Can Subscapularis Augmentation Serve as an Alternative to the Remplissage Procedure? A Case Report
Abstract
1. Introduction
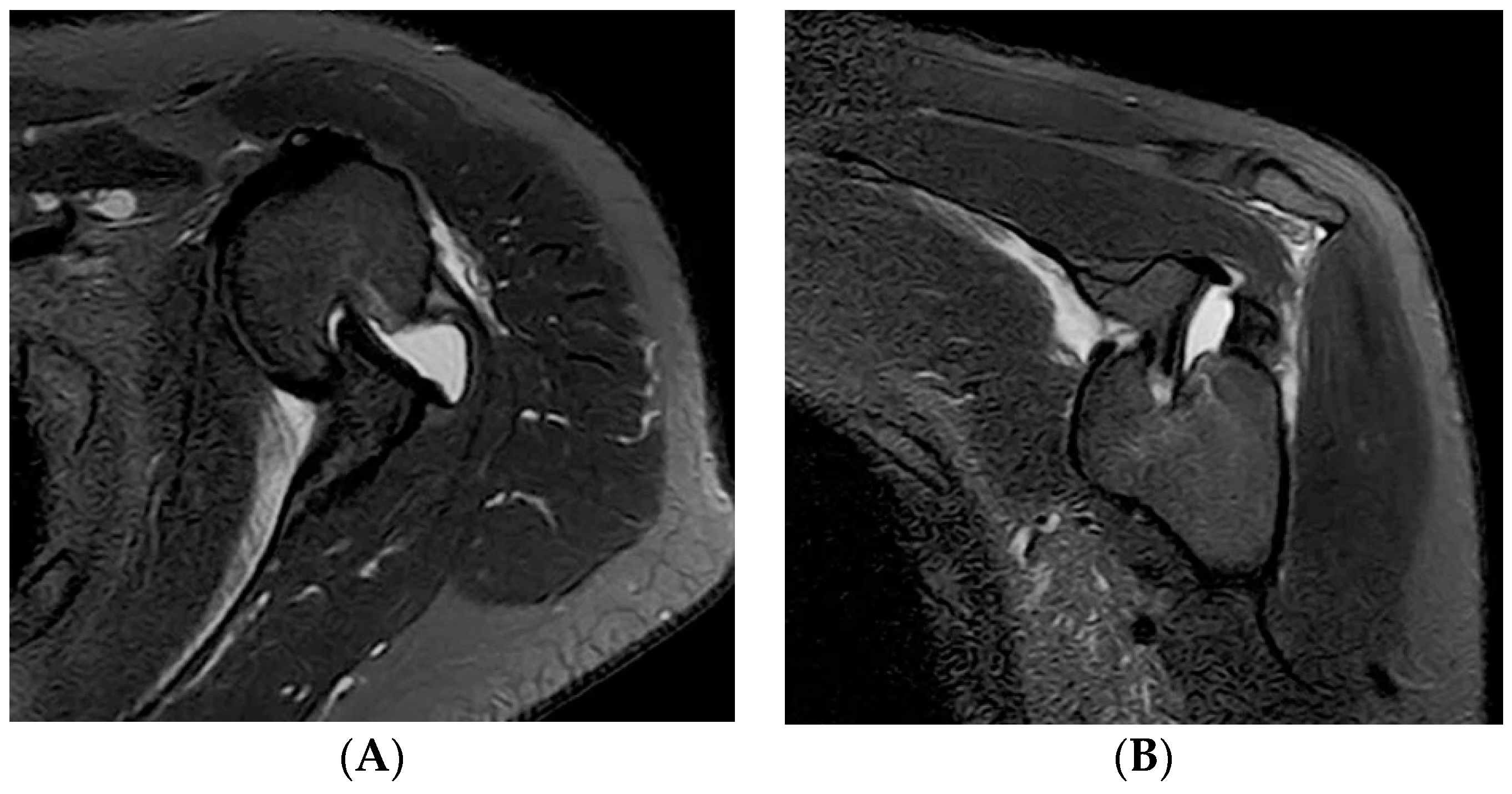
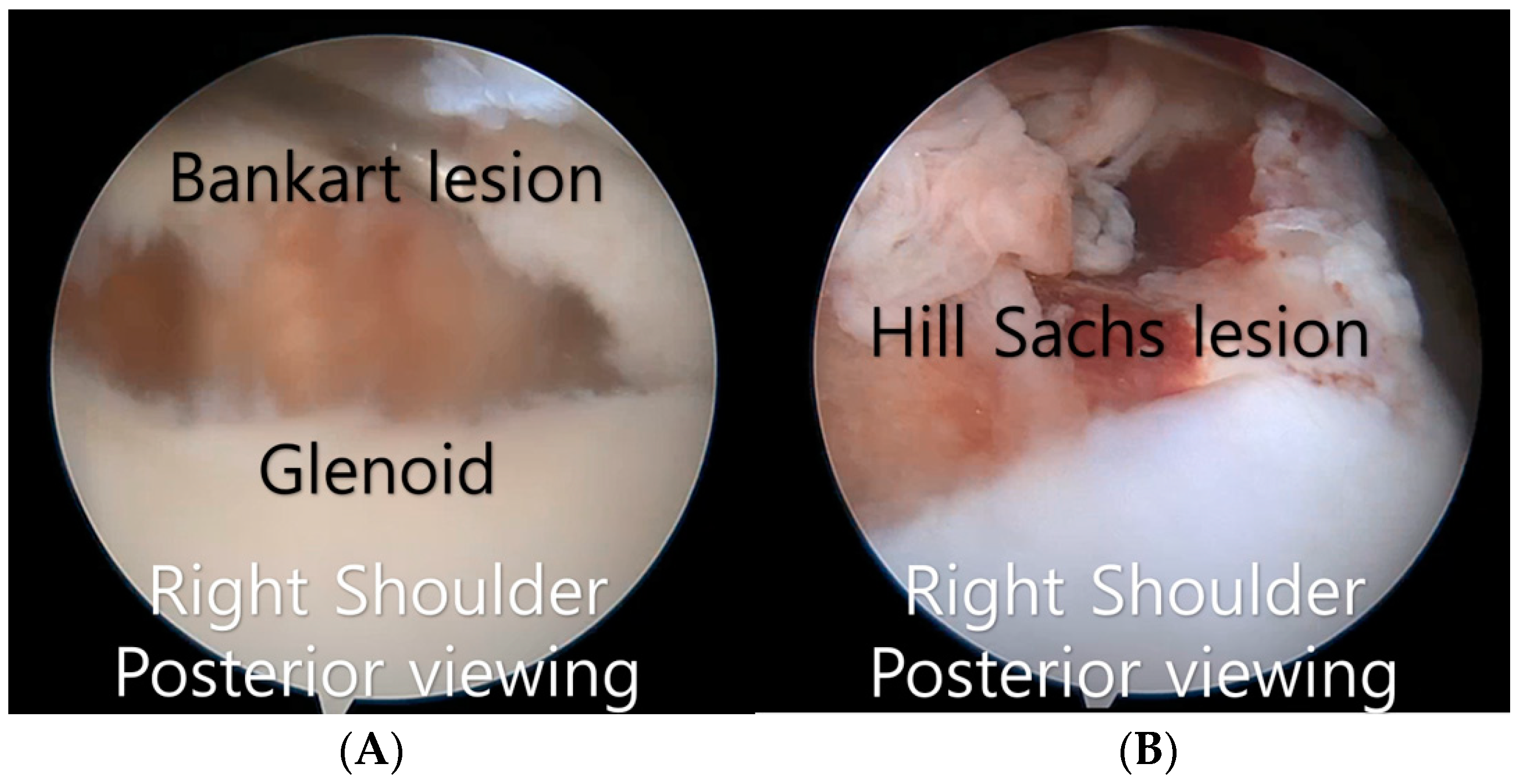
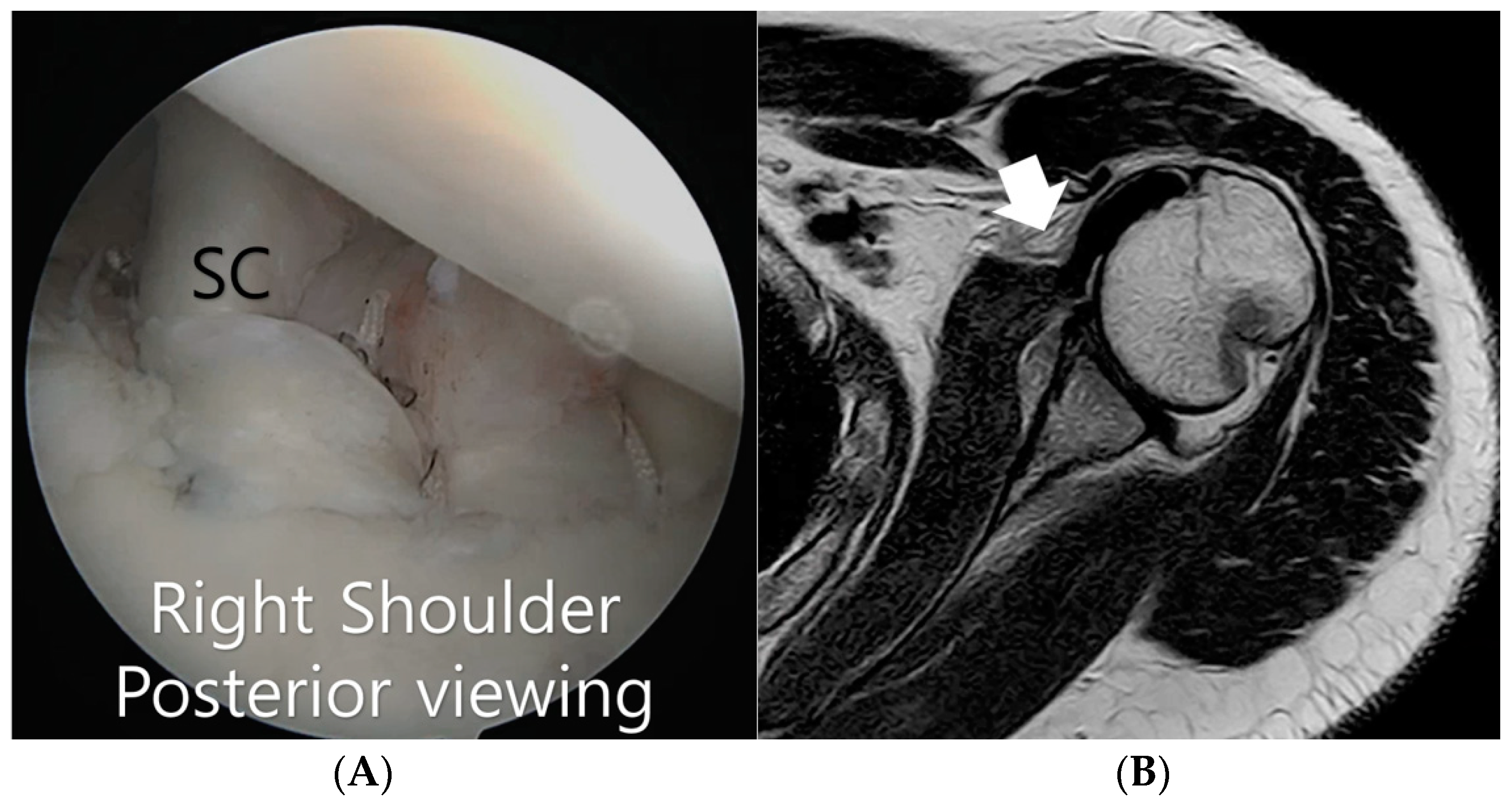
2. Case
3. Surgical Technique
4. Postoperative Rehabilitation
5. Discussion
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Di Giacomo, G.; Itoi, E.; Burkhart, S.S. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: From “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy 2014, 30, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Itoi, E. ‘On-track’ and ‘off-track’ shoulder lesions. EFORT Open Rev. 2017, 2, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Burkhart, S.S.; De Beer, J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000, 16, 677–694. [Google Scholar] [CrossRef] [PubMed]
- Rashid, M.S.; Crichton, J.; Butt, U.; Akimau, P.I.; Charalambous, C.P. Arthroscopic “Remplissage” for shoulder instability: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 578–584. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Lee, K.H.; Park, D.H.; Lee, B.G. Is revision remplissage possible for failed primary remplissage operation?: A case report. J. Shoulder Elbow Surg. 2014, 23, e256–e260. [Google Scholar] [CrossRef] [PubMed]
- Goudie, E.B.; Murray, I.R.; Robinson, C.M. Instability of the shoulder following seizures. J. Bone Jt. Surg. Br. Vol. 2012, 94, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Thangarajah, T.; Lambert, S. The management of recurrent shoulder instability in patients with epilepsy: A 15-year experience. J. Shoulder Elbow Surg. 2015, 24, 1723–1727. [Google Scholar] [CrossRef] [PubMed]
- Buhler, M.; Gerber, C. Shoulder instability related to epileptic seizures. J. Shoulder Elbow Surg. 2002, 11, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Lim, K.H.; Kim, J.W. Risk factors for recurrence of anterior-inferior instability of the shoulder after arthroscopic Bankart repair in patients younger than 30 years. Arthroscopy 2018, 34, 2530–2536. [Google Scholar] [CrossRef] [PubMed]
- Purchase, R.J.; Wolf, E.M.; Hobgood, E.R.; Pollock, M.E.; Smalley, C.C. Hill-Sachs “remplissage”: An arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy 2008, 24, 723–726. [Google Scholar] [CrossRef] [PubMed]
- Guity, M.R.; Sobhani, E.A. Mid-term results of arthroscopic Bankart repair and remplissage for recurrent anterior shoulder instability in patients with a history of seizures. BMC Musculoskelet. Disord. 2022, 23, 12. [Google Scholar] [CrossRef] [PubMed]
- Russo, R.; Della Rotonda, G.; Cautiero, F.; Ciccarelli, M.; Maiotti, M.; Massoni, C.; Di Pietto, F.; Zappia, M. Arthroscopic Bankart repair associated with subscapularis augmentation (ASA) versus open Latarjet to treat recurrent anterior shoulder instability with moderate glenoid bone loss: Clinical comparison of two series. Musculoskelet. Surg. 2017, 101, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Schröter, S.; Krämer, M.; Welke, B.; Hurschler, C.; Russo, R.; Herbst, M.; Stöckle, U.; Ateschrang, A.; Maiotti, M. The effect of the arthroscopic augmentation of the subscapularis tendon on shoulder instability and range of motion: A biomechanical study. Clin. Biomech. 2016, 38, 75–83. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, D.; Seo, J.; Jung, J.; Yoo, J. Can Subscapularis Augmentation Serve as an Alternative to the Remplissage Procedure? A Case Report. Surgeries 2024, 5, 571-576. https://doi.org/10.3390/surgeries5030046
Lee D, Seo J, Jung J, Yoo J. Can Subscapularis Augmentation Serve as an Alternative to the Remplissage Procedure? A Case Report. Surgeries. 2024; 5(3):571-576. https://doi.org/10.3390/surgeries5030046
Chicago/Turabian StyleLee, Daehee, Joongbae Seo, Jaewook Jung, and Jaesung Yoo. 2024. "Can Subscapularis Augmentation Serve as an Alternative to the Remplissage Procedure? A Case Report" Surgeries 5, no. 3: 571-576. https://doi.org/10.3390/surgeries5030046
APA StyleLee, D., Seo, J., Jung, J., & Yoo, J. (2024). Can Subscapularis Augmentation Serve as an Alternative to the Remplissage Procedure? A Case Report. Surgeries, 5(3), 571-576. https://doi.org/10.3390/surgeries5030046







