1. Introduction
Radial head fractures comprise approximately one-third of all elbow fractures, with up to one-third of these cases involving concurrent fractures of adjacent elbow structures such as the capitellum, coronoid process, and proximal ulna [
1,
2]. Surgical management is typically indicated for displaced radial head fractures that lead to a mechanical block. Non-reducible, comminuted fractures of the radial head are most often treated with radial head arthroplasty (RHA), especially if the trauma has also resulted in concomitant instability of the elbow [
3].
Monteggia fractures are relatively rare and account for only 2–5% of all proximal forearm fractures [
3]. This injury is characterized by a proximal ulnar fracture accompanied by a radial ligamentous failure and a subsequent radial head dislocation [
4,
5]. Concurrent fractures of the radial head and proximal ulna are a unique entity, defined as Monteggia-equivalent (or Monteggia-like) fractures [
3,
5,
6,
7].
Considering the rarity of these injuries, evidence-based treatment guidelines are relatively scarce [
6]. Together with their technically demanding nature, Monteggia-equivalent fractures continue to pose a challenge for orthopedic surgeons [
7,
8].
Key factors for achieving favorable outcomes in Monteggia fractures include the following: first, early identification of the fracture type; second, performing an open reduction and achieving stable internal fixation of the ulna; third, primarily utilizing open reduction in the radial head; and finally, minimizing immobilization time [
6]. The standard treatment for Monteggia dislocation typically involves open reduction and internal fixation of the ulnar fracture, coupled with closed reduction in the radial head.
There are several surgical approaches to the elbow, including the posterolateral Kocher approach, lateral Kaplan approach, extensor digitorum communis splitting techniques, and posterior Boyd approach [
9,
10,
11]. In the context of a Monteggia-equivalent injury, two approaches are most commonly utilized, depending on the requirement for accessing the ulna [
12,
13,
14].
In contrast to the more commonly used two-incisions approach for concurrent radial head and proximal ulna fractures, a single-incision approach involves accessing the radial head through the ulnar fracture followed by fixation of the ulnar fracture. This approach may diminish the soft-tissue dissection while maintaining visibility and control of the various stages of the procedure [
10,
14].
Compared to the traditional two-incisions approach, the evidence for the single, trans-olecranon approach is scarce [
10,
15,
16]. Considering the relatively high complication rate, secondary procedures, and consequently impaired postoperative outcomes associated with Monteggia-equivalent fractures [
7,
17], this study aims to assess the clinical outcomes, radiological measurements, and secondary procedure rates of the single, trans-olecranon approach for RHA in the treatment of Monteggia-equivalent fractures of the radial head and proximal ulna.
2. Methods
A retrospective cohort study was conducted, comprising 45 adults following a Monteggia-equivalent injury with concurrent radial head fractures, spanning from June 2004 to January 2021 at a tertiary trauma center. This analysis focused on cases managed surgically via the trans-olecranon approach with all procedures performed by a single fellowship-trained orthopedic surgeon.
Inclusion criteria were patients older than 18 years presenting with Monteggia-equivalent fractures (classified as Bado type II, Jupiter type IIB, Mason type III) and having undergone a primary concomitant RHA and open reduction and internal fixation (ORIF) of the proximal ulna via the trans-olecranon approach. A summary of inclusion and exclusion criteria is provided in
Table 1.
Evaluated variables included demographic data and clinical parameters (e.g., postoperative range of motion (ROM)).
Reported descriptive radiographic measurements include the following:
Osteolysis defined by thinning of ≥2 mm of the adjacent cortices.
Loosening defined by positional difference on consecutive radiographs.
Erosions of the capitulum assessed by examining the articular surface for signs of wear or degeneration.
Heterotopic ossification was evaluated by identifying abnormal bone formation in and around the joint.
Complications, including infections, uncontrolled pain, ROM limitation, non-union of the ulna, and neurovascular compromise were documented as well. Follow-up endpoint was defined as a revision procedure for any reason.
