in 887 children at diagnosis. Arch. Pediatr. Adolesc. Med. 2006, 160, 603–608. [Google Scholar] [CrossRef] [PubMed]
- Stirnemann, J.; Belmatoug, N.; Camou, F.; Serratrice, C.; Froissart, R.; Caillaud, C.; Levade, T.; Astudillo, L.; Serratrice, J.; Brassier, A.; et al. A Review of Gaucher Disease Pathophysiology, Clinical Presentation and Treatments. Int. J. Mol. Sci. 2017, 18, 441. [Google Scholar] [CrossRef] [PubMed]
- Ruff, M.E.; Weis, L.D.; Kean, J.R. Acute thoracic kyphosis in Gaucher’s disease. A case report. Spine 1984, 9, 835–837. [Google Scholar] [CrossRef] [PubMed]
- Katz, K.; Sabato, S.; Horev, G.; Cohen, I.J.; Yosipovitch, Z. Spinal involvement in children and adolescents with Gaucher disease. Spine 1993, 18, 332–335. [Google Scholar] [CrossRef] [PubMed]
- Wiesner, L.; Niggemeyer, O.; Kothe, R.; Meiss, L. Severe pathologic compression of three consecutive vertebrae in Gaucher’s disease: A case report and review of the literature. Eur. Spine J. 2003, 12, 97–99. [Google Scholar] [CrossRef] [PubMed]
- Yan, C.; Li, Y.; Yu, Z. Prevalence and Consequences of the Proximal Junctional Kyphosis after Spinal Deformity Surgery: A Meta-Analysis. Medicine 2016, 95, e3471. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Chen, Z.H.; Qiu, Y.; Zhu, Z.Z.; Li, S.; Xu, L.; Sun, X. Proximal Junctional Kyphosis after Posterior Spinal Instrumentation and Fusion in Young Children With Congenital Scoliosis: A Preliminary Report on its Incidence and Risk Factors. Spine 2017, 42, E1197–E1203. [Google Scholar] [CrossRef] [PubMed]
- Piantoni, L.; Remondino, R.G.; Tello, C.A.; Wilson, I.A.F.; Galaretto, E.; Noel, M.A. Proximal junction kyphosis after posterior spinal fusion for early-onset scoliosis. Spine Deform. 2020, 8, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Mika, A.P.; Mesfin, A.; Rubery, P.T.; Molinari, R.; Kebaish, K.M.; Menga, E.N. Proximal Junctional Kyphosis: A Pediatric and Adult Spinal Deformity Surgery Dilemma. JBJS Rev. 2019, 7, e4. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; Kawakami, N.; Tsuji, T.; Ohara, T.; Saito, T.; Tauchi, R.; Morishita, K. Corrective surgery for kyphosis in a case of Gaucher’s disease without history of vertebral compression fractures. Spine Surg. Relat. Res. 2017, 1, 222–224. [Google Scholar] [CrossRef] [PubMed]
- Yagi, M.; King, A.B.; Boachie-Adjei, O. Incidence, risk factors, and natural course of proximal junctional kyphosis: Surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine 2012, 37, 1479–1489. [Google Scholar] [CrossRef] [PubMed]
- Messelodi, D.; Bertuccio, S.N.; Indio, V.; Strocchi, S.; Taddia, A.; Serravalle, S.; Bandini, J.; Astolfi, A.; Pession, A. iPSC-Derived Gaucher Macrophages Display Growth Impairment and Activation of Inflammation-Related Cell Death. Cells 2021, 10, 2822. [Google Scholar] [CrossRef] [PubMed]
- Kacher, Y.; Futerman, A.H. Impaired IL-10 transcription and release in animal models of Gaucher disease macrophages. Blood Cells Mol. Dis. 2009, 43, 134–137. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).