2.1. The Trans-Olecranon Approach for Monteggia-Equivalent Fractures, Surgical Technique
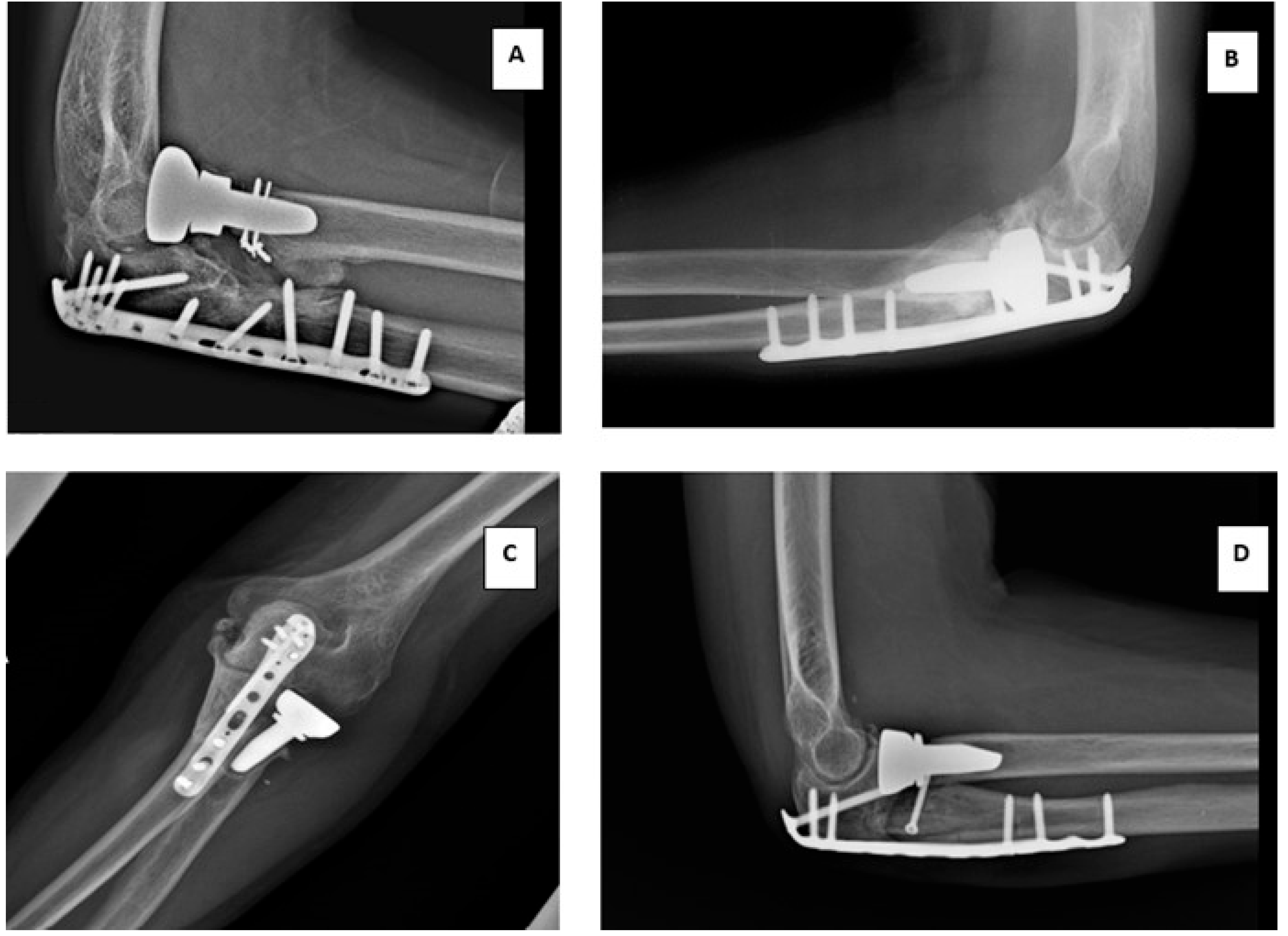
The radiographic presentation of this injury is illustrated in
Figure 1.
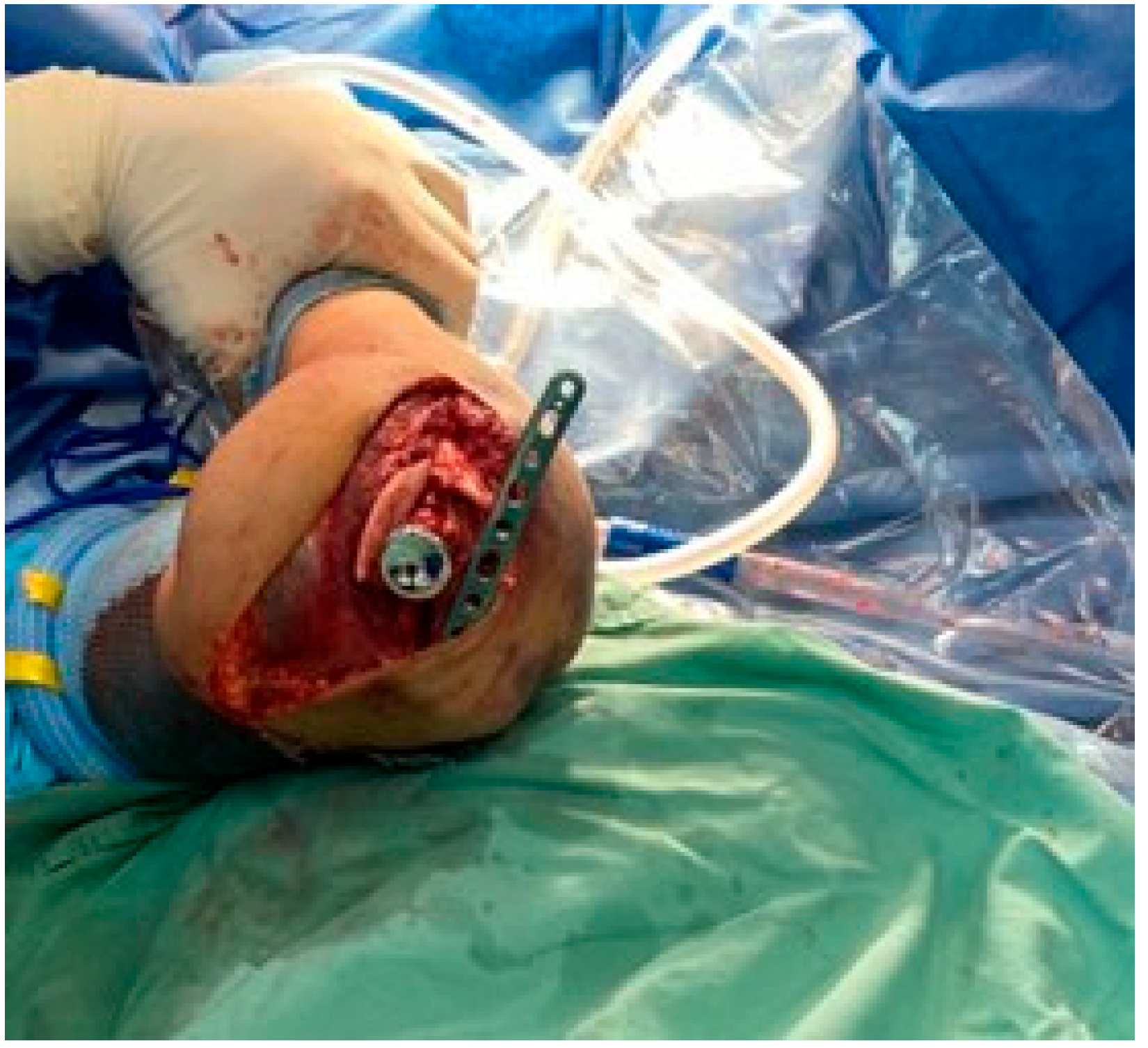
The procedure is typically performed under general anesthesia and peripheral nerve block, with the application of a tourniquet. The patient is lying supine with the operated arm supported on a pillow bolster. A 5 cm skin incision is made proximal to the lateral epicondyle, following the lateral edge of the triceps tendon. The incision then curves distally over the lateral aspect of the olecranon along the subcutaneous edge of the ulna for approximately 7 cm. Subsequently, the deep fascia of the anconeus and extensor carpi ulnaris is identified and longitudinally incised in line with the skin incision (
Figure 2).
Once the olecranon is exposed, the ulnar fracture is temporarily reduced and fixated with Kirschner wires (KWs). Next, an ulnar locking plate is properly sized and secured to the olecranon with a single screw. This screw allows pivoting the plate and accessing the radial head (
Figure 3).
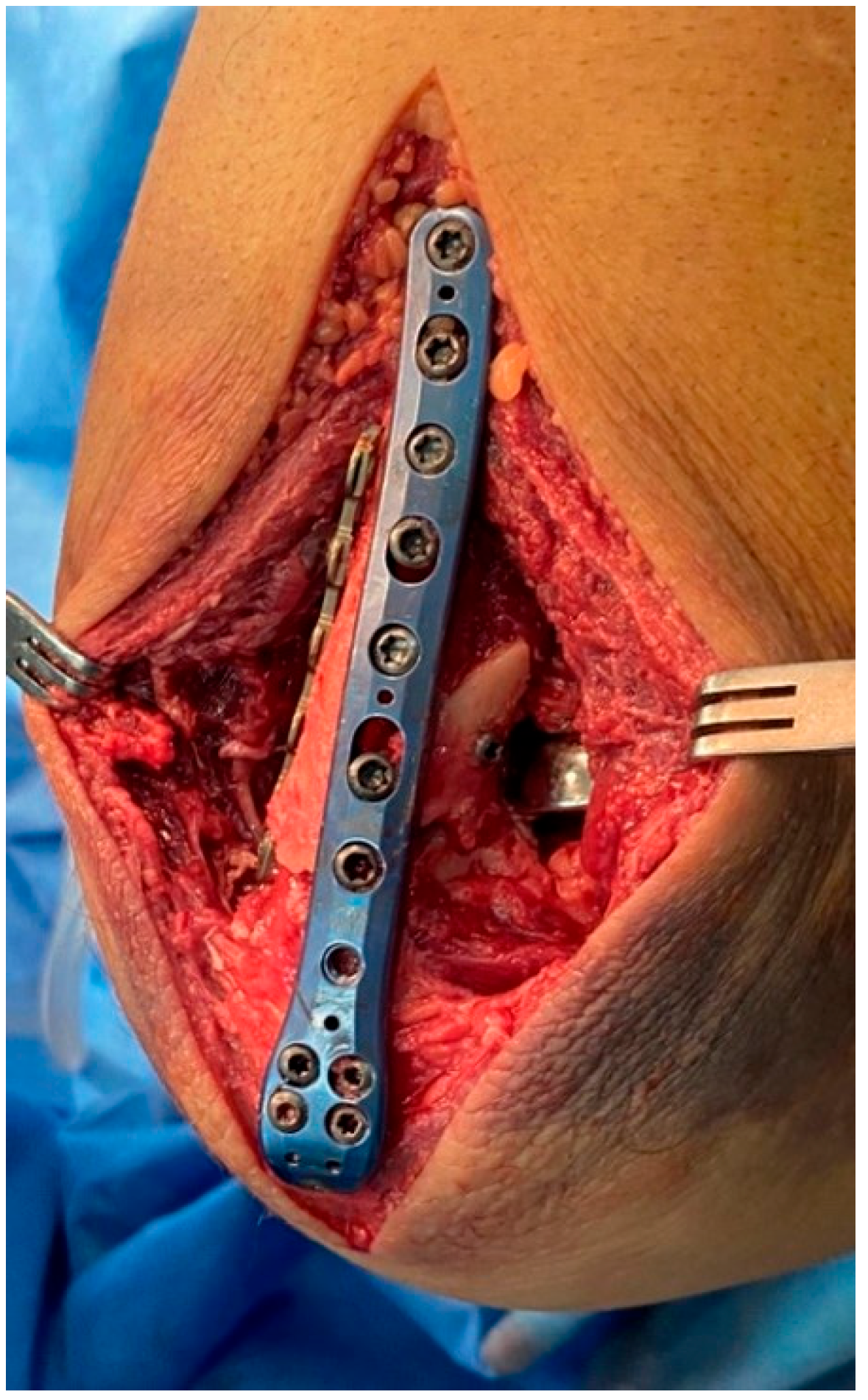
RHA is conducted through the olecranon fracture by pivoting the plate around the proximal screw (
Figure 4). Attention should be given to proper trialing of the radial head prosthesis to avoid overstuffing (assessed by a wide humero-ulnar joint space in intraoperative X-rays, known as “river delta sign” [
18]). Also, proper sizing of the neck is indicated by a visible congruency between the coronoid and the trochlea.
Following placing the final radial head prosthesis, the locking plate is then pivoted and fixated into place with screws (
Figure 5).
2.2. Statistical Analysis
Descriptive statistics in terms of mean, standard deviation, percentiles, and ranges were performed for all continuous variables in this study. For categorical parameters, the Fisher exact test was used. Kaplan–Meier (KM) method of censored data estimation was used to analyze ‘time-to-event’ data. The outcome in KM analysis was defined as the duration between the primary and the secondary procedures. SPSS version 27 was used for all statistical analyses.
3. Results
The final cohort comprised 45 patients who underwent a primary RHA via the trans-olecranon approach, concomitant with internal fixation of the ulnar fracture. Four patients were lost to follow-up. Among them, 22 were male and 23 were female. The mean follow-up, defined as the timeframe from the primary procedure to either the removal or revision of the hardware, was 30 months. For those who did not require a revision procedure, traditionally, these patients typically undergo multiple clinical visits in the months following the initial operation, with subsequent follow-up appointments scheduled on an as-needed basis in the absence of any notable complications. During the post-surgery follow-up visits, ROM and radiological evaluation were documented. The average time between surgery and the functional assessment was 4.53 months. However, in cases where complications necessitating a secondary procedure, such as the removal or replacement of the radial head, arise, the follow-up period is extended accordingly.
The average body mass index (BMI) was 27.70 ± 4.06. The mean age of the patients was 55.6 ± 15.4 years, and the mean duration of hospitalization following the surgical procedure was 4 days. The patient’s demographics are reported in
Table 2.
3.1. Clinical Outcomes and Radiographic Assessment
Recorded mean postoperative ROM was 112.37° ± 13.7° for flexion, 24.27° ± 17.9° for extension, 57.63° ± 28.9° for supination, and 62.16° ± 29.07° for pronation.
In terms of postoperative radiographic measurement, heterotopic ossification was observed in 17 patients (37.7%), erosion of the capitulum in seven patients (15.5%), osteolysis in 10 patients (22.2%), and loosening of the radial head prosthesis in 2 patients (4.4%) (
Table 3). Examples of the radiographic measurements are shown in
Figure 6.
3.2. Secondary Surgeries
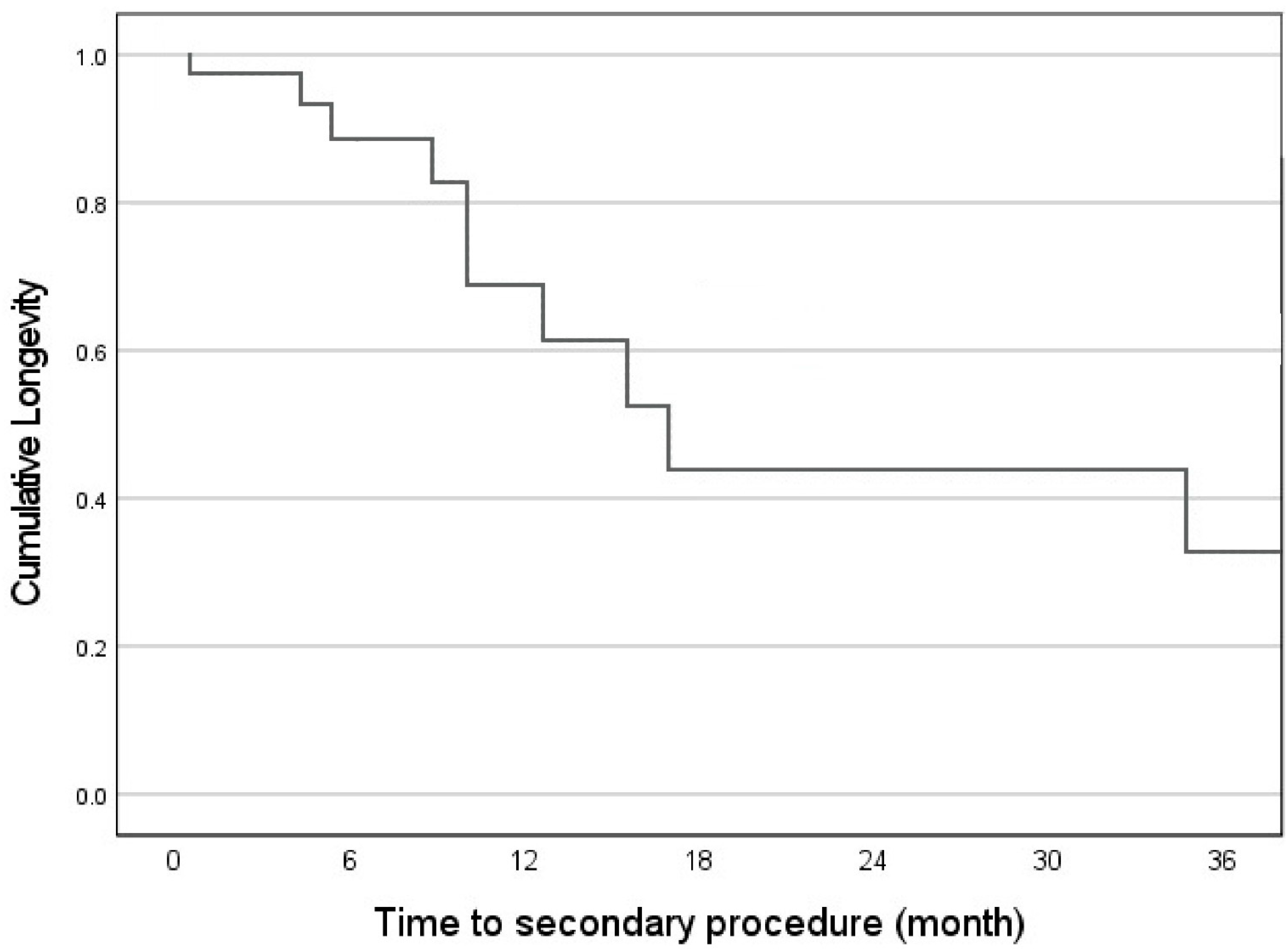
Secondary procedures, defined as follow-up endpoint, have been documented in 16 (24%) of the patients. Of these, 90.9% were for hardware removal. The remaining 9.1% were other revision surgeries.
Figure 7 presents a Kaplan–Meier curve, which is used to estimate the time to the occurrence of secondary procedures. The primary indications for secondary procedures are detailed in
Table 4.
4. Discussion
This study has presented a case series of 45 patients following RHA and ulnar fixation via a single, trans-olecranon approach for a Monteggia-equivalent fracture involving the radial head and proximal ulna. This study tried to shed some light on the benefits of this specific approach by presenting the clinical and radiological outcomes of a relatively large cohort of patients who were treated at a tertiary trauma center by a single surgeon.
This study has investigated the clinical outcomes following the trans-olecranon approach. Colliton et al. [
15] investigated the outcomes of seven patients with Monteggia-equivalent fractures following the trans-olecranon approach. Of these, four patients underwent RHA and two underwent radial head fixation. The authors’ reported average ROM was 133°–13° for flexion–extension, respectively, 76° for pronation and 72° for supination. In this study, the reported average ROM was 112.37° for flexion, 24.27° for extension, 57.63° for supination, and 62.16° for pronation. The trend in disadvantageous ROM in this study may be attributed to the difference in the severity of the injury, reflected by the radial head management (i.e., no treatment, fixation, and RHA in Collion et al.’s study in comparison to RHA for all patients in the current study). Nevertheless, in both studies, patients have achieved functional ROM [
19].
There is no consensus in the literature regarding the significance of postoperative radiographic measures in assessing the longevity of the radial head prosthesis. In their meta-analysis, Kaur et al. [
20] investigated radiographic and clinical outcomes in patients following isolated RHA. Of the 21 enrolled studies, 391 patients underwent RHA. In their study, the overall reported percentages for osteolysis, heterotopic ossification, and capitellar erosions were 36.49%, 26.46%, and 13.09%, respectively. Despite these relatively high percentages, the authors reported good to excellent functional outcomes in the short- to mid-term follow-up. In this study, the radiographic measures were somewhat differently distributed, but the clinical outcome was satisfactory. This finding aligns with some reports in the literature, which suggest that radiological findings may not have a significant impact on clinical outcomes [
20,
21].
It is worth noticing that this study reports a 40% ossification rate in elbow fractures, higher than the 26% commonly cited in the literature, indicating a critical complication that demands attention. Such ossification can be debilitating for patients, affecting mobility and quality of life. Future studies should focus on identifying patients with risk factors for developing this condition.
Additionally, the current study aimed to investigate the occurrence of secondary procedures in patients undergoing an RHA in Monteggia-equivalent fractures accompanying radial head fractures. A study by Konrad et al. [
4] evaluated 47 Monteggia injuries after a mean time of 8 years. Among them, eleven patients suffered a radial head fracture, a fracture of a coronoid process, or a combination of both (Monteggia-like lesions). A 26% secondary procedures rate was noted, with poor clinical outcomes associated with intra-articular radial head and coronoid process fractures. While the specific surgical technique was not elaborated upon, it is noteworthy that the trans-olecranon approach yielded a similar removal or revision rate of 24%. Although this is a hardly satisfactory rate, it is in line with the current literature. Also, it seems that the main indication for secondary surgery is similar to those described in the literature [
22].
This study substantiated the current literature with a relatively large cohort of patients. The trans-olecranon approach for treating Monteggia-equivalent injuries provided a good approach to the proximal ulna and radial head, concomitantly. Notably, this approach demonstrated the potential for minimizing the extent of soft-tissue dissection, thereby promoting a more conservative surgical technique while maintaining visibility. These factors, in conjunction, contributed to achieving satisfactory clinical results.
5. Limitations
While this study provides valuable insights into the trans-olecranon approach for RHA in Monteggia-like fractures, there are some limitations. The surgical procedure included in this study was performed by a single surgeon with extensive experience in upper extremity trauma. The outcomes achieved may not be representative of those achieved by surgeons with different levels of expertise or in centers with varying levels of resources. Also, due to the uncommon nature of this injury, a control group was not included in this study. Nonetheless, a comparison of the study outcomes with the results presented in the current literature yields satisfactory results.
6. Conclusions
Overall, the trans-olecranon, single-incision approach is a valuable technique for managing fractures involving the proximal ulna and radial head. It allows sufficient access to the lateral structures of the elbow while minimizing secondary damage to the surrounding soft tissue, leading to satisfactory clinical and radiological outcomes. This approach should be considered for patients with a Monteggia-equivalent fracture. This article provides a step-by-step description of the procedure, highlighting key surgical landmarks.
Author Contributions
D.S.Z.—Conceptualization, data interpretation, and writing of the manuscript. I.R.—Data analysis and revision of the manuscript. D.N.—Data collection and writing of the manuscript. J.D.—Data collection/analysis and writing of the manuscript. B.P.—Data analysis and revision of the manuscript. N.G.—Review and editing, data interpretation, and revision of the manuscript. J.S.—Data interpretation, supervision, revision of the manuscript, and writing of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was performed in accordance with the ethical standards in the 1964 Declaration of Helsinki. Details that might disclose the identity of the subjects under study have been omitted. This study was approved by the Rambam Medical Center’s Helsinki committee, (IRB). (IRB ID: RMB-0789-020).
Informed Consent Statement
The local Institutional Ethical Committee approved the design of this study, and considering its observational nature, waived requirements for informed consent from the patients.
Data Availability Statement
The datasets presented in this article are not readily available because of technical limitations. Requests to access the datasets should be directed to the corresponding author.
Acknowledgments
Thanks to Yaron Katz for his help with the graphics.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Carroll, P.J.; Morrissey, D.I. Posterior (Boyd) approach to terrible triad injuries. JSES Int. 2022, 6, 315–320. [Google Scholar] [CrossRef]
- Colliton, E.; Leung, N. Transolecranon exposure of monteggia variant fracture-dislocations of the elbow. Tech. Hand Up. Extrem. Surg. 2021, 25, 111–115. [Google Scholar] [CrossRef]
- Colliton, E.; Lovett, J.; Lee, S.; Leung, N. Outcomes of Posterior Monteggia Variant Fractures Repaired Through a Trans-Olecranon Approach. J. Hand Surg. Glob. Online 2022, 4, 337–343. [Google Scholar] [CrossRef]
- Egol, K.A.; Tejwani, N.C.; Bazzi, J.; Susarla, A.; Koval, K.J. Does a Monteggia variant lesion result in a poor functional outcome? A retrospective study. Clin. Orthop. Relat. Res. 2005, 438, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Gauci, M.O.; Winter, M.; Dumontier, C.; Bronsard, N.; Allieu, Y. Clinical and radiologic outcomes of pyrocarbon radial head prosthesis: Midterm results. J. Shoulder. Elb. Surg. 2016, 25, 98–104. [Google Scholar] [CrossRef]
- Josten, C.; Freitag, S. Monteggia and monteggia-like-lesions: Classification, indication, and techniques in operative treatment. Eur. J. Trauma Emerg. Surg. 2009, 35, 296–304. [Google Scholar] [CrossRef]
- Jung, M.; Groetzner-Schmidt, C.; Porschke, F.; Grützner, P.A.; Guehring, T.; Schnetzke, M. Monteggia-like lesions in adults treated with radial head arthroplasty-mid-term follow-up of 27 cases. J. Orthop. Surg. Res. 2020, 15, 5. [Google Scholar] [CrossRef] [PubMed]
- Jupiter, J.B.; Leibovic, S.J.; Ribbans, W.; Wilk, R.M. The posterior monteggia lesion. J. Orthop. Trauma 1991, 5, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Kaas, L.; van Riet, R.P.; Vroemen, J.P.A.M.; Eygendaal, D. The incidence of associated fractures of the upper limb in fractures of the radial head. Strateg. Trauma Limb Reconstr. 2008, 3, 71–74. [Google Scholar] [CrossRef]
- Kachooei, A.R.; Baradaran, A.; Ebrahimzadeh, M.H.; van Dijk, C.N.; Chen, N. The Rate of Radial Head Prosthesis Removal or Revision: A Systematic Review and Meta-Analysis. J. Hand Surg. 2018, 43, 39–53.e1. [Google Scholar] [CrossRef]
- Kaur, M.N.; MacDermid, J.C.; Grewal, R.R.; Stratford, P.W.; Woodhouse, L.J. Functional outcomes post-radial head arthroplasty: A systematic review of literature. Shoulder Elb. 2014, 6, 108–118. [Google Scholar] [CrossRef] [PubMed]
- Klug, A.; Konrad, F.; Gramlich, Y.; Hoffmann, R.; Schmidt-Horlohé, K. Surgical treatment of the radial head is critical to the outcome of Monteggia-like lesions. Bone Jt. J. 2019, 101, 1512–1519. [Google Scholar] [CrossRef] [PubMed]
- Konrad, G.G.; Kundel, K.; Kreuz, P.C.; Oberst, M.; Sudkamp, N.P. Monteggia fractures in adults long-term results and prognostic factors. J. Bone Jt. Surg. 2007, 89, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Laun, R.; Wild, M.; Brosius, L.; Hakimi, M. Monteggia-like lesions-treatment strategies and one-year results. GMS Interdiscip. Plast. Reconstr. Surg. DGPW 2015, 4, Doc13. [Google Scholar] [CrossRef]
- Levy, J.C.; Formaini, N.T.; Kurowicki, J. Outcomes and radiographic findings of anatomic press-fit radial head arthroplasty. J. Shoulder Elb. Surg. 2016, 25, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Mehta, J.A.; Bain, G.I. Surgical approaches to the elbow. Hand Clin. 2004, 20, 375–387. [Google Scholar] [CrossRef] [PubMed]
- Rahmi, H.; Kozusko, S.D.; Fuller, D. Transolecranon surgical approach for radial head arthroplasty. Orthopedics 2016, 9, e992–e996. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Van Riet, R.P.; Morrey, B.F.; O’Driscoll, S.W.; van Glabbeek, F. Associated injuries complicating radial head fractures: A demographic study. Clin. Orthop. Relat. Res. 2005, 441, 351–355. [Google Scholar] [CrossRef] [PubMed]
- Ring, D. Monteggia Fractures. Orthop. Clin. North Am. 2013, 44, 59–66. [Google Scholar] [CrossRef]
- Robinson, P.M.; Li, M.K.H.; Dattani, R.; Van Rensburg, L. The boyd interval: A modification for use in the management of elbow trauma. Tech. Hand Up. Extrem. Surg. 2016, 20, 37–41. [Google Scholar] [CrossRef]
- Sardelli, M.; Tashjian, R.Z.; MacWilliams, B.A. Functional elbow range of motion for contemporary tasks. J. Bone Jt. Surg. 2011, 93, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Weber, M.M.; Rosteius, T.; Schildhauer, T.A.; Königshausen, M.; Rausch, V. Monteggia fractures and Monteggia-like-lesions: A systematic review. Arch. Orthop. Trauma Surg. 2023, 143, 4085–4093. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).